fluid and electrolytes
Transcript of fluid and electrolytes



Physiologic homeostasis depends on normal Physiologic homeostasis depends on normal fluid and electrolyte balance, and is important in both fluid and electrolyte balance, and is important in both health promotion and treatment of disorders. Fluid health promotion and treatment of disorders. Fluid and electrolyte imbalances commonly accompany and electrolyte imbalances commonly accompany illnesses. Severe imbalances may result to death illnesses. Severe imbalances may result to death Some imbalances affect not only the acutely and Some imbalances affect not only the acutely and chronically ill but also clients with faulty diet or those chronically ill but also clients with faulty diet or those who take selected medication such as diuretics and who take selected medication such as diuretics and glucocorticoids preparation. Every nurse must glucocorticoids preparation. Every nurse must understand the process of fluid and electrolyte understand the process of fluid and electrolyte balance identify client at risk for imbalances, balance identify client at risk for imbalances, recognize early signs and symptoms of imbalances, recognize early signs and symptoms of imbalances, intervene as appropriate and evaluate the outcomes.intervene as appropriate and evaluate the outcomes.

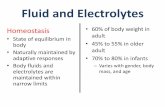
*Body Water*Body WaterPrincipal body fluids ;solvent responsible for the body’s Principal body fluids ;solvent responsible for the body’s structures and function.structures and function.Consists of 45-75% of the total body weight.Consists of 45-75% of the total body weight.

NORMAL WATER NORMAL WATER DISTRIBUTION/BALANCEDISTRIBUTION/BALANCE
Body Fluids FunctionBody Fluids Function Facilitates transport of nutrients, Facilitates transport of nutrients,
hormones, CHON and other hormones, CHON and other molecules into the cells.molecules into the cells.
Aids in the removal of cellular Aids in the removal of cellular metabolic waste products.metabolic waste products.
PProvides the medium in which cellular rovides the medium in which cellular metabolism takes place.metabolism takes place.
Regulates lubrication of musculo-Regulates lubrication of musculo-skeletal joints.skeletal joints.
Acts as a component all body cavities Acts as a component all body cavities ( pericardial fluid, pleural, CSF)( pericardial fluid, pleural, CSF)


Fluid CompartmentsFluid Compartments::
1. Intracellular Fluid (ICF)1. Intracellular Fluid (ICF)– Includes all water Includes all water
and electrolytes and electrolytes inside the cells.inside the cells.
– 2/3 of the body 2/3 of the body weight is contained weight is contained within cell within cell membranesmembranes

2. Extra cellular Fluid (ECF)2. Extra cellular Fluid (ECF)– Includes interstitial fluid, Includes interstitial fluid,
intravascular and intravascular and
Trancellular fluidTrancellular fluid– Constitutes about 1/3 of Constitutes about 1/3 of
body waterbody water
Functions of ECF:Functions of ECF:– Transports nutrients and Transports nutrients and
electrolytes to cell and waste electrolytes to cell and waste products for excretionproducts for excretion
– Regulates heatRegulates heat– Lubricates and cushions Lubricates and cushions
jointsjoints– Hydrolyzes food for digestive Hydrolyzes food for digestive
processprocess

NORMAL WATER BALANCENORMAL WATER BALANCE
Intake
Output
LiquidWater in foodMetabolism
1,200-1,500 ml700- 1,000 ml200- 400 ml
UrineFecesInsensible Loses: Skin Lungs
1,200 -1,500 ml100-250 ml
350 -400 ml350- 400 ml
TOTAL 2,100 – 2,900 ml
TOTAL 2,100 – 2,900 ml

Fluid Intake & OutputFluid Intake & Output

Routes of Gains and LossesRoutes of Gains and Losses

CONTINUAL MOVEMENT OF FLUIDS CONTINUAL MOVEMENT OF FLUIDS AND ELECTROLYTES AND ELECTROLYTES
Fluids move between Fluids move between components to maintain components to maintain homeostasis homeostasis
Fluid Movement from Pressure Fluid Movement from Pressure Changes-body fluid shifts Changes-body fluid shifts between the interstitial space between the interstitial space and the vascular space in the and the vascular space in the capillary as a result of capillary as a result of differences in the hydrostatic differences in the hydrostatic pressure and oncotic pressurepressure and oncotic pressure

Fluid Movement by Diffusion and OsmosisFluid Movement by Diffusion and Osmosis
Diffusion- means by which substances such as Diffusion- means by which substances such as nutrients and wastes produces move between blood nutrients and wastes produces move between blood and interstitial spaces.and interstitial spaces.

Osmolality – refers to the concentration of Osmolality – refers to the concentration of solutes in 1 liter of solutionsolutes in 1 liter of solution
OSMOSIS: diffusion of H2O across a selectively OSMOSIS: diffusion of H2O across a selectively permeable membrane from an area of lower solute permeable membrane from an area of lower solute concentration to an area of higher solute concentration to an area of higher solute concentration.concentration.

FACTORS RESPONSIBLE FOR NORMAL FACTORS RESPONSIBLE FOR NORMAL REGULATION AND FLUID BALANCEREGULATION AND FLUID BALANCE
Regulator of fluids Balance:Regulator of fluids Balance:
ThirstThirst– Hypothalamus- thirst Hypothalamus- thirst
center of the braincenter of the brain– Activated by an increase Activated by an increase
in ECF Osmolality due to:in ECF Osmolality due to:
HypotensionHypotension PolyuriaPolyuria Fluid volume depletionFluid volume depletion

Hormones/ Hormonal Influence Antidiuretic Hormone (ADH)-
stored in the posterior pituitary gland; reduces urinary output; returns fluids to the body rather than excreting them
Aldosterone - secreted by the adrenal cortex and conserves the body’s sodium by promoting potassium excretion from the kidneys.
Lymphatic system – It plays an important role in returning excess fluid and protein from interstitial spaces to the blood.

RENIN-ANGIOTENSIN MECHANISM ATRIAL NATRIURETIC PEPTIDE
Nervous System - when the ECF volume increases, mechanoreceptors in the wall of the atrium respond to atrial distention by increasing cardiac stroke volume and triggering a sympathetic response in the kidney, stimulation of the of the renal sympathetic nerves decreases renal excretion of sodium by both increasing renin release and through a direct effect in the kidneys.

KidneyKidney – maintain fluid volume and the connection – maintain fluid volume and the connection of urine by filtrating the ECF through the glomeruli. of urine by filtrating the ECF through the glomeruli. Reabsorbtion and excretion of ECF occurs in the Reabsorbtion and excretion of ECF occurs in the renal tubules.renal tubules.

