Asthma PED Thai CPG 2555
description
Transcript of Asthma PED Thai CPG 2555
-
5/22/2018 Asthma PED Thai CPG 2555
1/58
.. 2555
-
5/22/2018 Asthma PED Thai CPG 2555
2/58
100
(bronchial hyper-responsiveness)
(variable airow obstruction) (wheeze)
-
5/22/2018 Asthma PED Thai CPG 2555
3/58
101
1. Airway inammation 2. Structural changes in the airways (airway remodeling) 3. Bronchial hyper-responsiveness
4. Variable and partially reversible airway obstruction
/
1. ( ++)
1.1
1.2
-
5/22/2018 Asthma PED Thai CPG 2555
4/58
102
1.3 atopic dermatitis, allergicrhinitis
1.4
Cough-variant asthma peak expiratory ow bronchial hyper-
responsiveness
1.
2. 3. 4. 5. (> 10 ) 6.
2.
2.1 (wheeze)
-
5/22/2018 Asthma PED Thai CPG 2555
5/58
103
2.2 2.3
2.4 allergicrhinitis, allergic conjunctivitis atopic dermatitis
3.
3.1 ( +) 1) Spirometry 5 FEV1 FVC
- FEV1 12 % 200 . (pre and postbronchodilator) - FEV1/FVC ratio < 0.75
2) Peak expiratory ow (PEF) meter- PEF 20 % (pre and post bronchodilator)
- PEF variability > 20%
PEF variability = PEF max PEF min x 100%
1/2(PEF max + PEF min)
-
5/22/2018 Asthma PED Thai CPG 2555
6/58
104
3.2 1) allergy skin test, serum spe-cic IgE 2) bronchial hyperresponsiveness methacholine, histamine, mannitol, exercise challenge
test3) airway inammation non-invasive
sputum eosinophil, exhaled nitric oxide, exhaledcarbon monoxide
-
5/22/2018 Asthma PED Thai CPG 2555
7/58
105
3
Viral-induced Wheezing
-5 ----
Suggestive of Asthma
------Options: ( )
Pre-post bronchodilator PEFR FEV112%
- Skin test positive to aeroallergens
1
Therapeutic trial2-3 - ICS (Budesonide) 200 mcg - LTRA
gastroesophagealreflux, anatomical
anomaly,
immunodeficiency,
cows milk protein
allergy, etc.
-ICSLTRA- - ICS LTRA
1
-
5/22/2018 Asthma PED Thai CPG 2555
8/58
106
recurrent wheezing
1. Chronic rhinosinusitis 2. Gastroesophageal reux 3. Recurrent lower respiratory tract infections
4. Cows milk protein allergy 5. Congenital heart diseases 6. Bronchopulmonary dysplasia 7. Tuberculosis 8. Congenital malformation causing narrowing of the
intrathoracic airways 9. Foreign body aspiration 10. Immune deciency 11. Primary ciliary dyskinesia syndrome
12. Cystic brosis
-
5/22/2018 Asthma PED Thai CPG 2555
9/58
107
1. 2. 3. 4.
5. 6.
5 1.
2. 3. 4.
5.
-
5/22/2018 Asthma PED Thai CPG 2555
10/58
108
1.
( > 5 )
2.
(1)
-
5/22/2018 Asthma PED Thai CPG 2555
11/58
109
/
- 55-60 30
-
- () - -
- - -
- - ()
1 /
-
5/22/2018 Asthma PED Thai CPG 2555
12/58
110
/
- ( - ) -
- (pesticides)
(exterminator)
-
- - HEPA -
-
-
-
5/22/2018 Asthma PED Thai CPG 2555
13/58
111
/
-
-
-
-
- -
-
-
-
- short-acting beta 2 agonist long-acting beta 2 agonist 15-30
-
5/22/2018 Asthma PED Thai CPG 2555
14/58
112
/
-
(warm-up) 6-10
- food preservative
aspirin NSAIDs -
- beta-blockers
3.
