Fluid and electrolytes,_balance_and_disturbances
-
Upload
v-chandiran-chetiyar -
Category
Health & Medicine
-
view
76 -
download
1
Transcript of Fluid and electrolytes,_balance_and_disturbances

Fluid and Electrolytes, Balance and Disturbances
Mr. v. chandiran, MSN,
K.M.C.H. CON

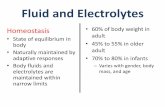
Fluid and Electrolytes
• 60% of body consists of fluid
• Intracellular space [2/3]
• Extracellular space [1/3]
• Electrolytes are active ions: positively and negatively charged

Regulation of Body Fluid Compartments
• Osmosis is the diffusion of water caused by fluid gradient

Regulation of Body Fluid Compartments 2
• Tonicity is the ability of solutes to cause osmotic driving forces
• Determines the cell size and hydration

Regulation of Body Fluid Compartments 3
• Diffusion is the movement of a substance from area of higher concentration to one of lower
concentration
• “Downhill
Movement”

Regulation of Body Fluid Compartments 4
• Filtration is the movement of water and solutes from an area of high hydrostatic pressure to an area of low hydrostatic pressure

Regulation of Body Fluid Compartments 5
• Osmolality reflects the concentration of fluid that affects the movement of water between fluid compartments by osmosis

Regulation of Body Fluid Compartments 6
• Osmotic pressure is the amount of hydrostatic pressure needed to stop the flow of water by osmosis

Sodium-Potassium Pump
• Sodium concentration is higher in ECF than ICF
• Sodium enters cell by diffusion
• Potassium exits cell into ECF

Gains and Losses
• Water and electrolytes move in a variety of ways–Kidneys. 1ml/kg
–Skin. perspiration
–Lungs. 300ml/day
–GI tract. 100-200 ml/day

Regulation of body water
The default is get rid of it
The control processes include:
Release of ADH (antidiuretic hormone)
Thirst

Regulation of body water
Any of the following:
• Decreased amount of water in body
• Increased amount of Na+ in the body
• Increased blood osmolality
• Decreased circulating blood volume
Results in:
• Stimulation of osmoreceptors in hypothalamus
• Release of ADH from the posterior pituitary
• Increased thirst
And thus: water consumption and conservation

Fluid Volume Disturbances
• Fluid Volume deficit.

Fluid Volume Deficit
• Mild – 2% of body weight loss
• Moderate – 5% of body weight loss
• Severe – 8% or more of body
weight loss

Fluid Volume Deficit
• Pathophysiology – results from loss of body fluids and occurs more rapidly when coupled with decreased fluid intake

Fluid Volume Deficit 4
• Risk factors:– Diabetus insipidus. Excessive thirst .
Excretion of large amounts of severly diluted urine
– Adrenal insufficiency. aldosterone– Hemorrhage– Third space fluid shift. Edema in burns and
ascites with liver dysfunction.

Fluid Volume Deficit 2
• Clinical manifestations
?

Fluid Volume Deficit 3
- Acute weight loss- Decreased skin turgor
- Oliguria
- Concentrated urine
- Postural hypotension
- Weak, rapid, heart rate
- Flattened neck veins
- Increased temperature
- Decreased central venous pressure

Fluid Volume Deficit 5
• Assessment:– BUN ELEVATED 7-30 mg/dl– BUN : CREATININE(0.7-1.2 mg/dl) > 20:1– Hypokalemia due to GI or renal loss– Hyperkalemia occurs with adrenal insufficiency– Hyponatremia with thirst and ADH release– Hypernatremia results from insensible loss and DI.– Urine osmalality > 450 mOsm/kg– Urine sp. Gravity 1.001-1.035

Difference between andHYPOVOLEMIA• Extracellular fluid volume
is reduced, results in decreased tissue perfusion.
• It can be produced by salt and water loss (e.g., with vomiting, diarrhea, diuretics or third spacing)
• salt and water loss comes from Extracellular fluid
• TREATMENT: salt-based so- called “crystalloid” infusion.
DEHYDRATION• Water loss alone is
termed as DEHYDRATION.
• Pure water loss comes from total body water, only about 1/3 is of ECF.
• ALWAYS HYPERNATREMIC.
• TREATMENT: free water administration.