Fxns of the KidneysFxns of the KidneysRegulation of ECF volume and Regulation of ECF volume and
osmolality by selective retention of osmolality by selective retention of needes substances and excretion fluids.needes substances and excretion fluids.
Regulation of electrolytes level in the Regulation of electrolytes level in the ECF by selective retention of substances ECF by selective retention of substances and excretion of unneeded substancesand excretion of unneeded substances
Regulation of pH of the ECF by retention Regulation of pH of the ECF by retention of H+ ionsof H+ ions

REGULATION OF FLUID VOLUME
HYPERVOLEMIA HYPOVOLEMIA
stimulatesinhibits
ADH
INCREASEDURINATION
ofDilute urine
NORMAL FLUID VOLUME RESTORED
DECREASEDURINATION
ofConcentrated urine
Aldosterone Thirst Thirst ADH Aldosterone

FLUID IMBALANCESFLUID IMBALANCESI. Extra Cellular Fluid Volume DeficitI. Extra Cellular Fluid Volume Deficit
Causes:Causes:
1. Lack of fluid intake1. Lack of fluid intake– 1,500 – 2,000 ml 1,500 – 2,000 ml
RF:RF:– Hospitalized/bed boundHospitalized/bed bound– People w/ dysphagia/ risk for aspirationPeople w/ dysphagia/ risk for aspiration– Tube-fed patients who are not given adequate free waterTube-fed patients who are not given adequate free water– Pts. w/ decreased access to fluidsPts. w/ decreased access to fluids– Pts. w/ impaired thirst mechanismPts. w/ impaired thirst mechanism
People w/ debilitating illnessesPeople w/ debilitating illnesses Older adultsOlder adults
MILD: 1-2 L of H2O (2% body wt.)
MODERATE: 3-5 L of H2O (5%)
SEVERE: 5-10 L of H2O (8%)

2. Excessive Fluid Losses2. Excessive Fluid Losses
– Vomiting, diarrhea, fever, hyperglycemia, suction, Vomiting, diarrhea, fever, hyperglycemia, suction, fistula, burns, blood loss, diabetes insipidus, fistula, burns, blood loss, diabetes insipidus, diaphoresis, hyperthyroidism, excessive diuretics, diaphoresis, hyperthyroidism, excessive diuretics, ileostomy, hyperventilation, Diuretic phase of ARFileostomy, hyperventilation, Diuretic phase of ARF
Types of ECFVDTypes of ECFVD Hyperosmolar (hypertonic): water loss is > electrolyte lossHyperosmolar (hypertonic): water loss is > electrolyte loss Hypotonic: electrolyte loss is > fluid lossHypotonic: electrolyte loss is > fluid loss Isotonic (iso-osmolar): water and electrolyte loss are equalIsotonic (iso-osmolar): water and electrolyte loss are equal

CLINICAL MANIFESTATIONS:CLINICAL MANIFESTATIONS:
1. Loss of body wt.1. Loss of body wt.– Most accurate indicator of fluid lossMost accurate indicator of fluid loss– 1 L of sol’n=1 kg of body wt.1 L of sol’n=1 kg of body wt.
2. Changes in I &O2. Changes in I &O– U. O. of 400-500 ml/day- oliguriaU. O. of 400-500 ml/day- oliguria– ThirstThirst
3. Changes in V/S3. Changes in V/S– ↓↓ed BP ed BP – Weak pulseWeak pulse– ↓↓ed CVP, ↓ed PCWPed CVP, ↓ed PCWP– Postural hypotension Postural hypotension – ↑↑ed PR ed PR – Flat JV and prolonged peripheral venous filling time of more than 5 sec.Flat JV and prolonged peripheral venous filling time of more than 5 sec.– Elev. Body tempElev. Body temp
4. M4. Manifestations of cellular dehydrationanifestations of cellular dehydration– dry mucus membrane of mouth and eyesdry mucus membrane of mouth and eyes– cracked lipscracked lips– poor skin turgor poor skin turgor – muscle weakness muscle weakness – cerebral sx (fluid shifting)cerebral sx (fluid shifting)

FLUID VOLUME DEFICIT
•IS move to IV•ADH & aldosterone is released
•Fluids reabsorbed in the ileum & colon•Baroreceptors SNS: increase HR &
Peripheral vasoconstriction•Osmoreceptors: Thirst mechanism
DEHYDRATION
•Impaired temperature regulation•Decrease ability to transport heat
•Decrease CSF•Decrease Sodium

II. Intracellular Fluid Volume Deficit (ICFVD)II. Intracellular Fluid Volume Deficit (ICFVD)– Due to severe dehydrationDue to severe dehydration
RF:RF:
- older clients; w/ acute water loss- older clients; w/ acute water loss
s/sx:s/sx: - ThirstThirst– OliguriaOliguria– FeverFever– Confusion, coma, cerebral hemorrhageConfusion, coma, cerebral hemorrhage
DIAGNOSTIC TEST FOR ECFVD/ICFVD:DIAGNOSTIC TEST FOR ECFVD/ICFVD:Osmolality > 295 mOsm/LOsmolality > 295 mOsm/L Na >145 mEq/lNa >145 mEq/l
BUN > 25 mg/dlBUN > 25 mg/dl Glucose >120 mg/dlGlucose >120 mg/dl
Hct > 55%Hct > 55% Urine sp. Gr. > 1.030Urine sp. Gr. > 1.030

III. Extra Cellular Fluid III. Extra Cellular Fluid Volume ExcessVolume Excess
(ECFVE)(ECFVE)
Fluid overloadFluid overload
2 types:2 types:
1. hypervolemia-↑ed fluids in 1. hypervolemia-↑ed fluids in vascular systemvascular system
2. third spacing-↑ed fluids in 2. third spacing-↑ed fluids in interstitial spaceinterstitial space

EtiologyEtiologySimple overloading of fluids (too many Simple overloading of fluids (too many
IVF)IVF)↑ ↑ ADH and aldosteroneADH and aldosterone↓ ↓ kidney fxnkidney fxnCHFCHFLiver CirrhosisLiver CirrhosisVenous disorderVenous disorderExcessive ingestion of fluids/ food with Excessive ingestion of fluids/ food with
NaNa

MECHANISM OF EDEMA FORMATION
FLUID OVERLOAD
Increased peripheralVascular resistance
Increased leftVentricular pressure
Increased left atrialpressure
Fluid movementinto tissues
Increase hydrostaticpressure in arterial end
of capillary
edema
Pulmonary edema

ALTERED LYMPHATICFUNCTION
TISSUE INJURYDECREASE PLASMA & ALBUMIN
Decrease productionof plasma CHON
Decrease CapillaryOncotic Pressure
Decrease ReabsorptionAt venous end
EDEMA
Lymphatic obstructiondecreases absorption
of interstitial fluid
Decrease transportof capillary filtered
protein
Increase tissue oncoticpressure, which pulls
fluid towards it
EDEMA
Increase capillarypermeability
Movement of plasmaCHON in tissues
Increase tissue Oncotic pressure
EDEMA

IMPAIRED RENAL FXN
↓ Na and H20 excretion
↑ Fluid Volume
Heart compensates by increasing HR and Hypertrophy
If compensatory mechanism fails, heart failure develops

Clinical Manifestations:Clinical Manifestations:
> respiratory > respiratory
> cardiovascular > cardiovascular
> others> others
EdemaEdema
Anorexia/bloatingAnorexia/bloating
Wt. gainWt. gain
Fluid shifting from IV/IS Fluid shifting from IV/IS
DIAGNOSTICS:DIAGNOSTICS:Osmolality < 275 mOsm/LOsmolality < 275 mOsm/L Na < 135 mEq/lNa < 135 mEq/l
BUN < 8 mg/dlBUN < 8 mg/dl Urine sp. Gr. < 1.010 Urine sp. Gr. < 1.010 Hct < 45%Hct < 45%

