T IMPACT OF THE W H O FLANDERS A CASE S WHO’ N F · THE IMPACT OF THE WORLD HEALTH ORGANIZATION...
Transcript of T IMPACT OF THE W H O FLANDERS A CASE S WHO’ N F · THE IMPACT OF THE WORLD HEALTH ORGANIZATION...

PAPER NR. 34, FEBRUARY 2016
THE IMPACT OF THE WORLD HEALTH ORGANIZATION IN
FLANDERS: A CASE STUDY OF THE WHO’S NORMATIVE
FUNCTION
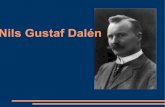
Nils Vanstappen
Jan Wouters
www.globalgovernancestudies.eu www.steunpuntiv.eu

2
THE IMPACT OF THE WORLD HEALTH ORGANIZATION IN FLANDERS: A CASE STUDY OF THE WHO’S NORMATIVE
FUNCTION
Nils Vanstappen Jan Wouters
Abstract
The World Health Organization (WHO) fulfils several important functions within the global (public) health system. One of its central functions is a normative one: the WHO provides technical and normative guidance on all matters of (public) health that are of global concern. Although it has received a strong mandate in its constitutive instrument to adopt binding instruments, the WHO has consciously opted for a soft law approach, preferring (non-binding) guidelines and recommendations over (binding) conventions and regulations. In the development of these guidelines, (technical) experts play a central role.
In the light of the choice of the WHO for non-traditional mechanisms of international law-making, the objective of this report is to study how the WHO is impactful in Flanders in the exercise of its normative function. We consider both binding and non-binding instruments, as both serve the exercise of the normative function. In terms of methodology, this report and its results are based on a document analysis and a limited set of interviews.
We start with a discussion of (1) the institutional characteristics of the WHO, including the actors involved and the relevant bodies and their decision-making procedures. Thereafter, we discuss (2) the binding instruments (conventions and regulations) which the WHO has adopted. With regard to the International Health Regulations, the case of the Ebola crisis will be touched upon to show the relevance in practice of these regulations. Then, the research will turn to (3) the non-binding instruments adopted by the WHO. First, we discuss recently developed mechanisms to streamline the process of guideline development, namely the Guideline Review Committee and the Guideline Development Handbook. Thereafter, we study different guidelines as case studies to distinguish some of the characteristics of these guidelines. Finally, (4) our conclusion is based on the distinction between rule-makers, where we explain how the WHO exercises its normative function, and rule-takers, where we outline how these norms are impactful in Flanders.
Key words
Public international law, sources of law, soft law, non-traditional international law-making, World Health Organization, guidelines, recommendations, normative function.

3
AUTHORS Nils Vanstappen is a researcher and PhD student at the Leuven Centre for Global Governance Studies (KU Leuven). Jan Wouters is Jean Monnet Chair ad personam EU and Global Governance, Full Professor of International Law and International Organizations and Director of the Leuven Centre for Global Governance Studies and the Institute for International Law (KU Leuven). © 2016 by Nils Vanstappen and Jan Wouters. All rights reserved. No portion of this report may be reproduced without permission of the authors. Working papers are research materials circulated by their authors for purposes of information and critical discussion. They have not necessarily undergone formal peer review.
ACKNOWLEDGMENTS The authors would like to express their gratitude towards Axel Marx, Sanderijn Duquet and Philip De Man for useful comments on earlier drafts of this report. Additionally, we would like to thank the interviewees for the practical insights they provided which contributed to our final result. Finally, we would like to thank all those who have helped and supported us in the writing of this report. All errors and omissions remain, of course, our own.
NOTE Het onderzoek dat aan de basis ligt van dit rapport kadert in het programma ‘Steunpunten voor Beleidsrelevant Onderzoek’ dat gefinancierd wordt door de Vlaamse Overheid. Wij danken de Vlaamse Overheid voor de financiële steun en interesse in het onderzoek.

4
SAMENVATTING
De Wereldgezondheidsorganisatie (WHO) speelt een centrale rol in het internationaal
gezondheidssysteem. De organisatie vervult verschillende functies binnen dit systeem,
waaronder administratieve, coördinerende, enz. In dit rapport gaan we dieper in op de
normatieve functie van de WHO, die erin bestaat technische en normatieve standaarden en
aanbevelingen uit te vaardigen. We gaan na op welke manier de WHO in de uitoefening van
deze functie een impact heeft in Vlaanderen. In een eerste deel bespreken we de actoren die
deelnemen aan de besluitvorming in de WHO, evenals de institutionele kenmerken van deze
organisatie, met aandacht voor de belangrijke rol van experten en de grote mate van
regionalisering. Vervolgens wordt een onderscheid gemaakt tussen bindende en niet-
bindende normen. Wat betreft bindende normen, worden zowel het enige verdrag dat ooit is
aangenomen door de WHO, het Kaderverdrag voor Tabaksbestrijding, als de beide
reglementen die deze organisatie heeft uitgevaardigd, het Internationaal
Gezondheidsreglement en het Nomenclatuurreglement, bediscussieerd. Bij de bespreking van
het Internationaal Gezondheidsreglement wordt bovendien dieper ingegaan op de recente
Ebola-crisis in West-Afrika, aangezien het reglement het kader vormde voor de respons van
de organisatie op deze crisis. Vooraleer enkele niet-bindende normen te bespreken – een
overzicht van alle niet-bindende normen is praktisch onhaalbaar – gaan we dieper in op de
procedure voor het ontwikkelen van dergelijke normen, met speciale aandacht voor het Comité
ter Controle van de Richtlijnen (Guideline Review Committee). Vervolgens kijken we naar een
beperkte selectie van richtlijnen. Een eerste richtlijn (de “suikerrichtlijn”) werd geselecteerd om
aan te tonen hoe de WHO een impact kan hebben op beleidsmakers. Bij de bespreking van
de tweede richtlijn (de richtlijn met betrekking tot handhygiëne) wordt aangegeven hoe de
WHO direct impact kan hebben op private actoren (zonder interventie van een nationaal of
regionaal implementerend beleidsniveau). Tot slot bespreken we het proces van het
ontwikkelen van een farmaceutisch product en de verschillende WHO-richtlijnen die op een
dergelijk proces van toepassing zijn. Hiermee willen we wijzen op de enorme hoeveelheid en
verscheidenheid aan bestaande WHO-richtlijnen. De conclusie is gestructureerd rond de
concepten van regelmaker (“rule-maker”) en regelnemer (“rule-taker”) met als doel enerzijds
inzicht te verschaffen in hoe regels gemaakt worden bij de WHO en anderzijds hoe deze regels
toepassing vinden in de Vlaamse context. Aan de kant van de regelmaker stellen we vast dat
(1) de WHO vaak kiest voor niet-bindende normen in de uitoefening van haar normatieve
functie; (2) een belangrijke rol wordt gespeeld door experten in het ontwerpen van de WHO’s
normen; (3) de WHO niet alleen technische richtlijnen uitvaardigt, maar ook durft optreden als
normatieve actor of als tegengewicht tegen multinationale industriële belangen; en (4) de WHO
steeds meer concurrentie krijgt in het mondiale gezondheidsnetwerk aangezien andere
actoren ontstaan of aan belang winnen. Aan de andere kant, die van de regelnemer, stellen
we vast dat (1) implementatie op het beleidsniveau gecompliceerd is door de Vlaamse
institutionele context, waarin Vlaanderen niet alleen bevoegdheden moet delen met het
federale niveau, maar ook met het Europese niveau; (2) de normen van de WHO niet bindend
hoeven te zijn om een impact te hebben in Vlaanderen; en (3) verschillende normen van de
WHO rechtstreeks gericht zijn op – en ook rechtstreeks impact hebben op – private actoren,
en dat de WHO private actoren ook aanmoedigt om rechtstreeks naar haar normen terug te
grijpen.

5
Executive summary
Since its establishment in 1946, the World Health Organization (WHO) has occupied a
prominent role in the international public health system. In addition to important coordinative
and administrative functions, it has been delegated a significant normative function. In other
words, it was expected to adopt rules and norms in all matters related to public health. In this
report, we consider the impact the WHO has in Flanders in the exercise of this normative
function.
Institutionally, the WHO is structured like most international organizations, with a body
grouping delegations from all Member States (the World Health Assembly or WHA), a body
with a more limited, rotating membership which has a more executive role (the Executive Board
or EB), and a Secretariat providing administrative support (headed by the Director-General or
D-G). When it comes to membership, it can be considered a traditional international
organization, as statehood is a central criterion. Federal states are allowed only one delegation
and Flanders is thus represented by (and in) the Belgian delegation to the WHO. Moreover,
membership has remained off limits to the EU. Nevertheless, it maintains a close partnership
with the WHO on issues of public health. In other regards, the WHO is rather unique. Firstly,
although all international organizations rely on technical experts to some extent, the WHO has
granted these experts a central role in the exercise of its normative function, whereas this role
is normally occupied by representatives from Member States. Secondly, the WHO has a
strongly regionalized structure, as it has six regional offices with their own structures (including
a Regional Director) and a large degree of autonomy.
For the exercise of its normative function, the WHO has received extensive powers to adopt
binding instruments, either in the form of conventions (article 19 WHO Constitution) or in the
form of regulations (article 22 WHO Constitution). Nevertheless, it has only made very limited
use of these powers. The Framework Convention on Tobacco Control, which was modelled
after earlier environmental framework conventions, was the first and only time the WHO made
use of its powers to develop conventions. Spurred by the ambition to counter the tobacco
industry’s strong opposition to national anti-tobacco legislation, this convention requires
Member States to adopt certain measures to reduce tobacco consumption. It has also provided
for an institutional machinery to help Member States with the implementation, both through
precision of the convention’s provisions, and through offering aid in countering industry tactics.
On the basis of article 22 WHO Constitution, only two regulations have been adopted: the
International Health Regulations and the Nomenclature Regulations. The first set of regulations
– together with the recently developed Emergency Response Framework – provide the legal
framework for the WHO’s action in case of health emergencies (both epidemics and other
emergencies with a public health dimension). This framework has been harshly challenged in
the follow-up of the Ebola crisis, mostly because of the WHO’s inability to swiftly and correctly
coordinate the response. The Nomenclature Regulations provide a bare framework for the
WHO’s classification systems, which allow for the comparison of data worldwide (on, for
example, causes of death).
In contrast with the limited amount of binding instruments adopted by the WHO, the
organization has been quite prolific in the adoption of non-binding norms, in different forms
(e.g. global strategies, plans of action, programmes, etc.). Undoubtedly the most important
instruments are “guidelines” which are developed by technical experts in accordance with the
Guideline Development Handbook, and reviewed by the Guideline Review Committee,
established in 2008. These guidelines cover practically every field of public health issues. In
this paper, we have discussed only a limited selection of these guidelines, in an attempt to

6
identify some common features of (but also show some differences between) WHO guidelines.
The Guidelines on Sugar Intake for Adults and Children, adopted in 2015, provide a benchmark
for policies on this subject-matter, and will thus have clear impact on policy-makers. The
Guidelines on Hand Hygiene in Health Care, adopted in 2009, demonstrated the WHO’s
capacity to ensure the accessibility of their guidelines for private actors directly, which makes
implementation by policy-makers unnecessary. Our discussion of guidelines affecting the
process of developing pharmaceutical products highlighted the immensity of public health
subject-matters covered (in some detail) by WHO guidelines. It also revealed the importance
of the EU in moderating between the WHO level and the (sub-)national level, both in the
development and the implementation of norms.
Our concluding remarks are subdivided in thoughts about rule-makers (how the rules are
made) and rule-takers (how rules are implemented). On the rule-maker side, we observed (1)
the WHO’s clear and conscious choice for non-binding instruments to exercise its normative
function; (2) its clear reliance on technical expertise as a basis for its legitimacy (although we
also marked an increasing attempt to draw legitimacy from stakeholder involvement); (3) the
different roles which the WHO fulfils, which consist not only of providing technical guidance (in
the form of guidelines), but also of a more normative role (e.g. promoting more investment in
therapies for diseases prevalent in developing countries); and (4) the growing network of actors
engaged in global health governance, in which the WHO is manoeuvring in an attempt to
maintain its leader position. On the rule-taker side, we referred (1) to the complexity of the
Flemish context, which not only involves a federal state, but equally the European context.
This complexity can give raise to coordination issues hindering the successful implementation
of WHO norms. We also discussed (2) the different ways for the WHO’s instruments to have
impact in Flanders. While a limited number of norms are directly binding, some instruments
have become binding through other means (e.g. transplantation into EU directives or
regulations). Other instruments, although not legally binding, can still have an impact on
Flemish policy-makers, e.g. by providing a benchmark for developing policy proposals,
supporting certain policy choices. Finally, (3) WHO guidelines often also directly affect private
actors, which can, for example, occur because they provide the state-of-the-art in medical
research, which doctors can use in medical procedures, or they are taken over in private
certification schemes. Indeed, even in the absence of binding force, WHO guidelines often find
their way into practice somehow.

7
Table of contents
Executive summary ............................................................................................................... 5
Table of contents ................................................................................................................... 7
List of abbreviations .............................................................................................................. 9
Introduction ..........................................................................................................................12
1. Background ...................................................................................................................17
1.1 Introduction ............................................................................................................17
1.2 Actors .....................................................................................................................18
1.2.1 Membership ..........................................................................................................18
1.2.2 Other participants .................................................................................................20
1.2.3 Involvement of experts .........................................................................................21
1.3 Institutional structure ..............................................................................................23
1.3.1 The three levels and federalism ......................................................................23
1.3.2 The structure of headquarters .........................................................................24
1.3.3 The structure of the European regional level ...................................................27
1.4 Reforming the WHO ...............................................................................................28
2. Legally binding instruments ...........................................................................................31
2.1 The law-making powers of the WHO ......................................................................31
2.2 The treaty-making powers of the WHO: article 19 of the WHO constitution ............32
2.2.1 The Framework Convention on Tobacco Control ............................................32
2.2.2 Proposals for other conventions ......................................................................36
2.3 The International Health Regulations and the role of the WHO in public health
emergencies .....................................................................................................................38
2.3.1 The role of the WHO in health emergencies ....................................................38
2.3.2 The International Health Regulations ..............................................................40
2.3.3 The Ebola Virus Disease (EVD) outbreak ........................................................43
2.3.4 Impact in Flanders ...........................................................................................48
2.3.5 Reform of the WHO’s health emergency response system..............................51
2.4 Nomenclature regulations.......................................................................................52
3. Legally non-binding instruments ....................................................................................55
3.1 Recommendations and guidelines ..........................................................................55
3.1.1 The difference .................................................................................................55
3.1.2 New rules for guideline development ...............................................................57
3.2 Impact on policy-makers.........................................................................................59
3.2.1 Introduction .....................................................................................................59

8
3.2.2 Translating the Global Strategy on Diet, Physical Activity and Health into
“gezondheidsdoelstellingen rond Voeding & Beweging 2015-2021” ..............................60
3.2.3 An example: the guideline on sugar intake for adults and children ..................62
3.3 Impact on private actors .........................................................................................66
3.3.1 Introduction .....................................................................................................66
3.3.2 Impact on health-care providers and hospital managers: hygiene guidelines ..67
3.4 The development of pharmaceutical products .............................................................68
3.4.1 A broad approach: development phases of pharmaceutical products ...................68
3.4.2 The R&D phase: steering R&D and clinical trials ..................................................71
3.4.3 Registration of the pharmaceutical product and intellectual property rights ...........74
3.4.4 Manufacturing and distribution ..............................................................................76
4. The impact of the WHO in Flanders...............................................................................80
4.1 Rule-maker ............................................................................................................80
4.1.1 The WHO’s choice for soft law ..............................................................................80
4.1.2 WHO as an expert organization ............................................................................81
4.1.3 The WHO’s multiple roles .....................................................................................82
4.1.4 The global health network .....................................................................................84
4.2 The multi-layered and complex nature of the rule-taker ..........................................86
4.2.1 Implementation in a multi-layered and complex context ..................................86
4.2.2 Different ways and levels of impact ......................................................................86
4.2.3 Impact on private actors directly ...........................................................................87
Annexes ...............................................................................................................................89
Annex I: Organigram of the WHO .....................................................................................89
Annex II: The core functions of the WHO ..........................................................................90
Annex III: Dietary guideline development process .............................................................91

9
List of abbreviations
ATC Anatomical Therapeutic Chemical
CDC Centres for Disease Control
CEFS Comité Européen des Fabricants de Sucre
CHMP Committee for Medicinal Products for Human Use
COP Conference of the Parties
CSI Civil Society Initiative
CTG Commissie Tegemoetkoming Geneesmiddelen
DG Sanco Directorate-General for Health and Food Safety
D-G Director-General
EB Executive Board
ECDC European Centre for Disease Control
EEA European Economic Area
EFPIA European Federation of Pharmaceutical Industries Associations
EMA European Medicines Agency
EMP Essential Medicines and Health Products
EphMRA European Pharmaceutical Market Research Alliance
ERF Emergency Response Framework
EU European Union
EVD Ebola Virus Disease
FAGG Federaal Agentschap voor Geneesmiddelen en Gezondheidsproducten
FAO Food and Agricultural Organization
FCTC Framework Convention on Tobacco Control
G20 Group of 20
GDP Good distribution practices
GINA Global Database on the Implementation of Nutrition Action
GMP Good manufacturing practices
GOARN Global Outbreak Alert and Response Network
GPW Global Programme of Work
GRC Guideline Review Committee
GSPA-PHI Global Strategy and Plan of Action on Public Health, Innovation and
Intellectual Property
HCAI Health care-associated infections
HEPA Europe European Network for the Promotion of Health-Enhancing Physical
Activity

10
HIS Cluster of Health Systems and Innovation
IASC Inter-Agency Standing Committee
IATA International Air Transport Association
ICD International Classification of Diseases
ICDRA International Conference of Drug Regulatory Authorities
ICF International Classification of Functioning, Disability and Health
ICH International Conference for the Harmonisation of Technical
Requirements for Registration of Pharmaceuticals for Human Use
ICHI International Classification of Health Interventions
ICMJE International Committee of Medical Journal Editors
IFPMA International Federation of Pharmaceutical Manufacturers and
Associations
IHR International Health Regulations
INN International Non-proprietary Name
IPR Intellectual property right
LNHO League of Nations Health Office
NCD Non-communicable disease
NGO Non-governmental organization
NHD Department of Nutrition for Health and Development
NUGAG Nutrition Guidance Expert Advisory Group
OIHP International Office of Public Health
PAHO Pan American Health Organization
PHEIC Public Health Emergency of International Concern
PPRI Pharmaceutical Pricing and Reimbursement Information
RHN Regions for Health Network
SCRC Standing Committee of the Regional Committee
SSFFC Substandard, spurious, falsely labelled, falsified and/or counterfeit
(pharmaceutical products)
TFEU Treaty on the Functioning of the European Union
UN United Nations
UNFCCC United Nations Framework Convention on Climate Change
UNMEER United Nations Mission for Ebola Emergency Response
WHA World Health Assembly
WHO World Health Organization
WHO-FIC World Health Organization Family of International Classifications
WHO ICTRP World Health Organization International Clinical Trials Registry Platform

11
WIPO World Intellectual Property Organization
WIV-ISP Wetenschappelijk Instituut voor Volksgezondheid
WTO World Trade Organization

12
Introduction
This report forms part of a series of reports and papers which aims to better understand forms
of ‘non-traditional international law-making’1 and their legal and policy consequences for sub-
national regional authorities, in casu the government of Flanders. These reports and papers
have been written as part of one of the research trajectories of the Flemish Policy Research
Centre on "Foreign Affairs, International Entrepreneurship and Development Cooperation".2 In
a first phase of this research trajectory, a theoretical and conceptual framework for non-
traditional international law-making was developed, which inter alia provided an overview of
the different relevant legal schools.3 The second major phase of this research trajectory
involved the comparison of six case studies of instances where non-traditional international
law was produced.4 In this final report, we intend to deepen the study of one of these case
studies, namely the World Health Organization. This case study has been selected after
consultation with the Flemish government’s representatives.
The main objective of this report is to assess how (and, where possible, to what extent) the
World Health Organization (hereinafter: WHO) is impactful in Flanders in the exercise of its
normative function. It will attempt to make connections between the WHO’s initiatives and
actions on the one hand and domestic policies and situations on the other. However, it will
generally prove difficult to establish a causal link between both; it is often unclear how great a
role should be attributed to one factor (in casu the WHO’s initiatives and actions) to change of
policy or circumstance. Where evidence is available on the relationship between the WHO and
concrete changes in Flanders, this will be presented. Otherwise, we will limit ourselves to
describing the different ways in which the WHO has impact in Flanders without specifying how
important this impact has been.
Two short notes on one of the main elements of this study, “Flanders”, is in order. Traditionally,
international law has been solely concerned with the relationship between States, excluding
intra-state affairs and nationals of States. However, because of the non-traditional international
law framework in which this report is framed, we will not limit ourselves to the impact of the
WHO on the Flemish governmental level.5 Indeed, earlier reports in this research trajectory
have suggested that a central element of non-traditional international law-making might be that
no implementation of international regulation is required by national or sub-national
1 We chose this general term to include different theoretical approaches that all refer to similar and largely overlapping phenomena, inter alia: Informal International Law-making (IN-LAW), Global Administrative Law (GAL), International Public Authority, and Transnational Private Regulation. For an overview see Sanderijn Duquet and Jan Wouters, ‘Non-Traditional Norms in International Law: Approaches in Legal Scholarship’ (2014) 5 Czech Yearbook of Public and Private International Law 3. 2 The website of this research project can be found at https://ghum.kuleuven.be/ggs/projects/policy-research-centre. 3 This report is available at https://ghum.kuleuven.be/ggs/projects/policy-research-centre/documents-1/11-duquet-wouters.pdf. It has also been published in the Czech Yearbook of Public and Private International Law. See Duquet and Wouters (n 1). 4 Nils Vanstappen and others, ‘International Informal Law-Making. A Comparative Case Analysis Across Policy Areas’ (Steunpunt Internationaal Vlaanderen 2014) <https://ghum.kuleuven.be/ggs/projects/policy-research-centre/documents-1/23-vanstappen-p1-comparative-report-informal-law.pdf>.This report is available on the website of the policy research centre at https://ghum.kuleuven.be/ggs/projects/policy-research-centre/documents-1/23-vanstappen-p1-comparative-report-informal-law.pdf. 5 The institutional context will be sketched in section 1.

13
governments, but that private actors in the domestic setting are directly affected by the
regulatory (or other) action.6 Skipping the domestic implementation phase is, however, no
condition sine qua non for regulative action to be considered non-traditional. Therefore, both
impact at the level of policy-making (which thus requires further implementation) and impact
on private actors directly will be discussed in this report.
Secondly, referring to “Flanders” or “the Flemish government” might require some clarification
in institutional legal terms. The Flemish government represents two legally separate sub-
national entities within the Belgian state, which are the Flemish Community and the Flemish
Region. For the purpose of this report, the Flemish Community will be the most important entity,
as it is the sub-national entity responsible for matters of public health.7 However, the Flemish
Region also holds some relevant competences. One can, for example, refer to their
competence in the field of environment.8 In practice, the distinction is less relevant as the
Flemish Parliament and Government represent both the Flemish Community and the Flemish
Region.9 In addition, the Belgian federal state still retains10 some relevant competences as
well, for example in the field of pharmaceutical products (see infra). Finally, some competences
are shared with or exclusively exercised by the European Union (and/or its decentralised
agencies, such as the European Medicines Agency, EMA). In all, this paints a complex, multi-
layered institutional picture. In what follows, while the focus will remain on the Flemish
government, both as representative of the Flemish Community and Flemish Region, we will
also try to present the broader institutional context in which the Flemish government operates
in the different case studies.
The WHO has influenced domestic policies and situations in distinct manners. Even at a very
basic level, the WHO has shaped our conception of “health”, which is defined in the preamble
of its Constitution11 as “a state of complete physical, mental and social well-being and not
merely the absence of disease or infirmity”.12 Indeed, one author states that “WHO’s most
valuable influence is probably in the imperceptible shifts it causes in people’s thinking—away
from doctors and nurses in hospitals towards primary health care and traditional birth
attendants, from drugs to safe water, from health service to intersectoral health promotion.”13
This broad thinking about health is, for example, reflected in the work of the WHO on social
6 Vanstappen and others (n 4). 7 Article 5, §1, I of the Special Law for the Reform of the Institutions (Bijzondere Wet tot Hervorming der Instellingen) of 8 August 1980 (hereinafter BWHI) grants the Flemish Community several competences with regard to public health policy (“gezondheidsbeleid”). 8 See article 6, §1, II BWHI. 9 Due to the different relationship with the territory of the Brussels Capital Region, there are, however, (limited) differences in terms of decision-making procedure and territorial scope of application of legal instruments. Although we acknowledge these differences here, they will not play a role in the rest of the discussion. 10 We use the verb “to retain” since Belgian federalism is historically centrifugal, which means that the evolution has been to devolve competences from the former unitary state to the “new” sub-national entities. See X, “The Federal System of Belgium”, available at http://www.diplomatie.be/rabat/media/rabat/NoteFedSystem.pdf. 11 Constitution of the World Health Organization of 22 July 1946, 14 UNTS 185. Available at http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?ua=1. 12 Machteld Huber and others, ‘How Should We Define Health?’ (2011) 343 BMJ 4163; Norman Sartorius, ‘The Meanings of Health and Its Promotion’ (2006) 47 Croatian medical journal 662; Gian Luca Burci and Claude-Henri Vignes, ‘World Health Organization’, International Encyclopedia of Law: Intergovernmental Organizations, vol 14 (2003) 107–113. 13 Jill Turner, ‘For WHO or for Whom?’ (1997) 349 The Lancet 1639, 1640.