Fluid Volume Deficit 6
• Management:– Isotonic solution (RL/ 0.9% NACL)-
Hypotensive & FVD– HYPOTONIC SOLUTION (0.45% NACL) –
normotensive + FVD

• 0.9% NaCl • Na+ 154 mEq/L• Cl− 154 mEq/L• (308 mOsm/L)
• expands the extracellular fluid volume, used in hypovolemic states, resuscitative efforts, shock, metabolic alkalosis, hypercalcemia, mild Na+ deficit.
• Supplies an excess of Na+ and Cl−; can cause fluid volume excess and hyperchloremic acidosis if used in excessive volumes, particularly in patients with compromised renal function, heart failure, or edema
• Not desirable as a routine maintenance solution, as it provides only Na+ and Cl− (and these are provided in excessive amounts)

• Lactated Ringer’s solution
• (Hartmann’s solution)• Na+ 130 mEq/L• K+ 4 mEq/L• Ca++ 3 mEq/L• Cl− 109 mEq/L• Lactate (metabolized
to bicarbonate)• 28 mEq/L (274
mOsm/L)
• Contains multiple electrolytes in roughly the same concentration as found in plasma (note that solution is lacking in Mg++): provides 9 calories/L
• Used in the treatment of hypovolemia, burns, fluid lost as bile or diarrhea, and for acute blood loss Replacement
• Should not be used in renal failure because it contains potassium and can cause hyperkalemia
• Similar to plasma

• Hypotonic Solutions• 0.45% NaCl (half-
strength saline)• Na+ 77 mEq/L• Cl− 77 mEq/L• (154 mOsm/L)
• Provides Na+, Cl−, and free water
• Free water is desirable to aid the kidneys in elimination of solute.
• Used to treat hypertonic dehydration, Na+ and Cl− depletion, and gastric fluid loss
• Not indicated for third-space fluid shifts or increased intracranial pressure
• Administer cautiously, as it can cause fluid shifts from vascular system into cells, resulting in cardiovascular collapse and increased intracranial pressure.

Nursing Diagnosis
• Fluid volume Deficit r/t Insufficient intake, vomiting, diarrhea, hemorragem/b dry mucous membranes, low BP, HR 112-122,
BUN 28, Na 152, urine dark amber; Intake 200mL/Output 450mL over 24 hours
Goal: Client will have adequate fluid volume within 24 hours AEB:
Moist tongue, mucous membranes, HR WNL, BUN between 8-20, Na 135-145, Urine clear yellow, balanced I/O

Fluid Volume Deficit 5
• Nursing management - Restore fluids by oral or IV- Treat underlying cause- Monitor I & O at least every 8 hours- Daily weight 0.5kg= 500ml loss- Vital signs- Skin turgor- Urine concentration

Fluid Volume Disturbances 2
• Fluid Volume Excess (Hypervolemia)

Fluid Volume Excess
• Pathophysiology – may be related to fluid overload or diminished function of the homeostatic mechinisms responsible for regulating fluid balance
• Contributing factors – CHF, renal failure, cirrhosis

Fluid Volume Excess 2
• Clinical manifestations – edema, distended neck veins, crackles, tachycardia, increased blood pressure, increased weight

Fluid Volume Excess 3• DIAGNOSTIC FINDINGS:
– Hb & Hematocrit– serum & urine osmolarity– urine sodium and sp. Gravity– CXR- pulmonary congestion

Fluid Volume Excess 4
• Diuretics: – thiazide (hydrochlorothiazide)
• mild to moderate hypervolemia (block Na reabsorption in the distal tubule- where 5-10% filtered Na is reabsorbed)
– Loop (frusemide)• severe (blocks in asending limb of henle’s loop – where
20-30% filtered Na is reabsorbed)• Renal replacement therapy- To remove nitrogenous waste
and control potassium and acid base balance.
• Nutritional therapy

Nursing Diagnosis and Goal
• Fluid volume excess r/t CHF, excess sodium intake, renal failure AEB:
Weight gain of 6 lb. in 24 hours; lungs with crackles in bases bilaterally; 2+ edema in ankles bilaterally
Goal: Client will have normal fluid volume within 48 hours AEB:
Decreased weight of 1 lb. per day, lung sounds clear in all fields, ankles without edema