IV. Intracellular Fluid Vol. excess (ICFVE)IV. Intracellular Fluid Vol. excess (ICFVE)- water intoxication; - water intoxication; cells are resistant to fluid shiftscells are resistant to fluid shifts
Etiology:Etiology:– water excess- number of solutes is normal but there water excess- number of solutes is normal but there
is water excessis water excess– solute deficiency=amt. of water is normal but ↓ed solute deficiency=amt. of water is normal but ↓ed
solutesolute
= most common cause: administration of excessive amts. Of = most common cause: administration of excessive amts. Of hypoosmolar IVFhypoosmolar IVF
= a= adults who dults who
consume excessive amts. of tap H2O consume excessive amts. of tap H2O
w/o adequate nutrient intakew/o adequate nutrient intake
=SIADH=SIADH
=people w/ psych. d/o → schizophrenia =people w/ psych. d/o → schizophrenia
with compulsive water consumptionwith compulsive water consumption

V.V. Extracellular Fluid Volume Shifting – third spacingExtracellular Fluid Volume Shifting – third spacing
2 types:2 types:
1. vascular fluid shifts to interstitial space (hypovolemia)1. vascular fluid shifts to interstitial space (hypovolemia)
2. interstitial fluid shifts to vascular space (hypervolemia)2. interstitial fluid shifts to vascular space (hypervolemia)
* third space= fluid that shifts into IS and remains there* third space= fluid that shifts into IS and remains there = common sites:pleural cavity, peritoneal cavity, & = common sites:pleural cavity, peritoneal cavity, & pericardial sacpericardial sac
Etiology:Etiology:
↑ ↑ ed capillary permeability ed capillary permeability ↑ ↑ ed fluid reabsorption in venous end ed fluid reabsorption in venous end Decreased serum CHON levelsDecreased serum CHON levels Obstruction of venous end of capillaryObstruction of venous end of capillary Non-functional lymphatic drainage systemNon-functional lymphatic drainage system

Clinical Manifestations:Clinical Manifestations:
1. 1. Fluid shifting from IV to ISFluid shifting from IV to IS– Pallor, cold limbs, weak &rapid pulse, Pallor, cold limbs, weak &rapid pulse,
hypotension, oliguria, ↑ ed skin turgor & ↓ ed level hypotension, oliguria, ↑ ed skin turgor & ↓ ed level of consciousnessof consciousness
– No changes in body wt. because fluid has not No changes in body wt. because fluid has not been lost but redistributedbeen lost but redistributed
2.2.fluid returns to the IV space from IS – s/sx similar to fluid returns to the IV space from IS – s/sx similar to fluid overloadfluid overload– bounding pulse, crackles, JVD, ↑ ed BPbounding pulse, crackles, JVD, ↑ ed BP

Types of Intravenous FluidsTypes of Intravenous FluidsTypes of Intravenous Fluids:Types of Intravenous Fluids:
ISOTONICISOTONIC – a solution that has the same osmotic pressure – a solution that has the same osmotic pressure
externally as that found across a semi-permeable membraneexternally as that found across a semi-permeable membrane
--0.9% NaCl, D5W, 5% Dextrose in 0.225% Saline and LRS--0.9% NaCl, D5W, 5% Dextrose in 0.225% Saline and LRS
HYPOTONICHYPOTONIC –a solution that has a lower osmotic press than –a solution that has a lower osmotic press than
that of the blood causing the cell to expand and swell.(They that of the blood causing the cell to expand and swell.(They contain lower concentration of salt/ solute than other solution)contain lower concentration of salt/ solute than other solution)
--0.3 % NaCl, D in water, 0.45 % NaCl and distilled water.--0.3 % NaCl, D in water, 0.45 % NaCl and distilled water.
HYPERTONIC HYPERTONIC – a solution that has a higher osmotic pressure – a solution that has a higher osmotic pressure
than that of the blood causing the cell to shrink. ( It has higher than that of the blood causing the cell to shrink. ( It has higher concentration of solutes.)concentration of solutes.)
--D5LRS, Mannitol, 10% D in water, and 5% D in 0.45% NaCl--D5LRS, Mannitol, 10% D in water, and 5% D in 0.45% NaCl


Cell appearance on different solutions
Blood cells in an Hypotonic Fluid
Blood cells in an Hypertonic Fluid


ElectrolytesElectrolytes – these are chemical substances which – these are chemical substances which
when dissolved dissociates into ions and passeswhen dissolved dissociates into ions and passes
electrical potential.electrical potential.
Types:Types: Cations – ions carrying positive charge Cations – ions carrying positive charge
– NaNa– KK– CaCa– MgMg
Anions – ions carrying negative Anions – ions carrying negative

CATIONS ANIONS
Na- 135-145 m Eq/L
K- 3.5 – 5.0 m Eq/L
Ca- 4.5-5.5 mEq/L
Mg -1.5 – 2.5 mEq/L
HCO3- 22-26 mEq/L
Cl- 96-106 mEq/L
PO4 – 1.2 -3.0 mEq/L


A. Sodium ImbalancesA. Sodium Imbalances Derminant of serum osmolalityDerminant of serum osmolality Chloride is the anion that usually accompanies Chloride is the anion that usually accompanies
NaNa Sodium balance is regulated by the interaction Sodium balance is regulated by the interaction
among neural, hormonal, and vascular among neural, hormonal, and vascular mechanismsmechanisms
Renal glomerulus filters 1000 mEq of sodium/hr Renal glomerulus filters 1000 mEq of sodium/hr and 99% is reabsorbed in the loop of Henleand 99% is reabsorbed in the loop of Henle
ProstaglandinProstaglandin

FUNCTIONSFUNCTIONS
Primary regulator of ECF volumePrimary regulator of ECF volumeEstablishing electrochemical state Establishing electrochemical state
necessary for muscle contraction and necessary for muscle contraction and nerve impulse transmissionnerve impulse transmission
““WHERE SODIUM GOES WATER WHERE SODIUM GOES WATER FOLLOWS”FOLLOWS”

1. 1. HyponatremiaHyponatremia –one of the most common electrolyte imbalance–one of the most common electrolyte imbalance
Hypovolemic: Na loss > H2O lossHypovolemic: Na loss > H2O loss
Euvolemic: TBW is mod. increased & total body Na is normalEuvolemic: TBW is mod. increased & total body Na is normal
Hypervolemic: Greater increased in TBW than in total NaHypervolemic: Greater increased in TBW than in total Na
Redistributive: no change in TBW or total body Na.Redistributive: no change in TBW or total body Na.
RF:RF: Excessive perspirationExcessive perspiration Altered thirst mech.Altered thirst mech. w/o access to fluids w/o access to fluids rapid rehydration after excessive fluid lossrapid rehydration after excessive fluid loss altered percentage of total body wateraltered percentage of total body water decreased intake of sodium: decreased intake of sodium: fruits, vegetables, oatmeal, rice, wheat, fresh fruits, vegetables, oatmeal, rice, wheat, fresh
meat, chicken, fish (1 oz)meat, chicken, fish (1 oz)
excessive administration of diuretic and laxativesexcessive administration of diuretic and laxatives NGT irrigation with plain waterNGT irrigation with plain water Vomiting, drhVomiting, drh

Clinical Manifestations: 125 mEq/LClinical Manifestations: 125 mEq/L neurological manifestationsneurological manifestations Cardiovascular manifestations Cardiovascular manifestations
– Tachycardia- Tachycardia- – Sympathetic responses – stimulation of Sympathetic responses – stimulation of
chemoreceptors in the aortic and carotid bodieschemoreceptors in the aortic and carotid bodies Respiratory ManifestationsRespiratory Manifestations
– Crackles in the lungsCrackles in the lungs– Tachypnea, dypnea, orthopnea, SOBTachypnea, dypnea, orthopnea, SOB
GI ManifestationsGI Manifestations– n/v, drh, abdominal cramping, hyperactive bowel n/v, drh, abdominal cramping, hyperactive bowel
soundssounds Others:Others:
– Dry skin, tongue & mucus membrane Dry skin, tongue & mucus membrane