14
determinants for health14 and the relationship between health and a healthy climate.15
Moreover, in promoting this shift of thinking, it has not only had an impact on Member States,
but also on other international actors, such as the European Union16.17
Besides promoting a shift in people’s way of thinking about “health”, the WHO has impacted
upon domestic policies and actors in other, more concrete ways. Getting a complete picture of
the WHO’s impact is, unfortunately, impossible due to the great diversity of ways in which the
WHO has influence. This diversity is due to several factors. Firstly, the WHO exercises different
functions in relation to global health governance.18 It does not only act as a standard-setter
and rule-developer, but it is also the main coordinator of international responses to global
public health emergencies, in particular global epidemics. In addition, it acts as an important
repository for the collection of health data (for which it promotes standardized reporting
schemes19) and provides technical assistance (for example in the form of the training of
medical staff). An overview is provided in Annex II. Another factor contributing to the diversity
of the WHO’s impact rests in the fact that the end-users or target public of WHO (regulatory)
actions include both policy-makers (governments, parliaments, and administrations) and
private actors (e.g. patients, medical staff, health-care providers, hospital managers, etc.).20
14 See WHO, ‘Social determinants for health’, available at http://www.who.int/social_determinants/en/. According to the 12th Global Programme of Work, “the concept of social determinants of health constitutes an approach and a way of thinking about health that requires explicit recognition of the wide range of social, economic and other determinants associated with ill health, as well as with inequitable health outcomes.” See WHO, ‘Twelfth Global Programme of Work: Not Merely The Absence of Disease’ (2014), available at http://apps.who.int/iris/bitstream/10665/112792/1/GPW_2014-2019_eng.pdf?ua=1, 35. The scope of WHO action has not always been this broad. A major change occurred with the adoption of the Health for All Strategy through the Declaration of Alma-Ata. In this regard, Taylor states that “prior to the Declaration of Alma-Ata, most of WHO’s endeavors were confined to the traditional activities of early international public health agencies.” See Allyn Lise Taylor, ‘Making the World Health Organization Work: A Legal Framework for Universal Access to the Conditions for Health’ (1992) 18 American Journal of Law and Medicine 301, 316. 15 Maria Neira, ‘The 2014 WHO Conference on Health and Climate’ (2014) 92 Bulletin of the World Health Organization 546; Gary Humphreys, ‘Reframing Climate Change as a Health Issue’ (2014) 92 Bulletin of the World Health Organization 551; Alistair Woodward, ‘Climate Change and Health: Recent Progress’ (2014) 92 Bulletin of the World Health Organization 774. This is further evidenced by the ‘call to action’ directed towards those participating in the Paris COP on climate change. See http://www.who.int/globalchange/global-campaign/call-for-action/en/. 16 See, for example, Council Conclusion on the EU role in Global Health (10 May 2010), available at http://www.consilium.europa.eu/uedocs/cms_Data/docs/pressdata/EN/foraff/114352.pdf and Council Conclusions on Equity and Health in All Policies: Solidarity in Health (8 June 2010), available at http://www.consilium.europa.eu/uedocs/cms_data/docs/pressdata/en/lsa/114994.pdf. 17 According to Taylor, “the primary health care paradigm has influenced the structure of health service delivery provided by other international bilateral and non-governmental organizations.” Taylor, ‘Making the World Health Organization Work’ (n 14) 320. 18 The functions granted to the WHO are listed in article 2 of its Constitution. Given the fact that article 2 mentions no less than 22 functions, several of which overlap, there have been several efforts to develop a clear categorization of its functions. See infra 1.1. See inter alia Burci and Vignes (n 12) 119–123. The WHO outlines six functions on its website: (1) providing leadership on matters critical to health and engaging in partnerships where joint action is needed; (2) shaping the research agenda and stimulating the generation, translation and dissemination of valuable knowledge; (3) setting norms and standards and promoting and monitoring their implementation; (4) articulating ethical and evidence-based policy options; (5) providing technical support, catalysing change, and building sustainable institutional capacity; and (6) monitoring the health situation and assessing health trends. See http://www.who.int/about/what-we-do/en/. 19 See section 2.4. 20 The end-users of WHO guidelines, for example, can be “public health policy-makers, health programme managers, health-care providers, patients, caregivers”, etc. See World Health Organization,

15
Thirdly, the WHO covers a wide array of topics, ranging from various traditional public health
topics (such as vaccinations and epidemics) to more loosely related topics (such as a healthy
living environment as well as diet and physical activity), which should come as no surprise
given the broad conception of health it promotes. Finally, several other factors can be
discussed, such as the differing degrees of collaboration with external partners (e.g. with
UNICEF in the development of the Child Growth Charts), the level of involvement of the
different organs of the WHO (e.g. whether the World Health Assembly has endorsed a certain
guideline or recommendation)21, etc.
As our general research framework concerns non-traditional international law-making, this
working paper will mainly consider the impact flowing from the WHO exercising its normative
function, i.e. developing binding (conventions or regulations) or non-binding (recommendations
or guidelines) instruments.22 Where relevant for the discussion at hand, the impact from its
other functions will shortly be touched upon in the course of the paper. While it is possible to
be rather comprehensive in discussing the binding instruments elaborated and adopted by the
WHO, the amount and diversity of non-binding instruments produced by the WHO is such that
any attempt at completeness would be defeated from the outset. Therefore, we have rather
opted to work on the basis of case studies in these instances. These case studies have been
thusly selected to account for the diversity of instruments produced by the WHO.
The research objectives and limitations described above have resulted in the following
structure. We start by discussing the competence of the WHO to elaborate legally binding
instruments. A distinction is made between binding instruments adopted under article 19 of the
WHO Constitution (“conventions” or “agreements”) and article 21 of the WHO Constitution
(“regulations”). As of yet, the WHO has only adopted one instrument on the basis of article 19,
which is the Framework Convention on Tobacco Control (hereinafter FCTC). Under article 21
of the WHO Constitution, the WHO has adopted two types of regulations: the Nomenclature
Regulations and the International Health Regulations (hereinafter IHR). Both will be discussed
separately with most attention being devoted to the IHR. In discussing the IHR, we will also
touch more generally upon the role of the WHO in combatting global health emergencies (such
WHO Handbook for Guideline Development (2014) 2 <http://apps.who.int/iris/bitstream/10665/145714/1/9789241548960_eng.pdf> accessed 13 February 2015. 21 Burci and Vignes (n 12) 142. 22 For a discussion of the term non-traditional law-making, see the earlier reports of this research trajectory referred to in footnotes 3 and 4. The IN-LAW project played an important role in shaping our conceptions. For this project, see Joost Pauwelyn, Ramses A Wessel and Jan Wouters (eds), Informal International Lawmaking (Oxford University Press 2012); Joost Pauwelyn, Ramses A Wessel, Jan Wouters, Ayelet Berman and Sanderijn Duquet (eds), Informal International Lawmaking: Case Studies (Torkel Opsahl Academic EPublisher (TOAEP) 2013); Joost Pauwelyn, Ramses A Wessel and Jan Wouters, ‘Informal International Law as Presumptive Law: Exploring New Modes of Law-Making’ in Rain Liivoja and Jarna Peterman (eds), International Law-Making: Essays in Honour of Jan Klabbers (Routledge 2013); Sanderijn Duquet, Joost Pauwelyn, Ramses A Wessel and Jan Wouters, ‘Upholding the Rule of Law in Informal International Lawmaking Processes’ (2014) 6 Hague Journal on the Rule of Law 75; Joost Pauwelyn, Ramses A Wessel and Jan Wouters, ‘When Structures Become Shackles: Stagnation and Dynamics in International Lawmaking’ (2014) 25 European Journal of International Law 733; Joost Pauwelyn, Ramses A Wessel and Jan Wouters, ‘The Exercise of Public Authority through Informal International Lawmaking: An Accountability Issue?’ (The Jean Monnet Program in cooperation with the Hertie School of Governance 2011) Jean Monnet Working Paper 06/11.

16
as the 2014 Ebola outbreak in Western Africa) and the (legal) framework in which it operates
in doing so.
Section 3 will be devoted to the non-binding recommendations and guidelines developed by
the WHO, and will constitute the most important part of this working paper. In this section, we
have opted to discuss several programmes and guidelines of the WHO (see supra). We make
a first distinction between guidelines and recommendations directed at policy-makers on the
one hand and those directed at private actors. As such, the first case study will concern a WHO
initiative which is mainly aimed at policy-makers, while the second case study will concern a
set of recommendations which is mainly aimed at private actors (although in both cases, the
recommendations are certainly not limited to these actors). The third and final case study will
attempt to demonstrate the sheer number of WHO guidelines, strategies, and other
instruments relevant for one single sector or process (in casu the process of the developing a
pharmaceutical product), without clearly distinguishing between the target-public of the
instruments. Although we realize these case studies present only a limited selection, as there
are many different actors affected by WHO guidelines and recommendations, we estimate that,
through the selection of our case studies, we will be able to draw some generalized
conclusions. Moreover, and unfortunately, giving a more complete overview would be overly
ambitious.
In a fourth and final section we attempt to summarize the information gathered in the previous
sections in an attempt to answer our central research question. We will focus on both ends of
the regulatory process here (i.e. rule-makers and rule-takers), discussing on the one hand how
rules are made in the light of non-traditional law-making theories, and on the other hand on
how and by whom these rules are implemented.
We conclude this introduction with a word on the methodology employed in developing this
report. This report has mainly been based on literature studies and interviews. In terms of the
literature study, most of the primary literature was readily accessible on the WHO’s website.
Indeed, this website presents most relevant information in a structured and clear manner. This
primary literature was confronted with (critical) secondary literature which was searched for
through several online databases (mainly KU Leuven’s Limo database and HeinOnline).
Critical perspectives and clarifications were also sought through interviews. We interviewed
different individuals, including a representative from the pharmaceutical industry in Belgium, a
professor in medicine responsible for the hygiene policy of UZ Gasthuisberg, an official of the
Flemish Agency for Care and Health (“Agentschap Zorg & Gezondheid” in Dutch), and a
Belgian official working at the Regional Office for Europe of the WHO.

17
1. Background
1.1 Introduction
The World Health Organization (WHO) is the United Nations’ specialized agency for dealing
with issues of public health.23 As such, it is generally considered the most important
international actor in the field of global health governance and the organization most suitable
and capable to act as a coordinator of efforts to improve global health.24 In accordance with
article 1 of the WHO Constitution, the objective of the WHO is “the attainment by all peoples
of the highest possible level of health.” To achieve this objective, the WHO has been granted
competences in a wide array of areas. Its manifold functions are outlined in article 2 of the
WHO’s Constitution, which contains no less than 22 paragraphs. In 1997, however, the
Director-General (hereinafter D-G) classified the functions of the WHO in four different
categories25: a role of direction and coordination on international health work, a role of
assistance, including maintaining epidemiological and statistical services, a role of research,
and a normative role. This paper will mainly be concerned with the last function of the WHO,
although the distinction between the different categories is often not that clear-cut.
Public health was one of the first transboundary issues discussed at the early 19th century
multilateral diplomatic conferences, and, as such, part of the then nascent international legal
order.26 From the 1850s on, several International Sanitary Conferences were held to deal
mainly with the issue of infectious diseases. The idea to create a permanent international
agency was already raised at the 1874 Sanitary Conference in Vienna.27 Such an agency was
finally established some three decades later, and was named the International Office of Public
Hygiene (OIHP).28 In addition, the League of Nations established a Health Office (the LNHO).
After the Second World War, the international institutional framework was thoroughly revised,
including in the field of public health. The idea of establishing a single international organization
whose mandate would cover all fields of public health was launched for the first time at the
United Nations Conference on International Organisation, which was convened in San
Francisco from 25 April to 26 June 1945. Subsequently, an International Health Conference,
called for by the United Nations Economic and Social Council29, was held in New York from 19
23 The preamble of the WHO Constitution refers to article 57 of the UN Charter, which concerns the establishment of specialized agencies. On its website, the WHO calls itself “the directing and coordinating authority on international health within the United Nations’ system.” See WHO, ‘About WHO – What we do’, http://www.who.int/about/what-we-do/en/. 24 Gostin and Taylor point to the WHO’s “unique directive to provide leadership” (p. 60), although they also refer to the “multiplication of actors in global health” (p. 54) and “an increasing number of international organizations with lawmaking authority and relevant mandates […] for global health law negotiations” (p. 60). See Lawrence O Gostin and Allyn L Taylor, ‘Global Health Law: A Definition and Grand Challenges’ (2008) 1 Public Health Ethics 53. A central theme in the work of Allyn Taylor is that WHO has a “unique mandate to provide leadership”. See, inter alia, Allyn Taylor, ‘Global Health Governance and International Law’ (2003) 25 Whittier L. Rev. 253, 253. 25 See Burci and Vignes (n 9) 119 with reference to WHO Doc. EB 97/9. 26 Ilona Kickbusch and Margarita Ivanova, ‘The History and Evolution of Global Health Diplomacy’ in Ilona Kickbusch and others (eds), Global Health Diplomacy: Concepts, Issues, Actors, Instruments, Fora and Cases (Springer Science & Business Media 2012). 27 ibid 13. 28 The League of Nations also had a mandate to tackle issues of public health. See ibid 14. 29 The Economic and Social Council adopted a resolution calling for “an international conference to consider the scope of, and the appropriate machinery for, international action in the field of public health and proposals for the establishment of a single international organization of the United Nations.” See ECOSOC Resolution of 5 February 1946, UN Docs. E/9 Res. 1, 1946.

18
June to 22 July 1946. It was attended by 51 delegations from members of the United Nations
and a number of observers and adopted the Constitution for the future World Health
Organisation. Kickbusch and Ivanova describe this historic event as follows: “For the first time
in history, the leading role for health diplomacy was in the hands of a single international
institution, with broad mandate for strategic leadership at an international level.” As a
successor to earlier international public health organizations, “it would carry out the functions
of both the OIHP and the LNHO.”30
1.2 Actors
1.2.1 Membership
Article 3 of the WHO’s Constitution provides that membership in the Organisation “shall be
open to all States”, thus establishing statehood as a requirement for admission. The WHO’s
current membership stands at 194, i.e. practically universal. Membership, besides the right to
participate fully in the activities of the Organisation (e.g. in the discussion and the votes in the
World Health Assembly) and to benefit from its services, also entails the acceptance of the
obligations stipulated in the Constitution31 and the fulfilment of the objective of the
Organisation.
As evidenced by article 3 of its constitutional document, the WHO is a traditional organization
in terms of membership, as only States are allowed full membership. Of course, in the context
of our research, this raises the question of the status of sub-national entities within the WHO.
Sub-national entities, such as the Flemish Community and Region, are represented by their
federal state within the WHO.32 They play an important role in determining the negotiation
mandate for the representatives33, and Flemish experts and/or officials are included in the
Belgian delegations34, but they are not represented in their own capacity at the level of the
WHO. However, the Flemish government in the pursuit of its multilateral policy has adopted
several cooperation agreements with the WHO, where it mainly acts as a sponsor.35 In
30 Kickbusch and Ivanova (n 26) 15. 31 The most important obligation relates to the payment of an equitable share of the Organisation’s expenses as expressly mentioned in Article 56 of the Constitution. There are also some other obligations for a member such as the obligation to implement regulations adopted by the Assembly (Articles 21 and 22 Constitution), as well as the reporting obligations laid out in Articles 61 to 65. 32 Flanders does operate a permanent delegation in Geneva in order to promote cooperation with the international organizations which have their headquarters there. See 33 The general framework for representation in international organizations is set out in the framework agreement of 30 June 1994 for cooperation between the Federal State, the Communities and the Regions with regard to representation of the Kingdom of Belgium with International Organizations whose activities concern shared competences. 34 See Flanders Department of Foreign Affairs, ‘Multilateral Policy’, http://www.vlaanderen.be/int/en/projects-programs?page=4. 35 The Flemish Government claims it has “acquired an important place as a donor in Geneva in the past years, apart from the Belgian federal authorities. Particularly as a sub-state donor, this position in the five organizations with whom Flanders concluded a cooperation agreement (WHO, UNESCO, UNAIDS, IAO and the International Trade Centre), is quite unique, which leads to an exceptional visibility for Flanders as an international actor.” See Departement International Flanders, ‘Multilateral Policy’, http://www.vlaanderen.be/int/node/6337. Most of this cooperation concerns the funding of development projects in South Africa. An overview is available at http://www.vlaanderen.be/int/en/projects-programs?page=4. As this cooperation mainly concerns development, it will only be limitedly discussed in this report, which focusses mainly on the impacts internally in Flanders of the WHO’s normative acts.

19
addition, within the European region of the WHO, several (semi-)autonomous regions have
undertaken a cooperative effort under the denominator of the “Regions for Health Network”, in
which Flanders is directly represented.36 As the name suggests, the RHN mainly serves as a
networking forum and as a space to exchange best practices on regional health governance
(e.g. on horizontal or vertical coordination of health policies). As such, the weight of the RHN
with regard to decision-making at the European Region level, let alone at the level of WHO
headquarters, is limited.
In addition to the complexity arising from Belgian federalism, another layer adds to the
complexity of representation vis-à-vis the WHO, namely the EU. In accordance with article
4.2(k) of the Treaty on the Functioning of the European Union (TFEU), the EU has a shared
competence with the Member States with regard to “common safety concerns in public health
matters, for the aspects defined in this Treaty.”37 Under EU law, once the EU has exercised
such a shared competence, the Member States are barred from exercising their competence
with regard to the same matter.38 In addition, the EU has a more general, less invasive,
supporting competence in the field of “protection and improvement of human health”, in
accordance with articles 6 and 168 TFEU.39 Of course, one must also take the EU’s
competence in the field of development into consideration, as this forms a large part of the
WHO’s work.40 As a result, in some instances, the WHO negotiates directly with the EU rather
than with its Member States. Results of these negotiations might be binding on EU Member
States, including Belgium (and thus Flanders), when they are translated into EU law. However,
as the EU cannot be a member to the WHO, the relationship between the EU and the WHO
remains an external one; the EU’s position remains limited to that of an observer. For the EU,
this means that it grounds its cooperation with the WHO in its external powers to conclude
treaties.41 The basics of this relationship have been laid down in an exchange of letters of 14
December 200142, and the EU currently has a formal delegation at the WHO.43 Between the
EU and the European Region of the WHO (see infra) there exists even closer cooperation,
which was confirmed by a Joint Declaration in 2010.44
36 Membership is open to “any region, province, canton, county, state or oblast belonging to one of the 53 member states in the WHO European Region” and “sub-national authorities outside this region that have a special interest in the RHN work plan”. See WHO/Europe, ‘Membership information’, http://www.euro.who.int/en/about-us/networks/regions-for-health-network-rhn/about-rhn/membership-information. 37 This is relevant for the implementation of the International Health Regulations (see section 2.3.1). 38 Article 2.2 TFEU. 39 Article 168 TFEU stresses at two occasions that the EU “shall complement” Member States’ actions and policies. 40 Article 4.4 and 208-211 TFEU. See, for example, Memorandum of Understanding concerning the establishment of a strategic partnership between the World Health Organization and the Commission of the European Communities in the field of development (05 July 2004), available at http://www.enpi-info.eu/library/content/eu-who-partnership-agreement (hereinafter: the WHO-EC MoU). 41 Generally on the external competences of the EU, see Pieter Jan Kuijper and others, The Law of EU External Relations: Cases, Materials, and Commentary on the EU as an International Legal Actor (OUP Oxford 2013). 42 Text reproduced in Official Journal of the European Communities, 4 January 2001, C 1/7–10. See also http://ec.europa.eu/health/eu_world/international_organisations/who/index_en.htm. 43 R van de Pas and LG van Schaik, ‘Democratizing the World Health Organization’ (2014) 128 Public Health 195, 196. 44 Joint Declaration of the European Commission and WHO/Europe (13 September 2015), available at http://ec.europa.eu/health/eu_world/docs/ec_who_europe_joint_declaration_en.pdf.

20
1.2.2 Other participants
The WHO Constitution provides for the opportunity to enter into relations with other actors, be
it the United Nations (article 69), other intergovernmental organizations (article 70), or non-
governmental international organizations (NGOs) (article 71). Any formal agreement
establishing cooperation with such actors is subject to a two-thirds vote of the World Health
Assembly. The WHO has concluded formal agreements with some sixteen organizations other
than the United Nations. According to Burci and Vignes, “these organisations are mostly within
the UN system, but also include the African Development Bank, the League of Arab States
and the Pan American Health Organization.”45 However, not every cooperation is supported
by a formal agreement, as the Secretariat has developed a practice of informal agreements.46
The relationship with the EU, for example, is governed by informal agreements, such as the
exchange of letters of 2001 (see supra).
While the modalities of the cooperation with other intergovernmental organizations seem to be
determined on a more ad-hoc basis, the WHO has developed a clear institutional framework
and a set of principles for NGO involvement. Central to this framework is the Civil Society
Initiative, established in 2001, which “fosters relations between WHO and nongovernmental
and civil society organizations and is responsible for the administration of formal relations.”47
Its actions and decisions are guided by the Principles governing relations between WHO and
NGOs. The most recent version of these Principles dates from the 40th WHA meeting in 1988.48
In a fairly short, five-page document, it sets out the types of relations with NGOs49, the criteria
for the admission of NGOs in official relations with WHO50, the procedure for admitting NGOs
into official relations with WHO51, the privileges conferred on NGOs by relationship with
WHO52, and the responsibilities of NGOs in their relationship with WHO. As this document
dates from 1988, it is no surprise to find updated rules on the involvement of private actors in
the WHO’s work high on the current reform agenda of the WHO (see infra). An earlier attempt
to adapt this framework to changes in global governance structures stranded, which came forth
45 Burci and Vignes (n 12) 73. 12 of these agreements can be found in the Basic Documents, which are available online at http://apps.who.int/gb/bd/PDF/bd48/basic-documents-48th-edition-en.pdf. 46 ibid 74. 47 See WHO, ‘The Civil Society Initiative’, http://www.who.int/civilsociety/en/. The Standing Committee on Nongovernmental Organizations plays a central role in determining whether NGOs fulfill all conditions to enter into formal relations with WHO. A first report by the CSI, which dates back to 2002, is available at http://www.who.int/civilsociety/documents/en/CSICaseStudyE.pdf?ua=11. 48 They have been adopted by resolution WHA40.25. They are available at http://apps.who.int/gb/bd/PDF/bd47/EN/principles-governing-rela-en.pdf?ua=1. 49 Cooperation with NGOs can be formal (official relations) or informal (on an ad-hoc basis or “working relations”). In functional terms, the Secretariat divided the possible reasons for collaboration with NGOs into 12 categories. See Collaboration with nongovernmental organizations: Review of overall policy on collaboration with nongovernmental organizations (Report by the Director-General) (8 December 1997) WHO Docs. EB101/33, available at http://apps.who.int/gb/archive/pdf_files/EB101/pdfangl/ang33.pdf. 50 The criteria can be summarized as follows: (1) the NGO should be centred on development work in health or health-related fields and it should confirm to the WHO’s vision (the Health-for-All strategy); (2) it should be international and representative of the group/interest it claims to represent; (3) it should have an established institutional structure (with a constitution, headquarters, administrative structure, etc.); and (4) there should have been two years of prior working relations. 51 The Executive Board decides on this question. To this end, it has established a Standing Committee on Nongovernmental Organizations, which reviews the applications, makes recommendations to the Executive Board on these applications (the possibilities being to postpone, consider or reject), and reviews the usefulness of collaboration with all NGOs in official relations every three years. Once an NGO is admitted into official relations, a plan for collaboration is developed. 52 The most important privilege is the right to participate in all kinds of WHO meetings (albeit without the right to vote).

21
from a meeting in 1997 between WHO and 130 NGOs, established the Civil Society Initiative,
stranded in 2004 on the opposition of “a bare handful of countries (including China).”53
1.2.3 Involvement of experts
Experts from different fields also play an indispensable role within the WHO. They serve to
facilitate WHO’s exercise of its technical and research functions, but have also been playing a
pivotal role in WHO’s normative functions. As Burci and Vignes note, “[m]ost
recommendations, guidelines and standards do not take the form of a full-fledged regulatory
text approved by the Assembly, but rather that of technical documents elaborated by groups
of experts or external collaborators.”54
Expert involvement and consultation is generally subject to the Regulations for Expert Advisory
Panels and Committees and the Regulations for Study and Scientific Groups, Collaborating
Institutions and Other Mechanisms of Collaboration.55 While the first set of regulations has
been adopted by the World Health Assembly, the second set has been adopted by the
Executive Board.56 These regulations outline different methods to obtain expertise.
Firstly, there are the expert advisory panels, which give the Secretariat “technical guidance
and support within a particular subject.”57 Essentially, these panels are lists of experts upon
whose expertise the WHO can draw on individually or through expert committees. According
to the regulations, expert advisory panels are established and disestablished by the D-G, who
reports to the Executive Board on this matter.58 However, in practice, the authority to establish
and disestablish expert advisory panels is shared with the WHA and the EB, while the selection
of members, which happens for renewable four-year terms, is in the hands of the D-G.59
Currently, 47 expert advisory panels exist, which totaled 653 expert members in December
2014.60
Secondly, expert committees are set up “for the purpose of reviewing and making technical
recommendations on a subject of interest”61. They are composed of members from one or
several expert advisory panels.62 In accordance with articles 18(e) and 38 of the WHO
Constitution and section 2.3 of the regulations mentioned above, the authority to set up such
committees rests with the WHA and the EB. Again, practice differs as it is mainly the D-G who
decides when expert committees are convened and which experts sit in each meeting.63 In this
regard, it is important to note that there are no fixed lists for each expert committee. Rather,
53 van de Pas and van Schaik (n 43) 197. 54 Burci and Vignes (n 12) 146. See also section 3.1. 55 The text of these regulations can be found in the Basic Documents, which are online available at http://apps.who.int/gb/bd/PDF/bd48/basic-documents-48th-edition-en.pdf. 56 Burci and Vignes (n 12) 148. See respectively resolution WHA35.10 as amended by decision WHA45(10), resolution WHA49.29, resolution WHA53.8, and resolution WHA 55.24, and resolution EB69.R21 as amended by resolution EB105.R7. 57 Section 1.1 of the Regulations for Expert Advisory Panels and Committees. 58 Ibid., sections 2.1 and 2.2. 59 Burci and Vignes (n 12) 146. 60 In comparison with 720 in December 2013. More recent data are, unfortunately, not available. See WHO, ‘Knowledge management and health – Expert advisory panels and committees’, http://www.who.int/kms/expert_panels/en/. 61 Section 1.3 of the Regulations for Expert Advisory Panels and Committees. 62 Ibid., section 4.2. 63 Burci and Vignes (n 12) 146. They state that “[t]he establishment and convening of expert
committees instead falls under the authority of the Director-General.”

22
which experts are invited, depends on the subject of each separate meeting. This ensures that
relevant expertise is present for every expert committee meeting. The experts sitting in an
expert committee are deemed to serve the WHO exclusively and are not allowed to receive
instructions from Member States or other actors.64 The outcomes of these expert committees
are not considered official positions of the WHO, and thus do not commit the organization. In
this sense, section 4.12 of the Regulations for Expert Advisory Panels and Committees
specifically stipulates that “conclusions and recommendations [from these committees] shall
not commit the Organization and should be formulated in such a way as to advise the D-G on
future programme activities without calling upon him [to take certain actions]”. Nevertheless,
reports of these committees are routinely published in the “Technical Report Series” – although
the D-G can decide otherwise – and they often “exercise considerable influence on the
scientific development of the issue concerned.”65 As such, these expert committees play an
essential role even in the exercise of the WHO’s normative function.
Thirdly, study groups can be convened whenever technical expertise is required on a specific
subject but establishing or convening an expert committee is unsuitable.66 In essence, they
are a more informal and flexible form of expert committees.67 Scientific groups, which constitute
a separate category, “play for research a role comparable to that of expert committees and
study groups for the Organization’s programme in general.”68 These groups review “given fields
of medical, health and health systems research, to assess the current state of knowledge in
these fields.”69
Finally, collaborating centers are external institutions which help the WHO maintain an
extensive and elaborate institutional research network.70 Designation of research institutions
as collaborating centres is in the hands of the D-G71 who is supported by the Regional
Directors72, on the basis of criteria set out in the Regulations mentioned above.73 The
designation of an external institution as an official WHO collaborating centre ‘is independent
of financial support being given to the institution by WHO.’74 The relationship is generally based
on reciprocity, allowing the WHO to develop its research network and be able to “exercise
leadership in shaping the international health agenda”75, while granting the collaborating
centres more visibility as they can carry the official title of ‘WHO Collaborating Centre’. In total,
64 Section 4.6 of the Regulations for Expert Advisory Panels and Committees. 65 Burci and Vignes (n 12) 147. 66 Section 1.1 of the Regulations for Study and Scientific Groups, Collaborating Institutions and Other Mechanisms of Collaboration. 67 This is evidenced by the section on Study Groups in the Regulations for Study and Scientific Groups, Collaborating Institutions and Other Mechanisms of Collaboration, which regularly refers to the rules on expert committees. 68 Section 2.1 of the Regulations for Study and Scientific Groups, Collaborating Institutions and Other Mechanisms of Collaboration. 69 Ibid. 70 Burci and Vignes (n 12) 148. 71 See WHO, ‘Collaborating Centres – Background’, http://who.int/collaboratingcentres/cc_historical/en/index1.html. 72 The Regional Directors propose institutions to the D-G and provide him with the information necessary to decide upon their designation. 73 Section 3.5 of the Regulations for Study and Scientific Groups, Collaborating Institutions and Other Mechanisms of Collaboration. See also WHO, ‘Guide for WHO Collaborating Centres’ (2014), available at http://who.int/collaboratingcentres/Guide_for_WHO_collaborating_centres_2014.pdf?ua=1. 74 See WHO, ‘Collaborating Centres – Background’, http://who.int/collaboratingcentres/cc_historical/en/index1.html 75 Ibid., second tab.

23
over 700 institutions in over 80 countries are currently supporting the WHO as collaborating
centres.76
As a final note, it should be stated that, while working for the WHO, experts can enjoy limited
immunities.77 This confirms their status as (semi-)officials of the WHO, which implies that these
experts cannot defend their States’ interests.
1.3 Institutional structure
1.3.1 The three levels and federalism
Institutionally, the WHO consists of three levels: the headquarters (which is located in Geneva),
the six regional offices (for the six regions of Africa, the Americas, South-East Asia, Europe,
the Eastern Mediterranean and the Western Pacific) and the country offices. Debate persists
as to the division of tasks between the three levels, as evidenced by the establishment of a
taskforce with the aim of clarifying the roles and functions of the three levels.78 Nevertheless,
at a very basic level, the division of tasks can be summarized as follows. Headquarters is
responsible for providing global guidance, for example, in the form of global strategies and
plans of action, as well as for setting standards and norms. The regional offices help States in
implementing these global strategies by providing more concrete action plans, adapted to the
regional circumstances. Conversely, they relate regional concerns and experiences with
regard to the implementation of the global standards, norms and strategies to headquarters.
In addition, these regional offices often serve as a central contact point in the provision of
technical assistance. Country offices, then, provide States with technical advice and support
for the implementation of these global norms and standards which have been translated into
regional action plans. Given the technical assistance role of the country offices, country offices
have not been established in every state. Developed States, requiring little to no technical
support in the implementation of global standards, generally have no country offices. In the
European Region, for example, only 29 out of 53 Member States have a country office, and,
importantly, Belgium does not have a country office.
Historically, the relationship between headquarters and (some of) the regions has been
tense.79 The regions have always enjoyed a large degree of autonomy, which has even led
one author to use the term “federalism” to describe the WHO’s institutional structure.80 The
importance of the regional offices is stressed by the dedication of an entire chapter of the
WHO’s Constitution to their role. Especially the relationship with the American region remains
76 See WHO, ‘Collaborating Centres’, http://who.int/collaboratingcentres/en/. A database of all collaborating centres is available at http://apps.who.int/whocc/. 77 Clause 2 of Annex VII “The World Health Organization” to the Convention on the Privileges and Immunities of the Specialized Agencies (adopted on 21 November 1947, entered into force on 2 December 1948) 33 UNTS 261. 78 The division of tasks for each of the WHO’s functions is set out in ‘Annex 1. Overarching Roles and Functions of the Three Levels of WHO’ to the ‘Report of the Taskforce on the roles and functions of the three levels of WHO’. This document is available at http://www.who.int/about/who_reform/task_force_report_three_levels_who_2013.pdf. 79 However, how good the relationship is, depends heavily on the regional office concerned; the relationship with the European regional office, for example, seems to be relatively good. See van de Pas and van Schaik (n 43) 199. 80 Tine Hanrieder, ‘The Path-Dependent Design of International Organizations: Federalism in the World Health Organization’ [2014] European Journal of International Relations 215.

