ACLS EP cardiac1
-
Upload
brentupdegraff -
Category
Documents
-
view
229 -
download
0
Transcript of ACLS EP cardiac1
-
7/27/2019 ACLS EP cardiac1
1/48
1
Learning Station 1
CardiovascularEmergencies Case 11999 American Heart Association
-
7/27/2019 ACLS EP cardiac1
2/48
2
Acknowledgments
Janice Ritchie Saia, RN, EMT-P, of St. Petersburg,
FL, first developed these materials. She has
generously donated her work to the AHA. Steve Anderson, MD, of Auburn, WA, provided
helpful scripts for this case.
Mary Fran Hazinski, RN, MSN, and John Field, MD,
provided many refinements during final review. We
appreciate the hard work of each of these people.
2
-
7/27/2019 ACLS EP cardiac1
3/48
3
Learning Objectives
Apply the Five Quadrads Approach to patients withcomplex cardiovascular emergencies
Discuss, assess, and manage acute MI
Identify ECG changes consistent with
Myocardial ischemia/infarction
Location of infarct
Infarct-related coronary artery
After completing this learning station you should beable to
-
7/27/2019 ACLS EP cardiac1
4/48
4
Case History
Mr. B. Skimmer, age 45, complains of chest
discomfort, nausea, severe fatigue
Past Med Hx: hypertension (poor control),
2 to 3 pack/day cigarettes, high stress job
Refuses coworkers assistance
States: Its just the flu
Goes to break room to rest
-
7/27/2019 ACLS EP cardiac1
5/48
5
Case Progression
One hour later a coworker finds Mr. Skimmer
lethargic, pale, profusely diaphoretic
Coworker offers to drive Mr. Skimmer to ED,
only 3 minutes away
Should M r. Skimmer go to ED byALS ambulance?
WHY?
-
7/27/2019 ACLS EP cardiac1
6/48
6
Case Progression
Mr. Skimmer arrives at your ED with O2
via NRB; IV LR @ KVO
Received MONA in field; BP dropped
alarmingly, near syncope
Triaged as urgent
Placed in ED critical care bed
What should youas the key
ACLS providerdo first?
-
7/27/2019 ACLS EP cardiac1
7/487
The Five Quadrads Approachto ACLS-EP
1. Primary ABCD Survey
2. Secondary ABCD Survey
3. OxygenIVmonitorfluids
4. TempBPHRRR
5. Tanktankpumprate
-
7/27/2019 ACLS EP cardiac1
8/488
AssessmentF ive Quadrads Approach
Primary Survey
Airway: adequate
Breathing: present with equal chest rise,
adequate tidal volume
Circulation: pulse present carotid and
radial
Defibrillation: not needed
-
7/27/2019 ACLS EP cardiac1
9/48
9
Secondary Survey
Airway: adequate
Breathing: lung sounds clearOxygen sat 97% with NRB
Circulation: sinus rhythm
2-mm ST-elevation in leads II, III, aVF
BP 126/84 mm Hg; IV access present
Differential diagnosis: AMI. Others?
AssessmentF ive Quadrads Approach
-
7/27/2019 ACLS EP cardiac1
10/48
10
OxygenIVmonitorfluids
Started by EMS; continued in ED
Vital signs
T=99.1F, BP=126/84 mm Hg,HR=74 bpm, RR=28/min
Tanktankpumprate Consider sources of hemodynamic
compromise
AssessmentF ive Quadrads Approach
-
7/27/2019 ACLS EP cardiac1
11/48
11
What would you like to doNOW?
-
7/27/2019 ACLS EP cardiac1
12/48
12
Immediate ED Assessments
O2IVmonitorfluids (done by EMS)
Grade chest pain: character, intensity
H & P: focus on thrombolytic screening
VSfrequent recordings
Multilead ECG? (12, 15, or 22 leads)
First set serum markers Electrolytes; coagulation studies
Portable chest film
-
7/27/2019 ACLS EP cardiac1
13/48
13
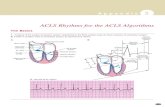
12-Lead ECG Findings
1. ST-segment
elevationor new LBBB
strongly suspicious
for injury
2. ST-segment
depression/dynamicT-wave inversion;
strongly suspicious
for ischemia
3. Nondiagnostic
or normal ECG;chest pain strongly
suspicious for
ischemia
-
7/27/2019 ACLS EP cardiac1
14/48
14
Localizing Ischemia or Injury
aVF inferiorIII inferior V3 anterior V6 lateral
aVL lateralII inferior V2 septal V5 lateral
aVRI lateral V1 septal V4 anterior
-
7/27/2019 ACLS EP cardiac1
15/48
15
ECG 1: Interpretation?