(Assessing asthma control)
2 3
controlled, partly controlled uncontrolled
-
5/22/2018 Asthma PED Thai CPG 2555
15/58
113
2 (Levels of Asthma Control)
( 7)
2.1
( 4 )
Controlled Partly Controlled Uncontrolled() ( 1 )
( 2
partly controlled 3
(< 2 ) > 2 (reliever/rescue
treatment)
< 80% predicted (PEF or personal best ()FEV1) 1 1
-
5/22/2018 Asthma PED Thai CPG 2555
16/58
114
2.2 (
)
- - 1 *
- - FEV1- -
*
3.1 1) (Treating toachieve asthma control) 2) (Monitoring to maintain control)
3)
-
5/22/2018 Asthma PED Thai CPG 2555
17/58
115
1) (Treating toachieve asthma control) 2 3 1 5
(Reliever medications) (Rapid-acting 2-agonist,RABA) (con-
troller medications) RABA
uncontrolled partly controlled (step up) controlled controlled 3 (step down) () controlled
controlled 1
-
5/22/2018 Asthma PED Thai CPG 2555
18/58
116
persistentasthma 2 (2) 3
1 (Step 1: As-needed reliever medication)
inhaled RABA ( ++) con-
trolled 2 RABA 2 step up (2) inhaled RABA ( +) RABA short-actingtheophylline exercise-induced bronchospasm inhaled RABA bronchospasm leukotriene modier
(LTRA) cromone (sodium cromoglycate)
-
5/22/2018 Asthma PED Thai CPG 2555
19/58
117
2 (Step 2: Reliever medication )
inhaled corticoster-oid (ICS) 200-400 (low-mediumdose inhaled corticosteroid) ( ++) (3) leukotriene modier ( +)
ICS ICS sustained-release theophylline ( +)
cromone (sodi-um cromoglycate)
3 (Step 3: Reliever medication
) low-dose ICS (Long-acting 2-agonist, LABA) ( ++)
low-dose ICS 3-4 ICS uncontrolled
partly controlled
-
5/22/2018 Asthma PED Thai CPG 2555
20/58
118
formoterol LABA formoterol reliever controller ( +) < 5 3 ICS ( ++) MDI spacer
low-dose ICS LTRA ( +) low-dose ICS sustained-release theophylline ( +) 2
(< 5 )
4 (Step 4: Reliever medication )
4 ( +)
(dicult-to-treat asthma)
-
5/22/2018 Asthma PED Thai CPG 2555
21/58
119
medi-um-dose ICS LABA ( ++)
3 LTRA sustained-release theo-phylline high-doseICS LABA 3-6 corticosteroid ICS LTRA ICS
sustained-release theophylline ICS LABA
5 (Step 5: Reliever medication
step 4) 4
(uncontrolled) oral corti-costeroid step 4 corticosteroid anti-IgE al-lergic asthma 4 ( +)
-
5/22/2018 Asthma PED Thai CPG 2555
22/58
120
1 2 3 4 5
2-agonist
ICS* ICS* +
LABA
ICS* + LABA
Steroid
()LTRA ICS* + LTRA IgE
ICS* + LTRA + theophylline
ICS* +theophylline
* ICS = steroid
LABA = long-acting 2-agonist, 2-agonist
LTRA = leukotriene modier Theophylline = sustained-release theophylline
2 > 5
( 7)
-
5/22/2018 Asthma PED Thai CPG 2555
23/58
121
3
( 7)
*
ICS = inhaled corticosteroid
LTRA = leukotriene modifier
Theophylline = sustained-release theophylline
* = controlled** = partly controlled uncontrolled controlled 1
ICS
2 (3)ICS + LABA
ICS + LTRAICS + Theophylline (3 )
ICS50% 3
-LABA LTRA
Theophylline
-
ICS 50%3
ICS +LTRA +
Theophylline (4)
ICS 200-400 mcg/
LTRA (2)
3
ICS 50%3
1-3 3
***
*
*
**
***
**
(5)
-
5/22/2018 Asthma PED Thai CPG 2555
24/58
122
1.
2. 3. 4. allergic rhinitis, sinusitis, obesity,obstructive sleep apnea, gastroesophageal reux,
/ 5. 1-3 ()
6.