24
difficult as the Pan American Health Organization (PAHO), which coordinates health
improvement efforts in the Americas, predates the establishment of the WHO. Although this
organization was meant to be fully integrated into the WHO81, it retains a special status, as
evidenced by the fact that the WHO has concluded an official agreement with it (see section
1.2.2). The tense relationship is most clearly demonstrated by debates about the status of
Regional Directors, focusing on the question of the appointment of Regional Directors and their
relationship vis-à-vis the D-G. Article 52 of the WHO Constitution reads: “The head of the
regional office shall be the Regional Director appointed by the Board in agreement with the
regional committee.” Although the formulation suggests that the Board can refuse candidates
proposed by the Regional Committee, it has never done so.82 This lack of control by the EB
has been questioned at several occasions.83 It has also led to limited oversight capabilities for
the D-G vis-à-vis the Regional Directors. Consequently, the question of appointment forms
part of the discussion with regard to the new WHO reform.
1.3.2 The structure of headquarters
At headquarters level, the WHO is governed by three central governing bodies, as is the case
for most international organizations.84 The most important organ consists of delegates and
representatives of all members, the World Health Assembly (WHA).85 The second organ, the
Executive Board, consists of delegates of a select, rotating group of members and is mainly
charged with implementation of the work of the first organ.86 Finally, the Secretariat, headed
by the D-G, consists of supporting staff tasked mainly with an administrative function.87
The World Health Assembly is the supreme decision-making body for the WHO. It generally
meets in Geneva in May each year88, and is attended by delegations from all 194 Member
States. A delegation is composed of a maximum of three actual delegates89, which may,
however, be accompanied by an unlimited amount of supporting staff (alternates and
advisers).90 However, these delegations of Member States are not the only component of the
Assembly, which also includes representatives and observers.
Under the qualification of “representative”, different categories of persons are subsumed. First
of all, under this heading the Executive Board sends representatives to participate in the work
of the Assembly as provided for in the WHA Rules of Procedure.91 Secondly, representatives
of the United Nations and of other intergovernmental and non-governmental organizations
81 Article 54 WHO Constitution. 82 Burci and Vignes (n 12) 75. This independent appointment has led to the question whether the D-G is the administrative and hierarchical superior of the Regional Directors. 83 ibid. 84 Article 9 WHO Constitution. 85 Article 10 WHO Constitution. 86 Article 24 WHO Constitution. 87 Article 30 WHO Constitution. 88 Art. 13 WHO Constitution. This article provides also that special sessions shall be convened at the request of the Board or of a majority of the members. So far, no special session have been requested or convened. 89 Article 11 WHO Constitution. 90 Article 12 WHO Constitution. 91 Rule 44 WHA Rules of Procedure. At present, four such persons represent the Executive Board at the Assembly; its Chairman is designated ex officio together with three others members of the Board.

25
admitted into relationship with the Organization also participate in the work of the Assembly
(see 1.2.2).92
Unlike delegates and representatives, observers are not mentioned in the Constitution.
Reference is made to them, however, in specific cases in the WHA Rules of Procedure. Their
role has mainly been developed in practice. Two categories of observers may be identified:
the observers invited for a limited period, on the one hand, and the “quasi-permanent
observers” on the other. The first category relates to potential members of the WHO: States
that have submitted an application for membership and States which have signed but not
ratified the Constitution.93 In the same category are observers representing “non-Member
States” mentioned in Rules 19 and 47 of the WHA Rules of Procedure. Besides these
observers, so-called “quasi-permanent observers” exist as well, that is, certain bodies which
are regularly invited to all sessions of the Assembly. At present, five observers are regularly
invited by the D-G to attend sessions of the Assembly: the Holy See, the Order of Malta, the
International Committee of the Red Cross, the International Federation of Red Cross and Red
Crescent Societies, and the Palestinian Authority.94
Article 18 of the Constitution enumerates the thirteen functions of the Assembly. Broadly
speaking, one can say that, within the frame of the Constitution, the Assembly has the power
to do “whatever it deems appropriate to achieve the objectives of the Organisation.”95 The
Assembly’s main function is to determine the policies of the Organization.96 The Health
Assembly appoints the D-G and designates the members entitled to send an official to serve
on the Executive Board. It also acts as a financial supervisor, reviewing and approving the
proposed programme budget. Finally, it sets the agenda for the Executive Board, which reports
to it, by designating areas in which further action is required.97
The Assembly appoints a number of Committees for divergent tasks.98 A prominent part in the
Assembly is played by the General Committee.99 It consists of 25 members, namely, the
President of the Assembly, who chairs the committee, the five Vice-Presidents, the Chairmen
of the two main committees and seventeen other members elected by the Assembly. The
General Committee is the steering committee of the Assembly: it deals with issues relating to
the agenda, initial allocation to the two main committees of items of the Agenda and, if
appropriate, the deferment of any item to a future Assembly, the election of members entitled
to designate persons to serve on the Executive Board, transfer of items from one committee
to another, decision on the programme of work, and it “otherwise facilitate[s] the orderly
dispatch of the business of the session.”100
There are two other “main committees”, Committee A and Committee B.101 The former deals
predominantly with programme and budget matters, the latter with administrative, financial and
legal matters. Despite their apparent limitation to administrative functions, these two
committees play an important role within the WHO: it is through them that most of the work of
92 See Rule 19 of the WHA Rules of procedure. 93 Rule 3 WHA Rules of Procedure. 94 A subtle distinction is made between these observers which becomes apparent in the list of participants where the Holy See appears under ‘Observer for a non-Member State’, the three following observers under ‘Observers’ and the last one, Palestine, under ‘Observers invited in accordance with Resolution WHA27.37 95 Burci and Vignes (n 12) 44. 96 Article 18(a) WHO Constitution. 97 WHO, ‘Governance’, available at http://www.who.int/governance/en/index.html 98 Article 18(e) WHO Constitution. 99 Rule 29 WHA Rules of Procedure. 100 See rule 31 WHA Rules of Procedure. 101 Rule 32 WHA Rules of Procedure.

26
the Assembly is conducted.102 In addition to these two bodies, the Assembly may establish
such other committees as it may consider necessary.103 In turn the main committees may also
set up sub-committees or other subdivisions under their own auspices.104
Typically, a simple majority is required for the adoption of a decision by the WHA.105
Exceptionally a two-thirds majority is required for questions considered as important either by
the Constitution itself (adoption of conventions or agreements, approval of agreements
bringing the Organization into relation with the UN and inter-governmental organizations and
agencies, amendments to the Constitution)106, or by the WHA Rules of Procedure (decisions
on the amount of the effective working budget, suspension of the voting privileges and services
under Article 7 of the Constitution)107. Nevertheless, consensus is the preferred voting method
in the WHA.108
The second body, which is more executive in nature, is the Executive Board. It is composed
of 34 members technically qualified in the field of health.109 Members are elected for three-year
terms.110 Although the members of the Board were initially supposed to serve in their personal
capacity, they de facto act as government representatives.111 The Executive Board meets twice
a year: once in January to prepare for and approve the agenda of the forthcoming Health
Assembly meeting, and once in May, immediately after the Health assembly, for more
administrative matters.112 The Board is designed to support the Health Assembly, both ex ante,
by advising it, and ex post, by handling the implementation of its decisions.113 Similar to
practices in the Assembly, the Board adopts decisions and resolutions most often by
consensus.114
The Secretariat of WHO, finally, is dispersed over different locations: the headquarters at
Geneva, the six regional offices and local delegations.115 Its 7000-odd-strong staff consists of
health and other experts and support staff on fixed-term appointments. The Secretariat is in
charge of the management of the Organization. It also has functions related to the activities of
the constitutional bodies, mainly the Assembly and the Board but also conferences convened
by the Organization. Within that framework, the Secretariat prepares the meetings, sends
invitations, drafts the documents, circulates them, and prepares the briefings which will be
used during the meetings. The Secretariat is also in charge of the execution of the decisions
taken by the constitutional bodies. The Organization is headed by the D-G, who is appointed
by the Health Assembly, which elects one of three candidates proposed by the Executive
Board.116 This appointment procedure has been changed recently after discussions in the
Working Group of Member States on the Process and Methods of the Election of the D-G of
102 Burci and Vignes (n 12) 43. 103 Article 18(e) WHO Constitution. 104 Rule 38 WHA Rules of Procedure. 105 Rule 71 WHA Rules of Procedure. 106 Article 60 WHO Constitution. 107 Rule 70 WHA Rules of Procedure. 108 Burci and Vignes (n 12) 47. 109 Article 24 WHO Constitution. 110 Article 25 WHO Constitution. 111 Res. WHA51.26, WHA51/1998/REC/1, p. 29. On this issue, see Claude-Henri Vignes, ‘Mythe et Réalité: Le Statut Des Membres Du Conseil Exécutif de L’organisation Mondiale de La Santé’ (1999) 103 Revue Générale de Droit International Public 685. 112 See WHO, ‘Governance – The Executive Board’, http://www.who.int/governance/eb/en/. 113 Ibid. 114 Burci and Vignes (n 12) 47. 115 WHO, ‘Governance – Governing Bodies’, http://who.int/governance/en/. 116 Article 31 WHO Constitution.

27
the World Health Organization.117 An organigram of the WHO Secretariat can be found in
Annex I.
1.3.3 The structure of the European regional level
The WHO Regional Office for Europe118, which is based in Copenhagen, has a membership
of 53 States, which include all Member States of the EU, in addition to countries such as
Turkey, Russia, and Kazakhstan. The most important organ at the European regional level is
the Regional Committee consisting of delegates of all members119, and which is established
directly through article 47 of the WHO Constitution. Its annual four-day meetings take place in
September.120 At these meetings, regional policies are formulated, the regional component of
WHO’s budget is commented upon, and, once every five years, a Regional Director is
nominated (who is subsequently endorsed by the headquarters’ EB).121 At these meetings, a
President, Executive President, and a Deputy Executive President are elected, as well as a
Rapporteur.122
The Regional Committee can equally establish sub-committees, of which the Standing
Committee of the Regional Committee (SCRC) – the regional equivalent of headquarters’ EB
– is the most important.123 The SCRC consists of representatives from 12 Member States,
elected for a three-year period124, and one Chairperson, a position de officio filled by the Deputy
Executive President of the Regional Committee125.126 These members are deemed to “consider
the general interests of the Region and act on behalf of the Regional Committee as a whole.”127
Member States of the Region can freely nominate representatives for these positions, after
which “the Officers of the Standing Committee, in consultation with the Executive President of
the Regional Committee, shall seek consensus among Member States submitting
nominations.”128 Regular attendance of SCRC meetings, which might occur by proxy, is
required, for fault of which the seat may be declared vacant.129 In terms of functions, the SCRC
closely resembles the EB at the headquarters level: it acts for and represents the Regional
Committee and ensures implementation of its decisions; it generally advises the Regional
Committee and counsels the Regional Director; it proposes items for the Regional Committee’s
agenda; etc.130 The SCRC convenes at least four times a year, with only the May session being
117 The documents from this working group are available online at http://apps.who.int/gb/edg/. 118 This is the name generally attributed to the European regional branch of the WHO. However, it refers mainly to the European branch of the WHO Secretariat. Therefore, we will use this term interchangeably with terms as ‘the European Region’ or WHO/Europe, which are equally used by the WHO. 119 WHO/Europe, ‘Regional Committee for Europe’, available at http://www.euro.who.int/en/about-us/governance/regional-committee-for-europe/regional-committee-for-europe2. 120 Ibid. 121 Ibid. 122 The Depute Executive President would normally become Executive President during the next session. Rule 10 of the Rules of Procedure of the Regional Committee for Europe (as last amended on 18 September 2013), available at http://www.euro.who.int/__data/assets/pdf_file/0016/242530/132552E_Rules-of-Procedure_2013_a4.pdf?ua=1 123 Rule 14.2 Rules of Procedure of the Regional Committee for Europe. 124 Rule 14.2.3 125 Rule 14.2.4 126 Rule 14.2.1 Rules of Procedure of the Regional Committee for Europe. 127 Rule 14.2.11. 128 Rule 14.2.2(b) Rules of Procedure of the Regional Committee for Europe. 129 Rule 14.2.7. 130 Rule 14.2.10.

28
open to all members of the European region (plus regional economic integration organizations,
i.e. the EU) and non-elected Member States participating without voting rights.131 At its first
annual meeting, the SCRC elects a Vice-Chairperson, who will – barring any serious opposition
– be elected Deputy Executive President of the Regional Committee by the Regional
Committee in the year following his/her election.132
The work of both the Regional Committee and its Standing Committee is supported by the
Regional Office, which is headed by the Regional Director133, but remains subject to “the
general authority of the Director General.”134 The WHO Constitution describes the Regional
Office as “the administrative organ of the Regional Committee.”135 In this administrative organ,
the Regional Director plays a central role. We mentioned some of the issues with regard to the
appointment/election of the Regional Director earlier. Although the formulation of article 52
WHO Constitution suggests a major role for the EB in a clear procedure of appointment, the
reality and article 47 of the Rules of Procedure of the Regional Committee for Europe rather
suggest a procedure of election where the main authority lies with the Regional Committee.136
Article 47 of these Rules of Procedure sets out a complex procedure, involving a Regional
Evaluation Group which develops an “unranked short-list of not more than five candidates” on
the basis of criteria laid down in two resolutions of the Regional Committee.137 On the basis of
this short-list and through secret ballot votes in private meetings of the Regional Committee,
candidates are eliminated until only one candidate remains. To enhance the legitimacy of this
process, a code of conduct was adopted by the Regional Committee in 2013, which lays down
non-binding rules for inter alia the submission of proposals, the electoral campaigns (e.g. with
regard to the transparency of the funding thereof), etc.138
1.4 Reforming the WHO
During the EB meeting of January 2011, the D-G presented a report on the future financing of
the WHO, which had become a serious cause for concern.139 Currently, the WHO’s is largely
funded by voluntary, and often earmarked, contributions, since the assessed contributions by
states have stagnated at the end of the 1990s. In the period 2010-2011, for example, “75% of
WHO’s programs […] were funded through extra-budgetary voluntary contributions, 91% of
which were earmarked for specific donor-driven priorities and programs.”140 The Bill and
Melinda Gates, for example, has become one of the WHO’s largest sources of funding, second
131 Rule 4 jo. Rule 3 of the Rules of Procedure of the Standing Committee of the Regional Committee for Europe. 132 Rule 9. 133 Article 52 WHO Constitution. 134 Article 51 WHO Constitution. 135 Article 51 WHO Constitution. 136 The term ‘election’ is even used on the website of the European Region of the WHO. See http://www.euro.who.int/en/about-us/regional-director/election-of-regional-director-2014/nomination-process-for-who-regional-director-for-europe. 137 Resolution EUR/RC40/R3 has been amended by resolution EUR/RC47/R5. Both are available at http://www.euro.who.int/en/about-us/regional-director/election-of-regional-director-2014/nomination-process-for-who-regional-director-for-europe. 138 This code of conduct has been adopted as Annex VI to the resolution EUR/RC63/R7 of the European regional committee, and is available online at http://www.euro.who.int/en/about-us/regional-director/election-of-regional-director-2014/nomination-process-for-who-regional-director-for-europe. 139 The future of financing for WHO (Report by the Director-General) (15 December 2010) WHO Docs. EB 128/21, available at http://apps.who.int/gb/ebwha/pdf_files/EB128/B128_21-en.pdf. 140 van de Pas and van Schaik (n 43) 197.

29
only to the United States. Not only has this caused constant concern over WHO’s continued
financing, it has also called into question the WHO’s independence.141 Referring both to the
opinion of Member States and the Global Policy Group – which consists of the D-G, the deputy
D-G and the 6 Regional Directors – the report stated that capitalizing on the WHO’s leadership
role in global health “requires fundamental reforms in the way the Organization operates.”142
As a response, the WHO decided to start up a reform process to clarify the role of the WHO in
the global health system, which the WHA endorsed at its 64th meeting in 2011.143 Although the
main trigger was the fear of financial instability, the reform process encapsulates a wider array
of issues, such as legitimacy, accountability, efficacy, and effectiveness.
The reform is constructed around three main axes: a programmatic reform, a governance
reform, and a managerial reform.144 The programmatic reform aims to rethink and spell out the
priorities of the WHO, and how to address and finance them. The governance reform seeks to
streamline the existing decision-making processes (inter alia by clarifying the roles and
functions of the three levels of WHO), but also to enhance their legitimacy (inter alia by the
closer involvement of a larger range of stakeholders145). The managerial reform, finally, targets
the efficiency and effectiveness of the WHO decision-making and administrative processes,
as well as its communication, financing, etc. A useful overview of the different areas of reform
and the progress in these different areas is available through a special app on the website of
the WHO.146
It is worth to take a – short – closer look at the governance reform, which is most likely to result
in significant changes from the point of view of actors and institutional structure, discussed
above. Two reports by the Secretariat were discussed at the 2014 WHA meeting and the
January 2015 EB meeting, entitled “Improved decision-making by the governing bodies”147 and
“Framework of engagement with non-state actors.”148 Indeed, these two items form the
centrepiece of the governance reform149, and especially the relationship with non-state actors
is subject to serious debate.150 Whereas some Member States consider the involvement of and
partnerships with all types of non-state actors151 essential to enhance the WHO’s legitimacy
141 Charles Clift, The Role of the World Health Organization in the International System (2013) 11 <http://www.chathamhouse.org/sites/default/files/public/Research/Global%20Health/0213%5Fwho.pdf> accessed 28 August 2015. 142 The future of financing for WHO (Report by the Director-General) (15 December 2010) WHO Docs. EB 128/21, available at http://apps.who.int/gb/ebwha/pdf_files/EB128/B128_21-en.pdf, 1. 143 Resolution WHA64.2 (“WHO Reform”) (20 May 2011), WHO Docs. WHA64/2011/REC/1, available at http://apps.who.int/gb/ebwha/pdf_files/WHA64-REC1/A64_REC1-en.pdf. 144 On the website of the WHO, a one-page document is available which broadly outlines the objectives and process of the reform. See http://who.int/about/who_reform/who_reform_story.pdf?ua=1. 145 Ilona Kickbusch, Wolfgang Hein and Gaudenz Silberschmidt, ‘Addressing Global Health Governance Challenges through a New Mechanism: The Proposal for a Committee C of the World Health Assembly’ (2010) 38 The Journal of Law, Medicine & Ethics 550. In this light, Gostin and Taylor have criticized the formal state-centric system of international law. See Gostin and Taylor (n 24). 146 See http://spapps.who.int/WHOReform/SitePages/Reports/Dashboard.aspx. 147 Available at http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_5-en.pdf?ua=1. 148 Available at http://apps.who.int/gb/ebwha/pdf_files/EB136/B136_5-en.pdf?ua=1. 149 See WHO, ‘About WHO – Governance reform’, http://www.who.int/about/who_reform/governance/en/. 150 We have mentioned above that the election methods and processes for the Director-General have also been reformed recently. 151 In the current draft of the ‘framework of engagement with non-state actors’, four types of actors are discerned: NGOs (non-profit entities operating independently of governments), private sector entities (commercial enterprises, including international business associations), philanthropic foundations (“non-profit entities whose assets are provided by donors and whose income is spent on socially useful purposes”), and academic institutions.

30
and effectiveness, others fear that such relationships might lead to conflicts of interest and
thus endanger the WHO’s independence, or that it might ‘white-wash’ the non-state actor’s
practices, especially in the case of business actors.152 Nevertheless, as stated in the
Assembly’s 2015 resolution WHA 68.9, the WHA hopes to finish the new framework document
by its next meeting (on 23-28 May 2016).153 The criteria guiding the improvement of the
decision-making process of the WHO governing bodies are the strengthening of its strategic
role, inclusiveness, transparency, and efficiency.154 Reform proposals range from a better use
of digital communications (e.g. through improved access to documentation online, through
webcasting and through online forums for prior and continuous discussion of items on the
agenda155) to increased flexibility (e.g. with regard to the late submission of proposals for
resolutions in the WHA156).
In addition, the WHO is also considering reforms in the field of health emergencies due to the
unsatisfactory response to the Ebola crisis.157 This will be discussed in section 2.3.3.
152 See Appendix to ‘Framework of engagement with non-state actors’ (WHA Resolution 68.9, 26 May 2015), available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R9-en.pdf, para 8. 153 See ‘Framework of engagement with non-state actors’ (WHA Resolution 68.9, 26 May 2015), available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R9-en.pdf. 154 See ‘Method of work of the governing bodies’ (Report by the Secretariat, 5 December 2014), WHO Docs. EB136/6, available at http://apps.who.int/gb/ebwha/pdf_files/EB136/B136_6-en.pdf, para 2. 155 See, in general, ‘Improved decision-making by the governing bodies’ (Report by the Secretariat, 7 May 2014) WHO Docs WHA67/5, available at http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_5-en.pdf?ua=1, para 2-4. 156 See ibid., para 12-14. 157 See WHO, ‘About WHO - Advisory Group on Reform of WHO’s Work in Outbreaks and Emergencies with Health and Humanitarian Consequences’, http://who.int/about/who_reform/emergency-capacities/advisory-group/en/. An executive summary of their first report was published on November 6, 2015 and is available at http://who.int/about/who_reform/emergency-capacities/advisory-group/face-to-face-report-executive-summary.pdf?ua=1.

31
2. Legally binding instruments
2.1 The law-making powers of the WHO
The WHO has a broad mandate and extensive powers to develop international rules.158 The
WHO can exercise this normative function through binding (conventions or agreements and
regulations) and non-binding measures (recommendations and guidelines). The WHO’s
powers to develop binding instruments are set out in articles 19-22 WHO Constitution. Article
19 of the Constitution designates the WHA as the forum for the negotiation of global health
conventions. In accordance with this article, the WHA can adopt conventions “with respect to
any matter within the competence of the Organization” with a two-thirds majority. These
conventions will become binding upon Member States after ratification in accordance with their
constitutional procedures. Despite this seemingly traditional method of developing international
law159, Gostin, Sridhar and Hougendobler argue that the twist lies in article 20 of the WHO
Constitution:
“It is Article 20 that is exceptional in that it directs members to ‘take action’ by accepting
or rejecting the convention or agreement within eighteen months after adoption by the
Assembly, presumably even if its WHA delegation voted ‘no.’ Each member must notify
the D-G of the action taken, such as submission of the treaty for ratification. If a member
does not accede to the treaty within the allotted time, it must furnish a statement of
reasons. This is a powerful mechanism, highly unusual in international law, as it
requires states to seriously consider the treaty in accordance with national
constitutional processes. Articles 20 and 62 give the D-G monitoring authority, as
members that accede to a treaty must report annually towards implementation.”160
Despite repeated calls to make more extensive use of this competence, the WHO has only
developed one convention in accordance with article 19 (see infra section 2.2).
Article 21 grants the WHO the competence to develop regulations with regard to five specific
topics.161 These regulations bind Member States in accordance with a system of opt-out:
Member States are bound by these regulations unless they explicitly reject them or make
reservations within a certain period.162 Only two types of regulations have been adopted under
158 Burci and Vignes (n 3) 124. 159 Taylor argues that the capacity to serve as a forum for the development of conventions in itself, is already exceptional: “Not all international organizations have lawmaking authority or the legal mandate to serve as a platform for lawmaking in health. In the international legal system, lawmaking authority is always express and never implied.” Allyn L Taylor, ‘Global Health Law’ in Ilona Kickbusch and Margarita Ivanova (eds), Global Health Diplomacy: Concepts, Issues, Actors, Instruments, Fora and Cases (Springer Science & Business Media 2012) 44. 160 LO Gostin, D Sridhar and D Hougendobler, ‘The Normative Authority of the World Health Organization’ (2015) 129 Public Health 854, 856. 161 The WHA can adopt regulations concerning: (a) sanitary and quarantine requirements and other procedures designed to prevent the international spread of disease; (b) nomenclatures with respect to diseases, causes of death and public health practices; (c) standards with respect to diagnostic procedures for international use; (d) standards with respect to the safety, purity and potency of biological, pharmaceutical and similar products moving in international commerce; (e) advertising and labelling of biological, pharmaceutical and similar products moving in international commerce. 162 This mechanism runs counter to the general principle of international law which requires express consent in order for States to be bound by treaties. Article 11 of the Vienna Convention reads as follows: The consent of a State to be bound by a treaty may be expressed by signature, exchange of instruments constituting a treaty, ratification, acceptance, approval or accession, or by any other means if so agreed.”

32
this article, namely the International Health Regulations (see section 2.3) and the
Nomenclature Regulations (see section 2.4).163 According to Gostin and Taylor, at the turn of
the millennium, these two regulations “were largely historical, were limited in scope and lacked
real-world impact.”164 This situation has clearly changed for the International Health
Regulations in the course of the new millennium.
All in all, the WHO has only made very limited use of its power to develop binding
instruments.165 Instead, the WHO has often opted to develop non-binding, soft law instruments
(such as guidelines and recommendations) in exercise of its normative function (see section
3). Indeed, “[d]espite WHO's impressive normative powers, modern international health law is
remarkably thin.”166 Several scholars have criticized the WHO for insufficient use of its ability
to develop binding instruments.167 One of the lead critics is Allyn Taylor, who proved critical of
the WHO’s “non-legal strategy” and defended an international law approach (through
framework conventions) in her doctoral dissertation. 168 In her PhD, she developed the idea of
a framework convention on tobacco control, modelled after the framework conventions then
recently adopted in the field of international environmental law (see infra). Other scholars, such
as Kevin Klock, have defended the WHO’s soft law approach for having certain advantages
over the hard law alternative, such as increased flexibility and a lower threshold for adoption.169
In this sense, Lawrence Gostin has remarked that “it is important not to discount the value of
‘soft’ norms.”170 Recent research has indeed pointed to the high compliances rates of certain
non-binding norms and has contrasted this with the low compliance rate of certain binding
norms.171 Nevertheless, academics and advocacy groups alike have continued to promote a
more proactive approach, making use of WHO’s law-making authority (see section 2.2.2).
2.2 The treaty-making powers of the WHO: article 19 of the WHO
constitution
2.2.1 The Framework Convention on Tobacco Control
Article 19 grants the WHO the authority to develop treaties. Although this authority has featured
in the WHO Constitution since 1946, the WHO has generally been reticent of using binding
norms of international law to further its goals. Indeed, as mentioned above, the WHO has only
made use of its authority under article 19 once.172
163 Burci and Vignes (n 12) 131. 164 Gostin and Taylor (n 24) 61. 165 Kevin A Klock, ‘The Soft Law Alternative to the WHO’s Treaty Powers’ (2013) 44 Georgetown Journal of International Law 821, 822. 166 Gostin, Sridhar and Hougendobler (n 160) 856. 167 David P Fidler, ‘The Future of the World Health Organization: What Role for International Law’ (1998) 31 Vand. J. Transnat’l L. 1079. 168 Taylor, ‘Making the World Health Organization Work’ (n 14) 335. 169 Klock (n 165). 170 Lawrence O Gostin and others, ‘Towards a Framework Convention on Global Health’ (2013) 91 Bulletin of the World Health Organization 790, 792. 171 Gregory Shaffer and Mark A Pollack, ‘Hard vs. Soft Law: Alternatives, Complements and Antagonists in International Governance’ (2010) 94 Minnesota Law Review 706. 172 The reasons for this reluctance are, undoubtedly, partly to be found in the composition of the WHO’s staff, which consists mainly of medical experts, whereas most international organizations are mainly staffed with legal experts (see supra).