Fluid Volume Excess
• Nursing management– I/O chart, weight daily, gain – 1 kg =1 lit, breath
sounds, edema
• Preventing FVE– Fluid restriction, sodium restricted diet
• Controlling FVE– Semi fowlers position, rest (diuresis),
medicines.
• Teaching patients about edema

Electrolyte Imbalances
Sodium!
Normal range – 135 to 145 mEq/L
- Primary regulator of ECF volume (a loss or gain of sodium is usually accompanied by a loss or gain of water)

Hyponatremia
• Sodium level less than 135 mEq/L
• May be caused by vomiting, diarrhea, sweating, diuretics, etc.

Hyponatremia 2
• Clinical manifestations
- Poor skin turgor
- Dry mucosa
- Decreased saliva production
- Orthostatic hypotension
- Nausea/abdominal cramping
- Altered mental status

Differential Diagnosis for Hyponatremia
• In almost all cases, results from the intake (either oral or intravenous) and subsequent retention of water
• In almost all cases, occurs because there is an impairment in renal water excretion, due most often to an inability to suppress ADH release
• Elevated– Syndrome of Inappropriate ADH secretion– Hormonal changes
Adrenal insufficiency, pregnancy.

Evaluation of Patients with Hyponatremia
• Serum sodium level.• Assess volume status of patient
– Hypovolemia: orthostatic, dry mucous membranes– Hypervolemia: peripheral edema, pulmonary edema,
JVD, ascites
• For Euvolemic pt:– Check urine osmolality for SIADH (inappropriately
concentrated urine- should be dilute in this setting)

Hyponatremia 3
• Medical management– Sodium Replacement
• mild- isotonic solution IV.• Moderate – 2-4 lit over 6-12 hrs.• Severe – 2-3 lit in first 2-3 hrs, followed by 2-5 lit
within 24-48 hrs.
– Formula: ?
- Water Restriction

Hyponatremia 4
• Nursing Management
- Detecting and controlling hyponatremia
- Returning sodium level to normal

Critical Thinking Exercise: Nursing Management of the Client with
Hyponatremia• Situation: An 87 year old man was
admitted to the acute care facility for gastroenteritis, 2 day duration. He is vomiting, has severe, watery diarrhea and is c/o abd cramping. His serum electrolytes are consistent with hyponatremia r/t excessive sodium loss.

Critical Thinking Exercise: Nursing Management of the Client with
Hyponatremia 2• 1. What is the relationship between
vomiting, diarrhea, and hyponatremia?– Hypovolemic hyponatremia.
• 2. What s/s should the client be monitored for that indicate the presence of sodium deficit?
• 3. In addition to examining the client’s serum electrolyte findings, how will the nurse know when the client’s sodium level has returned to normal?

Hypernatremia
• Sodium level is greater than 145 mEq/L
- Can be caused by a gain of sodium in excess of water or by a loss of water in excess of sodium

Hypernatremia 2
• Etiopathogenesis:- Fluid deprivation in patients who cannot perceive,
respond to, or communicate their thirst- Most often affects very old, very young, and
cognitively impaired patients- Insensible loss- parenteral administration of hypertonic solution (3-
5% nacl, 7.5% of sodium bicarbonate)- salt consumption- With water excess – edema.

Hypernatremia 3
• Clinical manifestations
- Thirst
- Dry, swollen tongue
- Sticky mucous membranes
- Flushed skin
- Postural hypotension

Hypernatremia 4• Medical Management• Isotonic non saline solution dextrose 5% in
water. (An isotonic solution that supplies 170 calories/L and free water to aid in renal excretion of solutes. Used in treatment of hypernatremia, fluid loss, and dehydration)
• Formula: ?
– Desmopressin acetate, synthetic ADH- diabetes insipidus
• Nursing Management• - Preventing Hypernatremia
• - Correcting Hypernatremia


Critical Thinking Exercise: Nursing Management of the Client with
Hypernatremia• Situation: A 47 year old woman was taken to the
ER after she developed a rapid heart rate and agitation. Physical assessment revealed dry oral mucous membranes, poor skin turgor, and fever of 101.3 orally. The client’s daughter stated her mother had been very hungry recently and drinking more fluids than usual. Suspecting DM, the practitioner obtained serum electrolytes and glucose levels, which revealed serum sodium of 163 mEq/L and serum glucose of 360 mg/dL.