-
7/27/2019 ACLS EP cardiac1
16/48
16
ECG 1: elevated ST segments; inferior leads (II, III, aVF);ST depression: precordial leads V2-V5; lateral leads I, aVL
Suspect occlusionr ight coronary artery
-
7/27/2019 ACLS EP cardiac1
17/48
17
Coronary Artery Distribution
Left
Septal wall of LV
Anterior and lateral
walls of LV
Inferior wall LV
(10%)
Both bundle branches
Right
Inferior wall of LV
Posterior wall of
LV (90%)
AV node (90%)
Right ventricle
-
7/27/2019 ACLS EP cardiac1
18/48
18
Cardiac Anatomy in Relationto Coronary Artery
Rightcoronary
artery
Septal wallV1-V2
Left anteriordescending artery
Anterior wallV3-V4
Left main
coronaryartery
Circumflexartery
Lateral wallI, aVL, V5-V6
-
7/27/2019 ACLS EP cardiac1
19/48
19
NOTE 1: Inferior wallsupplied by either the right
(85% to 90% of people) or
left coronary artery.
NOTE 2: If there is acute
injury in inferior leads(II, III, aVF), unknown
whether left or right
coronary artery is blocked.
NOTE 3: KEYyou
must obtain a RIGHT-SIDED ECG at once.
Posterior View of the Heart
HOW TO GET
RIGHT-SIDED ECG?
Leads II, III, aVF
(from leftcoronaryartery)
Lateral wall
Inferior wall
Right coronaryartery
Posteriordescending
artery
Posteriorwall
Circumflexartery
-
7/27/2019 ACLS EP cardiac1
20/48
20
Lead Placement for aRight-sided ECG
V1
V3R
V4RV5
RV6R
V2
-
7/27/2019 ACLS EP cardiac1
21/48
21
Right Ventricular Infarction
Inferior lead changes RV infarction?
Use lead V4R (ST elevation >1 mm)
Clinical significance:
Increased mortality
Preload dependence
Vasodilators may cause severe hypotension
What is management of RV infarction?
-
7/27/2019 ACLS EP cardiac1
22/48
22
How would you managethis patient?
-
7/27/2019 ACLS EP cardiac1
23/48
-
7/27/2019 ACLS EP cardiac1
24/48
24
Nitroglycerin
Mechanism of action
Indications
Administration
Cautions
-
7/27/2019 ACLS EP cardiac1
25/48
25
Narcotic Analgesia
Morphine sulfatereadily available
Effects
Relieves pain and anxiety Reduces myocardial oxygen needs
Administration
2 to 5 mg IV q 5 minutes (slow) Caution
N & V, low BP, respiratory depression
-
7/27/2019 ACLS EP cardiac1
26/48
26
Aspirin
Aspirin inhibits platelet cyclo-oxygenase
decreases thromboxane A2 production
Aspirin benefits
Reduces overall mortality in AMI
Reduces incidence of nonfatal reinfarction
Dose: 160 to 325 mg PO ASAP
-
7/27/2019 ACLS EP cardiac1
27/48
27
-BlockersMechanism of action
Block catecholamines from binding to
-adrenergic receptors
Nonselective and cardioselective
Reduce HR, BP, myocardial
contractility, and oxygen consumption
Decrease AV nodal conduction
-
7/27/2019 ACLS EP cardiac1
28/48
28
-Blockers
Severe CHF/PE Hypotension
(SBP
-
7/27/2019 ACLS EP cardiac1
29/48
29
Heparin
Mechanism of action
Indirect thrombin inhibitor (with AT III)
Indications
PTCA or CABG
With fibrin-specific lytics (eg, alteplase)
High risk for systemic emboli Large anterior MI, atrial fib, LV thrombus
-
7/27/2019 ACLS EP cardiac1
30/48
30
ACE Inhibitors
Mechanism of action
Lower BP by inhibiting angiotensin-
converting enzyme (ACE) Attenuate LV remodeling by inhibiting
tissue ACE
Lower peripheral vascular resistance byvasodilatation mechanism
Reduce mortality from AMI
P t i d
-
7/27/2019 ACLS EP cardiac1
31/48
31
Potassium andMagnesium Sulfate
Potassium deficiency but not magnesium
deficiency associated with arrhythmias,
sudden death Recent studies suggest no reduction in AMI
mortality with magnesium administration
-
7/27/2019 ACLS EP cardiac1
32/48
32
I s M r. Skimmer a candidate for
thrombolysis?
What information do you need to
make this decision?
