CPR2015 update: Adult ACLS
-
Upload
narenthorn-ems-center -
Category
Health & Medicine
-
view
1.651 -
download
1
Transcript of CPR2015 update: Adult ACLS

Adult Advanced Cardiovascular Life SupportPart 7


Oxygen Dose During CPR
2015 Recommendation-updated Class
When supplementary oxygen is available, it may be reasonable to use the maximal feasible inspired oxygen concentration during CPR
IIb, LOE C-EO
The higher ranges of arterial Po2 during CPR were associated with an increase in hospital admission rates. However, there was no statistical difference in overall neurologic survival

Monitoring Physiologic ParametersDuring CPR
2015 Recommendation—Updated Class
It may be reasonable to use physiologicparameters (quantitative waveform capnography, arterial relaxation diastolic pressure, arterial pressure monitoring, and ScVO2) when feasible to monitor and optimize CPR quality, guide vasopressortherapy, and detect ROSC
IIb, LOE C-EO

Ultrasound During Cardiac Arrest
2015 Recommendations—Updated Class
Ultrasound (cardiac or noncardiac) may be considered during the management of cardiac arrest, although its usefulness hasnot been well established
Class IIb, LOE C-EO

Ultrasound During Cardiac Arrest
2015 Recommendations—Updated Class
If a qualified sonographer is present and use of ultrasound does not interfere with the standard cardiac arrest treatment protocol, then ultrasound may be considered as an adjunct tostandard patient evaluation
IIb, LOE C-EO


Bag-Mask Ventilation Compared With AnyAdvanced Airway During CPR
2015 Recommendations—Updated Class
Either a bag-mask device or an advanced airway may be used for oxygenation and ventilation during CPR in both the inhospital and out-of-hospital setting
IIb, LOE C-LD
For healthcare providers trained in their use, either an SGA device or an ETT may be used as the initialAdvanced airway during CPR
IIb, LOE C-LD

Clinical Assessment of Tracheal Tube Placement
2015 Recommendations—Updated Class
Continuous waveform capnography is recommended in addition to clinical assessment as the most reliable method of confirming and monitoring correct placement of an ETT
I,LOE C-LD
If continuous waveform capnometry is not available, a nonwaveform CO2 detector, esophageal detector device, orultrasound used by an experienced operator is a reasonable alternative
IIa, LOE C-LD

Ventilation After Advanced Airway Placement
2015 Recommendation—Updated Class
After placement of an advanced airway, it may be reasonable for the provider to deliver 1 breath every 6 seconds (10breaths/min) while continuous chest compressions are being performed
IIb, LOE C-LD


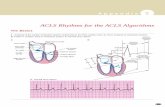
Defibrillation Strategies for VF or Pulseless VT: WaveformEnergy and First-Shock Success
2015 Recommendations—Updated Class
Defibrillators (using BTE, RLB, or monophasic waveforms) are recommended to treat atrial and ventricular arrhythmias
I, LOE B-NR
Using biphasic waveforms (BTE or RLB) are preferred to monophasicdefibrillators for treatment of bothatrial and ventricular arrhythmias
IIa, LOE B-R

Defibrillation Strategies for VF or Pulseless VT: Waveform Energy and First-Shock Success
2015 Recommendations—Updated Class
it is reasonable to use the manufacturer’s recommended energy dose for the first shock. If this is not known, defibrillation at the maximal dose may be considered
IIb, LOE C-LD

Defibrillation Strategies for VF or Pulseless VT: Energy Dose for Subsequent Shocks
2015 Recommendations—Updated Class
It is reasonable that selection of fixed versus escalating energy for subsequent shocks be based on the specific manufacturer’s instructions
IIa, LOE C-LD
If using a manual defibrillator capable of escalating energies,higher energy for second and subsequent shocks may beconsidered
IIb, LOE C-LD

Defibrillation Strategies for VF or Pulseless VT : Single Shocks Versus Stacked Shocks
2015 Recommendation—Updated Class
A single-shock strategy (as opposed to stacked shocks) is reasonable for defibrillation
IIa, LOE B-NR