DX results:DX results:
Na < 135 mEq/LNa < 135 mEq/LCl < 96 mEq/LCl < 96 mEq/LSerum Osmolality <275 mOsm/kgSerum Osmolality <275 mOsm/kgUrine Osmolality <40 mOsm/kgUrine Osmolality <40 mOsm/kg

2.2. Hypernatremia Hypernatremia - - associated w/ water loss or sodium associated w/ water loss or sodium gaingain
Types:Types:– Hypovolemic hypernatremia: TBW is greatly Hypovolemic hypernatremia: TBW is greatly
decreased compared to Nadecreased compared to Na
– Euvolemic hypernatremia: TBW is decrease Euvolemic hypernatremia: TBW is decrease relative to normal total body Narelative to normal total body Na
– Hypervolemic hypernatremia: TBW is increased Hypervolemic hypernatremia: TBW is increased but Na gain is > H2O gainbut Na gain is > H2O gain

Etiology/RF:Etiology/RF: Inadequate water intake in conjunction w/ decreased thirst Inadequate water intake in conjunction w/ decreased thirst
(hypodipsia)(hypodipsia) Lack of access to drinkable waterLack of access to drinkable water Physical or chemical restraintPhysical or chemical restraint Mental confusionMental confusion NPONPO Excessive water loss & insufficient water replacement Excessive water loss & insufficient water replacement Increased Na+ intake: Increased Na+ intake: bread, cereals, chips, convenience food, fast foodsbread, cereals, chips, convenience food, fast foods
IV administration of hypertonic saline or hypertonic tube IV administration of hypertonic saline or hypertonic tube feedingsfeedings
Retention of Na+ occurs in heart, renal or liver dse.Retention of Na+ occurs in heart, renal or liver dse. Cushing’s SyndromeCushing’s Syndrome HyperaldosteronismHyperaldosteronism Uncontrolled DM Uncontrolled DM

Clinical Manifestations: 155 mEq/LClinical Manifestations: 155 mEq/L
PolyuriaPolyuria Anorexia, N/V, weakness, restlessnessAnorexia, N/V, weakness, restlessness Early neurologic S/SxEarly neurologic S/Sx Hypervolemic stateHypervolemic state Hypovolemic state Hypovolemic state DysrhythmiaDysrhythmia Crackles, dysnea, pleural effusionCrackles, dysnea, pleural effusion Fever and increased thirstFever and increased thirst Dry skin and mucous membrane, tongue furrowsDry skin and mucous membrane, tongue furrows

Effect of Sodium to cellsEffect of Sodium to cells

B. Potassium ImbalancesB. Potassium Imbalances PISOPISO Poorly stored in the body, daily K+ intake is necessary Poorly stored in the body, daily K+ intake is necessary 80 to 90% of K+ is excreted through the kidneys & 80 to 90% of K+ is excreted through the kidneys &
remainder is excreted in fecesremainder is excreted in feces
Functions:Functions: Regulates ICF osmolalityRegulates ICF osmolality Promotes transmission and conduction of nerve impulses Promotes transmission and conduction of nerve impulses Muscle contractionMuscle contraction Enzyme action for cellular metabolism and glycogen Enzyme action for cellular metabolism and glycogen
storage in the liverstorage in the liver acid-base balanceacid-base balance

AlkalosisAlkalosis– can cause hypokalemiacan cause hypokalemia
AcidosisAcidosis– can cause hyperkalemiacan cause hyperkalemia
Substance that can alter K+ levels:Substance that can alter K+ levels:– InsulinInsulin– Glucagon Glucagon – Adrenocortical hormonesAdrenocortical hormones
cortisol and aldosteronecortisol and aldosterone StressStress
– Catecholamines & beta- adrenergic agonistsCatecholamines & beta- adrenergic agonists– Alpha-adrenergic agonistsAlpha-adrenergic agonists– EpinephrineEpinephrine– has alpha & beta – adrenergic propertieshas alpha & beta – adrenergic properties

1. Hypokalemia1. Hypokalemia- common, especially in elderly pop’n- common, especially in elderly pop’n
Etiology and RF:Etiology and RF:
A. Inadequate K+ intake body does not conserve K+A. Inadequate K+ intake body does not conserve K+– Debilitated, confused, restrained, lacking access to K+ Debilitated, confused, restrained, lacking access to K+
sources, malnourished, anorexic, bulimicsources, malnourished, anorexic, bulimic– Potassium- restricted diets or some wt. reduction dietsPotassium- restricted diets or some wt. reduction diets
( corn, potato, apple, blueberry, cranberry, coffee, cola, ( corn, potato, apple, blueberry, cranberry, coffee, cola, gingerale, soda)gingerale, soda)
– Those receiving K+ free IV sol’nsThose receiving K+ free IV sol’ns

B. K+ excretion exceeds K+ intakeB. K+ excretion exceeds K+ intake– Vomiting, drh, suctioning, intestinal fistulae, Vomiting, drh, suctioning, intestinal fistulae,
ileostomyileostomy– Osmotic diuresis that occurs with DKAOsmotic diuresis that occurs with DKA– Surgical clientsSurgical clients– Alcoholic clientsAlcoholic clients– Certain drugs (loop, osmotic, thiazide diuretics, Certain drugs (loop, osmotic, thiazide diuretics,
cathartics, steroids)cathartics, steroids)– Clients who are in the healing phase after a Clients who are in the healing phase after a
severe tissue injury or burnsevere tissue injury or burn– Cushing’s syndromeCushing’s syndrome– Diuretic Phase of RFDiuretic Phase of RF– HyperaldosteronismHyperaldosteronism

↓ serum K
↓ K gradient
↑ resting membrane potential
↓ neuromuscular irritability and excitability

Clinical Manifestations:Clinical Manifestations: GI ManifestationsGI Manifestations
– Slowed smooth muscle contraction Slowed smooth muscle contraction – Anorexia, abdominal distention, constipationAnorexia, abdominal distention, constipation– Extreme smooth muscle slowing - vomiting ileus, urinary retentionExtreme smooth muscle slowing - vomiting ileus, urinary retention
Slowed Skeletal Muscle Contraction- muscle weakness, Leg cramps, Slowed Skeletal Muscle Contraction- muscle weakness, Leg cramps, fatigue, paresthesia, hyporeflexia, paralysisfatigue, paresthesia, hyporeflexia, paralysis
ECG-most reliable tool for identifying abnormalities in intracellular K+ ECG-most reliable tool for identifying abnormalities in intracellular K+ level (peaked P wave, ST depressed & prolonged, level (peaked P wave, ST depressed & prolonged, Depressed or Depressed or inverted T wave, prominent U wave).inverted T wave, prominent U wave).
↓ ↓ ed myocardial contractilityed myocardial contractility Pulmonary manifestations Pulmonary manifestations Progressive neurologic consequences of altered conduction – Progressive neurologic consequences of altered conduction –
dysphasia, confusion, depression, convulsions, areflexia, comadysphasia, confusion, depression, convulsions, areflexia, coma Polyuria, nocturiaPolyuria, nocturia