Critical Thinking Exercise: Nursing Management of the Client with
Hypernatremia 2• 1. Interpret the client’s lab data.• 2. Why are clients with DM prone to the
development of hypernatremia?• 3. What precautions should the nurse take when
caring for the client with hypernatremia?• 4. List 4 food items this client should avoid and
why.

All About Potassium
• Major Intracellular electrolyte
• 98% of the body’s potassium is inside the cells
• Influences both skeletal and cardiac muscle activity
• Normal serum potassium
concentration –
3.5 to 5.5 mEq/L.

Hypokalemia
• Serum Potassium below 3.5 mEq/L
Causes:
Diarrhea, diuretics, poor K intake, stress, steroid administration

Hypokalemia 2
• Clinical manifestations:– Muscle weakness, cardiac arrythmias, increased
sensitivity to digitalis toxicity, fatigue, – ECG changes
• ST depression, inverted T waves, prolonged PR interval, large U waves.
– Respiratory hyperventilation.– Skeletal muscle weakness– Irregular, weak pulse– Orthostatic hypotension– Numbness (paresthesia)

Management
• 40-80 mEq/day of K is adequate.
• IV is manditory for severe hypokalemia.
• Diet – 50-100mEq/ day.
• KCL is used often.
• Food rich in K – banana, melon, vegetables.

Hypokalemia 3
• Nursing interventions:– Assess sign & symptoms.– Encourage high K foods– Monitor ECG results– Dilute KCl! – can cause
cardiac arrest if given IVP

Hypokalemia 4
• Administering IV Potassium- Should be administered only after adequate
urine flow has been established- Decrease in urine volume to less than 20
mL/h for 2 hours is an indication to stop the potassium infusion
- IV K+ should not be given faster than 20 mEq/h

Critical Thinking Exercise: Nursing Management of the Client with
HypokalemiaSituation:
A 69 year old man has a history of CHF controlled by Digoxin and Lasix. Two weeks ago he developed diarrhea, which has persisted in spite of his taking OTC antidiarrheal meds. His partner transported him to the ER when she found him lethargic and confused. Initial assessment of the client reveals heart rate at 86 bpm, respiratory rate 10, and blood pressure 102/56 mmHg.

Critical Thinking Exercise: Nursing Management of the Client with
Hypokalemia 2• 1. An electrolyte panel shows the client’s serum
potassium is 2.9 mEq/L. Does the nurse have cause to be concerned about the client’s serum potassium? Why or why not?
• 2. What data supports the presence of hypokalemia in this client?
• 3. What, if anything, should the nurse do?• 4. What foods should the client be advised to eat
that are high in potassium?

Hyperkalemia
Serum Potassium greater than
5.5 mEq/L
-More dangerous than hypokalemia because cardiac arrest is frequently associated with high serum K+ levels

Hyperkalemia 2
• Etiopathogenis:– Decreased renal potassium excretion as seen with
renal failure and oliguria
- High potassium intake - Hypoaldosteronism - Shift of potassium out of the cell as seen in acidosis.
ECF K- Severe infection, major trauma, crush injuries

Hyperkalemia 3
• Clinical manifestations:
- Skeletal muscle weakness/paralysis
- ECG changes – such as peaked T waves, widened QRS complexes, absent P wave, ST depression.

Hyperkalemia 4Management:-Monitor ECG changes.-Administer Calcium solutions to neutralize the potassium-Monitor muscle tone- Sodium bicarbonate- in severe metabolic acidosis, shift K in to cells.-Regular insulin and hypertonic dextrose D50W
- shift K inside.-Loop diuretic- excrete H2O, inhibit reabsorption of Na, K, Cl in ascending loop of Henle-Give Kayexelate –k removing resin. Draws k in large intestine and eliminates.