Antiarrhythmic Therapy for Refractory VF/pVT Arrest
2015 Recommendations—Updated Class
Amiodarone may be considered for VF/pVTthat is unresponsive to CPR, defibrillation, and a vasopressor therapy
IIb, LOE B-R
Lidocaine may be considered as an alternative to amiodarone for VF/pVT that is unresponsive to CPR, defibrillation,and vasopressor therapy
IIb, LOE C-LD
The routine use of magnesium for VF/pVT is not recommended in adult patients
III: No Benefit, LOE B-R

Antiarrhythmic Drugs After Resuscitation
2015 Recommendations—New Class
•There is inadequate evidence to support the routine use of lidocaine after cardiac arrest. •However, the initiation or continuation of lidocaine may be considered immediately after ROSC from cardiac arrest due to VF/pVT
IIb, LOE C-LD

Antiarrhythmic Drugs After Resuscitation
2015 Recommendations—New Class
•There is inadequate evidence to support the routine use of a β-blocker after cardiac arrest. •However, the initiation or continuation of an oral or intravenous β-blocker may be considered early after hospitalization from cardiac arrest due to VF/pVT
IIb, LOE C-LD


Standard-Dose Epinephrine
2015 Recommendation—Updated Class
Standard-dose epinephrine (1 mg every 3 to 5 minutes) may be reasonable for patients in cardiac arrest
IIb, LOE B-R

Standard Dose Epinephrine Versus High-DoseEpinephrine
2015 Recommendation—New Class
High-dose epinephrine is not recommended for routine use incardiac arrest
III: No Benefit, LOE B-R

Epinephrine Versus Vasopressin
2015 Recommendation—Updated Class
Vasopressin offers no advantage as a substitute for epinephrine in cardiac arrest
IIb, LOE B-R
•The removal of vasopressin has been noted in the Adult Cardiac Arrest Algorithm

Epinephrine Versus Vasopressin in Combination With Epinephrine
2015 Recommendation—New Class
Vasopressin in combination with epinephrine offers no advantage as a substitute for standard-dose epinephrine in cardiac arrest
IIb, LOE B-R

Timing of Administration of Epinephrine
2015 Recommendations—Updated Class
It may be reasonable to administer epinephrine as soon as feasible after the onset of cardiac arrest due to an initial nonshockable rhythm
IIb, LOE C-LD

Steroids
2015 Recommendations—New Class
•In IHCA, the combination of intra-arrest vasopressin, epinephrine, and methylprednisolone and post-arrest hydrocortisone may be considered;•However, further studies are needed before recommending the routine use of this therapeutic strategy
IIb,LOE C-LD

Steroids
2015 Recommendations—New Class
For patients with OHCA, use of steroids during CPR is of uncertain benefit
IIb, LOE C-LD

Prognostication During CPR:End-Tidal CO2
2015 Recommendations—New Class
In intubated patients, failure to achieve an ETCO2 > 10 mmHg by waveform capnography after 20 minutes of CPR may be considered as one component of a multimodal approach to decide when to end resuscitative efforts, but it should not be used in isolation
IIb,LOE C-LD

Prognostication During CPR:End-Tidal CO2
2015 Recommendations—New Class
In nonintubated patients, a specific ETCO2 cutoff value at any time during CPR should not be used as an indication to end resuscitative efforts
III: Harm, LOE C-EO

Overview of Extracorporeal CPR
2015 Recommendation—New Class
There is insufficient evidence to recommend the routine use of ECPR for patients with cardiac arrest. In settings where it can be rapidly implemented, ECPR may be considered for select cardiac arrest patients for whom the suspected etiology of the cardiac arrest is potentially reversible during a limited period of mechanical cardiorespiratory support
IIb,LOE C-LD


Post–Cardiac Arrest CarePart 8


Acute Cardiovascular Interventions
2015 Recommendations—Updated Class
Coronary angiography should be performed emergently (rather than later in the hospital stay or not at all) for OHCApatients with suspected cardiac etiology of arrest and ST elevation on ECG
I, LOE B-NR

