ACLS: 2015 Update - Amazon S3 · ACLS: 2015 Update Anything New? Mitchell Shulman MDCM FRCPC CSPQ...
Transcript of ACLS: 2015 Update - Amazon S3 · ACLS: 2015 Update Anything New? Mitchell Shulman MDCM FRCPC CSPQ...

ACLS:
2015 Update
Anything New?
Mitchell Shulman MDCM FRCPC CSPQEmergency Department, MUHCMaster Instructor ACLS, QHSFAssist Professor, Dept of Surgery

Copyright © 2017 by Sea Courses
Inc.
All rights reserved. No part of this document may be reproduced, copied, stored, or transmitted in any form or by any means – graphic, electronic, or mechanical,
including photocopying, recording, or information storage and retrieval systems without prior written
permission of Sea Courses Inc. except where permitted by law.
Sea Courses is not responsible for any speaker or participant’s statements, materials, acts or omissions.

CME Faculty
Disclosure
Dr. Shulman has no affiliation with the manufacturer of any commercial product or provider of any commercial service discussed in this CME activity.

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Key Points
Cardiac Arrests Happen
Be prepared (yourself and your staff)
AED?
Pt’s families / partners: know what to do?

Warning! Problems with the Data
Research in ACLS is difficult / challenging
Few good studies (even less RCT)
Consent ???
Animal vs Human Rural vs Urban ….

2015 Guidelines Update
ILCOR prioritized reviews (166)
Grading of Recommendations, Assessment, Development and Evaluation (GRADE)
Systemic Evidence Evaluation and Review System (SEERS)
Public disclosure
Public comment
Update only
Future changes will be similar
www.ilcor.org/seers

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Call 911 First vs
Call Fast: JUST CALL!
If no phone/reception/bystander:
Call first :sudden collapse victims of all ages(to get an AED there ASAP!)
Call fast :unresponsive pt (any age) where asphyxia is likely (e.g. submersion / near-drowning; overdose; lightning)
if in doubt, unwitnessed, or suspect > 4 min:
deliver about 2 min (5 cycles) of CPR before leaving the victim to call for an AED

Dispatchers / BCLS
Train them to recognize acute coronary syndromes (ACS)
Advise patients with ACS (w/o hx of ASA allergy / GI bleed)
chew 160 – 325 mg aspirinwhile waiting

Responsive?
If not:
Lay people:
Compression only CPR
Trained BCLS providers:C – A - B
Dispatchers / BCLS

Pulse check?
Long time to assess
Error rate (lay rescuer): 35%- detect a “pulse” 10% of cardiac arrests
- provide chest compressions 40% not in
cardiac arrest
Instead assess for signs of life(movement, breathing, coughing)
Trained provider: pulse check < 10 seconds

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Mouth to mouth???
CPR world wide > 30 yrsno HIV or other blood
borne pathogens via mouth-to-mouth
no documented cases of saliva transmitting:HIV, Hep B / C during CPR
few cases of HIV transmission:
“sharps” injury; blood exposure to
non-intact skin

Mouth to mouth??
15 cases of documented disease transmission (direct mouth to mouth)
Mycobacterium tuberculosis
Neisseria meningitidisShigella sonneiSalmonella infantisNeisseria gonorrhea Streptococcus: saliva to non-intact skin
Herpes simplex

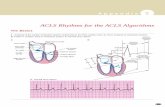
Chest compressions
Push Hard*, Push Fast*
Recommended rate:
30:2for all rescuers
responding alone to victims of any age(except newborns) before
advanced airway control
2 health care providers child/infant 15:2
*Rate: 100 – 120 / min*Depth: 2 – 2. 4 in
( 5 – 6 cm)

Intubate??
Why?Control airwayReduce risk of aspirationAdminister drugsVentilate without worrying
about timing
AlternativesLaryngeal mask airwayCombitube

Confirm ETT placement
Direct visualization
5 point clinical exam
Exhaled CO2 / esophageal detector device
Endotracheal tube holder
Continuous end-tidal CO2 monitoring

Ventilation
Advanced airway in place:
8 – 10 / min.
2 health care provider rescuersCompressor: 100 - 120 / minVentilator: 8 – 10 / min
Don’t stopDon’t pauseRotate compressor role ~ Q 2 min.

AED (Defibrillation)
AED’s do not require a prescription
Healthcare provider oversight not necessary

Defibrillation
Monophasic vsbiphasic ?
Monophasic: 360J
Biphasic: 120 - 200J
If in doubt: use max power available

Defibrillation
1 Shock
Immediate CPR for 2 minutes (start with chest
compressions)
Do NOT check for rhythm / pulse before restarting CPR

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Vasopressors?
Only
after 1 shock 2 2 minutes of CPRw/o perfusing rhythm

Epinephrine: How much?
Class indeterminate !
optimal physiologic response:
.045 - .20 mg / kgbut HDE no statistical increase in rate of survival to hospital discharge
1 mg IV Q 3 – 5 min

Vasopressin?
No longer part of the algorhythmsArginine vasopressin = antidiuretic hormone
Why?PhysiologyStimulates smooth muscle V1 receptors
(non-adrenergic peripheral vasoconstrictor)
StudiesElevated endogenous levels in survivors of
cardiac arrest
Increased coronary perfusion pressure, vital organ
blood flow, cerebral oxygen delivery (animal models)