33
When Ruth Roemer and Allyn Taylor suggested to develop an international treaty to combat
the tobacco epidemic under the auspices of the WHO in the early 1990s, many WHO officials
were initially unconvinced.173 Roemer and Taylor mention “an initial lack of enthusiasm from
most quarters for the idea of international law for tobacco control.”174 Indeed, for most WHO
officials, “the idea of a convention that utilized international law to further public health was
new”, as close supporter Judith Mackay would later state.175 Still, in 1994, both scholars
succeeded in convincing a quite unlikely coalition of States, namely Canada, Mexico, Finland
and Tanzania, to promote the proposal. Resistance persisted within the WHO with several
officials asking Taylor and Roemer to reconsider their proposals, preferring instead “a
nonbinding instrument that could be adopted by WHA as a resolution, or a treaty to be adopted
under the auspices of the United Nations.”176 Despite this opposition, the WHA adopted
resolution WHA49.17 in May 1996, requesting the D-G “to initiate the development of a
framework convention in accordance with Article 19 of the WHO Constitution.”177 Even then it
took three more years, and the support of a new, ambitious D-G, Gro Harlem Brundtland, and
extensive NGO campaigning178, for the drafting process to be put in motion by way of resolution
WHA 52.18(1). Finally, on 21 May 2003, the WHA formally adopted the Framework Convention
on Tobacco Control179 (hereinafter: FCTC) which entered into force on 27 February 2005.
Currently, 179 States and the European Union have ratified the Convention.180
Through ratification of this convention, States pledge to strengthen their anti-tobacco
legislation to the level of a global standard set out in this convention and its implementing
instruments.181 Article 5 of the FCTC requires States Parties to “develop, implement,
periodically update and review comprehensive multisectoral national tobacco control
strategies, plans and programmes.” In order to reduce the tobacco consumption, the
Convention follows a market-oriented approach, attempting to decrease both demand and
offer (or production).
In order to decrease demand for tobacco products, States Parties are encouraged to adopt
price and tax measures (articles 6-7 FCTC) and are required to regulate the contents, labelling
and advertisement of tobacco products (articles 9, 11 and 13 FCTC). In particular the obligation
to “undertake a comprehensive ban of all tobacco advertising, promotion and sponsorship” set
out in article 13.2 FCTC is quite intrusive, even if it is qualified by the phrase “in accordance
with its constitution or constitutional principles.” To reduce the supply of tobacco, States Parties
are obliged to take measures to combat the illicit trade of tobacco products and the sale to and
by minors (articles 15-16 FCTC). Wary of the possible economic counterarguments by the
tobacco industry, the convention requires States Parties to provide “economically viable
173 Ruth Roemer, Allyn Taylor and Jean Lariviere, ‘Origins of the WHO Framework Convention on Tobacco Control’ (2005) 95 American Journal of Public Health 936; World Health Organization, History of the WHO Framework Convention on Tobacco Control (WHO Press 2009) <http://whqlibdoc.who.int/publications/2009/9789241563925_eng.pdf?ua=1&ua=1> accessed 4 August 2015. 174 Roemer, Taylor and Lariviere (n 173) 937. 175 World Health Organization, History of the WHO Framework Convention on Tobacco Control (n 173). 176 Roemer, Taylor and Lariviere (n 173) 937. 177 “International framework convention for tobacco control” (WHA Resolution 49.16) (25 May 1996), available at http://www.who.int/tobacco/framework/wha_eb/wha49_17/en/ 178 van de Pas and van Schaik (n 43) 197. 179 WHO Framework Convention on Tobacco Control (adopted 21 May 2003, entered into force 27 February 2005) 2302 UNTS 166. 180 These data are available online in the UN’s treaty database. See https://treaties.un.org/pages/ViewDetails.aspx?src=TREATY&mtdsg_no=IX-4&chapter=9&lang=en 181 Christine P Bump, ‘Close but No Cigar: The WHO Framework Convention on Tobacco Control’s Futile Ban on Tobacco Advertising’ (2003) 17 Emory Int’l L. Rev. 1251, 1253.

34
alternative activities” for people working in the tobacco industry (article 17 FCTC). Finally,
article 21 FCTC requires States Parties to submit periodic implementation reports, which are
gathered in an online implementation database.182
Despite containing some far-going obligations, this convention only sets out a broad framework
to combat the tobacco epidemic which, as such, requires further implementation and
clarification. This “framework convention” approach was inspired by some of the major
environmental treaties adopted in the early 1990s, such as the Biodiversity Convention and
the UN Framework Convention on Climate Change (UNFCCC).183 However, Roemer and
Taylor note and deplore that “the treaty […] neglects to incorporate many mechanisms used
in other global framework conventions to encourage state parties to comply with their
international legal commitments.”184 Not only were many mechanisms not incorporated, some
mechanisms seem dysfunctional. For example, although the goal was to further specify and
clarify the provisions set out in the FCTC by way of protocols185, only one protocol (on the
elimination of the illicit trade of tobacco products) has been adopted so far and it has only
received 13 ratifications.186 Instead, the WHO has (again) preferred soft law and has opted to
develop non-binding guidelines through intersessional groups of the COP rather than binding
protocols to direct domestic policies.187 Central to these guidelines is the MPOWER188
programme which further elaborates upon the provisions of the FCTC and how to implement
them.189
In institutional terms, although the FCTC has been negotiated under the auspices of the WHO,
it has been donned with an independent institutional structure, consisting most importantly of
a Conference of the Parties190 (COP) and a separate FCTC Secretariat191. The Conference of
the Parties is responsible for monitoring the implementation of the convention.192 The FCTC
Secretariat plays an important role in gathering and organizing the data from the
implementation reports periodically submitted by Members, and in supporting Members in
developing and implementing anti-tobacco policies.
The Secretariat also plays an important role in providing a counterweight to the tobacco
industry. Indeed, it can be argued that this convention was largely inspired by an effort to
counter existing tactics of the tobacco industry to block States from enacting anti-tobacco
regulations. Arguably, one of the main reasons why the tobacco epidemic should be of global
182 See http://apps.who.int/fctc/implementation/database/. 183 Taylor (n 5). 184 Roemer and others (n 33) 938. 185 Several provisions of the FCTC refer to “the Convention and its protocols” (see, for example, articles 2-4 FCTC). Article 33 FCTC sets out the procedure for considering and developing protocols. 186 Admittedly, several of these ratifications have happened quite recently, meaning that the protocol may continue to gather support and eventually still become an important addition to the FCTC. France, for example, has ratified this protocol on 30 November 2015. Belgium has signed the protocol, but not yet ratified it. This information is available at https://treaties.un.org/pages/ViewDetails.aspx?src=TREATY&mtdsg_no=IX-4-a&chapter=9&lang=en 187 See http://www.who.int/fctc/guidelines/groups/en/ 188 MPOWER is an acronym for “Monitor tobacco use and prevention policies, Protect people from tobacco smoke, Offer help to quit tobacco use, Warn about the dangers of tobacco, Enforce bans on tobacco advertising, promotion and sponsorship, and Raise taxes on tobacco”. 189 See WHO, ‘Tobacco Free Initiative (TFI) – MPOWER’, http://www.who.int/tobacco/mpower/en/. 190 This COP has its own Rules of Procedure. These are available at http://www.who.int/fctc/cop/rules_procedure/en/. 191 The FCTC Secretariat does, however, maintain close bonds with the WHO and has been taken up in the WHO’s organigram (albeit with a dotted instead of a solid line). The organigram is available at http://who.int/about/structure/who-organigram.pdf?ua=1. 192 Article 21 FCTC.

35
concern – and should thus fall under the mandate of the WHO – would be the multinational
nature of the tobacco industry. This multinational industry has not only tried to stop the adoption
of the FCTC193, but has also continued to fight its implementation.194 Given this opposition and
the financial means of the multinational tobacco companies, one of the important functions of
the FCTC and its secretariat is to support countries implementing anti-tobacco policies in their
struggle against the tobacco industry. Therefore, several reports regarding the implementation
of the FCTC include tips on “countering industry tactics.”195 Through these initiatives, it
becomes clear that the WHO’s impact in this specific case has not been limited to the provision
of standards to which States could adapt their national legislation. It has also supported States
which encountered tobacco industry resistance. In that respect, the WHO’s impact has
probably been substantial.196
Finally, one essential question remains: what has the impact been in Flanders? As indicated
earlier, this is difficult to measure. However, some elements can be considered. Firstly, the
Flemish Action Plan for tobacco, alcohol, and drugs (2009-2015) explicitly mentions the FCTC
as a starting point for its anti-tobacco actions.197 In accordance with WHO recommendations,
Flanders has explicitly opted for an integral approach, which implies a concerted effort by
several ministries and agencies as well as a combination of different measures.
In addition, one should also consider Belgian and EU legislation in considering the impact of
WHO norms. In this case, the EU is party in its own right to the Framework Convention, and is
responsible for part of the implementation of this convention. EU rules, which have recently
been updated by Directive 2014/40/EU, should thus also be taken into account.198 This
Directive, inter alia, contains norms with regard to the packaging and the contents of tobacco
products.199 At several occasions, it obliges the Commission to “integrate standards agreed by
the parties to the FCTC or by the WHO” on several issues, such as maximum emission levels
of cigarettes.200 Through this obligation for the Commission, WHO’s non-binding standards
elaborated in the wake of the FCTC might indirectly become binding in Flanders. The Belgian
legislation with regard to tobacco products includes important features of an integral anti-
193 Evidence of attempts of the tobacco industry to prevent WHO dealing with issues of tobacco control is provided in a report published in 2000 by the Committee of Experts on Tobacco Industry Documents. This report is available at http://www.who.int/tobacco/en/who_inquiry.pdf. 194 In 2008, the WHO has published a report on the tobacco industry’s interference with tobacco control. This report is available at http://www.who.int/tobacco/publications/industry/interference/en/. See also Y Huang, ‘China’s Position in Negotiating the Framework Convention on Tobacco Control and the Revised International Health Regulations’ (2014) 128 Public Health 161; Tim K Mackey, Bryan A Liang and Thomas E Novotny, ‘Evolution of Tobacco Labeling and Packaging: International Legal Considerations and Health Governance’ (2013) 103 American Journal of Public Health e39; Mary Assunta, ‘Tobacco Industry’s ITGA Fights FCTC Implementation in the Uruguay Negotiations’ (2012) 21 Tobacco Control 563. 195 See, for example, WHO, Report on the Global Tobacco Epidemic, 2015: Raising Taxes on Tobacco (2015) 46–49. 196 World Health Organization (n 33) 18. 197 Flemish Agency for Care and Health, ‘Vlaams actieplan tabak, alcohol en drugs 2009-2015’, available at www.zorg-en-gezondheid.be/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=20725. 198 Directive 2014/40/EU of the European Parliament and of the Council of 3 April 2014 on the approximation of the laws, regulations and administrative provisions of the Member States concerning the manufacture, presentation and sale of tobacco and related products and repealing Directive 2001/37/EC, OJ 29 April 2014, L127/1, available at http://ec.europa.eu/health/tobacco/docs/dir_201440_en.pdf. 199 The Directive is recognized by the WHO as a FCTC implementing instrument, and thus features in the implementation database. See http://apps.who.int/fctc/implementation/database/groups/european-union-specifications-health-warnings-cigarette-packages-adopted-today. 200 Article 3.4 Directive 2014/40/EU. See also articles 4.5 (on measurement methods).

36
tobacco policy, such as taxes on tobacco products, and packaging regulations.201 Currently,
the legislation with regard to smoking in public places is also Belgian, but this competence will
probably be handed over to the Flemish Community with the State reform.202
With regard to the impact in Flanders, we should finally refer to a recent case before the
Constitutional Court.203 The case concerned the Belgian legislation with regard to smoking in
public spaces, which is largely prohibited. One of the exceptions to this rule, which allows for
smoking in bars which do not offer snacks, was challenged in this case. The Constitutional
Court based its judgment inter alia on article 23 of the Belgian Constitution, which guarantees
the right to health. In line with its earlier case law, it considered that this provision should be
read taking into account relevant international treaties to which Belgium is party. As such, the
FCTC formed an integral part of article 23 according to the Court. However, it added an
interesting note, stating that the guidelines for implementation of the FCTC equally form part
of the right to health ensured in article 23 of the Belgian Constitution, as they concretized the
FCTC.204 As such, implementing instruments of the FCTC should mandatorily be taken into
account when developing Belgian tobacco legislation.
We end this section by referring to the fact that, on 10 August 2015, an expert group on impact
assessment of the WHO FCTC has started its work.205 It has been established by the 6th FCTC
COP, which stated that “the purpose of the impact assessment should be to assess and
examine the impact of the WHO FCTC on implementation of tobacco control measures and
on the effectiveness of its implementation in order to assess the impact of the Convention as
a tool for reducing tobacco consumption and prevalence after its first 10 years of operation.”206
Unfortunately, this expert group has not yet produced any substantial results that could further
inform the findings of this section.
2.2.2 Proposals for other conventions
When the Framework Convention on Tobacco Control was adopted, several people hoped that
this ushered in a new era in which international law (in the sense of binding international
instruments) would play a greater role in tackling global health issues. In spite of these high
hopes, the WHO has not made use of article 19 since the adoption of the FCTC. Still, some
scholars keep arguing for the development of binding international instruments, sometimes
even when providing expertise to the WHO itself.
In a report from April 2012, the Consultative Expert Working Group on Research and
Development: Financing and Coordination released a report dealing with the issue of
underinvestment in pharmaceutical research with regard to diseases that mainly concern
201 For an overview of the relevant Belgian legislation, see http://www.health.belgium.be/eportal/Myhealth/Tobacco/index.htm?ssUserText=type_IE2Law#.VnrBKlnZaDc. 202 All competences with regard to prevention in public health care should be transferred to the Communities. See Flemish Agency for Care and Health, ‘Impact van de zesde staatshervorming op Zorg en Gezondheid’, http://vitalink.be/staatshervorming/. 203 Constitutional Court (BE) 15 March 2011, Judgment No. 37/2011. This judgment is available at http://www.const-court.be/public/n/2011/2011-037n.pdf. 204 Ibid., para B.6.2. 205 http://www.who.int/fctc/mediacentre/news/2015/assmntgva/en/. 206 ‘Impact assessment of the WHO FCTC’ (Decision, 18 October 2014), WHO Docs. FCTC/COP6(13), available at http://apps.who.int/gb/fctc/PDF/cop6/FCTC_COP6%2813%29-en.pdf, para 4.

37
developing countries.207 This report set out why the current system, which is mainly based on
market mechanisms, has failed to provide sufficient incentives to pharmaceutical companies
to devote funds to this research and discussed a number of alternative ways of financing this
research. In chapter 6 of this report, the authors weigh the advantages and disadvantages of
a soft or hard law approach to securing sufficient funding. They unequivocally recommend a
hard law approach, stating that the WHO should adopt a binding agreement based on article
19. Although the WHA has taken these recommendations into account, its response has been
somewhat lukewarm. The item has remained on its agenda, but the current discussions
concern the establishment of a fund sponsored by voluntary contributions, thus leaving binding
instruments out of their scope.208
Closely related are the proposals to develop a framework convention on global health. An
entire campaign has formed around this idea (the Platform for a Framework Convention on
Global Health209), which is mainly carried by the Joint Action and Learning Initiative on National
and Global Responsibilities for Health (JALI)210 and advocated by Lawrence Gostin in
academic circles211. The main goal of developing such a framework convention would be to
combat the problem of vast health inequities by “empowering people struggling for their health
and rights through a binding legal foundation”212. This debate even appeared in the Bulletin of
the WHO in the guise of an article published by Lawrence Gostin and several other scholars
explaining the main idea behind the framework convention.213 Indeed, one of the goals of the
Platform is to empower the WHO in its role in global health governance.214 However, despite
the continuous advocacy by these groups and scholars, currently, the governing bodies of the
WHO have not taken action towards such a convention.
Finally, there have been scholars who have suggested developing an international legal
framework (by way of a framework convention or otherwise) for obesity control215, alcohol
control216, and in the field of antimicrobial resistance217. It remains to be seen, however,
207 This Consultative Expert Working Group was established by resolution WHA 63.28 in 2010 and built on the work of an earlier Expert Working Group dealing with the same issue. The research of both working groups was underpinned by the objectives set out in the Global Strategy and Plan of Action on Public Health, Innovation and Intellectual Property (GSPA-PHI). Consultative Expert Working Group on Research and Development: Financing and Coordination, ‘Research and Development to Meet Health Needs in Developing Countries: Strengthening Global Financing and Coordination’ (April 2012) 8. 208 See ‘Follow-up of the report of the Consultative Expert Working Group on Research and Development: Financing and Coordination’ (Report by the Director-General, 10 April 2015), WHO Docs. WHA A68/34, available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_34-en.pdf. 209 See http://www.globalhealthtreaty.org/ 210 See http://jalihealth.org/index.php 211 Lawrence O Gostin and Eric Friedman, ‘Towards a Framework Convention on Global Health: A Transformative Agenda for Global Health Justice’ (2013) 13 Yale Journal of Health Policy, Law, and Ethics 1; Gostin and others (n 31); Lawrence O Gostin, ‘A Proposal for a Framework Convention on Global Health’ (2007) 10 J Int Economic Law 989; Lawrence O Gostin, ‘A Framework Convention on Global Health: Health for All, Justice for All’ (2012) 307 JAMA 2087. 212 Platform for a Framework Convention on Global Health, ‘Platform for a Framework Convention on Global Health: Realizing the Universal Right to Health. Fundamental Principles and Joining the Platform’ (14 May 2014) 1. 213 Gostin and others (n 170). 214 ibid 3. 215 Steven J Hoffman and others, ‘A Framework Convention on Obesity Control?’ (2011) 378 The Lancet 2068. 216 Allyn L Taylor and Ibadat S Dhillon, ‘An International Legal Strategy for Alcohol Control: Not a Framework Convention—at Least Not yet’ (2013) 108 Addiction 450; Allyn L Taylor and Ibadat S Dhillon, ‘Twenty-First Century International Lawmaking for Alcohol Control’ (2013) 108 Addiction 461. 217 Steven J Hoffman and others, ‘An International Legal Framework to Address Antimicrobial Resistance’ (2015) 93 Bull World Health Organ 66.

38
whether the WHO will be willing to develop any further conventions. At the moment, it seems
that the WHO has returned to its familiar policy of working through soft law.
2.3 The International Health Regulations and the role of the WHO
in public health emergencies
2.3.1 The role of the WHO in health emergencies
As explained earlier, the WHO has only adopted two regulations in accordance with article 21
of its Constitution.218 From these two types of regulations, the International Health
Regulations219 (IHR) are undoubtedly the most important. They serve as the framework for the
exercise of WHO’s coordinating role in monitoring and combatting global epidemics, and –
since the revision of 2005 – also for other types of disasters, such as nuclear disasters, which
might trigger the international spread of disease. As stated in the foreword to the International
Health Regulations, “a central and historic responsibility for the World Health Organization
(WHO) has been the management of the global regime for the control of the international
spread of disease.”220 Since 2005, the IHR have adopted an all-hazard approach, abandoning
the focus on clearly defined diseases, and including other types of health hazards.
The history of the international legal and institutional framework with regard to health
demonstrates the central role which the fight against epidemics has played in the field of
(international) public health law. Together with the laws of war, epidemiological surveillance
has been one of the first areas in which the fledgling international legal system of the late 19th
century moved beyond mere co-existence between States towards actual cooperation.221 This
cooperation was triggered by the vicious cholera epidemics in Europe between 1830 and
1847.222 Initially, multilateral conferences were organized, which were considered quite
innovative at that point in time.223 These multilateral conferences were followed-up by others
during which the implementation and effectiveness of the agreed measures were discussed.
This follow-up gradually became systematic and led to the development of actual institutions,
such as the OIHP and the LNHO discussed above, which were to predecessors of the WHO.224
When this institution was finally established in 1946, epidemics surveillance and control, and
more generally the fight against the international spread of disease, became central to its
mandate.
However, the WHO’s role has not been limited to epidemics only. Rather, as the international
system for humanitarian aid and crisis response grew, the WHO started playing an important
role in humanitarian crises with public health consequences, even when the IHR were not
triggered. Indeed, in a recent report delivered by the D-G to the WHA on the WHO response
in severe, large-scale emergencies, only 3 out of 31 emergencies to which the WHO has
218 However, the WHO has been mandated to develop regulations for five different topics. 219 Revision of the International Health Regulations (23 May 2005) WHO Docs. WHA58.3, available at http://www.who.int/csr/ihr/en/. 220 Ibid., 1 (foreword). 221 This terminology is borrowed from Wolfgang Friedmann. See Wolfgang Friedmann, The Changing Structure of International Law (Columbia University Press 1964). 222 WHO, ‘Frequently asked questions about the International Health Regulations (2005), available at http://www.who.int/ihr/about/FAQ2009.pdf?ua=1&ua=1. 223 Kickbusch and Ivanova (n 26). 224 See section 1.1.

39
responded and in which it is still engaged, concern “public health emergencies” (MERS, Avian
Influenza and Ebola), while the others concern both man-made (conflict/civil-strife) or natural
(storms, earthquakes, …) disasters with public health implications.225 This is further
exemplified by the recommendations made (by HQ226) and technical assistance offered (by the
European Regional Office) in the current refugee crisis in Europe227, or the humanitarian crisis
in Ukraine.228 Moreover, within the global humanitarian system, the WHO has become the
leading organization of the health cluster of the Inter-Agency Standing Committee (IASC) for
humanitarian emergencies.229
In 2013, the WHO has attempted to develop an overarching framework for all types of
emergencies with public health implications in the Emergency Response Framework (ERF).230
As an overarching framework, it was also meant to subsume instances covered by the IHR.
However, during the Ebola crisis, coordination of the WHO’s outbreak response (under the
IHR) and emergency response (under the ERF) has proven problematic. As such, attempts
are being taken to further integrate the WHO’s structures for these two issues.231
Other organizations also play an important role in health emergencies. Sketching a complete
picture would prove overly ambitious, but some organizations can and should be mentioned
here. The Centers for Disease Control, for example, develop guidelines on safe treatment of
pandemics victims and for surveilling the state or region in which they operate.232 Within the
European context, the European Center for Disease Control (ECDC), which is an independent
agency established by the EU,233 is “charged with identifying, assessing, and communicating
current and emerging threats to human health from communicable diseases”, which is
essentially a surveillance task.234 Some initiatives have also been developed to aid States in
225 See Annex to ‘WHO response in severe, large-scale emergencies’ (Report of the Director-General, 15 May 2015), WHO Docs. WHA 68/23, available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_23-en.pdf. 226 WHO, ‘Frequently asked questions on migration and health’ (September 2015), http://who.int/features/qa/88/en/ 227 “Population movement is a challenge for refugees and migrants as well as for the receiving population” (Statement by Zsuzsanna Jakab, WHO Regional Director for Europe, 2 September 2015), available at http://www.euro.who.int/en/health-topics/health-determinants/migration-and-health/news/news/2015/09/population-movement-is-a-challenge-for-refugees-and-migrants-as-well-as-for-the-receiving-population 228 See WHO European Region, ‘Humanitarian crisis in Ukraine’, available at http://www.euro.who.int/en/countries/ukraine/humanitarian-crisis-in-ukraine. 229 The Inter-Agency Standing Committee (IASC) is the primary mechanism for inter-agency coordination of humanitarian assistance. See https://interagencystandingcommittee.org/. The WHO’s role is described in the Emergency Response Framework. See http://www.who.int/hac/about/erf_.pdf 230 The ERF refers to several other relevant WHO instruments for WHO’s leading role in emergencies, namely “Article 2(d) of WHO’s Constitution and World Health Assembly Resolutions: 34.26, 46.6, 48.2, 58.1, 59.22, 64.10, 65.20.” WHO, Emergency Response Framework (2013), http://www.who.int/hac/about/erf_.pdf, 11. 231 Lawrence Gostin, ‘JAMA Forum: Critical Choices for the WHO After the Ebola Epidemic’ <http://newsatjama.jama.com/2015/05/27/jama-forum-critical-choices-for-the-who-after-the-ebola-epidemic/> accessed 23 December 2015.See http://www.oneillinstituteblog.org/jama-forum-critical-choices-for-the-who-after-the-ebola-epidemic/ 232 The CDC’s guidelines for safe treatment of (possible) Ebola patients have been updated in October 2014. See http://www.cdc.gov/vhf/ebola/healthcare-us/hospitals/infection-control.html 233 It was established by Council Regulation No 851/2004 (http://ecdc.europa.eu/en/aboutus/Key%20Documents/0404_KD_Regulation_establishing_ECDC.pdf). See also Communication from the Commission to the European Parliament and the Council on the International Health Regulations (26 September 2006) COM(2006)552final, 9. 234 Communication from the Commission to the European Parliament and the Council on the International Health Regulations (26 September 2006) COM(2006)552final, 9.

40
implementing the IHR, such as the Global Health Security Initiative.235 Other initiatives are
designed to pool the resources of several international organizations meant to tackle global
crises. Central in this regard is the Global Outbreak Alert and Response Network (GOARN),
which is “a ‘one-stop shop’ of global resources to help respond to a public health
emergency.”236 Regional organizations are also relevant. The EU, for example, plays an
important role vis-à-vis its members, as it inter alia established the ECDC.237 A communication
from the Commission from 26 September 2006 outlines its vision on the role of the EU in the
implementation of the International Health Regulations.238 Within the European Commission,
the Directorate-General for Health and Food Safety (DG Sanco) is responsible for the
implementation of the policies. Finally, some non-state actors, such as Médecins Sans
Frontières, play an important role in combatting diseases outbreaks on the ground. Indeed,
“since WHO is not primarily an operational agency, its collaboration with, and reliance on, non-
governmental partners for its emergency and humanitarian action is of crucial importance.”239
In what follows, this report will explore the role of the WHO in combatting health emergencies,
mainly through the IHR. The recent Ebola crisis will be used to draw examples from.240 The
section will start by discussing the IHR and the main obligations flowing therefrom for both
Member States and the WHO itself. Secondly, the WHO’s response to the recent Ebola crisis
in Western Africa will be discussed. Finally, we will shortly discuss the ongoing debate on the
reform of the WHO’s emergency response mechanisms and capacities.
2.3.2 The International Health Regulations
Article 21(a) of the WHO Constitution grants the Health Assembly the authority to adopt
regulations concerning “sanitary and quarantine requirements and other procedures designed
to prevent the international spread of disease.” In accordance with article 22, these regulations
“come into force for all Members after due notice […] except for such Members as may notify
the Director-General of rejection or reservations within the period stated in the notice.” In other
235 GHSI, ‘GHSI Background’, http://www.ghsi.ca/english/background.asp. 236 WHO, ‘International Health Regulations. Guidance for national policy-makers and partners’, 2008, available at http://www.who.int/ihr/lyon/WHO_CDS_EPR_IHR_2007_2EN.pdf, 13. Gostin et al define GOARN as “a technical collaboration of institutions that pool human and technical resources for the rapid identification, confirmation, and response to disease outbreaks of international importance.” See Gostin, Sridhar and Hougendobler (n 160) 856. 237 European Commission, “Health Security in Belgium”, http://ec.europa.eu/chafea/documents/health/leaflet/2014_health_security-be_informationsheet_en.pdf. Conversely, the European Regional Office of the WHO recognizes the European Commission (as well as the ECDC) as key partners in the fight against health emergencies. See http://www.euro.who.int/en/health-topics/emergencies/ebola-outbreak-2014. 238 Communication from the Commission to the European Parliament and the Council on the International Health Regulations (26 September 2006) COM(2006)552final, available at http://ec.europa.eu/health/eu_world/key_documents/index_en.htm. 239 Burci and Vignes (n 12) 91. These authors further add that “[s]uch interaction takes place both at a central planning and coordination level, through WHO’s participation in the Inter-Agency Standing Committee on Humanitarian Questions as well as regarding its activities in specific emergencies, be they natural, man-made or complex emergencies. Major partners in this context are the International Committee of the Red Cross (ICRC), the International Federation of Red Cross and Red Crescent Societies (IFRC), Care International, Caritas, Oxfam and the World Council of Churches.” 240 A report from the Ebola Interim Assessment Panel established by the WHO, published on 7 July 2015, will provide important information on the WHO’s intervention and its adequacy. Report of the Ebola Interim Assessment Panel, http://www.who.int/csr/resources/publications/ebola/report-by-panel.pdf?ua=1

41
words, this constitutes an opt-out system: Member States are bound by these regulations
unless they explicitly opt out.241 Only two States, India242 and the United States243, made any
reservations to the document.244
On the basis of these articles, the WHA adopted the IHR in 1969, as successor to the
International Sanitary Regulations which had been adopted in 1951. These regulations, in turn,
were “derived from a pre-WHO set of rules.”245 Since 1969, the IHR have been revised three
times. Although the first two revisions (in 1973 and 1981) did not introduce any major changes,
the last revision which was adopted in 2005 and entered into force on 15 July 2007 did contain
some major innovations.246 In contrast to earlier versions which were mainly concerned with
six serious infectious diseases (cholera, plague, yellow fever, smallpox, relapsing fever and
typhus), the 2005 IHR are no longer limited in application to specific diseases.247 Instead, the
‘new’ IHR have adopted a broad definition of the concept of ‘disease’, namely “an illness or
medical condition, irrespective of origin or source, that presents or could present significant
harm to humans.”248 Thus, according to Burci and Quirin, “the openness of these concepts
means that the regulations now follow an “all-hazards approach,” under which the accidental
or intentional release of biological, chemical, or radiological agents would fall within the purview
of the instrument if it could lead to the international spread of disease.”249 Transboundary health
effects of biological or nuclear weapons would thus fall under the purview of the new IHR. In
further contrast with earlier versions of the IHR, the IHR 2005 also require Member States to
develop core capacities to deal with sudden outbreaks of diseases (see infra).
The purpose of the IHR is “to prevent, protect against, control and provide a public health
response to the international spread of disease in ways that are commensurate with and
restricted to public health risks, and which avoid unnecessary interference with international
traffic and trade.”250 In other words, the IHR attempt to balance two objectives: combatting (the
spread of) disease and minimizing interference with international traffic and trade. Indeed, this
article reflects one of the historical reasons for developing an international legal framework to
cope with epidemic diseases: to prevent unnecessary interferences with international trade
which might have considerable negative effects on the economy of the affected state.251
According to the WHO, the IHR contain five main elements: a notification requirement for
States, the obligatory establishment of national IHR focal points, a requirement for national
241 This opt-out system is quite rare, especially given the high possible incursion on state sovereignty. See Eric Mack, ‘The World Health Organization’s New International Health Regulations: Incursion on State Sovereignty and Ill-Fated Response to Global Health Issues’ (2006) 7 Chicago Journal of International Law 365. 242 The Indian reservation is available at http://www.who.int/ihr/india_Dec2006.pdf?ua=1. 243 The American reservation is available at http://www.who.int/ihr/usa.pdf?ua=1. 244 WHO, ‘States Parties to the International Health Regulations (2005), http://www.who.int/ihr/legal_issues/states_parties/en/. 245 Klock (n 165) 829. 246 A list of all innovations can be found in the foreword to the IHR 2005. In general, the changes were received with great enthusiasm in the academic community. David P Fidler, ‘From International Sanitary Conventions to Global Health Security: The New International Health Regulations’ (2005) 4 Chinese Journal of International Law 325. 247 WHO, Frequently Asked Question about the International Health Regulations (2005), http://www.who.int/ihr/about/FAQ2009.pdf?ua=1, 1. 248 Article 1 IHR (2005). 249 Gian Luca Burci and Jakob Quirin, ‘Ebola, WHO, and the United Nations: Convergence of Global Public Health and International Peace and Security’ (2014) 18 ASIL Insights <http://www.asil.org/insights/volume/18/issue/25/ebola-who-and-united-nations-convergence-global-public-health-and>. 250 Article 2 IHR. 251 Kickbusch and Ivanova (n 26).