Acute Cardiovascular Interventions
2015 Recommendations—Updated Class
Emergency coronary angiography is reasonable for select (eg, electrically or hemodynamically unstable) adult patients who are comatose after OHCA of suspected cardiac origin but without ST elevation on ECG
IIa, LOE B-NR

Acute Cardiovascular Interventions
2015 Recommendations—Updated Class
Coronary angiography is reasonable in post–cardiac arrest patients for whom coronary angiography is indicated regardless of whether the patient is comatose or awake
IIa,LOE C-LD

Hemodynamic Goals
2015 Recommendation—New Class
Avoiding and immediately correcting hypotension (systolic blood pressure less than 90 mm Hg, MAP less than 65 mm Hg) during postresuscitation care may be reasonable
IIb,LOE C-LD


Induced Hypothermia2015 Recommendations—Updated Class
Recommend that comatose (ie, lack of meaningful response to verbal commands) adult patients with ROSC after cardiac arrest have TTM
•Class I, LOE B-R for VF/pVT OHCA
•Class I, LOE C-EO for non-VF/pVT
Recommend selecting and maintaining a constant temperature between 32C and 36C during TTM
Class I, LOE B-R
It is reasonable that TTM be maintained for at least 24 hours after achieving target temperature
Class IIa, LOE C-EO

Hypothermia in the Prehospital Setting
2015 Recommendation—New Class
We recommend against the routine prehospital cooling of patients after ROSC with rapid infusion of cold intravenous fluids
Classs III: No benefit, LOE A

Avoidance of Hyperthermia
2015 Recommendation—New Class
It may be reasonable to actively prevent fever in comatose patients after TTM
IIb, LOE C-LD


Seizure Management
2015 Recommendations—Updated Class
An EEG for the diagnosis of seizure should be promptly performed and interpreted, and then should be monitored frequently or continuously in comatose patients after ROSC
I, LOE C-LD
The same anticonvulsant regimens for the treatment of status epilepticuscaused by other etiologies may be considered after cardiac arrest
IIb, LOE C-LD


Ventilation
2015 Recommendation—Updated Class
Maintaining the PaCo2 within a normal physiological range, taking into account any temperature correction, may be reasonable
IIb, LOE B-NR

Oxygenation
2015 Recommendations—New and Updated Class
To avoid hypoxia in adults with ROSC after cardiac arrest, it is reasonable to use the highest available oxygen concentration until the arterial oxyhemoglobin saturation or the partial pressureof arterial oxygen can be measured
IIa, LOE C-EO

Oxygenation
2015 Recommendations—New and Updated Class
When resources are available to titrate the Fio2 and to monitor O2sat, it is reasonable to decrease the Fio2 when oxyhemoglobinsaturation is 100%, provided O2sat can be maintained at 94% or greater
IIa, LOE C-LD


Glucose Control
2015 Recommendation—Updated Class
The benefit of any specific target range of glucose managementis uncertain in adults with ROSC after cardiac arrest
IIb, LOE B-R


Timing of Outcome Prediction
2015 Recommendations—New and Updated Class
The earliest time for prognostication using clinical examination in patients treated with TTM, where sedation or paralysis could be a confounder, may be 72 hours after return to normothermia
IIb, LOE C-EO

Timing of Outcome Prediction
2015 Recommendations—New and Updated Class
Recommend the earliest time to prognosticate a poor neurologic outcome using clinical examination in patients not treated with TTM is 72 hours after cardiac arrest
I, LOE B-NR
This time until prognostication can be even longer than 72 hours after cardiac arrest if the residual effect of sedation or paralysis confounds the clinical examination
IIa, LOE C-LD

Clinical Examination Findings That Predict Outcome
2015 Recommendations—New and Updated Class
In comatose patients who are not treated with TTM, the absence of pupillary reflex to light at 72 hours or more after cardiac arrest is a reasonable exam finding with which to predict poor neurologic outcome
IIa, LOE B-
NR

