I ntroduction d’androgènes en contraception orale ( Androgen Restored Contraception-ARC)
CONTRACEPTION: A PHARMACIST'S GUIDE TO...
Transcript of CONTRACEPTION: A PHARMACIST'S GUIDE TO...
CONTRACEPTION: A PHARMACIST'S GUIDE TO PRESCRIBING
SATURDAY/11:30AM-12:30PM
ACPE UAN: 0107-9999-17-234-L01-P 0.1 CEU/1.0 hr Activity Type: Application-Based Learning Objectives for Pharmacists: Upon completion of this CPE activity participants should be able to: 1. Choose an initial self-administered hormonal contraceptive product based on patient characteristics. 2. Recommend an alternative contraceptive product for a patient experiencing side effects from current
treatment. 3. Identify women who may require referral for additional evaluation by other healthcare team members due to
contraceptive-related needs. Speaker: Sarah Westberg, PharmD, FCCP, BCPS Dr. Westberg is currently a Co-Associate Dean for Clinical Affairs and an Associate Professor in the College of Pharmacy at the University of Minnesota. She graduated with her Pharm.D. from Drake University, completed a Pharmaceutical Care Leadership Residency at the University of Minnesota, and then joined the University of Minnesota faculty. During her career she has provided comprehensive medication management services in family medicine and internal medicine clinics, and is currently caring for patients at the Women’s Health Specialist Clinic. Her areas of interest are in developing and maintaining interprofessional team practices, women’s health, diabetes, and teaching learners to provide optimal care to patients in an interprofessional environment. Speaker Disclosure: Sarah Westberg reports no actual or potential conflicts of interest in relation to this CPE activity. Off-label use of medications will not be discussed during this presentation.
2/12/2018
1
Contraception:A Pharmacist’s Guide
to PrescribingSarah M. Westberg, Pharm.D., BCPS, FCCP
Associate Professor & Co-Associate Dean for Clinical Affairs
University of Minnesota College of Pharmacy
Disclosure
• Sarah Westberg reports no actual or potential conflicts of interest associated with this presentation
2/12/2018
2
Learning Objectives
• Upon successful completion of this activity, participants should be able to:
- Choose an initial self-administered hormonal contraceptive product based on patient characteristics.
- Recommend an alternative contraceptive product for a patient experiencing side effects from current treatment.
- Identify women who may require referral for additional evaluation by other healthcare team members due to contraceptive-related needs
Overview of Efficacy of Contraceptive Products% of Women Experiencing Unintended pregnancy within first year of use
Method Typical Use Perfect Use
Chance 85% 85%
Periodic Abstinence 24 0.4-5
Withdrawal 22 4
Spermicides 28 18
Male condom 18 2
Injectable MPA 6 0.2
COC 9 0.3
POP 9 0.3
Transdermal patch 9 0.3
Vaginal ring 9 0.3
Copper IUD 0.8 0.6
Levonorgestrel IUD 0.2 0.2
Implanon 0.05 0.05Adapted from CDC Select Practice Recommendations for Contraceptives. MMWR / June 21, 2013 / Vol. 62 / No. 5
2/12/2018
3
Mechanism of Action
EstrogensInhibit ovulation by preventing
development of dominant follicle by suppressing FSH
Inhibition of implantation
Accelerated ovum transport
Induction of luteolysis
ProgestinsInhibit ovulation by
suppressing LH secretion
Production of thick cervical mucus
Reduces sperm penetration into ovum
Slowing of ovum transport
Inhibition of implantation by altering endometrial lining
2/12/2018
4
COC preparations• Estrogen Dosage
- High dose: 50 mcg ethinyl estradiol- Low dose: 30-35 mcg ethinyl estradiol- Very low dose: 10-25 mcg ethinyl estradiol
• Length of cycle- 21 days active/7 days placebo OR- 24 days active/4 days placebo OR- 84 days active/7 days placebo OR- Continuous active
• Dose adjustments within cycle:- Monophasic, biphasic, triphasic, quadriphasic
• Unique characteristics- Some formulations contain small dose estrogen or iron in
the last “placebo” week
Extended-Cycle CHCs
• Unscheduled breakthrough bleeding and spotting is common
- Especially in 1st 3-6 months- Improves with continued use
• More common with no break from active pills- Usually improves over time
• Discuss with patients if they would prefer regular scheduled, predictable bleeding, or unpredictable breakthrough bleeding
2/12/2018
5
Non-Contraceptive Benefits: CHCs• Menstrual cycle benefits
- PMDD- Dysmenorrhea- Anemia- Menstrual – related migraines (without aura)- Any other cyclical mood complaint
• Improvement in benign breast disease - Benefit from progestin; use higher progestin/lower estrogen
• Possible decrease risk of colorectal CA
• Improvement in acne
• Decreased frequency of bacterial vaginosis
• Decrease risk of ovarian and endometrial cancers
US Medical Eligibility Criteria for Contraceptive Use
• Goal: “remove unnecessary medical barriers to accessing and using contraception, thereby decreasing the number of unintended pregnancies.”