42
core capacities to detect and react to outbreaks, a mandate for the WHO to develop
recommended measures in case of a “public health emergency of international concern”, and
the establishment of an independent external review system concerning IHR
implementation.252
Historically central to the IHR is the obligation to notify certain public health events to the WHO,
which has been codified in article 6 of the IHR. Article 5 of the IHR requires States to develop
sufficient national capacities to surveil their territory effectively in order to swiftly detect any
possible public health emergencies. The modalities of these capacities are set out in Annex I.
Relevant events have to be evaluated making use of the instrument provided in annex 2, which
contains a simple decision tree. When certain conditions are met, States are obliged to notify
these events to the WHO through their National IHR Focal Points. These have to be
established in accordance with article 4 IHR, and are States’ central contact point for the WHO
in the case of health emergencies. The WHO may also receive information about possible
public health emergencies through other channels (article 9 IHR).253 In this case, the WHO is
bound to verify reports originating from other sources with the state in question (article 10 IHR).
This verification obligation for the WHO is meant to maintain trust between the WHO and the
state in question.
A major issue with regard to notification is the fear of States to suffer greatly economically if a
public health event would receive too much publicity. Often other States react to this kind of
information by adopting stringent anti-travel and anti-trade measures, which can seriously
harm the plagued state’s economy and even its ability to counter the epidemic, as has
happened in the case of Ebola (see section 2.3.3). The IHR attempt to limit the amount of trade
restrictions to what is strictly necessary. The outline of what is strictly necessary is generally
set out in temporary recommendations, adopted in accordance with article 15 IHR. These
recommendations may concern trade and travel restrictions as well as clinical practices,
procedures to ensure the safety of health care workers, etc. These recommendations are
adopted by the D-G on the basis of the advice of the Emergency Committee (see infra), and
although they are not binding254, they “represent authoritative guidance and enhance
accountability by requiring States going beyond them to justify their actions.”255 Indeed, article
43.1 IHR allows States Parties to adopt more stringent restrictions on travel only if these
restrictions can be justified.256 The enforcement of this principle has, however, not been an
easy task for the Secretariat.
These temporary recommendations can only be adopted “if it has been determined in
accordance with article 12 that a public health emergency of international concern is
occurring.”257 A public health emergency of international concern – or PHEIC as it is commonly
252 WHO, Frequently Asked Question about the International Health Regulations (2005), http://www.who.int/ihr/about/FAQ2009.pdf?ua=1&ua=1, 2. 253 According to Kamradt-Scott, the ability to make use of NGO reports and information has been accepted due to the dedicated pursuit of this possibility by a small group of WHO Secretariat individuals. See Adam Kamradt-Scott, ‘The WHO Secretariat, Norm Entrepreneurship, and Global Disease Outbreak Control’ (2010) 1 Journal of International Organizations Studies 72. 254 Article 1 IHR defines temporary recommendations as “non-binding advice issued by WHI pursuant to Article 15 for application on a time-limited, risk-specific basis, in response to a public health emergency of internation concern, so as to prevent or reduce the international spread of disease and minimize interference with international traffic.” 255 Burci and Quirin (n 249). 256 “Article 43 International Health Regulations (2005) requires all countries to behave with appropriate responsibility towards the international community in the adoption of travel and trade restrictions.” See Report of the Ebola Interim Assessment Panel, http://www.who.int/csr/resources/publications/ebola/report-by-panel.pdf?ua=1, para 16. 257 Article 15 IHR.

43
abbreviated – is “an extraordinary event which is determined […] (i) to constitute a public health
risk to other States through the international spread of disease and (ii) to potentially require a
coordinated international response.”258 This determination is made by the D-G, who “shall
make the final determination on these matters.”259 However, both in making this determination
and in the development of recommendations, the Emergency Committee takes centre stage.260
A separate Emergency Committee is set up for specific outbreaks or diseases as required.261
It constitutes the main advisory body for the D-G in these instances and exercises substantial
influence; its recommendations are generally simply endorsed by the D-G.
Finally, ports and airports, and their operators, equally have to develop capacities to handle
cases.262 For Belgium, Saniport is responsible for monitoring international travel from and to
affected areas through Belgian ports and the Brussels-National airport.263
The IHR are not the only framework in use by the WHO in determining its response to health
emergencies. The Emergency Response Framework, mentioned above, has been developed
in an attempt to harmonize the WHO’s humanitarian and IHR response systems and to “clarify
WHO’s roles and responsibilities in this regard and to provide a common approach for its work
in emergencies.”264 It sets out a grading system for emergencies on the basis of the gravity of
the event, which determines the framework for the response. In addition, the WHO has
developed a separate ‘preparedness framework’ for influenza in 2011 with a separate grading
system, which consists of six different phases.265
2.3.3 The Ebola Virus Disease (EVD) outbreak266
258 Article 1 IHR. Since the adoption of the new IHR, only four epidemics have been declared “public health emergency of international concern”: the pandemic flue of 2009, the poliovirus in the Middle East in 2014, and the Ebola outbreak in Western Africa. Recently, on 1 February 2016, the D-G declared the current Zika viruse epidemic a PHEIC. See WHO, ‘WHO Director-General summarizes the outcome of the Emergency Committee regarding clusters of microcephaly and Guillain-Barré syndrome’ (1 February 2016), http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/. 259 Article 49.5 IHR 260 The Emergency Committee is established in accordance with article 48 IHR. The affected country is also always closely involved in these decisions. 261 One report suggested the establishment of one Standing Emergency Committee for all health emergencies. See Suerie Moon and others, ‘Will Ebola Change the Game? Ten Essential Reforms before the next Pandemic. The Report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola’ (2015) 386 The Lancet 2204, 2204, recommendation 4. 262 Article 20 IHR. 263 FOD Volksgezondheid, Veiligheid van de Voedselketen en Leefmilieu, “Saniport (Port Health Authority)”, http://health.belgium.be/eportal/Healthcare/CrisisManagement/Internationalactors/Saniport/19069829?ie2Term=inspectie?&fodnlang=nl#.Vo-XTVnZaDc. 264 Emergency Response Framework, 7. 265 A schematic description of the different phases is available at http://www.who.int/influenza/resources/documents/pandemic_phase_descriptions_and_actions.pdf. See also David P Fidler and Lawrence O Gostin, ‘The WHO Pandemic Influenza Preparedness Framework: A Milestone in Global Governance for Health’ (2011) 306 JAMA <http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2011.960> accessed 4 September 2015. 266 This case study was selected on the basis of the interviews, as several interviewees noted its importance.

44
On 23 March 2014, the WHO’s African Regional Office reported that the first case of Ebola
Virus Disease (EVD) in the Forestière region of Guinea267 had been documented two days
earlier. Meanwhile, reports have shown that “cases may have occurred as early as December
2013.”268 The following months, the disease spread violently; the website of the WHO features
a story map of the spread of the disease (as well as of the international response)269. On 29
March 2014, the first case was reported in Liberia. This was followed on 25 May 2014 by the
first documented case in Sierra Leone. In these three countries, which had only recently started
recovering from different political problems270, the outbreak soon spiraled out of control. The
disease also spread to other West-African countries, and cases were reported in Nigeria (on
27 July 2014), Senegal (on 30 August 2014) and Mali (on 23 October 2014). However, in these
countries, the outbreak was soon contained. Some cases were also reported in Western
countries, namely Spain (6 October 2014) and the United States (30 September 2014), but
again, these cases were quickly contained.
What is Ebola virus disease (EVD)? On its website, the WHO provides a fact sheet on EVD. It mentions fruit bats as the probably original host of the ebola virus. Humans are infected by “close contact with the blood, secretions, organs or other bodily fluids of infected animals such as chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the rainforest.” Ebola then spreads from human to human, “via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.” The incubation period is 2 to 21 days and humans only become infectious once they show symptoms. Symptoms include “the sudden onset of fever fatigue, muscle pain, headache and sore throat [and later,] vomiting, diarrhoea, rash, symptoms of impaired kidney and liver function, and in some cases, both internal and external bleeding (e.g. oozing from the gums, blood in the stools).” EVD has historically been limited to more central parts of Africa, with the Democratic Republic of the Congo (DRC) being mainly affected. It first appeared there in 1976 near the Ebola river, from which the disease’s name is derived.271 (Source: WHO, “Ebola virus disease” (Fact sheet no 103), available at http://who.int/mediacentre/factsheets/fs103/en/, last updated April 2015)
267 This is the region near the border with Liberia and Sierra Leone. 268 “WHO response in severe, large-scale emergencies” (Report of the Director-General), 15 May 2015, WHO Documents A68/23, available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_23-en.pdf, para 27. 269 See http://www.who.int/features/ebola/storymap/en/ 270 Indeed, the loss of control can partly be attributed to a lack of national capacities for monitoring, surveillance, and treating cases after several years of political turmoil. See Marie-Paule Kieny and others, ‘Health-System Resilience: Reflections on the Ebola Crisis in Western Africa’ (2014) 92 Bulletin of the World Health Organization 850. 271 See also http://www.who.int/features/ebola/storymap/en/

45
The WHO responded to the first documented case of EVD in Guinea by declaring the outbreak
a Grade 2 emergency in accordance with the ERF on 25 March 2014.272 Exactly two months
later, a Regional Ebola Response Center was opened by the WHO as the outbreak was scaled
up to a Grade 3 emergency.273 Finally, the D-G established an Emergency Committee on 6
August 2014, which declared the EVD outbreak a PHEIC at its first (teleconference) meeting
only two days later.274
In September, a powerful response to the worsening crisis became more and more pressing:
the amount of cases was growing exponentially and D-G Margaret Chan described the
outbreak as “unprecedented”.275 Still, an adequate response proved impossible due to a lack
of means (financial and other). As David Nabarro, the UN Secretary-General’s Special Envoy
on Ebola, stated on 31 July 2015 that “the response was increasing at a relatively slow pace,
and we were in real danger, as a global community, of being overwhelmed by the outbreak, so
extraordinary measures were needed.”276 Consequently, at the request of the D-G, the issue
was taken up by the UN Secretary-General. Earlier attempts to enhance involvement of the
UN system by appointing David Nabarro as Senior United Nations System Coordinator for
Ebola on 12 August 2014 and Anthony Banbury (United States) as Deputy Ebola Coordinator
and Operation Crisis Manager on 8 September 2014277 did not suffice to attract the means
necessary to combat the Ebola crisis and to ensure effective coordination of the efforts of all
actors involved. Therefore, Secretary-General Ban Ki-Moon decided to set up a UN mission.
On 17 September 2014, he sent an identical letter to the UN Security Council and the UN
General Assembly, explaining the situation and the urgency and informed them of his intention
to set up the UN Mission for Ebola Emergency Response (UNMEER).278 Both institutions
declared their support for the Secretary-General’s plan on the next day, and UNMEER was
officially established on 19 September 2014.279
This response by the UN system was exceptional. Firstly, UNMEER was the first UN Mission
ever established to combat an epidemic. Traditionally, these missions have been limited to
humanitarian crises caused by armed conflicts. Secondly, it was only the second time the UN
Security Council dealt directly with a public health issue.280 In Resolution 2177, the UN Security
272 ‘WHO response in severe, large-scale emergencies’ (Report of the Director-General), 15 May 2015, WHO Documents A68/23, available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_23-en.pdf, para 28. 273 Ibid. As we will discuss later, the WHO has been widely criticized for its late response. 274 ‘Statement on the 1st meeting of the IHR Emergency Committee on the 2014 Ebola outbreak in West Africa’ (WHO statement), 8 August 2014, available at http://www.who.int/mediacentre/news/statements/2014/ebola-20140808/en/. 275 The D-G made this statement at the occasion of her speech delivered to the Presidents of Guinea, Liberia, Sierra Leone, and Cote d’Ivoire’. The text of the speech is available at http://reliefweb.int/report/guinea/who-director-general-dr-margaret-chan-speech-ebola-virus-disease-outbreak-delivered. 276 WHO, ‘Virtual Press Conference regarding WHO reform for emergencies with health consequences’ (31 July 2015), available at http://www.who.int/mediacentre/multimedia/vpc-31-july-2015.pdf?ua=1. 277 ‘Secretary-General Appoints Anthony Banbury of United States Deputy Ebola Coordinator and Operation Crisis Manager’ (UN Secretary-General Press Release, 8 September 2014), http://www.un.org/press/en/2014/sga1503.doc.htm 278 Identical letters dated 17 September 2014 from the Secretary-General addressed to the President of the General Assembly and the President of the Security Council, UN Docs. A/69/389 – S/2014/679, available at http://www.securitycouncilreport.org/atf/cf/%7B65BFCF9B-6D27-4E9C-8CD3-CF6E4FF96FF9%7D/S_2014_679.pdf 279 See Global Ebola Response, ‘UN Mission for Ebola Emergency Response (UNMEER)’, http://ebolaresponse.un.org/un-mission-ebola-emergency-response-unmeer. 280 The only other health issue the UN Security Council discussed was the HIV/AIDS pandemic.

46
Council termed the Ebola crisis a “threat to international peace and security.”281 This led Gian
Luca Burci and Jakob Quirin to note “a convergence of global public health and international
peace and security.”282 This unparalleled response was triggered by the exponentially growing
number of cases and the fact that it took place in a politically fragile region.283 In the meantime,
however, UNMEER has already wound down on 31 July 2015, as the first successful trials of
a possible vaccine were announced by WHO D-G Margaret Chan and the outbreak seemed
to come under control. It handed leadership and the role of coordinator back over to the
WHO284 due to “having achieved its core objective of scaling up the response on the ground.”285
And, recently, the WHO declared the three central countries in this crisis Ebola-free286,
although possible new Ebola cases have already emerged.287
Substantively, the response had three legs: response and support for the affected countries,
building preparedness in countries at risk of spread, and development of possible medicines
and vaccines.288
In terms of response in the affected countries, the WHO had an important coordinating role. It
coordinated the efforts of the different actors, such as Médecins sans Frontières289 on the
ground (and elsewhere) through its leading role in UNMEER at first, and in its own capacity
later on. In addition, it provided technical assistance on the ground. They did not only provide
material, but also had their own people on the ground, who helped inter alia with contact
tracing.290 These WHO officials also provided support to national health care personnel. As the
response became more effective, and more people survived their illness, the WHO also started
working on taking care of the survivors.291
In terms of preparedness, the WHO provided technical assistance to neighboring countries to
which the disease could spread. WHO helped the ministries of health develop capacities to
monitor, surveil, and treat (possible) cases. In addition, and more importantly for Flanders, the
D-G issued temporary recommendations concerning treatment of Ebola patients292, as well as
281 UNSC Res 2177 (18 September 2014) UN Doc S/RES/2177. 282 Burci and Quirin (n 67). 283 Due to the political fragility of the region, and recent conflicts, the health systems in these States were also insufficiently developed. See Kieny and others (n 270). 284 See ‘Ebola: UN Emergency Response Mission Winds down as WHO Announces Possible “game Changer” Vaccine’ (Global Ebola Response, 31 July 2015) <https://ebolaresponse.un.org/ebola-un-emergency-response-mission-winds-down-who-announces-possible-game-changer-vaccine> accessed 3 September 2015. 285 See also http://www.un.org/sg/statements/index.asp?nid=8874 286 As the last country, Guinea was declared free of Ebola on 29 December 2015. See WHO African Region, ‘End of Ebola transmission in Guinea’, http://www.afro.who.int/en/media-centre/pressreleases/item/8252-end-of-ebola-transmission-in-guinea.html. The declaration o f the head of Guinea’s country office is available at http://www.afro.who.int/en/media-centre/pressreleases/item/8255-declaration-dr-mohammed-belhocine-end-of-ebola-outbreak-in-guinea.html. 287 X., ‘Officieel: nieuw geval van ebola in Sierra Leone’ (De Morgen, 15 January 2016), http://www.demorgen.be/buitenland/waarschijnlijk-nieuw-geval-van-ebola-in-sierra-leone-b65b4076/ 288 The WHO provides some numbers with regard to the substantial response in an infographic on its website. See http://apps.who.int/ebola/our-work/achievements. 289 “Doctors Without Borders have done more on the response side than any other agency.” https://www.youtube.com/watch?v=utEmDruf7Ss (26:10) 290 WHO, ‘Emergencies, Preparedness, Response – Contact tracing’, available at http://www.who.int/csr/disease/ebola/training/contact-tracing/en/. 291 WHO, ‘Ebola survivors clinic opens in Moravia’ (August 2015), http://who.int/features/2015/ebola-survivors-clinic/en/. 292 We can already note here that the suggested health safety measures were considered too light by certain Flemish hospitals. Consequently, these hospitals developed their own, more stringent, safety measures for possible cases of Ebola.

47
travel and trade restrictions. During the epidemic, it again proved very challenging for the WHO
Secretariat to enforce these recommendations. This is exemplified by the following excerpt
from a report on the implementation of the IHR:
“One of the key challenges of the ongoing Ebola virus disease epidemic is to ensure
that the temporary recommendations issued by the Director-General under the
International Health Regulations (2005) in respect of the Ebola virus disease are
properly understood and implemented. Of particular concern is the recommendation
urging Member States not to adopt unilateral travel and trade measures affecting
countries experiencing intense transmission. In this connection, the Secretariat
monitors travel and trade measures that vary from the above recommendations and
communicates with Member States to confirm the exact nature and public health
rationale for the measures. As at 19 February 2015, 505 reports had been recorded
concerning such measures, involving a total of 69 countries. Where these measures
were perceived as excessive, 42 verification requests were sent to the countries in
question and 23 justifications for the measures were received. A further follow-up
request for justification or update on measures implemented was sent to 40 countries.
Three countries denied having closed their borders because of concerns relating to
Ebola virus disease.”293
Finally, in terms of research, the WHO helped speed up the process for the development of
Ebola vaccines and medicines. The D-G confirmed that, with regard to research and
development in emergency situations, “WHO is the convening authority to bring together all
the partners and stakeholders to come together and work”294 and that, similarly, in this
outbreak, WHO has been “taking the lead in a major international drive to test potential
therapies.”295
This drive was especially urgent given the fact that “clinical trials of potential therapies for Ebola
can only be conducted during an outbreak.”296 Therefore, the WHO has stimulated fast-tracking
the test phases of medicines and vaccines. Under normal circumstances, pharmaceutical
products have to undergo three different human test phases before entering the market297,
which each have a different focus and with an increasing tested population.298 In the first phase,
the first tests on humans take place; the pharmaceutical product is mainly tested for safety.
The test subjects generally consist of a limited population of less than 100 healthy
volunteers.299 In the second phase, therapeutic activity and short-term safety of the active
ingredients in patients suffering from the relevant disease are tested, in addition to an initial
293 WHA, Implementation of the International Health Regulations (2005): Responding to public health emergencies (15 May 2015) WHO Documents A68/22, http://apps.who.int/gb/ebwha/pdf_files/WHA68 /A68_22-en.pdf, para 10. 294 Statement by Margaret Chan during the WHO’s virtual press conference of 31 July 2015. A transcript is available at http://www.who.int/mediacentre/multimedia/survivor-meeting-vpc.pdf?ua=1 295 Fiona Fleck, ‘Tough Challenges for Testing Ebola Therapeutics’ (2015) 93 Bulletin of the World Health Organization 70, 70. 296 ibid. 297 A fourth test phase consists of post-marketing surveillance. 298 World Health Organization, ‘Guidelines for Good Clinical Practice (GCP) for Trials on Pharmaceutical Products’ [1995] WHO Technical Report Series Annex 3. 299 For the first phase of the clinical trials of Johnson&Johnson’s Ebola vaccine, 72 people were selected as test subject. See X, ‘Johnson & Johnson Announces Start of Phase 1 Ebola Vaccine’ (6 January 2015) <http://www.janssenbelgium.be/en/science/johnson-johnson-announces-start-of-phase-1-ebola-vaccine> accessed 3 September 2015.

48
determination of the appropriate dosage.300 In the third and final301 phase, the product is fine-
tuned, as tests are run to determine “the short- and long-term safety/efficacy balance of
formulation(s) of the active ingredient” in “larger (and possibly varied) patient groups”.302
Generally, phase II and III operate with use of a placebo, but in the case of Ebola, this was
considered unethical.303
Under normal circumstances, these three test phases can span almost a decade. As this was
considered unacceptable in the case of Ebola, and since the development of vaccines and
medicines requires the availability of infected test subjects, the WHO organized the possibility
to fast-track some of these procedures.304 On its website, it explains that “[f]ast-tracking of the
process has […] not resulted from cutting corners in the process to evaluate the vaccines, but
from doing phase II and III trials in parallel, reducing procedural time lags; for example, by
facilitating multi-country joint reviews of trial data by the concerned authorities, by accelerating
data sharing between reviewers and manufacturers, and by harmonizing the requirements of
the different ethics and regulatory committees.”305 This possibility to fast-track exemplifies the
influence WHO can exercise over regulatory or administrative processes in certain
circumstances, and especially in case of health emergencies.
2.3.4 Impact in Flanders
2.3.4.1 Implementation of the IHR
In a recent report, the WHO Secretariat noted that, globally, the national capacities required
under article 5 of the IHR had insufficiently been developed.306 This statement was confirmed
by the Ebola Interim Assessment Panel which considered “this situation, in which the global
community does not take seriously its obligations under the International Health Regulations
(2005) – a legally binding document – to be untenable.”307 Other global actors have affirmed
these conclusions. The EU, for example, deplored the weak implementation of the IHR,308 and
300 World Health Organization, ‘Guidelines for Good Clinical Practice (GCP) for Trials on Pharmaceutical Products’ (n 298). 301 Some consider the post-marketing phase of pharmacovigilance to constitute the fourth phase. See section 3.3.3.1. 302 World Health Organization, ‘Guidelines for Good Clinical Practice (GCP) for Trials on Pharmaceutical Products’ (n 298). 303 Instead, the pharmaceutical companies opted, in close cooperation with the WHO for a method called “ring vaccination”, in which contacts and contacts of contacts of an indexed case are vaccine. See WHO, ‘Questions and Answers – Ebola ça Suffit! - Phase III Vaccine Trial in Guinea’ (WHO) <http://www.who.int/medicines/ebola-treatment/q_a_phase3vaxtrial_guinea/en/> accessed 3 September 2015. 304 According to the infographic on the website of the WHO, they shortened the normal clinical trials period from more than 10 years to less than a year. See http://apps.who.int/ebola/our-work/achievements. 305 WHO, ‘Questions and Answers – Ebola ça Suffit! - Phase III Vaccine Trial in Guinea’ (n 303). 306 WHO Secretariat, ‘Implementation of the International Health Regulations (2005): Responding to public health emergencies’ (Report of the Director-General, 15 May 2015), WHO Docs. WHA68/22. The report includes an annex in which the national capacities of the different Member States are graded for several elements (legislation, coordination, surveillance, etc.). See also Isabelle Nuttall, ‘International Health Regulations (2005): Taking Stock’ (2014) 92 Bulletin of the World Health Organization 310. 307 The report of this panel, which was finished in July 2015, is available at http://www.who.int/csr/resources/publications/ebola/report-by-panel.pdf?ua=1. 308 ‘Matters arising out of the Resolutions and Decisions of the World Health Assembly and Executive Board: International Health Regulations’ (EU Statement at the 64th session of the WHO Regional

49
in 2013 the G20 has called upon on countries “to strengthen compliance” with the IHR.309 The
weak implementation is often ascribed to the lack of formal mechanisms to enforce
compliance. In terms of reporting obligations, currently only self-reporting mechanisms exist in
article 54 IHR. Moreover, there is no enforcement mechanism, although the WHO suggests
that “perhaps the best incentives for compliance are "peer pressure" and public knowledge.”310
Consequently, the EU held a plea for “the use of solid, transparent and reliable assessment
instruments like external assessment and certification processes”, at the WHA of 2015.311
In contrast to this general picture, Belgium does quite well in terms of implementation of its
obligations under the IHR, according to a recent Secretariat report, except with regard to
preparedness312. Indeed, as most Western industrial countries, Belgium already had a
functioning surveillance and response system for health emergencies. Coordination, however,
remains an issue. Indeed, due to the combination of competences being spread across
different levels in the Belgian federal state and the adoption by the IHR of an all-hazards
approach, coordination has been very difficult.313 Thorough implementation of the IHR will
require more collaboration between the federal state and the federated entities, even though
several attempts at coordination have already been undertaken. Currently, the national IHR
focal point, which is operated by the Operational Service Communicable Diseases314, has been
established by a Protocol Agreement of 11 December 2006.315 Other relevant agreements can
be found on the website of the Public Service Public Health, Safety of the Food Chain and
Environment.316
Committee for Europe, 15-18 September 2014), available at http://eeas.europa.eu/delegations/un_geneva/documents/eu_statments/who/20140918_who_rc64_item_3_ihr.pdf. 309 ‘Saint-Petersburg Declaration’ (G20 Leaders’ Declaration, September 2013), available at https://g20.org/wp-content/uploads/2014/12/Saint_Petersburg_Declaration_ENG_0.pdf, para 88. 310 WHO, Frequently Asked Question about the International Health Regulations (2005), http://www.who.int/ihr/about/FAQ2009.pdf?ua=1&ua=1, 3. 311 See ‘Implementation of the International Health Regulations (2005)’ (EU Statement at the 68th WHA, 18-26 May 2015), available at http://eeas.europa.eu/delegations/un_geneva/documents/eu_statments/who/20150522_ihr.pdf. 312 It is not entirely clear why Belgium does not score well on the preparedness issue. During one interview, it was suggested that this was due to a lack of coordination of preparedness and response mechanisms for epidemics and for other health issues. 313 Kumanan Wilson, ‘Strategies for Implementing the New International Health Regulations in Federal Countries’ (2008) 86 Bulletin of the World Health Organization 215; Kumanan Wilson, Christopher McDougall and Ross Upshur, ‘The New International Health Regulations and the Federalism Dilemma’ (2005) 3 PLoS Med e1. 314 Wetenschappelijk Instituut voor Volksgezondheid (WIV-ISP), ‘Operationele directie – Overdraagbare en besmettelijke ziekten’, https://www.wiv-isp.be/Programs/communicable-infectious-diseases/Pages/NL-Direction.aspx. 315 Protocol Agreement of 11 December 2006 between the Federal Government and the governments mentioned in articles 128,130 and 135 of the Constitution with regard to: Focal Point International Health Regulations, BS 19 July 2007, 38876 (in Dutch: Protocolakkoord van 11 december 2006 tussen de Federale Regering en de in artikelen 128, 130 en 135 van de Grondwet bedoelde overheden inzake: Focal Point Internationaal Gezondheidsreglement). The text is available online at http://reflex.raadvst-consetat.be/reflex/pdf/Mbbs/2007/07/19/106070.pdf 316 Public Service Public Health, Safety of the Food Chain and the Environment, ‘Protocollen’, http://health.belgium.be/eportal/Healthcare/Consultativebodies/Interministerialconferences/Protocols/7468407?ie2Term=vaccination?&&fodnlang=nl#.Vd7RF5drt-I.