Vasopressin??
Why not?No survival
advantage over epinephrine
When?Perhaps severe
acidosis
Dose ?? 40 IU x 1

Lidocaine?
No study has demonstrated clinical efficacy
Use was supported by animal studies and extrapolation
Conflicting data in the literature
Compared unfavorably to Amiodarone

Lidocaine?
Successful in converting V tach to NSRonly 20- 30% (inferior to Procainamide and Amiodarone)
Advantages:ease of dosing / administrationwhen it works it works rapidlyminimal side effectslow cost
Consider 1 – 1.5 mg / kg 1st dose;
then 0.5 – 0.75 mg / kg IV
Max. 3 doses or 3 mg / kg

Amiodarone
History:structural analogue of thyroxinedeveloped in the 1960’s (anti-
anginal coronary vasodilator)
acutely: anti-sympathetic & Ca+
channel blockingchronically: prolongs action potential
duration (Class III)long elimination half-life (14 -59 days)large volume of distribution

Amiodarone
ARREST (Amiodarone for Resuscitation after Out-of-hospital Cardiac Arrest Due to Ventricular Fibrillation)
300 mgs (n= 246) vs placebo (n= 258)44% vs 34% survive to be admittedno difference in survival to hospital discharge
ALIVE (Amiodarone as compared with Lidocaine for Shock-Resistant ventricular Fibrillation)
5 mg/kg Amiodarone (n= 179) vs 1.5 mg/kg Lidocaine (n= 165)
22.8% vs 12% survival to admissionno difference in survival to discharge

Amiodarone
Problem:“attempts to defibrillate should not be
delayed by administration of Amiodarone”
significant time required to reconstitute & prepare (high viscosity, generates bubbles)
300 mg IV X 1; then 150 mg X 1

Anti-arrhythmics
Bottom line:
no anti-arrhythmic agent to date
has been demonstrated in clinical trials of
Vfib / pulseless Vtach to improve survival to hospital discharge !
CPR, CPR, CPRDefibrillate, defibrillate, defibrillate

Anti-arrhythmics
In the setting of tachycardia:all anti-arrhythmics are pro-arrhythmic
Stable, narrow complex, regular:adenosinediltiazem
Stable, narrow complex, irregular:diltiazembeta-blockers
Stable, wide complex:amiodaronemagnesium
Adenosine:6 mgs; 12 mgs
Diltiazem:0.25 mg/kg; 0.35 mg/kg
Metoprolol: 5 mg IV Q 5min. Tot: 15 mg
Amiodarone:150 mg; repeat PRNmax: 2.2 g IV / 24 hrs
Magnesium:1 – 2 grams in 50 - 100 ml D5W over 5 – 60 min IV.

Key Points
Cardiac Arrests Happen
Be prepared (yourself and your staff)
AED?
Pt’s families / partners: know what to do?

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Let’s Put It All Together

Vfib / Vtach
1 shock (biphasic 120 – 200J; monophasic 360J)
Resume CPR at once (5 cycles)
Check rhythm
Shockable?
1 shock Resume CPR (5 cycles)
Epinephrine 1 mg IV / IO (repeat Q 3 – 5 min)
Check rhythm
Shockable?
1 shock Resume CPR
Amiodarone 300 mg IV/IO

Asystole / PEA
CPR 5 cycles
Epinephrine 1 mg IV / IO Q 3 – 5 min.
CPR 5 cycles
Check rhythm
Look for a treatable causeGive EPI FAST!Hypovolemia
HypoxiaHydrogen ionHypo/hyper K+HypoglycemiaHypothermia
ToxinsTamponade (cardiac)Tension (pneumo)Thrombosis (cor / pulm)Trauma

Symptomatic BradycardiaHR < 60 bpm + ………..
Prepare forTranscutaneous pacing
Consider Atropine 0.5 mg IV (total dose 3 mg)
Consider Epinephrine 2 – 10 microg/min
Dopamine 2 – 10 microg / kg / min
+ Acute altered mental status /Ongoing chest pain /Acute heart failure /Hypotension / signs of shock
Oxygen, IV access, Monitor, EKG
Glucagon? Beta –blocker or calcium channel blocker OD3 – 10 mgs over 3 -5 min, then infuse @ 3 mg/h

Agenda
Problems with data
Call 1st? / Dispatch
The Basics: CPR, Intubation, Defibrillation
The Drugs
Putting it all together
Post- Resuscitation

Post resuscitation
Don’t hyperventilate8 – 10 breaths / min
PETCO2 : 35- 40 mm Hg
Cool: 32- 36C for 24 hrs. *
Maintain BP Fluids; Epi / Norepi: 0.1 – 0.5 mcg / min
(70 kg = 7 – 35 mcg / min)
Maintain O2 saturation > 94%
Watch blood sugar
Treat fever
* Green, RS, CJEM 7(1) Jan. 2005 p. 42 – 7.

Key Points
Cardiac Arrests Happen
Be prepared (yourself and your staff)
AED?
Pt’s families / partners: know what to do?

The Most Important Message
“Any improvements resulting from advanced life support therapies are less substantial than the increases in survival rate reported from the successful deployment of lay rescuer CPR and Automated External Defibrillationprograms in the community.”