- ()
- () -
- - -
: (spirom-etry) 6-12
-
5/22/2018 Asthma PED Thai CPG 2555
25/58
123
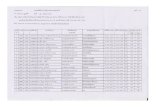
3 inhaled corticosteroids
(equivalent dose)
Drug Low Daily Dose
(mcg)
Medium Daily
Dose (mcg)
High Daily Dose
(mcg)
Beclomethasone dipropionate
- MDI (50, 100, 200, 250 mcg)
- DPI (Easyhaler; 200 mcg)
100 200 > 200 400 > 400
Budesonide*
- MDI (100, 200 mcg)
- DPI (Easyhaler, Turbuhaler; 100, 200 mcg)
- Nebulized solution (500, 1000 mcg)
100 200 > 200 400 > 400
Ciclesonide* #
- MDI (80, 160 mcg)
80 160 > 160 320 > 320
Fluticasone propionate
- MDI (50, 125, 250 mcg)
- DPI (Accuhaler; 100, 250 mcg)
- Nebulized solution (500, 2000 mcg)
100 200 > 200 500 > 500
Mometasone furoate* #
- DPI (220 mcg)
100 > 200 > 400
* #
-
5/22/2018 Asthma PED Thai CPG 2555
26/58
124
2) (Monitoring to maintain control)
1-3 3 controlled
4-6
step down
controlled
1. controlled ICS 3 50%
low-dose ICS 2. controlled ICS LABA ICS LTRA LABA LTRA ICS ICS 3 low-dose ICS
-
5/22/2018 Asthma PED Thai CPG 2555
27/58
125
3. controlled 1
step up
(Loss of control)
- - - -
- (Gastroesophageal reux) obstructive sleepapnea
1. RABA RABA 1-2
2. ICS formoterol
controlled
-
5/22/2018 Asthma PED Thai CPG 2555
28/58
126
3. low-medium dose ICS step up ICS LABA ICS ICS LTRA 4. (acute exacer-
bation) step up
3) 2
1. (Reliever) RABA LABA
2. (Controller)
-
5/22/2018 Asthma PED Thai CPG 2555
29/58
127
( 4) 2.1 Corticosteroids meditors cytokines 2-adrenergic receptors
corticosteroids 2
1) (Systemic form) corticosteroids
2) (Inhalation form)
(Persistent asthma) 2
ICS < 200 / ()
2.2 Leukotriene modier (LTRA) leukotriene leukot-riene receptor
mild persistent asthma low-dose ICS LTRA
(add-on) ICS
-
5/22/2018 Asthma PED Thai CPG 2555
30/58
128
LTRA viral inducedasthma exacerbation 2-5 intermit-tent asthma
2.3 Inhaled 2-agonist (Long-acting 2-agonist) 12
ICS (uncontrolled) medium-dose ICS 4
2.4 Sustained-release theophylline ICS drug interaction 10 ././
2
2.5 Anti-IgE (omalizumab) 6 IgE
-
5/22/2018 Asthma PED Thai CPG 2555
31/58
129
(IgE-mediated) ICS anti-IgE 6-60
(add-on therapy) anaphylacticreaction 2
-
5/22/2018 Asthma PED Thai CPG 2555
32/58
130
4
( 7)
-
5/22/2018 Asthma PED Thai CPG 2555
33/58
131
5
5
( 7)
< 4 MDI plus spacer Nebulizer with face mask with face mask4 - 6 MDI plus spacer Nebulizer with mouthpiece with mouthpiece
> 6 DPI MDI plus spacer Nebulizer with mouthpiece with mouthpiece
:
DPI accuhaler, easyhaler turbuhaler
Spacer corticosteroid spacer valve valve
spacer mouth piece
-
5/22/2018 Asthma PED Thai CPG 2555
34/58
132
Allergen immunotherapy
Allergen immunotherapy
1. 2. 3. 4.