50
2.3.4.2 Impact of the WHO’s response to Ebola317
Although the Ebola outbreak never actually reached Flanders, the WHO response still
impacted Flanders in several ways. Indeed, the response had three legs, which included
enhancing preparedness, and supporting and coordinating research. The first leg, which was
concerned with the response in the affected States, might not be as relevant to Flanders
(except for Flemish citizens or organizations aiding the response) but the other legs proved to
have some relevance. Indeed, with regard to preparedness, both at the governmental level
and the level of non-governmental actors (e.g. hospitals), those responsible closely followed
the WHO’s recommendations with regard to safety procedures for handling cases. As even
States as close by as “Germany, Norway, France, Italy, Switzerland and the UK have all
treated patients who contracted the virus in West Africa”318, these safety procedures were not
irrelevant as the risk existed that Flanders would also have to take care of Ebola patients.
However, some actors quickly dismissed the WHO recommendations and guidelines on safe
and hygienic treatment of Ebola patients as being too light and unsafe, and they developed
their own guidelines.319 Finally, the Belgian Minister of Public Health decided to appoint a
national coordinator for the Ebola crisis, Erika Vlieghe from the Institute for Tropical Diseases,
who has since been responsible for coordinating the Belgian Ebola response, both for the
treatment of possible cases and for the dissemination of information.320 The coordinator is
supported by a Risk Management and a Risk Assessment Group which consist of officials from
the federal state and the federated entities and health experts (mainly from the Scientific
Institute for Public Health or Wetenschappelijk Instituut Volksgezondheid; WIV-ISP).321 The
Communities were responsible for assessing possible cases of Ebola, which all health
personnel was obliged to notify to them. However, if a case would be confirmed, the response
would be coordinated at the federal level.
The recommendations with regard to necessary travel and trade restrictions also form part of
the preparedness package. In accordance with article 43 IHR, although these
recommendations are not strictly binding, States should motivate their deviation from these
recommendations. To our knowledge, Belgium has not adopted travel or trade restrictions
which would run counter to the temporary recommendations, although it did adopt some safety
measures for travelers to and from the affected area. It seems that Belgium maintained its
flights to the affected area, unlike several other States.322
Finally, as explained above, the WHO allowed for fast-tracking the human subjects test phases
of pharmaceutical products meant to combat the Ebola outbreak. Vaccines from Belgian
pharmaceutical companies were in the running323, but eventually the WHO mainly supported
317 It should be remembered that this outbreak never reached Flanders. In these circumstances, it is natural that the impact of the WHO remained rather limited. In case of an outbreak in Belgium, WHO could potentially play a more important role. 318 BBC, ‘Ebola: Mapping the Outbreak’, available at http://www.bbc.com/news/world-africa-28755033. 319 We gathered this from our interview at Gasthuisberg. 320 ‘Ebola – Wat doen de gezondheidsautoriteiten?’, http://www.info-ebola.be/nl/wat-doet-de-overheid/ 321 Ibid. 322 See ‘Ebola – Reisadvies’, http://www.info-ebola.be/nl/reisadvies/. 323 Janssen Pharmaceuticals has been developing an Ebola vaccine at the request of their mother company Johnson & Johnson. See Alan Hope, ‘Janssen Pharma to Produce New Ebola Vaccine’ Flanders Today (23 October 2014) <http://www.flanderstoday.eu/innovation/janssen-pharma-produce-new-ebola-vaccine> accessed 3 February 2016.

51
vaccines developed by GlaxoSmithKline, NewLink Genetics and Merck Vaccines USA in
cooperation with the public health department of Canada.324
2.3.5 Reform of the WHO’s health emergency response system
The WHO’s response to the Ebola crisis has been harshly criticized, both internally and
externally. In January 2015, the EB decided to establish an interim assessment panel to assess
the effectiveness of the WHO’s response to the Ebola crisis. This panel presented its report to
the WHA in May 2015, in which it castigated the WHO’s slow response. It identified several
organizational shortcomings as well as deficiencies in the workings of the IHR.325 Despite
earlier warnings that a reform of the IHR was warranted after the swine flu (H1N1) epidemic in
2009, the WHO remained inactive. In the words of the Interim Assessment Panel, “[h]ad the
recommendations for revision made in 2011 by the Review Committee in relation to Pandemic
(H1N1) 2009 been implemented, the global community would have been in a far better position
to face the Ebola crisis. The world simply cannot afford another period of inaction until the next
health crisis.”326 In the meantime, a new and final Review Committee has been set up, which
held its first meeting on 24-25 August 2015.327 The WHO has responded to this call for
reform.328 Discussions are now ongoing with regard to the establishment of a contingency fund,
a global health emergency workforce and a restructuring of the WHO’s internal organization
for tackling global health emergencies which would be better coordinated and less fragmented.
The WHO has faced heavy criticism with regard to its tardy and generally insufficient response
to the Ebola crisis. Despite several calls for reform of the WHO outbreak response system after
the H1N1-outbreak in 2009 as it showed some important flaws329, little had happened to
improve this system. In the course of 2015, both the EB330 and the WHA331 have mandated the
324 See WHO, ‘Essential medicines and health products – Ebola vaccines, therapies, and diagnostics’, http://www.who.int/medicines/emp_ebola_q_as/en/. 325 The panel stated that “the Ebola crisis not only exposed organizational failings in the functioning of WHO, but it also demonstrated shortcomings in the International Health Regulations (2005).” The full report is available at http://www.who.int/csr/resources/publications/ebola/ebola-interim-assessment/en/. See also Rebecca Katz and Scott F Dowell, ‘Revising the International Health Regulations: Call for a 2017 Review Conference’ [2015] The Lancet Global Health <http://www.sciencedirect.com/science/article/pii/S2214109X1500025X> accessed 3 September 2015. For a critique of the critique, see David Fidler, ‘Ebola Report Misses Mark on International Health Regulations’ (Chatham House) <http://www.chathamhouse.org//node/18159> accessed 3 September 2015. 326 Report of the Interim Assessment Panel, 5. 327 A webcast of the first meeting is available online at http://www.who.int/ihr/review-committee-2016/webcast-aug2015/en/ 328 See WHO, ‘About WHO – Learning from Ebola: Readiness for Outbreaks and Emergencies’, http://who.int/about/who_reform/emergency-capacities/en/. 329 Kumanan Wilson, John S Brownstein and David P Fidler, ‘Strengthening the International Health Regulations: Lessons from the H1N1 Pandemic’ (2010) 25 Health Policy and Planning 505, 1. Similarly, some called for reform after the SARS outbreak of 2002. See David Bishop, ‘Lessons from SARS: Why the WHO Must Provide Greater Economic Incentives for Countries to Comply with International Health Regulations’ (2005) 36 Georgetown Journal of International Law 1173. 330 ‘Ebola: ending the current outbreak, strengthening global preparedness and ensuring WHO’s capacity to prepare for and respond to future large-scale outbreaks and emergencies with health consequences’ (EB Resolution, 25 January 2015), WHO Docs. EBSS3.R1, available at http://apps.who.int/gb/ebwha/pdf_files/EBSS3-REC1/EBSS3_REC1.pdf#page=12 331 ‘2014 Ebola virus disease outbreak and follow-up to the Special Session of the Executive Board on Ebola (WHA Decision, 5 June 2015), WHO Docs. WHA68(10), available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_DIV3-en.pdf.

52
D-G to reform the WHO’s health emergency response system in line with the recommendations
of the Ebola Interim Assessment Panel332. On 21 July 2015, the WHO D-G established an
‘Advisory Group on Reform of WHO’s Work in Outbreaks and Emergencies with Health and
Humanitarian Consequences.’333
According to recent reports, the WHO failed on several accounts.334 The response was late,
slow to develop, and inadequate. There was a lack of coordination and information-sharing, as
well as uncertainty with regard to the division of responsibilities among the engaged actors.
Initially, affected communities were insufficiently engaged in the response.335 According to the
report of the independent audit, there were ‘failures in both technical judgment and political
leadership.’336
The Advisory Group established by the D-G stated the necessary changes “will require political
commitment from WHO’s Member States, structural change within the Organization, an
evolution of internal culture, a renewal and strengthening of relationships with external actors,
and the application of new authorities, mechanisms, procedures and systems for
accountability.”337 One recurring recommendation refers to the establishment of an
independent institutional framework within the WHO to deal with outbreaks and health
emergencies, as it currently lacks operational capacities to ensure effective and swift
responses.338 Another recurring recommendation is improving the leadership role of the WHO.
What the impact of these reforms would be in Flanders remains to be seen as the reform is
still work in progress, and limited real details are available.
2.4 Nomenclature regulations
The WHO Regulations regarding nomenclature (including the compilation and publication of
statistics) with respect to diseases and causes of death (hereinafter: Nomenclature
Regulations) have been adopted in 1967 and entered into force on 1 January 1968.339 They
have been adopted on the basis of article 21(b) WHO Constitution which grants the WHA the
332 Next to this internal audit, the WHO has also asked for an external audit of its response and the possible reforms. This was performed by the Harvard-LSHTM Independent Panel on the Global Response to Ebola, which published its report in the Lancet on 22 November 2015. See Moon and others (n 261). 333 WHO, ‘About WHO – ‘Advisory Group on Reform of WHO’s Work in Outbreaks and Emergencies with Health and Humanitarian Consequences’, http://www.who.int/about/who_reform/emergency-capacities/advisory-group/en/. Several of the reports of this Advisory Group’s meetings are available at http://www.who.int/about/who_reform/emergency-capacities/advisory-group/reports/en/. 334 For an overview, see Suerie Moon and others, ‘Will Ebola Change the Game? Ten Essential Reforms before the next Pandemic. The Report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola’ (2015) 386 The Lancet 2204. See also Lawrence O Gostin, ‘Reforming the World Health Organization after Ebola’ (2015) 313 JAMA 1407. 335 Stephen B Kennedy and Richard A Nisbett, ‘The Ebola Epidemic: A Transformative Moment for Global Health’ (2015) 93 Bulletin of the World Health Organization 2. 336 Moon and others (n 261) 2206. 337 WHO, ‘Advisory Group on Reform of WHO’s Work in Outbreaks and Emergencies. First Report’ (15 November 2015), available at http://www.who.int/about/who_reform/emergency-capacities/first-report-advisory-group.pdf, para 5. 338 Ibid., para 6. 339 World Health Organizations Regulations regarding nomenclature (including the compilation and publication of statistics) with respect to diseases and causes of death (adopted on 22 May 1967, entered into force 1 January 1968) 1172 UNTS 345 (Nomenclature Regulations). The Nomenclature Regulations are available at http://www.who.int/classifications/icd/docs/en/NOMREGS.pdf

53
“authority to adopt regulations concerning nomenclatures with respect to diseases, causes of
death and public health practices”.340 These Regulations (and their implementing instruments)
serve to fulfill “a key role of WHO[, which] is to produce, maintain and implement international
health information standards, to provide a consensual, meaningful and useful common
language for use by governments, health care providers and consumers”341, by providing a
standardized scheme of reporting for both health professionals and countries. In other words,
every type of disease and cause of death is categorized. For example, “tuberculosis of lung,
confirmed by sputum microscopy with or without culture” corresponds with A15.0 in the ICD-
10 Version of 2015, while the category of V01 corresponds with “pedestrian injured in collision
with pedal cycle”342.
Since this categorization scheme requires constant updating, and updating regulations is a
sinuous exercise, there has been a ‘workaround’ via the International Classification of
Diseases (ICD).343 The Nomenclature Regulations haven’t been updated since 1967. Instead,
article 2 of these Regulations provides that “Members compiling mortality and morbidity
statistics shall do so in accordance with the current revision of the International Statistical
Classification of Diseases, Injuries and Causes of Death as adopted from time to time by the
World Health Assembly. This Classification may be cited as the International Classification of
Diseases.” The ICD forms part of the WHO Family of International Classifications (WHO-FIC),
alongside the International Classification of Functioning, Disability and Health (ICF) and the
International Classification of Health Interventions (ICHI).344 To these “reference
classifications”, several “derived classifications” and “related classifications”345 have been
attached to form the WHO-FIC. A Family Development Committee ensures the coherence of
the family and reviews the merits of new classifications proposed to be added to the family.346
The ICD can be more easily revised than the Nomenclature regulations. Nevertheless, the 11th
revision of the ICD, which is currently underway, has already taken at least three years, and
will not be finalized until 2018.347 This protracted revision process is mainly due to a change in
revision procedure, as for the first time, the WHO has organized a large consultation round,
asking experts around the globe to provide feedback on the functioning of the ICD. In a May
2012 communication on the WHO website, it stated that “for the first time, experts in the public
health community who work with patient diagnosis and treatment have an opportunity to
contribute to the development of the next version of the International Classification of Diseases
(ICD).”348
The ICD and the Nomenclature Regulations reflect the central role of the WHO in the
classification of diseases. Although classification as such can hardly be considered regulation
or standard-setting, the choice of certain classification systems can have a pertinent impact on
340 These Regulations and their implementing instruments serve to fulfil WHO’s function “to establish and revise as necessary international nomenclatures of diseases, of causes of death and of public health practices”, described in article 2(s) of the WHO Constitution. 341 WHO, ‘Classification of diseases’, http://www.who.int/topics/classification/en/. 342 In this category, V01.0 corresponds to a nontraffic accident whereas V01.1 corresponds to a traffic accident and V01.9 is used when it is unsure whether the injury was sustained in a traffic accident. 343 Klock (n 165) 829. 344 Richard Madden and others, ‘World Health Organization Family of International Classifications: Definition, Scope and Purpose’ (2007). See also http://www.who.int/classifications/en/ 345 These may also include classifications not developed by the WHO (e.g. ISO classifications). 346 Richard Madden, Catherine Sykes and T Bedirhan Ustun, ‘World Health Organization Family of International Classifications: Definition, Scope and Purpose’ (2007) 12 <http://www.who.int/classifications/en/FamilyDocument2007.pdf?ua=1> accessed 13 August 2015. 347 The last revision, which resulted in ICD-10 dates from 1992. 348 WHO, ‘WHO seeks health experts’ input for 11th International Classification of Diseases’ (May 2012), http://www.who.int/features/2012/international_classification_disease/en/.

54
other policy instruments and options. How a certain disease or cause of death is classified can,
for example, affect the amount of reimbursement it receives. Indeed, when Belgium was
planning to shift from using ICD-9 to ICD-10, it was considered that this would lead to a more
accurate division of the available financial means.349 In addition, these classification systems
determine how States should report to the WHO. As domestic administrations are forced to
report in certain terms and by using certain categorizations, some issues might become more
apparent than others. If the WHO, for example, requests data from Belgium on whether
nutrition is part of medical curricula,350 the Flemish administration might be interested in
including nutrition into medical curricula, or at least start thinking about the importance of
including this in the medical curricula.
The central role which the WHO occupies in both the collection and the classification of public
health information will feature also in section 3.4 (with regard to the classification of
pharmaceutical products).
349 FOD Volksgezondheid, Veiligheid van de Voedselketen en Leefmilieu, ‘Overgang van ICD-9-CM naar ICD-10-BE’, http://health.belgium.be/eportal/Healthcare/Healthcarefacilities/Registrationsystems/ProjectICD10BE/index.htm?fodnlang=nl#.Vo_JmlnZaDc. 350 WHO, ‘Nutrition Landscape Information System (NLiS)’, http://apps.who.int/nutrition/landscape/report.aspx?iso=bel.

55
3. Legally non-binding instruments
3.1 Recommendations and guidelines
3.1.1 The difference
While the WHO Constitution has given the WHO a strong mandate to develop binding
instruments, this mandate has not been extensively used throughout the years.351 Instead, the
WHO has fostered a tradition of soft law.352 It has consistently preferred non-binding
instruments over binding instruments.353 In the words of Burci and Vignes, “[t]he setting of a
wide variety of recommendations and other non-binding standards is without doubt the most
prolific and successful normative activity of the Organization.”354 This soft law approach has
been favoured because of the increased flexibility, the adaptability and even for its low
threshold for adoption.355
In accordance with article 23 of the WHO Constitution, the WHA can adopt recommendations
towards the Member States “with respect to any matter within the competence of the
Organization.”356 However, the WHO Secretariat has equally developed guidelines without a
mandate or de post facto approval of the WHA, often with the help of experts sitting in different
types of expert bodies.357 Indeed, according to the WHO’s Handbook on Guideline
Development (see infra), “[g]uidelines are the fundamental means through which the
Organization fulfils its technical leadership in health, as identified in the GPW”,358 and these
guidelines are characterised by the fact that they are developed by experts. Moreover, they
are not always endorsed by the WHA.
Burci and Vignes have divided these soft law instruments into three broad categories:
“(1) Regulatory recommendations adopted by the Health Assembly or, within the limits
of its constitutional functions, by the Executive Board. Such recommendations are
normally elaborated by the Secretariat, on its own initiative or at the request of a
governing body.
351 Gostin, Sridhar and Hougendobler (n 160). 352 For a discussion of different legal methods for approach soft law, see Duquet and Wouters (n 1). See also Shaffer and Pollack (n 171). 353 In what follows, we will not distinguish between different types of soft law. We are aware that certain instruments, which we will discuss, could be considered to rather constitute policymaking or PR. However, we would contend that even in these cases the WHO exercises its normative function and attempts to convince actors to act according to certain rules, norms or principles. As such, these instruments could also be considered “soft law”. Therefore, we have elected to not distinguish between the instruments discussed hereafter on this basis. We will, however, return shortly to this theme in section 4.1.3. 354 Burci and Vignes (n 12) 141. 355 ibid. 356 However, the WHA does not always refer to this article in adopting recommendations. See ibid 142. 357 In the words of Burci and Vignes, “Most […] recommendations, guidelines and standards do not take the form of a full-fledged regulatory text approved by the Assembly, but rather that of technical documents elaborated by groups of experts or external collaborators.” See ibid 146. 358 World Health Organization, WHO Handbook for Guideline Development (n 20) 1.

56
(2) Standards and recommendations developed by the Secretariat on the basis of a
grant of authority by a governing body but not endorsed or approved as such by the
latter.
(3) Standards developed by expert bodies convened by the Secretariat and published
by WHO as such, without formal endorsement.”359
Gostin, Sridhar and Hougendobler have proposed a similar categorization.360
It remains, however, extremely difficult to draw clear lines between recommendations stricto
sensu which have received endorsement from the WHA, and guidelines emanating purely from
the technical level, as these last often have at least a very limited form of WHA endorsement.
Still, the distinction remains important. Although the legal basis for recommendations adopted
by the WHA can clearly be found in article 23 WHO Constitution, there does not seem to be
any general legal basis for the development of normative guidelines by the Secretariat without
WHA endorsement. Although certain paragraphs of article 2 clearly accord the WHO a
normative function, the WHO Constitution does not mandate the Secretariat or the Director-
General to adopt these guidelines autonomously. It is equally difficult to discern implied powers
for the Secretariat in this sense, as this would run counter to the presumption that States have
not intended to delegate their normative function. The Handbook seems to avoid this issue by
placing the initiative firmly in the hands of relevant stakeholders: “WHO develops guidelines
whenever Member States, WHO country offices, external experts or other stakeholders ask for
guidance on a clinical or public health problem or policy area”,361 although, admittedly, this
should not be considered as defining a “right of initiative”. Alternatively, the practice itself, which
consists of the Secretariat autonomously overseeing the development of guidelines, has never
been contested, and can, as such, be legitimized as “subsequent practice”.362 A legal basis
could also be found in the regulations for expert involvement discussed earlier, which gives
the Secretariat considerable leeway in organizing expert gatherings without oversight from the
governing bodies.363
The question of the legal basis also relates to the question of to whom the recommendations
and guidelines are attributable. Indeed, as Burci and Vignes note, “this system of standard
setting – involving on the one hand the recommendations emanating solely from the technical
level and on the other hand those having received formal Health Assembly endorsement – has
worked reasonably well over the life of the Organization. It does, however, provide an
opportunity for a degree of uncertainty on what are the positions of the Organization in specific
cases.”364 In principle, approval by the Director-General or the WHA is required to ascribe
359 Burci and Vignes (n 12) 141. 360 “First, the WHA can pass a resolution, which expresses the will of member states, representing the highest level of commitment. Second, the Secretariat can set a standard on a grant of authority from the Assembly or Board, but without the governing authority's formal approval. Finally, the Secretariat can convene expert committees and disseminate their findings without formal endorsement.” See Gostin, Sridhar and Hougendobler (n 160) 855. 361 World Health Organization, WHO Handbook for Guideline Development (n 20) 1. 362 Article 31.3(b) VCLT. See also José E Alvarez, International Organizations as Law-Makers (Oxford University Press 2006) 87–92. 363 Burci and Vignes (n 12) 150. They state that “the aforementioned regulations for expert committees and other mechanisms have granted the Secretariat general authority to select experts, to limit participation in technical meetings, and to draw the relevant conclusions from the findings of expert bodies without the need for specific approval by WHO’s governing bodies. The governing bodies only exercise general oversight authority on the basis of reports by the Director-General, or consider his recommendations for the purpose of adopting standards and policies.” 364 ibid.

57
these guidelines to the WHO.365 “In practice however, once they are published, these
conclusions and recommendations have become identified as being the position of the
Organisation on the scientific issues covered by the meeting concerned.”366
3.1.2 New rules for guideline development
For a long time, no clear procedure existed for developing guidelines. Even the reference to
the WHA for political endorsement seemed – and still seems – to occur on an ad-hoc basis.367
However, in 2007, Andrew Oxman and some of his colleagues heavily criticized the WHO
system for guideline development.368 In their external review, they considered the system to
be too heavily dependent on expert opinion, and insufficiently evidence-based. This critique
reverberated throughout the scientific community and threatened the WHO’s image as a “as a
scientifically and technically reliable organization”369, an image which was crucial for its
credibility and consequentially for the adoption and implementation of its guidelines and
recommendations by the addressees thereof. Consequently, WHO recognized the need for
reform370 and, in response, the WHO elaborated a Handbook on Guideline Development
(hereinafter: the Guideline Handbook), which was meant to formalize the procedure for
developing guidelines and ensure their scientific soundness. A Guideline Review Committee
(hereinafter: the GRC) was equally established to overview the correct implementation of this
handbook by the expert bodies consulted by the WHO. This committee made use of the
GRADE method to assess guidelines.371 Recently, several articles have re-assessed the
quality of the guidelines.372 They have marked a positive evolution, although they stress that
the GRC’s role should be stressed even more within the WHO’s functioning.373 The guidelines
approved by the GRC can be found on the website of the WHO arranged by topic374, by year
of publication or alphabetically.375 It is important to note that not all WHO guidelines in
existence have received GRC approval, as many have been developed before the GRC was
established.
365 ibid. 366 ibid 149. 367 ibid. “Occasionally, when for one reason or another it was felt desirable or necessary to obtain a formal political endorsement of the particular ‘position’ emanating from the experts group system (often involving guidelines or recommended practices), the matter has been submitted to the Health Assembly for endorsement, thereby becoming a formal position or policy of the Organization.” 368 Andrew D Oxman, John N Lavis and Atle Fretheim, ‘Use of Evidence in WHO Recommendations’ (2007) 369 The Lancet 1883. 369 Burci and Vignes (n 12) 141. 370 Priya Shetty, ‘Making WHO Recommendations More Responsive’ (2014) 92 Bulletin of the World Health Organization 778. 371 ibid. 372 BU Burda, AR Chambers and JC Johnson, ‘Appraisal of Guidelines Developed by the World Health Organization’ (2014) 128 Public Health 444; David Sinclair and others, ‘World Health Organization Guideline Development: An Evaluation’ (2013) 8 PLoS ONE e63715. 373 Recently, the WHO Secretariat has also presented a report to the EB on guideline development. See ‘WHO guidelines: development and governance’ (Report by the Secretariat, 20 May 2015), WHO Docs. EB137/5, available at http://apps.who.int/gb/ebwha/pdf_files/EB137/B137_5-en.pdf. 374 There are 12 different topics: child health, chronic diseases, injuries and disability, communicable diseases, environmental health, HIV/AIDS, health systems, malaria, maternal, reproductive health and women’s health, mental health and substance abuse, nutrition, patient safety and tuberculosis. 375 See WHO, ‘WHO guidelines approved by the Guidelines Review Committee’, http://www.who.int/publications/guidelines/en/.

58
The WHO has not only struggled with the scientific basis for their guidelines, but also with the
involvement of relevant stakeholders.376 The obstinate image of WHO as a dominated by “the
conservative medical community”377 threatened its legitimacy, which in turn was dangerous for
the effectiveness of their guidelines. Aware of this danger, WHO is “[i]ncreasingly seeking
public input into the development of guidelines [and] has started opening up its guidelines to
public consultation.”378
The establishment of the GRC and the concomitant standardization of the guideline-
developing procedure has also shed new light on the question of attributability. One can now
safely assume that guidelines reviewed by the GRC can be attributed to the WHO. Evidence
for this statement can be found in a footnote added at the start of each guideline stating: “This
publication is a World Health Organization (WHO) guideline. A WHO guideline is a document,
whatever its title, containing WHO recommendations about health interventions, whether they
be clinical, public health or policy interventions. A recommendation provides information about
what policy-makers, health-care providers or patients should do. It implies a choice between
different interventions that have an impact on health and that have ramifications for the use of
resources. All publications containing WHO recommendations are approved by the WHO
Guideline Review Committee.” As such, guidelines have become a specific type of
instruments, adopted in accordance with clear procedural rules, which are clearly attributable
to the WHO.
Once adopted and published, these guidelines and recommendations require implementation.
Several pathways are open for implementation. Generally, the WHO tries to cooperate with
governments in order to bring about policy changes. To illustrate this process, we will focus on
the Global Strategy on Diet, Physical Activity and Health in the next section, with specific
attention being paid to the Guidelines on Sugar Intake. However, the WHO has also interacted
more directly with private actors. Doctors, for example, are represented at the WHO by their
professional representative bodies, which often inform their members directly of decisions
taken, recommendations made, or research published at the level of the WHO. Other channels
for directly impacting on private actors also exist. To highlight some of these processes, we
will focus on the Clean Care is Safer Care programme in section 3.3.2. Finally, in section 3.3.3,
we attempt to demonstrate the sheer number of WHO guidelines and programmes, and how
these affect a certain process or sector. We do this by discussing the development of
pharmaceutical products from the R&D phase until the marketing phase, while noting different
WHO programmes and guidelines which affect these different phases.
Independent from the pathway for implementation, the question remains whether the
implementation is actually happening. Indeed, effective implementation of its guidelines has
increasingly become a concern for the WHO.379 The effectiveness depends on several factors:
the awareness of the target public of the existence of the guidelines, the technical capacities
of the addressees (the WHO often offers technical assistance), the perception of the guidelines
as useful, etc.380 An essential tool for the WHO is the obligation for member states to report on
the implementation of recommendations in accordance with article 62 WHO Constitution.
376 Shetty (n 370). 377 Taylor, ‘Making the World Health Organization Work’ (n 14) 303. 378 Shetty (n 370) 779. 379 Shetty (n 370). 380 World Health Organization, WHO Handbook for Guideline Development (n 20) 18.

59
However, the WHO has not made consistent use of their authority to require member states to
report.381 Therefore, it has been conducting researching with regard to implementation.382
3.2 Impact on policy-makers
3.2.1 Introduction
In general, the WHO cooperates with governments and policy-makers to ensure
implementation of its guidelines and recommendations. This coincides with the traditional idea
of the state as a black box. Under the black box theory, “international law can insert its
demands in the box, requiring certain results to come out of it; however, it cannot determine
how these results are reached within the box.”383 In other words, international law is something
between states, who retain complete freedom with regard to the implementation of obligations
derived from international law within their territories and vis-à-vis their nationals. The flipside
of the coin is that international law does not directly concern individual people or private actors.
Although international law has long moved away from this strict Westphalian model, as
individuals can now in some instances derive both rights and obligations from international
law, this traditional view still remains the point of departure.
To illustrate the impact of the WHO on domestic policy-making, we selected the topic of “diet
and physical activity” as a case study.384 This topic is relevant not only because the WHO has
developed a Global Strategy385 on this topic, but also because Flanders has developed health
objectives (“gezondheidsdoelstellingen”) which are currently under revision. Despite the fact
that the WHO in general encourages developing a multisectoral approach,386
recommendations in this field are mainly aimed at policy-makers, making it a relevant case
study to discuss the impact of the work of the WHO on policy-making at the domestic level.
After a more general discussion of how the WHO’s general strategy with regard to diet and
physical activity is translated into Flemish policy, we will discuss the impact of one specific
guideline, namely the guideline on sugar intake for adults and children, as this guideline has
stirred considerable controversy387, and might well have important economic impacts.
381 Gostin, Sridhar and Hougendobler (n 160) 855. 382 David H Peters and others, Implementation Research in Health: A Practical Guide (World Health Organization 2013). 383 Ward Ferdinandusse, ‘Out of the Black-Box-The International Obligation of State Organs’ (2003) 29 Brook. J. Int’l L. 45. 384 This is an interesting topic since it is clearly directed at developed states where the problem is often “over-nutrition” instead of undernutrition. 385 WHO, ‘Global Strategy on Diet, Physical Activity and Health’ (May 2004), available at http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf?ua=1. The Global Strategy was endorsed by the WHA in resolution WHA57.17. A formal mandate to develop this document was provided by resolution WHA55.23. 386 See Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013-2020, 80. 387 The WHO suggests intakes of sugar well below the current mean, which, if followed, could result in great losses for some of the major beverages companies. See, for example, Brian Owens, ‘Storm Brewing over WHO Sugar Proposal’ Nature (11 March 2014) <http://www.nature.com/news/storm-brewing-over-who-sugar-proposal-1.14854> accessed 3 February 2016.