Calcium
• More than 99% of the body’s calcium is located in the skeletal system
• Normal serum calcium level is 8.5 to 10mg/dL
• Needed for transmission of
nerve impulses
• Intracellular calcium is needed
for contraction of muscles

Calcium 2
• Extracellular needed for blood clotting
• Needed for tooth and bone formation
• Needed for maintaining a normal heart rhythm

Hypocalcemia
• Serum Calcium level less than 8.5 mEq/L

Hypocalcemia 2
• Causes- Vitamin D/Calcium consumption- Primary/surgical hypoparathyroidism- Radial neck dissection- Pancreatitis- Renal failure- Massive adm. Of citrated blood- transient hypocalcemia.- Medications- antacid, cisplatin, isoniazid, loop diuretics.

Hypocalcemia 3
• Clinical Manifestations
- Tetany and cramps in muscles of extremities
Definition – A nervous affection characterized by intermitten tonic spasms that are usually paroxysmal and involve the extremities

Hypocalcemia 4
• Seizures (irritability of CNS), mental changes
• Trousseau’s sign – carpal spasms

Hypocalcemia 5
- EKG shows
prolonged
QT intervals
• Chvostek’s sign – cheek twitching

Hypocalcemia 6
• Impaired clotting time
• Decreased prothrombin time
• Decreased blood pressure
• Diarrhea

Hypocalcemia 7
• Diagnostic findings:– Serum calcium levels– Calculate corrected serum calcium levels
= measured total serum Ca level (mg/dl)
+ 0.8
* [ 4.0- measured albumin level (g/dl) ]

Hypocalcemia 8
• Medical management- IV/PO Calcium Carbonate or Calcium Gluconate- Encourage increased dietary intake of Calcium- Monitor neurlogical status- Establish seizure precautions- Vit. D therapy.- Diet- Ca intake 1000-1500 mg/day

IV Treatment of Low Calciumper UofM CVC ICU Protocol Guidelines
Serum calcium concentration
Preferred calcium salt* Calcium dose
Recheck serum calcium
concentration
Ionized calcium = 1.05 – 1.11 mmol/L (or corrected calcium ~ 8 – 8.4 mg/dL)
Gluconate 1 g calcium gluconate over 30 – 60 minutes With next AM lab draw
Ionized calcium = 0.99 – 1.04 mmol/L (or corrected calcium ~ 7.5 – 7.9 mg/dL)
Gluconate 2 g calcium gluconate over 60 minutes 4 – 6 hours after completing dose
Ionized calcium = 0.93 – 0.98 mmol/L (or corrected calcium ~ 7 – 7.4 mg/dL)
Gluconate 3 g calcium gluconate over 60 minutes 4 – 6 hours after completing dose
Ionized calcium < 0.93 mmol/L (or corrected calcium < 7 mg/dL)
Gluconate 4 g calcium gluconate over 60 minutes and notify MD
4 – 6 hours after completing dose
72

Nursing consideration
• Check for digitalis medicine intake – as Ca exerts same effect and can cause digitalis toxicity.
• IV site – infiltration and extravasation.• 0.9% sodium chloride should not be used with
calcium- increases renal calcium loss.• Solution containing phosphates or bicarbonates
should not be used with calcium- precipitation.• Seizure precautions.

Hypercalcemia
• Serum Calcium level greater than 10.5 mEq/L (2.6 mmol/L)

Hypercalcemia 2
• Causes:
- Hyperparathyroidism & malignancies.- Excess PTH – increased release of calcium
from bones.
- Prolonged immobilization- bone mineral lost
- Thiazide diuretics
- Large doses of Vitamin A and D

Hypercalcemia 3
• Clinical manifestations:- Muscle weakness, nausea and vomiting- Lethargy and confusion- Constipation- Cardiac Arrest (in hypercalcemic crisis, level
17mg/dL or higher) severe thirst, polyuria, polydypsia, hypo active Deep tendon reflexes.
- ECG- short QT intervals.