Clinical Examination Findings That Predict Outcome
2015 Recommendations—New and Updated Class
In comatose patients who are treated with TTM, the absence of pupillary reflex to light at 72 hours or more after cardiac arrest is useful to predict poor neurologic outcome
I, LOE B-NR

Clinical Examination Findings That Predict Outcome
2015 Recommendations—New and Updated Class
Recommend that, given their unacceptable FPRs, the findings of either absent motor movements or extensor posturing should not be used alone for predicting a poor neurologic outcome
III: Harm, LOE B-NR
The motor examination may be a reasonable means to identify the population who need further prognostic testing to predict poor outcome
IIb, LOE B-NR

Clinical Examination Findings That Predict Outcome
2015 Recommendations—New and Updated Class
Recommend that the presence of myoclonus, which is distinct from status myoclonus, should not be used to predict poor neurologic outcomes because of the high FPR
Class III,Harm, LOE B-
NR

Clinical Examination Findings That Predict Outcome
2015 Recommendations—New and Updated Class
In combination with other diagnostic tests at 72 or more hours after cardiac arrest, the presence of status myoclonus during the first 72 to 120 hours after cardiac arrest is a reasonable finding to help predict poor neurologic outcomes
IIa, LOE B-NR

EEG Findings to Predict Outcome
2015 Recommendations—Updated Class
In comatose post–cardiac arrest patients who are treated with TTM, it may be reasonable to consider persistent absence of EEG reactivity to external stimuli at 72 hours after cardiac arrest, and persistent burst suppression on EEG after rewarming, to predict a poor outcome
IIb, LOE B-NR

EEG Findings to Predict Outcome
2015 Recommendations—Updated Class
Intractable and persistent (>72 hours) status epilepticus in the absence of EEG reactivity to external stimuli may be reasonable to predict poor outcome
IIb, LOEB-NR

EEG Findings to Predict Outcome
2015 Recommendations—Updated Class
In comatose post–cardiac arrest patients who are not treated with TTM, it may be reasonable to consider the presenceof burst suppression on EEG at 72 hours or more after cardiac arrest, in combination with other predictors, to predict a poor neurologic outcome
IIb, LOE B-NR

Evoked Potentials to Predict Outcome
2015 Recommendations—Updated Class
In patients who are comatose after resuscitation from cardiac arrest regardless of treatment with TTM, it is reasonable toconsider bilateral absence of the N20 SSEP wave 24 to 72 hours after cardiac arrest or after rewarming a predictor of poor outcome
IIa, LOEB-NR

Imaging Tests to Predict Outcome
2015 Recommendations—New Class
In patients who are comatose after resuscitation from cardiac arrest and not treated with TTM, it may be reasonable to use the presence of a marked reduction of the GWR on brain CT obtained within 2 hours after cardiac arrest to predict pooroutcome
IIb, LOE B-NR

Imaging Tests to Predict Outcome
2015 Recommendations—New Class
It may be reasonable to consider extensive restriction of diffusion on brain MRI at 2 to 6 days after cardiac arrest in combination with other established predictors to predict a poor neurologic outcome
IIb, LOE B-NR

Blood Markers to Predict Outcome
2015 Recommendations—Updated Class
Given the possibility of high FPRs, blood levels of NSE and S-100B should not be used alone to predict a poor neurologicoutcome
III: Harm, LOE C-LD

Blood Markers to Predict Outcome
2015 Recommendations—Updated Class
When performed with other prognostic tests at 72 hours or more after cardiac arrest, it may be reasonable to consider high serum values of NSE at 48 to 72 hours after cardiac arrest to support the prognosis of a poor neurologic outcome
IIb, LOE B-NR
Especially if repeated sampling reveals persistently high values
IIb, LOE C-LD


Organ Donation
2015 Recommendations—Updated and New Class
We recommend that all patients who are resuscitated from cardiac arrest but who subsequently progress to death or brain death be evaluated for organ donation
I, LOEB-NR