Case Progression
C t i di ti t
-
7/27/2019 ACLS EP cardiac1
33/48
33
Contraindications toThrombolytic Therapy
Previous hemorrhagicstroke any time
Other stroke, CVAwithin 1 year; ICneoplasm
Active internal bleeding(not menses)
Suspected aorticdissection
Severe uncontrolledhypertension (>180/110)
Current use ofanticoagulants
Recent trauma (2 to 4 wk);major surgery
-
7/27/2019 ACLS EP cardiac1
34/48
34
Percutaneous TransluminalCoronary Angioplasty
Direct treatment
Mechanical reperfusion of infarct-related
coronary artery
Best outcome achieved for patients with AMI
plus cardiogenic shock
-
7/27/2019 ACLS EP cardiac1
35/48
35
Case Progression
Mr. Skimmer received oxygen, aspirin,
metoprolol IV, and heparin
No nitroglycerin or morphine in ED
Now pain-free; stable BP; O2 sat 98%
Reperfusion therapy: t-PA + heparin
-
7/27/2019 ACLS EP cardiac1
36/48
36
ECG 2: Interpretation?
-
7/27/2019 ACLS EP cardiac1
37/48
37
Case Progression
Mr. Skimmer transferred to CCU
Uneventful night
No chest pain or shortness of breathNo arrhythmias
Treatment:
Oxygen at 2 L/min Heparin, ACE inhibitors, -blockers
Nitroglycerin not given
-
7/27/2019 ACLS EP cardiac1
38/48
38
The next day
In CCU Mr. Skimmer begins complaining of
Chest pressure
Light-headedness
Increasing intensity over 20 minutes
What should you do now?
-
7/27/2019 ACLS EP cardiac1
39/48
39
The Five Quadrads
Primary Survey: no CPR or defibrillation indicated
Secondary Survey
Airway: adequate Breathing: dyspnea, + JVD, rales in lower third
of lung fields
Circulation: diaphoretic; peripheralpulses weak
Differential diagnosis: obtain 12-lead ECG
-
7/27/2019 ACLS EP cardiac1
40/48
40
The Five Quadrads
OxygenIVmonitorfluids
Vital signs
BP 76/64 mm Hg, HR 80 bpm, RR 32/min
Tanktankpumprate
What is the nature of the problem?
Check 12-lead ECG
-
7/27/2019 ACLS EP cardiac1
41/48
41
ECG 3: Interpretation?
SR with ST-segment elevation in leads II, III,
aVF; reciprocal changes throughout
T t t C id ti
-
7/27/2019 ACLS EP cardiac1
42/48
42
Treatment ConsiderationsAcute Pulmonary Edema With Hypotension
Oxygen
Furosemide Avoid, if possible,
nitroglycerin or
morphine, especially if
patient is hypotensive
Dopamine
Dobutamine PEEP (caution)
CPAP
First-line Actions Second-line Actions
-
7/27/2019 ACLS EP cardiac1
43/48
43
Treatment Considerations
Priority actions
Thrombolytic therapy (repeat t-PA)
Coronary angiography and angioplasty or
emergency surgical revascularization
Intra-aortic balloon pump
-
7/27/2019 ACLS EP cardiac1
44/48
44
Differential Diagnosis
Reocclusion RCA; infarct extension
Mechanical complications (eg, mitral
regurgitation, VSD)
Low cardiac output
Pulmonary embolus
-
7/27/2019 ACLS EP cardiac1
45/48
45
Case Progression
Pulmonary edema persists
Cardiogenic shock continues
Patient remains hypotensive
ECG: ST elevation consistent with reocclusion
Strategy: coronary angiography
Outcome: angioplasty and stent proximal RCA
-
7/27/2019 ACLS EP cardiac1
46/48
46
Summary
Five Quadrads Layered approach; guides actions and thinking
Apply whenever you arrive at an emergency setting Goals of coronary syndrome treatment
Early reperfusion therapy (myocardial salvage) whenindicated
Reduce morbidity and mortality through adjunctive agents(ASA, -blockers, ACE, statins)
Recognize and anticipate serious early complications:unstable post-MI angina, CHF, late VT/VF
-
7/27/2019 ACLS EP cardiac1
47/48
47
Summary
A focused history and assessment facilitates
early initiation of reperfusion therapy
The 12-lead ECG may be used to localizeinjury and guide therapy
Serum markers may be used to triage patients
and assess prognosis
-
7/27/2019 ACLS EP cardiac1
48/48
Summary
Several treatments help patients by
Decreasing mortality
Limiting extent of infarction Limiting incidence of reinfarction
Knowledge of complicated AMIs enables us to
Anticipate complications Care for patients with complex acute coronary
syndromes