4.
asthma exacerbation
66 asthma exacerbation
Mild Moderate Severe
Respiratory arrest
* 30 /
-
5/22/2018 Asthma PED Thai CPG 2555
35/58
133
Mild Moderate Severe
Respiratory arrest
paradoxical thoraco-
suprasternal abdominal
retraction movement
wheeze
wheeze
and expiratory (/) < 100 100-120 > 120
PEF > 80 % 60-80% > 60 %(% predicted
personal best) PaO2(on air) > 60 mmHg >60 mmHg(dyanosis)/ < 45 mmHg < 45 mmHg > 45 mmHg
PaCO2 SaO2% (on air) > 95% 91-95% < 90%
*
< 2 < 60 / 2 - 12 < 50 / 1 - 5 < 40 /
6 - 8 < 30 / **
2 - 12 < 160 / 1 - 2 < 120 /2 - 8 < 110 /
6 asthma exacerbation ()
-
5/22/2018 Asthma PED Thai CPG 2555
36/58
134
4.1 asthma exacerbation
1) asthma exacerbation (4)
4 asthma exacerbation
,
Inhaled RABA* 2-4 puffs/dose3 20
4PEF> 80% predicted personalbest-inhaled RABA2-4 puffs 3-4 . 24 - 48 .
PEF < 60%predicted personal best-inhaled RABA6-10 puffs 1-2 .
3 PEF 60-80% predictedpersonal best- inhaled RABA6-10 puffs 1-2.
1-2
* MDI with spacer DPI1
-
5/22/2018 Asthma PED Thai CPG 2555
37/58
135
(1) (2) inhaled RABA
(3) (4)
2) asthma exacerbation (5)
(1) SaO2> 95% nasal canula, mask head box
SaO2
(2) SIADH
-
5/22/2018 Asthma PED Thai CPG 2555
38/58
136
(3) 2-agonist nebulized RABA salbutamol respiratory solution
0.15 ././ ( salbutamol respules 2.5-5./, terbutaline respules 5 -10 ./) NSS 2.5-4 . oxygen ow 6-8 / MDI with spacer 2-4 puffs/ 20-30
10puffs/ 4-6 nebulized RABA an-ticholinergic (ipratropium bromide) 250 / (
20 .) 500 / (20 .) poor air entry systemic 2-agonist terbutaline continuous nebulized sys-
temic IV drip2-agonist monitor EKG, heart rate
hypokalemia
-
5/22/2018 Asthma PED Thai CPG 2555
39/58
137
5 asthma exacerbation
()
-
5/22/2018 Asthma PED Thai CPG 2555
40/58
138
(4) glucocorticosteroids 3-4
prednisolone 1-2 ././ 60 ./ 5-7 hydrocorti-sone 5 ././ 6 250 ./ methylprednisolone 1 ././
6 60./ hydrocortisone methylprednisolone systemic corticosteroid predni-solone 5-7 taper off steroid
nebulized ICS acute ex-acerbation (+/-) ICS ICS
(+/-) (5) - Epinephrine 1:1000 (adrenaline) 0.01 ./. 0.3 .
- RABA NB MDI - anaphylaxis angioedema
-
5/22/2018 Asthma PED Thai CPG 2555
41/58
139
- Aminophylline 5./. loading dose IV drip 1 ././. loading dose
5-15 ./. (6) -
- (mucolytic) -
- asthma exacerbation
3)
(1) (2) 1-3 (PEF < 70%predicted personal best oxygen saturation < 95%) (3) (high risk)
- near fatal asthma ventilator
-
5/22/2018 Asthma PED Thai CPG 2555
42/58
140
- - prednisolone - 2-agonists ( 1 ) -
4) -
- oxygen saturation / PEF - arterial blood gas - 2-agonist - - exacerbation prednisolone
7
-
5/22/2018 Asthma PED Thai CPG 2555
43/58
141
5)
5.1 5.2
5.3 5.4 (Action Plan)
5.5 1-6 PEF (Action
Plan)
1.
2.
-
5/22/2018 Asthma PED Thai CPG 2555
44/58
142
3.
(Action Plan)
: 1. ................................................................
2. .............................................
:
3
2
2
peak ow ............... L/min
3
1. ()...................... 2
.........(14)..........
2. 2 puffs 4-6
:
-
-
5/22/2018 Asthma PED Thai CPG 2555
45/58
143
-
- 4
1. ......................................2 4 puffs
2. prednisolone........................mg
3. ..........................................
............................................................................ 4.
* (Action Plan)
-
5/22/2018 Asthma PED Thai CPG 2555
46/58
144
1. 2. (dicult-to-treatasthma) 3. asthma with respiratory failure
4. inhaled corticosteroid prednisolone 5. / immunotherapy,
anti-IgE
5.