60
3.2.2 Translating the Global Strategy on Diet, Physical Activity and Health into
“gezondheidsdoelstellingen rond Voeding & Beweging 2015-2021”
The Global Strategy forms part of the WHO’s fight against non-communicable diseases
(NCDs) which is one of the WHO’s current priorities.388 The fight against NCDs features
prominently as one of the six priorities in the 12th Global Programme of Work (GPW), which
sets out the broad guidelines for WHO action for the period of 2014-2019.389 As such, this
exemplifies the expansion of WHO’s mandate in global public health. Whereas international
public health law and diplomacy have traditionally been centered around communicable
diseases with a possible impact on trade, we have witnessed a veritable “diplomatization of
non-communicable diseases”390, with the fight against NCDs becoming a “global public
good”391, as the WHO noticed a shift in the main causes of death away from infectious diseases
towards NCDs, even in developing countries.392 How to tackle these NCDs has been
elaborated by the WHO in a Global Action Plan for the period 2013-2020393, which includes a
global monitoring framework.
Part of the fight against NCDs is the promotion of healthy nutrition and sufficient physical
activity. Indeed, both the GPW and the Global Action Plan provide the broader framework for
the development of more concrete guidance on the improvement of health through nutrition
and physical activity. As mentioned above, the Global Strategy is central to this guidance. The
initial mandate to develop a global strategy in this field was given to the WHO Secretariat at
the WHA meeting in May 2002.394 The document was finished in February 2003, and the WHA
endorsed it in 2004 placing “its full weight behind” it.395
According to this strategy, “[g]overnments have a central role, in cooperation with other
stakeholders, to create an environment that empowers and encourages behaviour changes by
individuals, families and communities, to make positive, life-enhancing decisions on healthy
diets and patterns of physical activity.”396 Moreover, as the European Food and Nutrition Action
Plan 2015–2020 stresses, governmental health departments cannot work independently, but
the problem rather requires “a whole-of-government, health-in-all-policies approach.”397
388 Sergey Boytsov, ‘Noncommunicable Diseases: Stepping up the Fight’ (2015) 93 Bulletin of the World Health Organization 9. 389 WHO (n 11). 390 David P Fidler, ‘Navigating the Global Health Terrain: Mapping Global Health Diplomacy’ (2011) 6 Asian J. WTO & Int’l Health L & Pol’y 1, 7. 391 Lincoln C Chen, Tim G Evans and Richard A Cash, ‘Health as a Global Public Good’ in Inge Kaul, Isabelle Grunberg and Marc A Stern (eds), Global Public Goods: International Cooperation in the 21st Century (Oxford University Press 1999). 392 See Global Strategy on Diet, Physical Activity and Health, 2. 393 WHO, ‘Global Action Plan for the prevention and control of noncommunicable diseases 2013-2020’ (2013), available at http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1. 394 WHO, ‘Global Strategy on Diet, Physical Activity and Health – Process for Developing the Global Strategy’, http://www.who.int/dietphysicalactivity/strategy/en/. 395 Gostin, Sridhar and Hougendobler (n 160) 855. The Global Strategy has been endorsed by Resolution WHA57.17. 396 Global Strategy on Diet, Physical Activity and Health, 3, para 14. 397 WHO/Europe, ‘European Food and Nutrition Action Plan’ (64th session of the Regional Committee for Europe, 15-18 September 2014), http://www.euro.who.int/__data/assets/pdf_file/0008/253727/64wd14e_FoodNutAP_140426.pdf

61
The Global Strategy mainly focuses on presenting governments at different levels the tools
required to develop effective action plans, although the importance of partnerships with private
actors is stressed, as well as the importance of a multi-sectoral and multidisciplinary approach.
It has four main objectives in the field of diet, physical activity and health: to reduce risk factors,
to raise awareness and understanding, to encourage the development of action plans at
different levels, and to promote and support research. Of course, this Global Strategy has seen
further implementation in other documents, such as guidelines, of which we will discuss the
guidelines on sugar intake below.
At the European level, this Global Strategy is further specified by the European Regional
Office. The Office has adopted an Action Plan for implementation of the European Strategy for
the Prevention and Control of NCDs 2012-2016.398 It has engaged in collaboration with the
European Commission in the field of physical activity.399 It also works closely with HEPA
Europe, the European Network for the Promotion of Health-Enhancing Physical Activity.400
In Flanders, the Flemish Agency for Care and Health is the competence body.401 This agency,
together with then Minister of Health, Steven Vanackere, has translated this Global Strategy
and its implementing or clarifying instruments in a set of health objectives
(“gezondheidsdoelstellingen”) with regard to diet and physical activity,402 which were discussed
at a major health conference in 2008.403 Consequently, an action plan was developed in order
to further these health objectives.404 This action plan spanned the period 2009-2015, and
negotiations for a new action plan for the period 2016-2022 are on the agenda for the end of
2015. These Flemish health objectives and the action plan were also supported by a Belgian
initiative, the National Diet and Health Plan for Belgium 2005-2010.405
The question remains to what extent the WHO’s policy documents have influenced Flemish
policy-making. Unfortunately, for lack of data, the answer will remain somewhat speculative.
However, the draft of the action plan did refer to the WHO at two occasions. Firstly, they state
that the central objective of the action plan is “in line with the recommendations of the WHO
and the European institutions.”406 In addition, the draft refers to the WHO in stating that the
398 WHO/Europe, ‘Action Plan for implementation of the European Strategy for the Prevention and Control of Noncommunicable Diseases 2012-2016’, available at http://www.euro.who.int/__data/assets/pdf_file/0019/170155/e96638.pdf. 399 See WHO/Europe, ‘Collaboration between WHO/European Commission (EC) on promoting physical activity for health’, http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/activities/monitoring-and-surveillance/collaboration-between-whoeuropean-commission-ec-on-promoting-physical-activity-for-health. See also European Commission, ‘EU platform for action on diet, physical activity and health’, http://ec.europa.eu/health/nutrition_physical_activity/platform/. 400 Brian W Martin and others, ‘Evidence-Based Physical Activity Promotion - HEPA Europe, the European Network for the Promotion of Health-Enhancing Physical Activity’ (2006) 14 Journal of Public Health 53. 401 “Vlaams Agentschap Zorg en Gezondheid” 402 See Flemish Agency for Care and Health, ‘Gezondheidsdoelstelling voeding en beweging’, http://www.zorg-en-gezondheid.be/gezondheidsdoelstelling-voeding-en-beweging. 403 Information about this conference can be found at http://www.zorg-en-gezondheid.be/Beleid/Gezondheidsdoelstellingen/Gezondheidsconferentie-voeding-en-beweging/ 404 www.zorg-en-gezondheid.be/workarea/linkit.aspx?linkidentifier=id&itemid=20720 405 X., ‘Nationaal Voedings- en Gezondheidsplan voor België 2005-2010 (December 2005), http://health.belgium.be/internet2Prd/groups/public/@public/@dg4/@consumerproducts/documents/ie2divers/7522417.pdf. This plan also features on the implementation website GINA (see footnote 397): https://extranet.who.int/nutrition/gina/en/node/8010. 406 “In lijn met de aanbevelingen van de WHO en de Europese instellingen pleit dit plan voor een meer evenwichtig beweeg- en eetpatroon in Vlaanderen, met de focus op het bewaken van een gezond

62
problem at hand requires an integrated solution.407 The Belgian initiative is equally based on
“international initiatives that exist at the level of the European Union and the WHO, and in
particular the WHO Global Strategy on Diet, Physical Activity, and Health.”408 Conversely, the
Flemish action plan features on the website of the WHO’s Global Database on the
Implementation of Nutrition Action (GINA).409 In the end, in this case, the WHO might weigh on
policy-making by requiring multi-sectoral and multidisciplinary approaches on the basis of a
whole-of-government or health-in-all-policies approach. The impact of the WHO might rest
essentially in its emphasis on a holistic approach to health problems.
Finally, it is worthwhile to note that several EU legal instruments (regulations and directives)
and other policy initiatives are also mentioned in the GINA as implementing the WHO’s nutrition
policy.
3.2.3 An example: the guideline on sugar intake for adults and children
According to the Global Strategy, under current circumstances, improving nutritional habits
and making people’s diet healthier requires reduction of the intake of fats (especially saturated
fats and trans-fatty acids), salt and sugar. The WHO made further, more specific,
recommendations with regard to sugars intake for adults and children in a guideline
(hereinafter: the Sugar Guideline). This guideline was published in March 2015 and presented
in a press release during the same month.410 They build on “the work of the 1989 WHO Study
Group on Diet, Nutrition and Prevention of Noncommunicable Diseases” and the 2002 Joint
WHO/FAO Expert Consultation on Diet, Nutrition and the Prevention of Chronic Diseases,
which had already provided guidance on free sugars intake.
This guideline is based on scientific research with regard to the effects of (free) sugars intake
on “unhealthy weight gain” and “dental caries”. Indeed, this guideline was considered
necessary as considerable debated existed in scientific literature on the impact of free sugars
with regard to these two health issues. Several scholars, such as Robert Lustig, advocated
strongly against free sugars and argued with governments to develop policy initiatives to
gewicht (WHO, 2007; Commissie van de Europese Gemeenschappen, 2007).” See “Ontwerp van Actieplan Voeding en Beweging 2008-2015” available at http://www.zorg-en-gezondheid.be/Beleid/Gezondheidsdoelstellingen/Vlaams-actieplan-voeding-en-beweging-2009-2015/. The document does not contain any page numbers. 407 “De Wereldgezondheidsorganisatie (WHO) en verschillende Europese instellingen bepleiten dat elk land zo’n evenwichtig voedings- en beweegbeleid uitwerkt, aangepast aan de eigen cultuur en normen (zie www.gezondheidsconferentie.be). Dit omvat een mix van educatieve interventies, structurele maatregelen en beleidsinitiatieven waarin alle beleidsniveaus elkaar vinden en ondersteunen. De verschillende internationale initiatieven ter bevordering van evenwichtige voeding en gezond bewegen vertrekken vanuit diezelfde integrale aanpak. Ze pleiten voor een brede consumenteninformatie én voor het werken met prioritaire groepen, voor educatie én voor aanpassingen in de omgeving, voor betrokkenheid van diverse maatschappelijke actoren én voor een engagement vanuit de private sector, voor interventies die inspelen op de noden van de bevolking én voor een duurzaam beleid.” 408 “Het NVGP-B baseert zich hiervoor op de internationale initiatieven die bestaan op niveau van de Europese Unie en de Wereldgezondheidsorganisatie, en in het bijzonder de WGO Globale strategie betreffende voeding, fysieke activiteit en gezondheid.” See National Diet and Health Plan Belgium 2005-2010, 4. 409 The relevant webpage is https://extranet.who.int/nutrition/gina/en/node/8331. See also WHO, ‘Nutrition Landscape Information System – Country Profile: Belgium’, http://apps.who.int/nutrition/landscape/report.aspx?iso=bel. 410 WHO, ‘WHO calls on countries to reduce sugars intake among adults and children’ (press release, 4 March 2015), available at http://www.who.int/mediacentre/news/releases/2015/sugar-guideline/en/

63
reduce the amount of free sugars intake through different policy measures.411 To this end, they
established several institutions, such as the Institute for Responsible Nutrition412, and the
Action on Sugar413, which should be placed somewhere in between research institutes and
advocacy institutes.414 This is perfectly exemplified by the usage of slogans as “a calorie is not
a calorie”415 and the likening of sugar to cocaine or tobacco.416 In response to Robert Lustig,
David Katz, for example, wrote a column for the Huffington Post, entitled “Sugar isn’t evil: a
rebuttal”.417 Conversely, at the other end of the spectrum, some scientific research,
commissioned or at least partly funded by the sugar industry, has been questioned because
of financial conflicts of interests. Indeed, a study from 2013 showed that scientific studies in
this field, which reported possible financial conflicts of interest, “were five times more likely to
report a conclusion of no positive association between [sugar-sweetened beverages]
consumption and weight gain or obesity than those reporting having no industry sponsorship
or conflicts of interest.”418 Moreover, the American Beverage Association has challenged
scientific findings and publications claiming a connection between sugar-sweetened
beverages and health issues at several occasions.419 The industry even developed a website
attempting to debunk scientific findings which related obesity and dental caries to sugars
consumption, entitled “Let’s Clear It Up”.420 Against this background of heavy political
engagement in scientific research, the WHO started its guideline development process.
The development process for the guideline is described at length in the text of the guideline. A
picture, available on the WHO website, is added in Annex III. The main responsibility rested
with the WHO Department of Nutrition for Health and Development (NHD), which cooperated
with the WHO Secretariat. Guidance was provided by the WHO Steering Committee for
Nutrition Guideline Development. The actual guideline was developed by the WHO Nutrition
Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health, which was formed
especially for this purpose. Although the WHO Secretariat spared no efforts in ensuring a good
balance of experts involved, industry experts were not invited “because the inclusion of such
individuals is considered to be inappropriate for membership of any WHO guideline group
411 Even Credit Suisse published a report critical of our current sugars intake levels. See Credit Suisse, ‘Is Sugar Turning the Economy Sour?’ (22 October 2013), https://www.credit-suisse.com/us/en/news-and-expertise/topics/health-care.article.html/article/pwp/news-and-expertise/2013/09/en/is-sugar-turning-the-economy-sour.html. 412 This Institute’s website is http://www.responsiblefoods.org/. 413 Information on this initiative is available at http://www.actiononsugar.org/. 414 See Zoe Williams, ‘Robert Lustig: the man who believes sugar is poison’ (24 August 2014), http://www.theguardian.com/lifeandstyle/2014/aug/24/robert-lustig-sugar-poison; Servaas van der Laan, ‘Vertelt ‘suikergoeroe’ Robert Lustig wel het eerlijke verhaal?’ (9 mei 2015), http://www.elsevier.nl/Buitenland/achtergrond/2015/5/Ook-suikergoeroe-Robert-Lustig-is-niet-onomstreden-1759904W/ 415 Institute for Responsible Nutrition, ‘Why aren’t all calories the same?’, http://www.responsiblefoods.org/a_calorie_is_not_a_calorie. 416 It is also exemplified by Robert Lustig’s performance at a TEDx-event. See https://www.youtube.com/watch?v=gmC4Rm5cpOI 417 David Katz, ‘Sugar Isn’t Evil: A Rebuttal’ (The Huffington Post, 18 June 2011) <http://www.huffingtonpost.com/david-katz-md/sugar-health-evil-toxic_b_850032.html> accessed 11 August 2015. 418 Maira Bes-Rastrollo and others, ‘Financial Conflicts of Interest and Reporting Bias Regarding the Association between Sugar-Sweetened Beverages and Weight Gain: A Systematic Review of Systematic Reviews’ (2013) 10 PLoS Med 1, 3. 419 See, for example, ‘Beverage Industry Responds to British Medical Journal Paper on Diabetes’ (22 July 2015) <http://www.ameribev.org/news-media/news-releases-statements/more/360/> accessed 10 September 2015; ‘Beverage Industry Responds to Study That Purports to Link Beverages to Global Disease’ (30 June 2015) <http://www.ameribev.org/news-media/news-releases-statements/more/359/> accessed 10 September 2015. 420 See http://www.letsclearitup.org/

64
because of actual, potential and perceived conflicts of interest.”421 An external peer-review
group was equally set up to “to review the draft guideline to identify any errors or missing
information before finalization of the guideline.”422 According to the Sugar Guideline, “[t]he
WHO Secretariat selected, as external peer reviewers, representatives of public institutions
that are members of the WHO Global Network of Institutions for Scientific Advice on Nutrition,
subject-matter experts (including those in dentistry) and other stakeholders (including
practitioners and editors of scientific journals).”423 The combination of an expert-manned
guideline development committee (NUGAG) and an external peer-review group was meant to
ensure that any recommendations made were based on sound scientific grounds.
In addition, public consultations were organized at two occasions. Firstly, “[a] public
consultation was held during the planning stages of guideline development”, which “called for
comments on the scope of the guideline and on the specific research questions to be
addressed and outcomes to be investigated in the systematic literature reviews.”424 Secondly,
“a public consultation was held to call for comments on the draft guideline before its
finalization.”425
The Sugar Guidelines made three closely-related recommendations: (1) “a reduced intake of
free sugars throughout the lifecourse”; (2) “reducing the intake of free sugars to less than 10%
of total energy intake”; and (3) “a further reduction of the intake of free sugars to below 5% of
total energy intake.” The first two recommendations constitute “strong recommendations”,
which means that scientific evidence conclusively shows that the benefits of adopting the
recommendation outweigh the possible adverse effects, and “the recommendation can be
adopted as policy in most situations”.426 The third recommendations, on the other hand, is a
“conditional recommendation”, for which there is less certainty that the balance will be in favor
of the recommendations, and, consequently, “policy-making will require substantial debate and
involvement of various stakeholders.”427 These three recommendations form a benchmark
against which policy-makers can assess current dietary patterns within their constituencies.
With regard to implementation, the guideline refer to existing practices, such as “food and
nutrition labelling, consumer education, regulation of marketing of food and non-alcoholic
beverages that are high in free sugars, and fiscal policies targeting foods and beverages that
are high in free sugars.”428 It is stressed that they require a broader framework and should be
implemented “in conjunction with other nutrient guidelines and dietary goals”.429
Unsurprisingly, the sugar and food industry were not pleased with the contents of the guideline,
as the recommendations made – if taken seriously – could greatly impact on their sales. The
Sugar Association criticized the drafting process for a lack of transparency in a letter addressed
to Director-General Chan430, and the Comité Européen des Fabricants de Sucre (CEFS) raised
421 Sugar Guideline, 8. 422 Ibid. 423 Ibid. 424 Ibid., 9. 425 “A total of 173 comments were received, from representatives of 24 government agencies, two UN agencies, 52 NGOs, 54 industry organizations and associations, 31 academic institutions and 10 other interested individuals. These comments were also reviewed by the WHO Secretariat, and were assessed and considered when finalizing the guideline. A list of people who submitted comments in response to the public consultations, summaries of their comments and the assessment of the received comments by the WHO Secretariat are available on the NHD website.” 426 Ibid., 16. 427 Ibid. 428 Ibid., 18. 429 Ibid. 430 Sugar Association, ‘The Sugar Association Voices Concern Regarding the World Health Organization (WHO) Draft Guideline Development Process and Lack of Transparency’ (The Sugar Association, 4

65
doubts about the validity of the scientific research underlying the recommendations, both
during the consultation round431 and with regard to the final outcome432. Moreover, similarly to
the tobacco industry, the sugar industry referred to the possible impact on the economy of all
kinds of possible measures. In its comments to the Draft Guidelines, the Sugar Association
noted that “the WHO is a powerful and highly respected voice; the implications of such
guidance have significant impact not only on public health, but also to multiple sectors of the
global economic landscape, particularly in developing countries.”433
Several methods are open for implementation of these guidelines.434 The Flemish government
does not have the necessary competences for every method. Competences with regard to
food and nutrition labelling435, agricultural policies436, and regulation of marketing of food and
non-alcoholic beverages are mainly situated at the EU level, and, although Flanders’ fiscal
autonomy has further increased with the last State reform, fiscal policy largely remains a
federal competence. Indeed, the federal government is preparing the establishment of a tax
on beverages. However, although initial proposals concerned a tax on sugar-sweetened
beverages only,437 the government finally opted for a tax on all sodas, including light versions
and versions without any sugar.438 Next to fiscal policy, and although the EU has important
competences with respect to food safety439, the federal government has retained the main
competence with regard to non-safety standards for products, including food products.
September 2014) <http://www.sugar.org/sugar-association-voices-concern-regarding-world-health-organization-draft-guideline-development-process-lack-transparency/> accessed 10 September 2015. 431 CEFS, ‘CEFS Comments to the Draft WHO Guideline on Sugars Intake for Adults and Children’ (2014) <http://www.comitesucre.org/site/wp-content/uploads/2014/04/CEFS-Comments-to-Draft-WHO-Guideline-on-Sugars-28-03-2014.pdf> accessed 10 September 2015. 432 Comité Européen des Fabricants de Sucre, ‘EU Sugar Producers Response to New WHO Guideline on Sugars Intake for Adults and Children’ (4 March 2015) <http://www.comitesucre.org/site/eu-sugar-producers-response-to-new-who-guideline-on-sugars-intake-for-adults-and-children/> accessed 10 September 2015. 433 Their comments, voiced on 28 August 2014, are available at http://www.sugar.org/sugar-association-voices-concern-regarding-world-health-organization-draft-guideline-development-process-lack-transparency/. 434 As we have noted in the introduction, it is difficult to ascertain whether certain policies/legal instruments have been adopted because of WHO’s initiatives. Indeed, causality is a tricky element to proof. We advise the reader to keep this in mind: not all Flemish and European policy initiatives will have been started up because of WHO’s initiatives. 435 See European Commission, ‘Food – Nutrition claims’, http://ec.europa.eu/food/safety/labelling_nutrition/claims/nutrition_claims/index_en.htm. See also European Food Information Council (EUFIC), ‘Nutrition labelling becomes mandatory in Europe’ (May 2012), http://www.eufic.org/article/en/artid/Nutrition-labelling-becomes-mandatory-in-Europe/. 436 For a study of the impact of the European sugar policies on Flemish farmers, see Pieter Gabriels, ‘Gevolgen van de hervorming van het EU-suikerbeleid voor de Vlaamse landbouwer’ (October 2004), available at http://www2.vlaanderen.be/landbouw/downloads/volt/21.pdf. 437 ‘“Suikertaks Op Frisdrank Vanaf 2016”’ (Knack, 18 September 2015) <http://www.knack.be/nieuws/belgie/suikertaks-op-frisdrank-vanaf-2016/article-normal-606257.html> accessed 18 September 2015. As a reaction, the soda companies have already upped their prices. See ‘Frisdrank Al Duurder Nog Vóór Suikertaks’ (HLN, 18 September 2015) <http://www.hln.be/hln/nl/943/Consument/article/detail/2428512/2015/08/19/Frisdrank-al-duurder-nog-voor-suikertaks.dhtml> accessed 18 September 2015. 438 See ‘De Block over suikertaks: “Ik was van plan om te wachten’ (Knack, 12 Oktober 2015). 439 See Regulation No 178/2002 of the European Parliament and of the Council of 28 January 2002 laying down the general principles and requirements of food law, establishing the European Food Safety Authority and laying down procedures in matters of food safety [2002] OJ L31/1. The text of this regulation is available online at http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32002R0178&from=EN.

66
A matter which is in Flemish hands, is consumer education.440 On the basis of article 58 of the
Decree of 21 November 2003 concerning the policy for preventive health care, the Flemish
government is estimated to develop initiatives to promote healthy nutritional habits. And,
indeed, the Flemish government has invested heavily in campaigns promoting healthier food,
for example by discouraging the consumption of (free) sugars.441 In addition, the Flemish
government disseminates information on healthy nutrition to different health care providers. To
this end, a consensual text (consensustekst) has been developed. The WHO’s guidelines and
standards have been taken as a benchmark for this guidance document.442 However, as the
Sugar Guideline has only recently been adopted and published, it is too early to discuss
whether this new guideline with its lower recommended sugars intake, will impact on Flemish
policy and, for example, lead to a renewed educational focus on free sugars.
The Sugar Guideline has also received attention from media, leading to a more direct impact
on individuals. One interesting example is the “suikertest” on the website of De Standaard, a
Belgian newspaper, which became available on 14 September 2015.443 In assessing whether
your sugar consumption is healthy, the test explicitly and exclusively refers to the WHO’s
standards.
3.3 Impact on private actors
3.3.1 Introduction
Policy-makers are not the only possible target audience for WHO guidelines. The Handbook
for Guideline Development states that “the audiences that WHO guidelines can target include
public health policy-makers, health programme managers, health-care providers, patients,
caregivers, the general public and other stakeholders.”444 Indeed, WHO often engages directly
with individuals and/or organizations “on the ground” in its guidelines. Even the Sugar
Guideline discussed above was not exclusively directed at policy-makers, but could also be
used by nutritional specialists.
A distinction should also be made between the target audience of the guideline and others
possibly affected thereby. Recommendations directed towards doctors or hospitals will
440 The Flemish Community is the competent with respect to preventive health care. See Decree of 21 November 2003 concerning the policy for preventive health care, available at http://codex.vlaanderen.be/Portals/Codex/documenten/1012025.html. See also Flemish Agency for Care and Health, ‘Preventie’, www.zorg-en-gezondheid.be/preventie/. 441 An overview of different programmes supported by the Flemish government can be found at http://www.zorg-en-gezondheid.be/Gezond-leven-en-milieu/Voeding-en-beweging/Campagnes-en-projecten-rond-voeding-en-beweging/. 442 “Internationaal gelden de aanbevelingen van de Wereldgezondheidsorganisatie WHO als standaard.” See Ministerie van Welzijn, Volksgezondheid en Gezin, ‘Vlaamse consensustekst in verband met evenwichtige voeding en beweging, ten behoeve van zorgverstrekkers’ (2012), available at www.eetexpert.be, 6. At page 54, the text also iterates the following: “De WHO definieert gezondheid als een toestand van volledige fysiek, mentaal en sociaal welzijn en niet enkel als de afwezigheid van ziekte. In overeenstemming met deze definitie, zou communicatie opgebouwd moeten zijn vanuit een holistisch perspectief, waar gelijke aandacht wordt gegeven aan sociale, emotionele en fysieke aspecten van gezondheid. Boodschappen mogen dus niet enkel de nadruk leggen op voldoende fysieke activiteit en gezonde voeding, maar ook op het bevorderen van zelfwaardering, tevredenheid met het lichaam en respect voor diversiteit in lichaamsmaten.” 443 The test was available at the following hyperlink: http://www.standaard.be/suikertest. 444 World Health Organization, WHO Handbook for Guideline Development (n 20) 2.

67
inevitably also affect patients. In the same vein, recommendations with regard to the pricing of
pharmaceutical products directed at policy-makers will inevitably affect producers and
distributors of these pharmaceutical products.
Given the great diversity and variety of WHO recommendations and guidelines, painting a
complete picture of the different actors impacted upon is impossible. However, we will present
one example in the following section. On the basis of earlier interviews, we have opted to look
at the impact of the “Clean Care is Safer Care” programme on health-care providers in general,
and hospital managers more specifically.
3.3.2 Impact on health-care providers and hospital managers: hygiene guidelines
In 2002, after a presentation by the WHO Secretariat445 explaining the dangers of adverse
effects from surgical and other medical operations, the WHA asked the WHO (Secretariat and
Member States) to bring the problem of patient safety in the limelight.446 In its resolution
WHA55.18, it asked the Director-General “to develop global norms, standards and guidelines
for quality of care and patient safety” and “to support the efforts of Member States to promote
a culture of safety within health care organizations and to develop mechanisms, for example
through accreditation or other means, in accordance with national conditions and
requirements, to recognize the characteristics of healthcare providers that offer a benchmark
for excellence in patient safety internationally”447, giving him a clear mandate to develop
normative guidelines.
To coordinate this effort, the WHO created an international alliance to improve patient safety
under the denominator “World Alliance for Patient Safety” in October 2004.448 The World
Alliance for Patient Safety has developed initiatives on the basis of biennial “Global Patient
Safety Challenges”, the first of which ran from 2005-2006 and was entitled “Clean Care is Safer
Care”.449 This resulted, inter alia in the guidelines on hand hygiene, which will be further
discussed below. A second campaign, “Safe Surgery Saves Lives” was initiated, which
resulted both in WHO Guidelines on Safe Surgery and in a basic checklist, the “Surgical Safety
Checklist”.450 Afterwards, to our knowledge, no further Global Patient Safety Challenges were
launched. Moreover, the programmes which were initially conceived as biennial, are still
running.451
The objective of the WHO in these programmes was to reduce the number of health care-
associated infections (HCAIs) by improving on hand hygiene in health care settings through a
twofold strategy: by conducting, collecting, assessing, structuring and disseminating research
on the issue (inter alia in the form of normative guidelines) and by raising awareness. Indeed,
445 WHO, ‘Quality of care: patient safety’ (Report by the Secretariat, 23 March 2002), WHO Docs. A55/13, available at http://apps.who.int/gb/archive/pdf_files/WHA55/ea5513.pdf?ua=1 446 WHA Resolution on ‘quality of care: patient safety’ (18 May 2002), WHO Docs. WHA55.18, available at http://apps.who.int/gb/archive/pdf_files/WHA55/ewha5518.pdf?ua=1 447 As such, it becomes clear that WHO guidelines are rarely addressed to one actor exclusively. 448 Didier Pittet and Liam Donaldson, ‘Clean Care Is Safer Care: The First Global Challenge of the WHO World Alliance for Patient Safety’ (2005) 33 American Journal of Infection Control 476, 476. 449 ibid. 450 See WHO, ‘Safe Surgery Saves Lives’ (2009), available at http://apps.who.int/iris/bitstream/10665/70080/1/WHO_IER_PSP_2008.07_eng.pdf. See also WHO, ‘Patient Safety – Safe Surgery’, http://www.who.int/patientsafety/safesurgery/en/. 451 Pittet mentioned Clean Care is Safer Care as an ongoing programme in a presentation dated May 5, 2015. The presentation is available at http://www.who.int/gpsc/5may/slcyh-10years.pdf?ua=1.