2. Hyperkalemia2. Hyperkalemia
Etiology and RF:Etiology and RF: Retention of K+ by the body because of ↓ ed or Retention of K+ by the body because of ↓ ed or
inadequate urine outputinadequate urine output Release of K+ from the cells during the 1Release of K+ from the cells during the 1stst 24 to 72 hours 24 to 72 hours
after traumatic injury on burns, or from cell lysis or after traumatic injury on burns, or from cell lysis or acidosisacidosis
Excessive infusion of IV solution that has K+ or excessive Excessive infusion of IV solution that has K+ or excessive oral intake of K+, especially in a person who has renal oral intake of K+, especially in a person who has renal dsedse
Therapy w/ K+ sparing diuretics, use of K+ supplements, Therapy w/ K+ sparing diuretics, use of K+ supplements, ACE inhibitors ACE inhibitors
Adrenal insufficiency or addison’s diseaseAdrenal insufficiency or addison’s disease

↑ serum K
Altered resting membrane potential
Cell membrane becomes easily excitable
Increased depolarization or action potential
Repeated irritation of cell membrane
↑ Excitation threshold of membrane
Cells become less excitable
Weak, flaccid paralysis of muscles

Clinical Manifestations:Clinical Manifestations:
N/VN/V DiarrheaDiarrhea Impaired nerve & muscle functionImpaired nerve & muscle function Severe neuromuscular weakness Severe neuromuscular weakness respiratory muscle paralysisrespiratory muscle paralysis ECG changes: (wide flat P wave, Depressed ST ECG changes: (wide flat P wave, Depressed ST
segment, segment, Narrow, peaked T wave)Narrow, peaked T wave) Impaired cardiac conduction (tachycardia, Impaired cardiac conduction (tachycardia,
hypotension, cardiac arrest, ventricular contractions)hypotension, cardiac arrest, ventricular contractions)

Effect of Potassium on ECGEffect of Potassium on ECG

C. Calcium Imbalances:C. Calcium Imbalances:FUNCTIONS:FUNCTIONS:
catalyst (nerve impulses)catalyst (nerve impulses) stimulates muscle contractionstimulates muscle contraction normal cellular permeabilitynormal cellular permeability blood coagulationblood coagulation absorption of Vitamin B12absorption of Vitamin B12 Bones and teethBones and teeth 99% of the body’s Ca# is in the bones & teeth99% of the body’s Ca# is in the bones & teeth 1 % is in the tses. And IV space1 % is in the tses. And IV space

3 types:3 types:
1. free/ ionized1. free/ ionized
2. Ca# bound to CHON2. Ca# bound to CHON
3. Complex3. Complex
Vit. DVit. D - is needed to absorb Ca# from GIT - is needed to absorb Ca# from GIT
PTHPTH– regulates plasma levels of Ca# and PO4 by ↑ ing resorption regulates plasma levels of Ca# and PO4 by ↑ ing resorption
from bone and reabsorption from renal tubule or the GITfrom bone and reabsorption from renal tubule or the GIT
CalcitoninCalcitonin– thyroid glandthyroid gland– opposes action of PTHopposes action of PTH– inhibits bone resorptioninhibits bone resorption

1. Hypocalcemia1. HypocalcemiaEtiology and RF:Etiology and RF: common in adult because of inadequate intake of Ca# and common in adult because of inadequate intake of Ca# and
Vit. D (GI dses – anorexia, liver dse., lactose intolerance, Vit. D (GI dses – anorexia, liver dse., lactose intolerance, alcoholism): oatmeal, hamburger, apples, bananas, alcoholism): oatmeal, hamburger, apples, bananas, chickenchicken
decreased intake for several days (NPO), high CHON dietdecreased intake for several days (NPO), high CHON diet hypoparathyroidism hypoparathyroidism people who don’t have exposure to the sunpeople who don’t have exposure to the sun pancreatitispancreatitis Open woundsOpen wounds Excess NaExcess Na

Overcorrection of AcidosisOvercorrection of Acidosis Multiple BTMultiple BT Certain drugsCertain drugs
– MgSO4, Colchicine, and neomycinMgSO4, Colchicine, and neomycin– Aspirin, anticonvulsants, and estrogenAspirin, anticonvulsants, and estrogen– PO4prep’n PO4prep’n – Steroids Steroids – Loop diureticLoop diuretic– Antacids and laxatives Antacids and laxatives

Partial depolarization of nerves and muscles because of ↓ threshold potential
↓ Calcium
Smaller stimuli initiates the action potential

Clinical Manifestations:Clinical Manifestations: paresthesiaparesthesia ↓ ↓ ed COed CO ↑ ↑ ed peristalsis and drhed peristalsis and drh Prolonged bleeding times and hemorrhageProlonged bleeding times and hemorrhage Bones become brittle and results in pathologic fracturesBones become brittle and results in pathologic fractures Facial TwitchingFacial Twitching (Chvostek’s sign)(Chvostek’s sign) Carpopedal spasmCarpopedal spasm (Trousseau’s sign)(Trousseau’s sign) ECG changes: prolonged QT intervalECG changes: prolonged QT interval Severe: seizure, tetany, hemorrhage, cardiac collapseSevere: seizure, tetany, hemorrhage, cardiac collapse True level of free Ca: ionized Ca levelTrue level of free Ca: ionized Ca level

Trousseau’s SignTrousseau’s Sign

2. Hypercalcemia2. Hypercalcemia
Etiology and RF:Etiology and RF: Major Causes Major Causes Metastatic malignancy (Tumor Lysis Syndrome)Metastatic malignancy (Tumor Lysis Syndrome) HyperparathyroidismHyperparathyroidism Thiazide diuretic therapyThiazide diuretic therapy
Other Causes:Other Causes: Excessive intake of Ca supplements w/ vit. D, Ca Excessive intake of Ca supplements w/ vit. D, Ca
containing antacidscontaining antacids Prolonged immobilization Prolonged immobilization Metabolic acidosisMetabolic acidosis HypophosphatemiaHypophosphatemia

↑ Calcium
↑ cell membrane potential threshold
cell membrane becomes refractory to depolarization
cell membrane becomes less excitable and requires greater stimulus to produce response

Clinical Manifestations:Clinical Manifestations: GI- anorexia, N/V, abdominal distention & GI- anorexia, N/V, abdominal distention &
constipationconstipation Neurologic Depression – weakness, fatigue, Neurologic Depression – weakness, fatigue,
depression, difficulty concentratingdepression, difficulty concentrating Osmotic diuresisOsmotic diuresis ureteral or kidney stonesureteral or kidney stones ECG Changes: short QT interval, widened T waveECG Changes: short QT interval, widened T wave
(cardiac depression (cardiac depression dysrhythmias & arrest) dysrhythmias & arrest)