-
5/22/2018 Asthma PED Thai CPG 2555
47/58
145
perinatal mortality perinatal prognosis
theo-
phylline, ICS budesonide beta2-agonists, montelukast LTRA fetal anomalies ICS asthma exacerbation
acute exacerbation hypoxia nebulized SABA systemic glucocorticosteroids
-
5/22/2018 Asthma PED Thai CPG 2555
48/58
146
() ()
FEV1 80 gluco-
corticosteroids systemic glucocorticoster-oids 6 (hydrocortisone 1-2 ././, 100 . 8
) 24 systemic glucocorticosteroids
(allergic rhinitis)
-
5/22/2018 Asthma PED Thai CPG 2555
49/58
147
2 glucocorticosteroids, cromones, leu-kotriene modier anticholinergic intranasal steroid
leukotriene modi-ers, allergen-specic immunotherapy anti-IgE therapy 2
-
5/22/2018 Asthma PED Thai CPG 2555
50/58
148
rhinosinusitis 10
topical nasal decongestants topical nasal sys-temic steroids
(Nasal polyps)
aspirin hypersensitivity 40 36-96 aspirin intolerance nasal polyp 29-70 nasal polyp
nasal polyps cystic brosis
immotile cilia syndrome Nasal polyps topical steroids nasal polyps topical steroids
(Occupational asthma)
-
5/22/2018 Asthma PED Thai CPG 2555
51/58
149
Respirato-ry syncytial virus wheezing
Rhinovirus
wheezing Parainuenza, Inuenza, Adenovirus Coronavirus Mycoplasma wheezing , IgE antibody , mediators late asthmatic re-sponse
asthma exacerbation
-
5/22/2018 Asthma PED Thai CPG 2555
52/58
150
inhaled SABA glucocorticosteroid inhaled corticosteroid 4
anti-inammatory drug
(Gastroesophageal reux disorder)
3 hiatalhernia theophylline, 2-agonist
pH (lungfunction test) theophylline 2-agonist proton pump
inhibitor, H2-antagonist
-
5/22/2018 Asthma PED Thai CPG 2555
53/58
151
(subgroup)
esophagitis
Aspirin-induced asthma (AIA) 28 asthma exacerbation aspirin NSAIDs severe asthma 30-40 vasomotorrhinitis nasal polyps asthma hypersensitivity aspirin
1 2 aspirin asthmatic attack
-
5/22/2018 Asthma PED Thai CPG 2555
54/58
152
aspirin COX-1 inhibitor dose bronchospasm respi-ratory arrest
markedeosinophilic inammation, epithelial disruption cy-tokines IL-5 adhesion molecules 70 genetic polymorphism LTC4 synthase gene aspirin bronchoconstriction
NSAIDs
aspirin challenge test
FEV1 70 predicted personal best bronchial nasal challenge lysine as-pirin oral challenge AIA aspirin
-
5/22/2018 Asthma PED Thai CPG 2555
55/58
153
COX-1 inhibitor progression inammation hydrocortisone hemisuccinate COX-2 inhibitor 1 asthma AIA ICS leukot-riene modier additional treatment
NSAIDs desensitization desensitization lower respiratory
tract desensitization aspirin 600-1,200 . adult onset nasal polyposis
NSAIDs paracetamol
Anaphylaxis Anaphylaxis acute wheezing
(biological substances)
-
5/22/2018 Asthma PED Thai CPG 2555
56/58
154
exercise-induced anaphylaxis exercise-inducedbronchoconstriction anaphylaxis 2-agonist epinephrine anaphylaxis
3 1. (primary prevention)
1.1 (prenatal prevention)
wheezing illness
-
5/22/2018 Asthma PED Thai CPG 2555
57/58
155
1.2 (postnatal prevention) 1)
46 (AAP 2008) (partially or extensively hy-
drolysated formula) (solid foods) 4-6
2) prenatal 3) RSV bronchiolitis
2. (secondary prevention) allergic sen-
sitization second generation H1-antihistamine
allergen immunotherapy
-
5/22/2018 Asthma PED Thai CPG 2555
58/58
156
3. (tertiary prevention)
(1)