• First published in 2010 (adapted from WHO), revised in 2016
• App available: CDC Contraception
U.S. Medical Eligibility Criteria for Contraceptive Use 2016. CDC. MMWR. July 29, 2016
2/12/2018
6
US Criteria for Contraceptive UseCategory Definition
1 A condition for which there is no restriction for the use of the contraceptive method
2 A condition for which the advantages of using the method generally outweigh the theoretical or proven risks
3 A condition for which the theoretical or proven risks usually outweigh the advantages of using the method
4 A condition which represents an unacceptable health risk if the contraceptive method is used.
U.S. Medical Eligibility Criteria for Contraceptive Use 2016. CDC. MMWR. July 29, 2016
Potential Risks of CHCs• Venous thromboembolism • Hypertension
- Less with desogestrel, norgestimate, drospirenone- From both estrogen & progestin
• Myocardial infarction- No increased risk except in smokers
• RR 3.5 if smoke < 15 cig/day• RR 21 if smoke > 15 cig/day
• Stroke- Risk only in smokers; possible increased risk with
uncontrolled HTN & migraines
2/12/2018
7
Let’s look at the chart…
…and the app
U.S. Medical Eligibility Criteria for Contraceptive Use 2016. CDC. MMWR. July 29, 2016
Common Clinically Relevant Medical Conditions limiting contraceptive use
• Hypertension / Elevated blood pressure (3-4)• Venous Thromboembolism & Stroke (3-4)• Personal history of breast cancer (3-4)• Diabetes with microvascular complications (3-4)• Migraines with aura (4)• H/O malabsorptive bariatric surgery (oral: 3)• ASCVD/Multiple risk factors for ASCVD (3-4)• Smoking (3-4 if >35 years)
• Less common: cirrhosis or other liver disease/tumor, peripartum cardiomyopathy, SLE, valvular heart disease
U.S. Medical Eligibility Criteria for Contraceptive Use 2016. CDC. MMWR. July 29, 2016
2/12/2018
8
Before Starting Contraceptives
• Be reasonably certain the woman is not pregnant:- No signs/symptoms AND 1 of the following:
• ≤ 7 days after start of normal menses• No intercourse since start of last menses• Correctly/consistently using reliable contraception• ≤ 7 days after spontaneous/induced abortion• Within 4 weeks postpartum• Is exclusively (or nearly) breastfeeding, amenorrheic and < 6
months postpartum
- May consider pregnancy test
CDC. Selected Practice Recommendations. MMWR 2016;65(4).
Using the CDC recommendations, which of the following patients should NOT take CHCs?