D. Phosphate ImbalancesD. Phosphate Imbalances Phosphate promotes strong and durables bonesPhosphate promotes strong and durables bones Phosphate is an integral part of ATP, ADPPhosphate is an integral part of ATP, ADP Phosphate plasma level is regulated by PTHPhosphate plasma level is regulated by PTH Facilitates release of Hgb and maintenance of acid-base balance, nervous Facilitates release of Hgb and maintenance of acid-base balance, nervous
system, and intermediary metabolism of CHO, CHON, and fatssystem, and intermediary metabolism of CHO, CHON, and fats
1. Hypophosphatemia1. Hypophosphatemia
Etiology and RF:Etiology and RF: Major loss/ long term lack of intakeMajor loss/ long term lack of intake Other RF: periods of ↑ ed growth or tse. Repair and recovery from Other RF: periods of ↑ ed growth or tse. Repair and recovery from
malnourished statesmalnourished states Prolonged/ excessive intake of antacidsProlonged/ excessive intake of antacids Administration of high levels of glucose via tube feeding/ IV lineAdministration of high levels of glucose via tube feeding/ IV line
(glucose cause the P to enter the cell for glucose phosphorylation) (glucose cause the P to enter the cell for glucose phosphorylation) ↑ ↑ ed Na+, ↑ ed Ca, ↓ ed PaCO2 in resp. alkalosised Na+, ↑ ed Ca, ↓ ed PaCO2 in resp. alkalosis Lead poisoningLead poisoning BurnsBurns

Clinical Manifestations:Clinical Manifestations: ↓ ↓ ed cardiac and respiratory fxned cardiac and respiratory fxn Muscle weaknessMuscle weakness FatigueFatigue Brittle bonesBrittle bones Confusion and SeizuresConfusion and Seizures
2. Hyperphosphatemia 2. Hyperphosphatemia
Etiology and RF:Etiology and RF: Excessive intake of high- PO4 foodsExcessive intake of high- PO4 foods Excess vit. DExcess vit. D Impaired colonic motility from ↑ ed absorptionImpaired colonic motility from ↑ ed absorption Hypoparathyroidism and Addison’s dse.Hypoparathyroidism and Addison’s dse. Renal failureRenal failure TLS TLS Post menopausal statePost menopausal state

Clinical Manifestations:Clinical Manifestations:
↑ ↑ ed PRed PR PalpitationsPalpitations RestlessnessRestlessness Anorexia, N/V, tetany, hyperreflexia, dydrhymiasAnorexia, N/V, tetany, hyperreflexia, dydrhymias
Food rich in PO4:Food rich in PO4: Milk, ice cream, cheese, large amounts of meat and fish, Milk, ice cream, cheese, large amounts of meat and fish,
carbonated beveragescarbonated beverages

E. Magnesium ImbalancesE. Magnesium Imbalances Actions similar to K+Actions similar to K+ Signs of imbalance similar to K+Signs of imbalance similar to K+ 22ndnd most abundant intracellular cation most abundant intracellular cation Fxns: transmission & conduction of nerve impulses Fxns: transmission & conduction of nerve impulses
– Contraction of MuscleContraction of Muscle– Responsible for the transportation of Na+ & K+ Responsible for the transportation of Na+ & K+
across cell membraneacross cell membrane– Responsible for the synthesis & release of PTHResponsible for the synthesis & release of PTH
increased Ca and Phosphorus= can ↓ Mg absorption increased Ca and Phosphorus= can ↓ Mg absorption from intestinesfrom intestines
↓ ↓ ed Mg can lead to hypokalemia and hypocalcemiaed Mg can lead to hypokalemia and hypocalcemia

Acts as an activator for many Acts as an activator for many intracellular enzyme system and plays a intracellular enzyme system and plays a role in both carbohydrate and CHON role in both carbohydrate and CHON metabolismmetabolism
1/3 CHON bound1/3 CHON bound2/3 free Mg2/3 free MgPredominantly found in bones and soft Predominantly found in bones and soft
tissues and eliminated by the kidney.tissues and eliminated by the kidney.

HypomagnesemiaHypomagnesemia Common cause of refractory hypokalemia and Common cause of refractory hypokalemia and
hypocalcemiahypocalcemia ETIOLOGY AND RF:ETIOLOGY AND RF:
– Critically illCritically ill– AlcoholicsAlcoholics– Malabsorption syndromesMalabsorption syndromes– GI lossesGI losses– Diuretic phase of renal failureDiuretic phase of renal failure– Excess Ca and excess Na inhibits MgExcess Ca and excess Na inhibits Mg– Prolonged IV or TPN therapy w/ Mg replacementProlonged IV or TPN therapy w/ Mg replacement– Hyperglycemia, osmotic diuresisHyperglycemia, osmotic diuresis– Many medicationsMany medications– Diuretics and antibiotics (aminoglycosides)Diuretics and antibiotics (aminoglycosides)– Corticosteroids and digitalis – promotes uptake of MgCorticosteroids and digitalis – promotes uptake of Mg– EstrogenEstrogen

Clinical Manifestations:Clinical Manifestations: Myocardial irritabilityMyocardial irritability Anorexia, nausea, abdominal distentionAnorexia, nausea, abdominal distention Psychological disordersPsychological disorders Neuromuscular Manifestations- Chvostek’s sign, Neuromuscular Manifestations- Chvostek’s sign,
Trousseau’s sign, tetany, convulsions, vasospasm Trousseau’s sign, tetany, convulsions, vasospasm leading to strokeleading to stroke
ECG changes – prolonged QT, widened QRS, ECG changes – prolonged QT, widened QRS, broadened T-wavesbroadened T-waves

2. Hypermagnesemia2. Hypermagnesemia
Etiology and RF:Etiology and RF: Renal insufficiencyRenal insufficiency Excessive use of Mg- containing antacidsExcessive use of Mg- containing antacids Excessive use of Mg- containing laxativesExcessive use of Mg- containing laxatives Administration of K+ sparing diureticsAdministration of K+ sparing diuretics Severe dhn from DKASevere dhn from DKA ↓ ↓ ed synthesis of aldosteroneed synthesis of aldosterone Overuse of IV MgSO4Overuse of IV MgSO4
Clinical Manifestations:Clinical Manifestations: Decreased muscle activityDecreased muscle activity HypotensionHypotension Severe muscle weakness, lethargy, drowsiness, loss of deep tendon Severe muscle weakness, lethargy, drowsiness, loss of deep tendon
reflex, respiratory paralysis and loss of consciousnessreflex, respiratory paralysis and loss of consciousness ECG – prolonged PR interval, widened QRSECG – prolonged PR interval, widened QRS


ACID BASE BALANCEACID BASE BALANCE
Concept : Normal functions of body cells depend or theConcept : Normal functions of body cells depend or the
regulation of Hydrogen ion (H+) concentration – theregulation of Hydrogen ion (H+) concentration – the
determinant of serum pH (acidity/ alkalinity)determinant of serum pH (acidity/ alkalinity)
Acid-Base Balance – refers to the Hydrogen (H+) ionAcid-Base Balance – refers to the Hydrogen (H+) ion
concentration in the body.concentration in the body.
AcidAcid- a substance which when dissolved in H20 can - a substance which when dissolved in H20 can dissociate and increase the H+ ion concentration; dissociate and increase the H+ ion concentration; hydrogen ion donor.hydrogen ion donor.
Base –Base – a substance which when dissolved in H20 can a substance which when dissolved in H20 can
dissociate and increase the Hydrogen ion (OH)dissociate and increase the Hydrogen ion (OH)
concentration and the therefore neutralizes theconcentration and the therefore neutralizes the
hydrogen ions; hydrogen ion acceptorhydrogen ions; hydrogen ion acceptor

pH – pH – used to express the degree of acidity or alkalinity of aused to express the degree of acidity or alkalinity of a
solution; normal serum pHs 7.35 -7.45solution; normal serum pHs 7.35 -7.45
Normal concentrations of H+ in the body fluids: 0.00004Normal concentrations of H+ in the body fluids: 0.00004
mEq/LmEq/L
Functions of H+Functions of H+ Necessary for proper cellular functionNecessary for proper cellular function Efficient functioning of every systemEfficient functioning of every system Binding of O2 with hemoglobinBinding of O2 with hemoglobin Acts as powerful chemical adjutator with body fluidsActs as powerful chemical adjutator with body fluids Determines the alkalinity and acidity of solutionDetermines the alkalinity and acidity of solution