Hypercalcemia 4 (>10.5mg/dL)• Assessment findings:
– Neuro – Disorientation, lethargy, coma, profound muscle weakness
– Resp. – Ineffective resp. movement– CV - Inc. HR, Inc. BP. , Bounding peripheral pulses, Positive
Homan’s sign. Late Phase – Bradycardia, Cardiac arrest– GI – Dec. motility. Dec. BS. Constipation– GU – Inc. urine output. Formation of renal calculi
• Diagnostic findings– Serum calcium level– ECG– PTH level increased– X ray – bone changes– Renal calculi,

Hypercalcemia 5
• Medical Management
- Eliminate Calcium from diet
- Monitor neurological status
- Increase fluids (IV or PO)
- IV phosphate
- Calcitonin
- Cancer- surgery/chemotherapy

Calcitonin
• - used to lower serum calcium level
- useful for pts with heart disease or renal failure
- reduces bone resorption
- increases deposit of calcium and phosphorus in the bones
- increases urinary excretion of calcium and phosphorus

• Parathyroid pulls, calcitonin keeps
Parathyroid hormone pulls calcium out of the bone.
Calcitonin keeps it there.

Magnesium
- Normal serum magnesium level is 1.5 to 2.5 mg/dL
- Helps maintain normal muscle and nerve activity- Exerts effects on the cardiovascular system,
acting peripherally to produce vasodilation- Thought to have a direct effect
on peripheral arteries and
arterioles

Hypomagnesemia
• Serum Magnesium level less than 1.5 mEq/L

Hypomagnesemia
• Causes - Chronic Alcoholism- Diarrhea, or any disruption in small bowel
function- TPN- Diabetic ketoacidosis- Malabsorption- Digitalis, diuretics, cyclosporin, cisplatin,
amphotericin, rapid adm. Of citrated blood.

Hypomagnesemia 3
• Clinical manifestations
- Neuromuscular irritability
- Positive Chvostek’s and Trousseau’s sign
- ECG changes with prolonged QRS, depressed ST segment, and cardiac dysrhythmias
- May occur with hypocalcemia and hypokalemia

STARVED
• Starved – possible cause of hypomagnesemia
• Seizures• Tetany• Anorexia and arrhythmias• Rapid heart rate• Vomiting• Emotional lability• Deep tendon reflexes increased

Hypomagnesemia 5
• Medical / Nursing management- IV/PO Magnesium replacement, including
Magnesium Sulfate- Give Calcium Gluconate if accompanied by
hypocalcemia- Monitor for dysphagia, give soft foods- Measure vital signs closely- Ca gluconate- to treat hypocalcemic tetany

IV Treatment of Low Magnesium
per UofM CVC ICU Protocol Guidelines
Serum magnesium concentration
Intravenous magnesium
sulfate dose†
Recheck serum magnesium concentration
1.9 – 2 mg/dL 1 g magnesium sulfate With next AM lab draw
1.7 – 1.8 mg/dL 2 g magnesium sulfate With next AM lab draw
1.6 – 1.7 mg/dL
3 g magnesium sulfate otherwise use sodium phosphate (1 mmol potassium phosphate = 1).
4 – 6 hours after completion of dose if symptomatic, otherwise with next AM lab draw
< 1.5 mg/dL Notify MD
Rate of intravenous infusion of magnesium
Recommend infusing 1 g magnesium sulfate/hour (~8 mEq magnesium/hour), up to maximum of 2 g magnesium sulfate/hour
87

Hypermagesemia
• Serum Magnesium level greater than 2.5 mEq/L

Hypermagnesemia 2
• Causes
- Renal failure
- Untreated diabetic ketoacidosis
- Excessive use of antacids and laxatives
- Treatment of hypertension in pregnancy
- Lithium intoxication
- Extensive soft tissue injury

Hypermagnesemia 3
• Clinical manifestations
- Flushed face and skin warmth
- Mild hypotension
- Heart block and cardiac arrest
- Muscle weakness and even paralysis
- Platelet clumping

• Reflexes decreased (plus weakness and paralysis)
• ECG changes (bradycardia and hypotension, prolonged PR interval, peaked T waves)
• Nausea and vomiting
• Appearance flushed
• Lethargy (plus drowsiness and
coma)

Hypermagnesemia 5• Medical/Nursing management
- Monitor Mg levels
- Monitor respiratory rate
- Monitor cardiac rhythm
- Increase fluids
- IV calcium for
emergencies

Thanks