A. A 18 year old woman diagnosed with gonococcal infection
B. A 35 year old woman with daily tension headachesC. A 28 year old woman who is exclusively
breastfeeding her 4 month old infantD. A 45 year old woman with uncontrolled
hypertension
2/12/2018
9
Patient Education:General for all contraceptives
Patient education should be sure to include:- How/when to start- When to use backup contraception- Adverse effects- Drug interactions- Risks- Non-contraceptive benefits
Adverse Effects from COC’sEstrogen Excess
NauseaBloating
Cervical mucorrhea, polyposisMelasma
Migraine headacheHypertension
EdemaCyclic weight gainBreast fullness or
tendernessVTE
Progesterone Excess
Increased appetiteWeight gain
FatigueHypomenorrhea
DepressionHair loss / hirsutism
AcneVaginal candidiasis
Estrogen Deficiency
Early/midcycle BTB (pill days 1-14)
Increased spottingHypomenorrhea
Irritability, depressionHot flashes
Atrophic vaginitisDyspareunia
Progesterone Deficiency
Late BTB (pill days 14-21)Hypermenorrhea
2/12/2018
10
Adverse Effects: CHCs• Headaches
- Women with a history of migraines may vary in their responses to COC’s
- Headaches/migraines often occur during the placebo week, and are likely due to estrogen withdrawal.
- Shortening the hormone-free time (24/4, 84/4 or continuous), or providing estrogen during the placebo week can decrease headaches/migraines that occur.
Adverse Effects: CHCs
• Breakthrough bleeding with monthly CHC’s:- Common in first 2-3 months; improve in time – warn
patients! Wait 3 months until switching.- More common with lower estrogen COCs than higher- After the first three months, have patient keep bleeding
diary to determine timing of BTB• Should be for 3 consecutive months• Missed pills; drug interactions can also cause BTB
2/12/2018
11
22 y/o started on norethindrone 0.5 mg/ EE 35 mcg in a continuous 84/7 day cycle 5 months ago; c/o
breast tenderness, cramping, bloating. Which of the following recommendations is most appropriate?
A. Change to a product with higher progestationalactivity
B. Change to a product with lower progestationalactivity
C. Change to a product with higher estrogenic activityD. Change to a product with lower estrogenic activityE. Change to a product with lower androgenic activity
An 18 y/o started on norethindrone acetate 1 mg / EE 20/30/35 mcg in a 21/7 day cycle seven months
ago. She has gained 8 pounds at a consistent rate, although she exercises and watches her diet. She is
concerned about the weight gain. Which of the following recommendations is most appropriate?
A. Change to a product with higher progestational activity
B. Change to a product with lower progestational activity
C. Change to a product with higher estrogenic activity
D. Change to a product with lower estrogenic activity
E. Change to a product with lower androgenic activity
2/12/2018
12
A 23 year old college student has been taking drospirenone 3 mg/EE 30 mcg in a 21/7 day cycle
for 8 months and has noticed that she has been having headaches every month during the placebo
pills. They are severe enough that she misses classes during those weeks, but they are not
migraine headaches (no aura). What is the most appropriate course of action?
A. Change to a product with lower estrogenic activityB. Change to a product with higher estrogenic activityC. Change to an extended cycle regimenD. Change to a product with EE 10mcg in final 7 days
Change to a product with ferrous fumarate in the final 7 days
Extended-Cycle CHCs:Unscheduled Bleeding
• Discontinue 3-4 active pills, then restart (e.g., have a hormone-free interval)
- Only do after 21 days of active pills- Do not do more than once per month- Bleeding may first worsen, then improves in ~10 days
• May need to rule out underlying gynecologic problem
CDC. Selected Practice Recommendations. MMWR 2016;65(4).
2/12/2018
13
“Uh-oh….I forgot my pills!”
• Need 7 days of active treatment to prevent against conception
- unless within first 5 days of cycle, at which time ovulation is highly unlikely
• Generally 48 hours off of treatment will not compromise efficacy.
• >48 hours off of treatment hours requires backup contraception to ensure efficacy – need 7 days back on active pills
• Recognize this is conservative----women are off of active treatment for 7 of 28 days every month with efficacy
CDC. Selected Practice Recommendations. MMWR 2016;65(4).
“Uh-oh….I forgot my pills!”If 1 pill is missed, anywhere in the pack:• Take missed pill ASAP*; continue taking rest of pack as usual• No backup contraception neededIf ≥ 2 pills are missed:• Take the last missed pill ASAP*; discard any earlier missed pills• Continue taking rest of pack as usual• Use backup contraception until active pills have been taken for 7 consecutive
days• SKIP placebo pills if:
• Pills were missed in last week of active pills• Finish active pills in current pack but SKIP placebo pills and start new pack• If can’t start a new pack immediately, use backup contraception until 7
consecutive hormonal pills taken- Consider EC if:
• Pills were missed in the first week of pack and had unprotected intercourse in previous 5 days
• As appropriate at other times
CDC. Selected Practice Recommendations. MMWR 2016;65(4).