Regulation of Acid-Base BalanceRegulation of Acid-Base Balance
1. Modulation of serum pH blood buffer system1. Modulation of serum pH blood buffer system
Buffer SystemBuffer System – consist of weak acid and salt of base – consist of weak acid and salt of base
which act together to neutralize either acid or bases;which act together to neutralize either acid or bases;
body line of defense against acid-base imbalance. body line of defense against acid-base imbalance.
Bicarbonate Buffer System:Bicarbonate Buffer System:
-Most important buffer system in the body (ECF)-Most important buffer system in the body (ECF)
-Comprises 1/12 of the buffer system-Comprises 1/12 of the buffer system

NaH CO3(Bicarbonate)NaH CO3(Bicarbonate)– Weak baseWeak base– Regulated by the kidneysRegulated by the kidneys
H2CO3 (Carbonic Acid)H2CO3 (Carbonic Acid)– A weak acid A weak acid – Regulated by the lungs through respirationRegulated by the lungs through respiration
In order to maintain the ph at a normal level (7.35-7.45 or In order to maintain the ph at a normal level (7.35-7.45 or an average of 7.4) the ration of bicarbonate to carbonic an average of 7.4) the ration of bicarbonate to carbonic acid must be 20:1.acid must be 20:1.
The pH of buffered solutions tend to remain fairly stable The pH of buffered solutions tend to remain fairly stable despite the addition of strong acids or bases because the despite the addition of strong acids or bases because the buffer system converts them to weaker forms.buffer system converts them to weaker forms.

2.Regulation of volatile acid by the lungs2.Regulation of volatile acid by the lungs
Volatile AcidsVolatile Acids- acids that can be converted to gases. - acids that can be converted to gases.
Carbon dioxideCarbon dioxide – potential acid; continuously produces by – potential acid; continuously produces by body cells as an end product of complete oxidative body cells as an end product of complete oxidative metabolism of nutrients for energy.metabolism of nutrients for energy.– 99.9 % of carbonic acid dissociates into CO2 to H2o. therefore by 99.9 % of carbonic acid dissociates into CO2 to H2o. therefore by
increasing or decreasing respiration, Co2 can be conserved or lost; increasing or decreasing respiration, Co2 can be conserved or lost; and carbonic acid concentration is affected.and carbonic acid concentration is affected.
The pH of the blood stimulates the respiration center so The pH of the blood stimulates the respiration center so that respiration are increased in alkalosis or decrease in that respiration are increased in alkalosis or decrease in acidosisacidosis
hypoventilation – hypercapnea (increased CO2)hypoventilation – hypercapnea (increased CO2) hyperventilation –hypocapnea (decrease CO2)hyperventilation –hypocapnea (decrease CO2)

3.Regulation of fixed Acids and Bicarbonate by the Kidneys3.Regulation of fixed Acids and Bicarbonate by the Kidneys
The Kidneys regulate bicarbonate concentration by:The Kidneys regulate bicarbonate concentration by: Excreting excess acid/baseExcreting excess acid/base Reabsorbing needed baseReabsorbing needed base
Urinary Buffer System- the kidney regulate serum pH by secretingUrinary Buffer System- the kidney regulate serum pH by secreting
H+ into the urine and by regenerating HCO3 for reabsorption intoH+ into the urine and by regenerating HCO3 for reabsorption into
the blood; permits tubular fluid to accept large quantities of H+the blood; permits tubular fluid to accept large quantities of H+
while limiting how much the urinary pH decreases.while limiting how much the urinary pH decreases.
pH is the direct indication of acidity (increased H+ concentration )pH is the direct indication of acidity (increased H+ concentration )
or alkalinity (decreased H+ concentration)or alkalinity (decreased H+ concentration) pCo2 is inversely proportional with pHpCo2 is inversely proportional with pH
– HCO3 and pO2 is directly proportional with pHHCO3 and pO2 is directly proportional with pH– pO2 and H2Co3 is directly proportionalpO2 and H2Co3 is directly proportional

Normal Values of ABG ( arterial blood Gas) AnalysisNormal Values of ABG ( arterial blood Gas) Analysis
pH = 7.35 to 7.45 mmHgpH = 7.35 to 7.45 mmHg
pCO2 = 34-45 mmHgpCO2 = 34-45 mmHg
HCO3 = 24-26 mEq/LHCO3 = 24-26 mEq/L
pO2 = 90 -110 mmHgpO2 = 90 -110 mmHg
In order to interpret ABG result, remember the followingIn order to interpret ABG result, remember the following pCO2 = respiratory parameterpCO2 = respiratory parameter
where:where: = acidosis= acidosis
==alkalosisalkalosis HCO3 = metabolic parameter HCO3 = metabolic parameter
where:where: = acidosis= acidosis
= alkalosis = alkalosis

IV Site Selection for ABGIV Site Selection for ABG

Interpretation of the Arterial Blood GasInterpretation of the Arterial Blood GasOverviewThe pH is a measurement of the acidity or alkalinity of the blood. It is inversely proportional to the number of hydrogen ions (H+) in the blood. The more H+ present, the lower the pH will be.Likewise, the fewer H+ present, the higher the pH will be. The pH of a solution is measured on a scale from 1 (very acidic) to 14 (very alkalotic). A liquid with a pH of 7, such as water, is neutral (neither acidic nor alkalotic).
The normal blood pH range is 7.35 to 7.45. In order for normal metabolism to take place, the body must maintain this narrow range at all times. When the pH is below 7.35, the blood is said to be acidic. Changes in body system functions that occur in an acidic state include a decrease in the force of cardiac contractions, a decrease in the vascular response to catecholamines, and a diminished response to the effects and actions of certain medications.
When the pH is above 7.45, the blood is said to be alkalotic. An alkalotic state interferes with tissue oxygenation and normal neurological and muscular functioning.
Significant changes in the blood pH above 7.8 or below 6.8 will interfere with cellular functioning, and if uncorrected, will lead to death.

Components of the Arterial Blood Gas
pH: Measurement of acidity or alkalinity, based on the hydrogen (H+) ions present.The normal range is 7.35 to 7.45
PaO2: The partial pressure of oxygen that is dissolved in arterial blood.The normal range is 80 to 100 mm Hg.
SaO2: The arterial oxygen saturation.The normal range is 95% to 100%.
PaCO2: The amount of carbon dioxide dissolved in arterial blood.The normal range is 35 to 45 mm Hg.
HCO3: The calculated value of the amount of bicarbonate in the bloodstream.The normal range is 22 to 26 mEq/liter

Step One
Assess the pH to determine if the blood is within normal range, alkalotic or acidotic. If it is above 7.45, the blood is alkalotic. If it is below 7.35, the blood is acidotic.

Step Two
If the blood is alkalotic or acidotic, we now need to determine if it is caused primarily by a respiratory or metabolic problem. To do this, assess the PaCO2 level. Remember that with a respiratory problem, as the pH decreases below 7.35, the PaCO2 should rise. If the pH rises above 7.45, the PaCO2 should fall. Compare the pH and the PaCO2 values. If pH and PaCO2 are indeed moving in opposite directions, then the problem is primarily respiratory in nature.