2/12/2018
14
“Uh-oh….I forgot my pills!”
• Extended or continuous use OCPs:- Up to 7 days can be missed. Hormone-free
interval (HFI) must not exceed 7 days. If HFI is > 7 days, follow instructions for missed pills for monthly OCPs
- Only applicable after 21 consecutive days after starting, or restarting (after missed pills)
• If significant vomiting or diarrhea, apply the same principles as missed pills
CDC. Selected Practice Recommendations. MMWR 2016;65(4).
Progestin-Only Pills (POPs)
• “Mini Pill”• Norethindrone 0.35 mg• 28 days of active pills; no placebo• Breakthrough bleeding/spotting and intermittent
amenorrhea common• Higher failure rates than COCs• Most common use is in breastfeeding women
2/12/2018
15
Progestin-Only Pills (POPs)
• If > 3 hours late in taking a pill or if vomiting or diarrhea occur within 3 hours of taking pill:
- Take 1 pill as soon as possible- Continue taking pills once daily at same time- May need to take 2 pills together or on same day if was
late with pill- Use backup contraception until 2 pills have been taken
on time for 2 consecutive days- Consider EC if unprotected intercourse
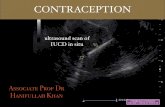
Contraceptive Patch
• Ethinyl estradiol & norelgestromin• Less effective in women > 198 lb.; avoid• Should stay attached during daily activities
(shower, swimming, exercise)• Same cautions/contraindications, risks, and drug
interactions as with combination COCs• Prescribe extra patch with Rx
2/12/2018
16
Contraceptive Vaginal Ring
• Flexible, transparent vaginal ring• Patient inserts themselves; no placement necessary• Releases ethinyl estradiol & etonorgestrel
- Same cautions, contraindications, etc as COCs
• Start between day 1-5 of menstrual cycle- Day 5 at the LATEST, even if still bleeding- Or start at any time and use backup contraception for 1st 7 days of 1st
cycle
• Ring inserted into the vagina & removed 3 weeks later (same day; approx. same time)
• Wait 1 week, then insert new ring (same day; approx. same time)
Adverse Effects: Contraceptive Vaginal Ring
• Similar adverse effects to COCs• Most common adverse effects reported:
- Vaginitis, vaginal secretion, headache, nausea, weight gain, URI, sinusitis
• In trials, women dropped out because of:- Foreign body sensation, coital problems, expulsion- Vaginal symptoms (discomfort, secretion)- Headache, emotional lability, weight gain
2/12/2018
17
A 35 year old woman has been using the combined contraceptive patch for the last year. She has been
following the 3 weeks on, 1 week off dosing as labeled. She comes in today stating that at the beginning of week 3 of the current cycle, she
realized her previous patch fell off, but she doesn’t know when. Has not had intercourse in the last
week. What should she do?
A. Apply a new patch immediately, use back-up for 7 days.
B. Apply a new patch immediately, use back-up for 7 days, skip placebo patch week and continue active patch
C. Apply a new patch immediately, no back-up is needed
D. Wait 1 week, use back-up, and then restart cycle
Pharmacists Prescribing Contraception
• Colorado, New Mexico, California- Via a state-wide protocol
• Oregon• Maryland, Hawaii recently passed legislation• New Hampshire has recommended passage• Possibly DC?
https://naspa.us/2017/05/pharmacists-authorized-prescribe-birth-control-states/
2/12/2018
18
Appropriate Triaging of Patients
Women who would best benefit from
LARC
Women with unexplained/unusual bleeding patterns on
contraceptives
Encourage appropriate
wellness/PAP guidelines
Active symptoms of VTE
Take Home Points
• For selection of appropriate hormonal contraception, CDC MEC will help determine appropriateness based on comorbidities
• Many side effects can be managed by switching between CHC’s
• Pharmacists will be prescribing contraceptives more widely….are you ready?