Step Three
Finally, assess the HCO3 value. Recall that with a metabolic problem, normally as the pH increases, the HCO3 should also increase. Likewise, as the pH decreases, so should the HCO3. Compare the two values. If they are moving in the same direction, then the problem is primarily metabolic in nature. The following chart summarizes the relationships between pH, PaCO2 and HCO3.

pH PaCO2 HCO3
Respiratory Acidosis ↓ ↑ normalRespiratory Alkalosis ↑ ↓ normalMetabolic Acidosis ↓ normal ↓Metabolic Alkalosis ↑ normal ↑

Jane Doe is a 45-year-old female admitted to the nursing unit with a severe asthma attack. She has been experiencing increasing shortness of breath since admission three hours ago.
Her arterial blood gas result is as follows: pH 7.22 PaCO2 55 HCO3 25
Follow the steps:1. Assess the pH. It is low (normal 7.35-7.45);therefore, we have
acidosis.2. Assess the PaCO2. It is high (normal 35-45) and in the
opposite direction of the pH.3. Assess the HCO3. It has remained within the normal range
(22-26).

pH PCO2 HCO3Respiratory Acidosis ↓ ↑ Normal
Refer to the chart. Acidosis is present (decreased pH) with the PaCO3 being increased, reflecting a primary respiratory problem. For this patient, we need to improve the ventilation status by providing oxygen therapy, mechanical ventilation, pulmonary toilet or by administering bronchodilators.

John Doe is a 55-year-old male admitted to your nursing unit with a recurring bowel obstruction. He has been experiencing intractable vomiting for the last several hours despite the use of antiemetics. Here is his arterial blood gas result:
pH 7.50 PaCO2 42 HCO3 33
Follow the three steps again:1. Assess the pH. It is high (normal 7.35-7.45)
2. Assess the PaCO2.
3. Assess the HCO3.

pH PCO2 HCO3
Metabolic Alkalosis ↑ normal ↑
Again, look at the chart. Alkalosis is present (increased pH) with the HCO3 increased, reflecting a primary metabolic problem. Treatment of this patient might include the administration of I.V. fluids and measures to reduce the excess base.

Compensation When a patient develops an acid-base imbalance,
the body attempts to compensate. Remember that the lungs and the kidneys are the primary buffer response systems in the body. The body tries to overcome either a respiratory or metabolic dysfunction in an attempt to return the Ph into the normal range.
A patient can be uncompensated, partially compensated, or fully compensated. When an acid-base disorder is either uncompensated or partially compensated, the pH remains outside the normal range. In fully compensated states, the pH has returned to within the normal range, although the other values may still be abnormal. Be aware that neither system has the ability to overcompensate.

Partial compensation:
1. Assess the pH.
2. Assess the PaCO2. In an uncompensated state, we have already seen that the pH and PaCO2 move in opposite directions when indicating that the primary problem is respiratory. But what if the pH and PaCO2 are moving in the same direction? We would then conclude that the primary problem was metabolic. In this case, the decreasing PaCO2 indicates that the lungs, acting as a buffer response, are attempting to correct the pH back into its normal range by decreasing the PaCO2. If evidence of compensation is present, but the pH has not yet been corrected to within its normal range, this would be described as a metabolic disorder with a partial respiratory compensation.
3. Assess the HCO3. In our original uncompensated examples, the pH and HCO3 move in the same direction, indicating that the primary problem was metabolic. But what if our results show the pH and HCO3 moving in opposite directions? That is not what we would expect to see. We would conclude that the primary acid-base disorder is respiratory, and that the kidneys, again acting as a buffer response system, are compensating by retaining HCO3, ultimately attempting to return the pH back towards the normal range.

Partially Compensated States
pH PaCO2 HCO3Respiratory Acidosis ↓ ↑ ↑Respiratory Alkalosis ↑ ↓ ↓Metabolic Acidosis ↓ ↓ ↓Metabolic Alkalosis ↑ ↑ ↑
Fully Compensated States
pH PaCO2 HCO3
Respiratory Acidosis normal ↑ ↑ but <7.40
Respiratory Alkalosis normal ↓ ↓ but >7.40
Metabolic Acidosis normal ↓ ↓ but <7.40
Metabolic Alkalosis normal ↑ ↑ but >7.40

John Doe is admitted to the hospital. He is a John Doe is admitted to the hospital. He is a kidney dialysis patient who has missed his kidney dialysis patient who has missed his last two appointments at the dialysis center. last two appointments at the dialysis center. His arterial blood gas values are reported as His arterial blood gas values are reported as follows:follows:
pH 7.32pH 7.32PaCO2 32PaCO2 32HCO3 - 18HCO3 - 18

pHpH PaCO2 PaCO2 HCO3HCO3
Metabolic Acidosis Metabolic Acidosis ↓ ↓ ↓ ↓ ↓ ↓1. Assess the pH. It is low (normal 7.35-7.45); therefore we have acidosis.2. Assess the PaCO2. It is low. Normally we would expect the pH and PaCO2 to move in opposite directions, but this is not the case. Because the pH and PaCO2 are moving in the same direction, it indicates that the acid-base disorder is primarily metabolic. In this case, the lungs, acting as the primary acid-base buffer, are now attempting to compensate by “blowing off excessive C02”, and therefore increasing the pH.3. Assess the HCO3. It is low (normal 22-26). We would expect the pH and the HCO3 to move in the same direction, confirming that the primary problem is metabolic.
Because there is evidence of compensation (pH and PaCO2 moving in the same direction) and because the pH remains below the normal range, we would interpret this ABG result as a partially compensated metabolic acidosis.

Jane Doe is a patient with chronic COPD Jane Doe is a patient with chronic COPD being admitted for surgery. Her admission lab being admitted for surgery. Her admission lab work reveals an arterial blood gas with the work reveals an arterial blood gas with the following values:following values:
pH = 7.35pH = 7.35
PaCO2 = 48PaCO2 = 48
HCO3 = 28HCO3 = 28

pHpH PaCO2 PaCO2 HCO3HCO3
Respiratory Acidosis Respiratory Acidosis normal ↑ ↑normal ↑ ↑ but <7.40 but <7.40
1.1. Assess the pH. It is within the normal range, but on the low side Assess the pH. It is within the normal range, but on the low side of neutral (<7.40).of neutral (<7.40).
2. Assess the PaCO2. It is high (normal 35-45). We would expect 2. Assess the PaCO2. It is high (normal 35-45). We would expect the pH and PaCO2 to move in opposite directions if the primary the pH and PaCO2 to move in opposite directions if the primary problem is respiratory.problem is respiratory.
3. Assess the HCO3. It is also high (22-26). Normally, the pH and 3. Assess the HCO3. It is also high (22-26). Normally, the pH and HCO3 should move in the same direction. Because they are HCO3 should move in the same direction. Because they are moving in opposite directions, it confirms that the primary acid-moving in opposite directions, it confirms that the primary acid-base disorder is respiratory and that the kidneys are attempting base disorder is respiratory and that the kidneys are attempting to compensate by retaining HCO3. Because the pH has returned to compensate by retaining HCO3. Because the pH has returned into the low normal range, we would interpret this ABG as a into the low normal range, we would interpret this ABG as a fully fully compensated respiratory acidosis.compensated respiratory acidosis.