68
a lack of research or scientific uncertainty were not the only – and perhaps not even the main
– issue, and ‘simple dissemination strategies have been described as unlikely to have any
impact at all on implementation’452. Several health-care workers, both in developing and
developed countries, were insufficiently aware of the potential dangers stemming from a lack
of hygiene (especially hand hygiene). Awareness raising through campaigns was considered
indispensable to properly convey the message. The central objective were furthered by the
development on guidelines and by several awareness campaigns – or social marketing
strategy as they call it themselves453, such as the #safeHANDS-campaign or the “SAVE LIVES:
Clean Your Hands”-campaign454, which includes the famous Five Moments of Hand
Hygiene.455 In addition, governments are pressured to “pledge”456 their support to the campaign
in order to add weight to the campaign and an informal network of campaigning countries,
“WHO CleanHandsNet”457, has been established.
In the WHO’s campaign for better hand hygiene in health care, simplicity and accessibility of
instruments seems to be central. This is evidenced by the WHO Multimodel Hand Hygiene
Improvement Strategy458, which includes a Self-Assessment Framework developed in 2010,
which helps individual health-care facilities assess and improve its own performance with
regard to hand hygiene.459
These initiatives were mainly aimed at improving the hygiene of health procedures in
developing countries. Indeed, in developed countries, health procedures were already subject
to rules ensuring hygiene. Although the WHO’s campaign also became popular in developed
countries, especially through its simple schematics, such as My Five Moments of Hand
Hygiene, they did not replace the existing hygienic procedures. Most of these procedures do,
however, conform to the WHO recommendations, even without strictly applying them.460 This
reflects a more general trend, where several of WHO’s guidelines and/or recommendations
are mainly relevant for developing countries, because developed countries generally already
are in conformity with most of the latest developments in health research.
3.4 The development of pharmaceutical products
3.4.1 A broad approach: development phases of pharmaceutical products
452 WHO, WHO Guidelines on Hand Hygiene in Health Care (2009) 175 <http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf?ua=1>. 453 See the ninth slide of Pittet’s presentation mentioned in footnote 439. 454 Information about this campaign is available on its website, which can be found at http://www.cleanhandssavelives.org/safehands/. 455 A chart of these five moments is available at http://www.who.int/gpsc/5may/Your_5_Moments_For_Hand_Hygiene_Poster.pdf. 456 See WHO, ‘Clean Care is Safer Care - Support from WHO Member States and autonomous areas’, http://www.who.int/gpsc/statements/en/. 457 See WHO, ‘Clean Care is Safer Care - Background to WHO's facilitated country or area campaigns informal network’, http://www.who.int/gpsc/national_campaigns/background/en/. 458 See WHO, ‘Clean Care is Safer Care – Tools and resoures’, http://www.who.int/gpsc/5may/tools/en/. 459 WHO, Hand Hygiene Self-Assessment Framework 2010: Introduction and user instructions, available at http://www.who.int/gpsc/country_work/hhsa_framework_October_2010.pdf?ua=1 460 However, there are examples where hospitals made use of the WHO’s simple schematics. See, for example, Kristin Alt Styer and others, ‘Implementing the World Health Organization Surgical Safety Checklist: A Model for Future Perioperative Initiatives’ (2011) 94 Association of Operating Room Nurses. AORN Journal 590.

69
At the outset of this section, a methodological note is in order. In contrast with the former
sections, we have opted for a different, broader approach to case studies in this section. Rather
than discussing one guideline in depth, we will demonstrate here how different WHO guidelines
and programmes affect the different stages of the development of pharmaceutical products.
With this change in methodology, we aim to demonstrate the great number of WHO guidelines
(and other instruments or actions) that impact on a single, albeit complex, process.461
The development of a pharmaceutical product occurs in several different phases, and involves
several different legal and policy issues.462 Accordingly, we will divide this section into three
different parts to reflect three major phases in the process, although, admittedly, the process
is not so easily divided in three phases, and some of the guidelines discussed will concern two
or even all three of the phases.463 The three phases concerned are (1) the research and
development phase; (2) the phase of registration of the product (both in terms of intellectual
property rights and in terms of market authorization); and (3) the phase of manufacturing,
distributing and marketing464 (including the issue of pharmacovigilance465 and the regulation of
medicine promotion and information).
On the basis of article 2(u) of its Constitution, the WHO has been mandated to “develop,
establish and promote international standards with respect to food, biological, pharmaceutical
and similar products.” The development of international standards for the different phases of
pharmaceutical product development is thus an integral part of the WHO’s work package, and,
on this basis, WHO has been engaged in all of these phases in some way. However, it has not
only designed standards for different processes (e.g. manufacturing practices or clinical trials),
but also attempted to promote a more equitable world order, by inter alia promoting more
pharmaceutical research with regard to type II and type III diseases, i.e. diseases which are
more or most prominent in developing countries. In addition, at certain points in time, the WHO
has also had a very specific impact. This was the case, for example, during the Ebola crisis,
where the WHO allowed for the speeding up of the clinical trials procedures for Ebola
medicines and vaccines.
The development of standards for pharmaceutical and related products is in the hands of the
WHO Essential Medicines and Health Products (EMP) Department, which forms part of the
461 A first taste of the diversity of issues the WHO deals with when it comes to the pharmaceutical sector comes from the pdfs compiled in 2011 as a precursor to the update of the World Medicines Report of 2004. This collection of pdfs is available online. See WHO, The World Medicines Situation Report (3rd edition, 2011), available at http://apps.who.int/medicinedocs/documents/s20054en/s20054en.pdf?ua=1. 462 A 2004 WHO report identified, for example, three ‘main components of stewardship in the medicines market’ – or areas where policy intervention is required, namely ‘product registration: assessing and authorizing products for market entry, and monitoring their effectiveness and safety after entry; regulation of manufacturing, importation and distribution; and regulation of medicine promotion and information.’ WHO, The World Medicines Situation, available at http://apps.who.int/medicinedocs/pdf/s6160e/s6160e.pdf, 93. 463 Alternatively, we could categorize the different guidelines and programmes on the basis of subject-matters. The WHO takes this approach on its website. With regard to pharmaceutical companies, the WHO has an impact in different fields, where it utilizes the following categories: policy, access and use; public health, innovation and intellectual property; regulation of medicines and other health technologies; prequalification of medicines, vaccines, diagnostics and devices; regulatory system strengthening; and safety and vigilance. See http://www.who.int/medicines/areas/en/. 464 This includes the decision on the price of the product, a matter which is also of concern to the WHO. See http://apps.who.int/iris/bitstream/10665/153920/1/9789241549035_eng.pdf?ua=1 465 WHO considers pharmacovigilance to form part of the clinical trial phase (as the fourth phase of the clinical trial). See http://www.who.int/ictrp/glossary/en/#TrialPhase

70
Cluster of Health Systems and Innovation (HIS).466 The European Regional Office also plays
a role in this field.467 In the European Region, the Health Technologies and Pharmaceuticals
Programme falls under the Division of Health Systems and Public Health.
On the other, implementing, end of the spectrum, the division of legal competences in the field
of pharmaceutical products is quite complex. The EU holds an important competence in the
field of pharmaceutical products regulation, as EU action is considered necessary to balance
the functioning of the internal market and the safeguarding of public health. It has developed
an extensive legal framework in this field for the entire European Economic Area (EEA). The
development of this framework was triggered in the 1960s by the thalidomide disaster.468
Central to the current framework are a Directive 2001/83/EC, adopted in 2001 and regularly
amended since, establishing a ‘Community Code relating to medicinal products for human use’
(hereafter ‘the Medicines Directive’)469 and a Regulation No. 726/2004, adopted in 2004 and
equally subject to regular amendment, ‘laying down Community procedures for the
authorization and supervision of medicinal products for human and veterinary use and
establishing a European Medicines Agency’ (hereinafter ‘the Medicines Regulation’).470 With
regard to the Medicines Directive, we can already refer to a general obligation of information
for Member States towards the WHO: article 123.3 of the directive requires Member States to
notify the WHO if and when actions taken with regard to medicinal products (e.g. withdrawal
of the marketing authorization) might affect third states. Institutionally, the European Medicines
Agency (EMA) established by the latter instrument is the centerpiece of the framework,
although the European Commission is equally involved (through DG Sanco)471. In accordance
with recital (19) of the Medicines Regulation, “the chief task of the Agency should be to provide
Community institutions and Member States with the best possible scientific opinions so as to
enable them to exercise the powers regarding the authorisation and supervision of medicinal
products conferred on them by Community legislation in the field of medicinal products.” Recital
(27) stipulates that the EMA should “participate actively in international scientific dialogue and
develop certain activities that will be necessary, in particular regarding international scientific
harmonisation and technical cooperation with the World Health Organisation.”472 Given the
high prominence of the European level in this field, pharmaceutical companies in general opt
to lobby at the European level, rather than at the national level. In this regard, it is important to
466 See WHO, ‘Essential medicines and health products – About us’, available at http://www.who.int/medicines/about/en/. 467 See WHO/Europe, ‘Medicines’, available at http://www.euro.who.int/en/health-topics/Health-systems/medicines/medicines. For an overview of its activities in 2014, see WHO/Europe, ‘Health Technologies and Pharmaceuticals (HTP) Programme: Annual Report 2014’, available at http://www.euro.who.int/__data/assets/pdf_file/0007/276667/Health-Technologies-Pharmaceuticals-HTP-programme-Annual-Report-2014.pdf?ua=1. 468 James H Kim and Anthony R Scialli, ‘Thalidomide: The Tragedy of Birth Defects and the Effective Treatment of Disease’ (2011) 122 Toxicological Sciences 1. 469 A consolidated version is available at http://ec.europa.eu/health/files/eudralex/vol-1/dir_2001_83_consol_2012/dir_2001_83_cons_2012_en.pdf. 470 A consolidated version is available at http://ec.europa.eu/health/files/eudralex/vol-1/reg_2004_726/reg_2004_726_en.pdf. Several other directives and regulations have been adopted in this field. An overview is available at http://ec.europa.eu/health/documents/eudralex/vol-1/index_en.htm. 471 The European Commission, for example, has ‘the task of coordinating the execution of the various supervisory responsibilities vested in the Member States, and in particular with the tasks of providing information on medicinal products and of checking the observance of good manufacturing, laboratory and clinical practices.’ See recital (31) of the Medicines Regulation. 472 Further on EMA-WHO cooperation, see EMA, ‘World Health Organization (WHO)’, http://www.ema.europa.eu/ema/index.jsp?curl=pages/partners_and_networks/general/general_content_000230.jsp&mid=WC0b01ac05801df742.

71
refer to the European Federation of Pharmaceutical Industries and Associations (EFPIA),
which is the main lobby group for the pharmaceutical industry at the European level.
At the national level, the competence with regard to pharmaceutical products has remained
largely at federal level.473 The basic legal document in this field is the 1964 law on medicinal
products, which has been most recently amended in 2012 to implement changes in the
Medicines Directive.474 In 2007, a Federal Agency for Medicinal Products and Pharmaceuticals
(‘Federaal Agentschap voor Geneesmiddelen en Gezondheidsproducten’) (hereinafter FAGG)
has been established which monitors the abidance with the Belgian legislation on
pharmaceutical products.475 It “guards, in the interest of public health, the quality, safety and
efficacy of pharmaceutical products, in clinical development and on the market.”476
3.4.2 The R&D phase: steering R&D and clinical trials
In the pharmaceutical industry, the phase of research and development (R&D) is one of the
most important phases in the production process. It often spans several years, and is extremely
costly.477 In part, this is due to the requirement to conduct substantive and thorough clinical
trials in (at least) three phases if a pharmaceutical product is meant for human use.
The WHO already intervenes in this R&D phase. Not only has it elaborated international
standards with regard to clinical trials as it has been explicitly mandated under article 2(u)
WHO Constitution (see below), it also attempts to steer the R&D investments. The WHO has
made serious efforts, especially in the last few years, to promote health research with regard
to so-called type II and type III diseases, which are respectively diseases of which a substantial
proportion of the cases are found in developing countries or which incident overwhelmingly or
almost exclusively in these countries.478 We have already shortly referred to these efforts in
section 2.2.2. Indeed, at least since 2003, the WHO has attempted to make global health
research more equitable. In that year, the WHA established the “Commission on Intellectual
Property Rights, Innovation and Public Health”, with the objective to “collect data and proposals
from the different actors involved and produce an analysis of intellectual property rights,
innovation, and public health, including the question of appropriate funding and incentive
mechanisms for the creation of new medicines and other products against diseases that
disproportionately affect developing countries.”479 This Commission finalized its report in
2006.480 As a follow-up, an Intergovernmental Working Group was established, which
473 For an overview of the Belgian legislation with regard to pharmaceutical products, see http://www.pharma.be/newsitem.aspx?nid=740. 474 See FAGG, ‘Geneesmiddelenbewaking’, available at http://www.fagg-afmps.be/nl/geneesmiddelenbewaking/. 475 Law of 20 July 2006 concerning the establishment and the functioning of the federal Agency for medicinal products and pharmaceuticals, BS 8 September 2006. A consolidated version is available at http://www.ejustice.just.fgov.be/cgi_loi/change_lg.pl?language=nl&la=N&cn=2006072078&table_name=wet. 476 See FAGG, ‘Over het FAGG’, available at http://www.fagg-afmps.be/nl/fagg/. 477 Joyce ter Heerdt, ‘Research and Development of Medicinal Products: Clinical Trials’ in Stefaan Callens (ed), Chapters on Pharmaceutical Law (Intersentia 2000) 17. 478 WHO Secretariat, ‘Defining Diseases Type I, II and III’ (14 November 2012), available at http://www.who.int/phi/3-background_cewg_agenda_item5_disease_types_final.pdf. 479 WHO, Resolution on ‘Intellectual property rights, innovation and public health’ (28 May 2003), WHO Docs. WHA56.27, available at http://apps.who.int/gb/archive/pdf_files/WHA56/ea56r27.pdf. 480 WHO, ‘Public health, innovation and intellectual property rights. Report of the Commission on Intellectual Property Rights, Innovation and Public Health’ (2006), available at http://www.who.int/intellectualproperty/documents/thereport/ENPublicHealthReport.pdf.

72
elaborated a Global Strategy and a concomitant Plan of Action (the GSPA-PHI).481 Afterwards,
a Consultative Expert Working Group further explored opportunities to finance research with
regard to type II and type III diseases (see above). Despite suggestions by the Consultative
Expert Working Group that a binding convention is essential to ensure sufficient investment in
this type of health research, the debate has now focused on funds established from voluntary
contributions, although the GSPA-PHI contains several other elements (108 specific actions in
total). This entire programme is led by the Public Health, Innovation and Intellectual Property
(PHI) Team.482 It seems too early to attempt to measure the effect or impact of these actions
by the WHO, as the debate is still very much ongoing and not much action has yet been
undertaken.483 It is, however, important to note that, in the framework of the right to health
discourse, the WHO has taken it upon itself to promote a more equitable world order.484
The WHO also plays a role in facilitating research, for example, through the WHO Pandemic
Influenza Preparedness Framework, which requires sharing of viruses and of vaccines.485 The
legal importance of this framework is underscored by Fidler and Gostin when they state that
“[this] framework uses standard agreements for laboratories and manufacturers participating
in [the Global Influenza Surveillance and Response System], creating legal consequences for
contracting partners.”486
We have also noted the importance of clinical trials in this first phase. During these clinical
trials, pharmaceutical products, which have already been extensively tested in cultures and on
test animals beforehand, are tested on humans in (at least) three different phases, which we
have already described in section 2.3.3. Given the risks involved in this process, these clinical
trials are subject to strict regulation. This regulation has been harmonized between different
states to a large extent. The main forum for harmonization efforts is the International
Conference for the Harmonisation of Technical Requirements for Registration of
Pharmaceuticals for Human Use (ICH).487 In this forum, three major public partners (the
pharmaceutical regulators from the EU, Japan and the United States) have the lead – with
their Canadian and Swiss counterparts being involved in a more secondary role. However,
private actors, and mainly the pharmaceutical industry, equally play an important role. The
European pharmaceutical industry is represented by EFPIA, while the Secretariat of the
Conference is run by the International Federation of Pharmaceutical Manufacturers and
Associations (IFPMA)488. This initiative came forth from the WHO Conference of Drug
Regulatory Authorities (ICDRA), in Paris, in 1989,489 and the WHO is still involved as an
481 Lisa Forman, ‘The Intergovernmental Working Group on Public Health, Innovation and Intellectual Property’ in OHCHR (ed), Realizing the Right to Development: Essays in Commemoration of 25 Years of the United Nations Declaration on the Right to Development (United Nations 2013) <http://www.ohchr.org/Documents/Issues/Development/RTDBook/PartIIIChapter22.pdf> accessed 18 December 2015. 482 WHO, ‘Public health, innovation, intellectual property and trade’, http://www.who.int/phi/about/en/. 483 WHO, ‘Follow-up of the report of the Consultative Expert Working Group on Research and Development: Financing and Coordination’ (Report by the Director-General, 19 December 2014), WHO Docs. EB 136/30, available at http://apps.who.int/gb/ebwha/pdf_files/EB136/B136_30-en.pdf. 484 In the light of this objective, and even within the same programme (the GSPA-PHI), actions are also undertaken which are relevant for other phases (e.g. with regard to the pricing of pharmaceutical products). 485 Fidler and Gostin (n 265). 486 ibid 200. 487 Information on the ICH is available on its website: http://www.ich.org/home.html. The ICH adopted a Guideline for Good Clinical Practice on 10 June 1996, which is available online at http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf. 488 See http://www.ifpma.org/ 489 ICH, ‘History’, http://www.ich.org/about/history.html.

73
observer, bringing its expertise to the table.490 As such, it plays more of a support role, rather
than taking the lead in this process. 491 The standards developed by the ICH are used by the
EU and its Member States.492
However, with regard to the registration of clinical trials, the WHO has been playing a more
prominent role in the last decade. Although WHO was one of the first organizations to refer to
the issue of unregistered clinical trials, and the problems it raised for consistent health
research, more influential was probably the statement by the International Committee of
Medical Journal Editors (ICMJE) from 2005 that it would not consider papers based on non-
registered trials for publication.493 The demand for registration of clinical trials was, moreover,
strongly supported at the 2004 Ministerial Summit on Health Research in Mexico City.494 It was
subsequently reiterated in WHA resolution 58.34, which mandated the Director-General “to
pursue with interested partners the development of a voluntary platform to link clinical trials
registers.”495 Since this resolution, the WHO Secretariat has been developing a system
whereby several registration database form part of the larger WHO International Clinical Trials
Registry Platform (WHO ICTRP).496 It has equally developed standards for submitting clinical
trials for registration to the WHO ICTRP, which concern, for example, which information should
be submitted for registration.497
The importance of this database is evidenced by the fact that, in the future, data from clinical
trials in the EU should be registered in the WHO ICTRP, for lack of which they will not be taken
up in the application dossier for authorization of a clinical trial.498 The registration system for
clinical trials also serves to promote more transparency with regard to the results of clinical
trials in order to further knowledge on public health issues.499 More importantly, the collection
490 “Since the outset of ICH, WHO has participated as an Observer to the Steering Committee.” See ICH, ‘Steering Committee’, http://www.ich.org/about/organisation-of-ich/steering.html. 491 The WHO also provides guidelines on best research practices for clinical trials. See, for example, WHO, ‘Guidelines for good clinical practice (GCP) for trials on pharmaceutical products’ (1995) WHO Technical Report Series, No 850, Annex 3, available at http://apps.who.int/medicinedocs/pdf/whozip13e/whozip13e.pdf; WHO, Handbook for Good Clinical Research Practice (GCP): Guidance for Implementation (WHO Press 2002), available at http://apps.who.int/prequal/info_general/documents/gcp/gcp1.pdf. However, on this matter, it refers to the guidelines of the International Conference on Harmonization (ICH) itself. Still, it should be kept in mind that the WHO has played an important role in establishing the ICH, and continues to play a role in its workings. See ICH, ‘History’, http://www.ich.org/about/history.html. 492 The EU’s guidelines and legislation with regard to clinical trials are available at http://ec.europa.eu/health/documents/eudralex/vol-10/index_en.htm. 493 A Metin Gülmezoglu and others, ‘WHO Facilitates International Collaboration in Setting Standards for Clinical Trial Registration’ (2005) 365 The Lancet 1829. 494 http://www.who.int/rpc/summit/agenda/en/mexico_statement_on_health_research.pdf?ua=1 495 WHA Resolution on the ‘Ministerial Summit on Health Research’ (25 May 2005), WHO Docs. WHA58.34, available at http://apps.who.int/gb/or/e/e_wha58r1.html. 496 WHO, ‘International Clinical Trials Registry Platform (ICTRP) – Welcome to the WHO ICTRP’, http://www.who.int/ictrp/en/. See also Timothy Evans, Metin Gülmezoglu and Tikki Pang, ‘Registering Clinical Trials: An Essential Role for WHO’ (2004) 363 The Lancet 1413. 497 WHO, International Standards for Clinical Trial Registries (WHO Press 2012), available at http://apps.who.int/iris/bitstream/10665/76705/1/9789241504294_eng.pdf. 498 Article 25.6 of Regulation No 536/2014 of the European Parliament and of the Council of 16 April 2014 on clinical trials on medicinal products for human use, and repealing Directive 2001/20/EC [2014] OJ L158/1. The text of this regulation is available at http://ec.europa.eu/health/files/eudralex/vol-1/reg_2014_536/reg_2014_536_en.pdf. The EU Directive 2001/20, which has been replaced by the Regulation No 536/2014, did not include such a requirement. 499 ‘WHO Statement on Public Disclosure of Clinical Trials Results’, available at http://www.who.int/ictrp/results/WHO_Statement_results_reporting_clinical_trials.pdf. See Vasee S Moorthy and others, ‘Rationale for WHO’s New Position Calling for Prompt Reporting and Public Disclosure of Interventional Clinical Trial Results’ (2015) 12 PLoS Med e1001819; D Ghersi and others,

74
of this kind of data in a single registration database would allow for better coordination and
steering of ongoing health research.500
3.4.3 Registration of the pharmaceutical product and intellectual property rights
Once the new pharmaceutical product has been subjected to clinical trials, and has been
deemed fit for human (or in other cases animal) use, companies have to seek registration of
their pharmaceutical products with the relevant governmental authorities, as well as
authorization to market their new products. Concurrently, discussions will take place with
regard to the price of the product, as well as the extent to which a reimbursement will be
provided by governmental authorities to users of the product. In Belgium, the pricing decision
has to be taken by the Minister of Economy501, while the reimbursement decision is taken by
the Minister of Social Affairs, who is supported by the Riziv’s Commission on the
Reimbursement of Medicines (in Flemish: “Commissie Tegemoetkoming Geneesmiddelen” or
CTG)502. Prior to this process, however, companies will seek to obtain intellectual property
rights (IPRs) – both patents and trademarks (the name of a product is of great importance) –
with regard to their new products.
During this registration phase, two WHO frameworks are central to the naming of the
pharmaceutical products and their active (chemical) substances, namely the International Non-
proprietary Names (INN) Programme and the Anatomical Therapeutic Chemical (ATC)
classification system. Both frameworks provide for standardized names in order for
comparability of different pharmaceuticals (or pharmaceutical substances) so everyone
involved can adopt a common language. The wide recognition of both frameworks is evidenced
by article 13.2 of the Medicines Regulation, which requires mention of the INN(s) and the
ATC(s) in the Official Journal of the European Union of any drug authorized to be marketed in
the EU.
The INN system has been set up by WHO in 1950. It provides for generic names for drugs –
INNs, which are non-proprietary and in the public domain. The goal of this system is to provide
a common language for doctors, pharmacists, and even researchers with regard to
pharmaceutical products. Although some states have set up their own nomenclature bodies,
the WHO still retains the sole authority to determine INNs for pharmaceutical products.503
Depending on the national situation, a pharmaceutical company or a national nomenclature
body forwards the request for a certain INN to the WHO. Thereafter, the INN expert group
seeks an agreement on an acceptable INN, which is first published as a proposed INN.
Stakeholders then get four months to contest this new INN, which might, for example, conflict
‘Reporting the Findings of Clinical Trials: A Discussion Paper’ (2008) 86 World Health Organization. Bulletin of the World Health Organization 492. 500 Roderik F Viergever, Robert F Terry and Ghassan Karam, ‘Use of Data from Registered Clinical Trials to Identify Gaps in Health Research and Development’ (2013) 91 World Health Organization. Bulletin of the World Health Organization 416. 501 FOD Economie, KMO, Middenstand en Energie, ‘Geneesmiddelen voor menselijk gebruik’, http://economie.fgov.be/nl/consument/Gereguleerde_prijzen/Geneesmiddelen/. 502 Riziv, ‘Commissie Tegemoetkoming Geneesmiddelen’, http://www.riziv.fgov.be/nl/riziv/organen/Paginas/commissie-tegemoetkoming-geneesmiddelen.aspx#.VpOE6VnZaDc. 503 WHO, ‘Selection Process of INNs’, http://www.who.int/medicines/services/inn/selection/en/.

75
with their trademarks or trade names. After this four-month period, the INN is published again
as a “recommended INN.”504
Not only are existing trademarks or trade names protected from confusion with new INNs,
pharmaceutical companies are also prohibited from claiming any trademarks or trade names
which might cause confusion with INNs. In this respect, the WHO has made several
recommendations.505 In its new guidelines, which entered into force on 1 January 2015,506 the
EMA recommends to take WHA46.19 into consideration when applying for a trademark or
naming a pharmaceutical product.507 In the European naming procedure for pharmaceutical
products, which is led by the Name Review Group of the EMA,508 “representatives from the
European Commission (EC) and the World Health Organization (WHO) and relevant experts
selected from the European experts list may participate in the group's activities and [are]
consulted on a case by case basis regarding naming issues.”509 This demonstrates the central
role the WHO plays in the naming of pharmaceutical products as well as the determination of
generic names.
Finally, there have recently been calls for adding INNs to patent applications by pharmaceutical
companies as this might facilitate searching pharmaceutical patent databases for non-
specialized actors, as well as a better understanding of the data contained in such databases.
This possibility was recently examined by Secretariat of the World Intellectual Property
Organization (WIPO), in cooperation with the World Trade Organization (WTO) and WHO.510
Next in line, the ATC system provides every active chemical substance with a separate code,
in accordance with its anatomical, therapeutic and chemical characteristics. The substance is
defined on five levels, with each level being more specific. The main objective of the ATC
system is to facilitate international comparative drug research.511 As such, it can serve private
actors which intend to do research with regard to drug use. However, it can also serve
governmental services when they wish to make comparisons. The Canadian health authorities,
for example, make use of the ATC classification system to compare their drug prices with those
of other countries and adapt them accordingly.512 A similar classification system, devised by
the European Pharmaceutical Market Research Alliance (EphMRA), is used by the European
Commission in cases of competition law in the pharmaceutical sector (e.g. when determining
whether mergers are acceptable).513 Notably, and despite some differences in set up of the
504 Ibid. 505 WHO, ‘Guidance on INN’, http://www.who.int/medicines/services/inn/innquidance/en/. 506 BioPharm International, ‘EMA Changes Guideline on Drug Name Acceptability’ (4 June 2014), http://www.biopharminternational.com/ema-changes-guideline-drug-name-acceptability. 507 EMA, ‘Guideline on the acceptability of names for human medicinal products processed through the centralised procedure’ (adopted on 22 May 2014), EMA/CHMP/287710/2014 – Rev. 6, available at http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2014/06/WC500167844.pdf. 508 Ibid., 17. See also EMA, ‘Mandate, objectives and rules of procedure for the Name Review Group (NRG)’ (adopted on 1 July 2014), EMA/411943/2014, available at http://www.ema.europa.eu/docs/en_GB/document_library/Other/2014/07/WC500169642.pdf 509 EMA (no 496), 11. 510 WIPO, ‘Feasibility Study on the Disclosure of International Non-Proprietary Names (INN) in Patent Applications and/or Patents’ (23 September 2014), WIPO Docs. SCP/21/9, available at http://www.wipo.int/edocs/mdocs/scp/en/scp_21/scp_21_9.pdf. 511 See WHO, ‘Classifications - The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD)’, http://www.who.int/classifications/atcddd/en/. 512 See Patented Medicines Prices Review Board, ‘Compendium of Policies, Guidelines and Procedures’ (last updated June 2015), available at http://www.pmprb-cepmb.gc.ca/view.asp?ccid=492#1636. 513 See EphMRA, ‘EphMRA Classifications (ATC and NFC)’, http://www.ephmra.org/Classification. See also Sean Greenaway and others, ‘Recent Commission Merger Control Decisions in the Pharmaceutical Sector: Sanofi-Aventis/Zentiva and Teva/Barr’ Competition Policy Newsletter 64.

76
classification system,514 EphMRA and WHO have been attempting to harmonize their ATC
classification systems.515 Therefore, the WHO’s ATC classification system might indirectly
European competition law rulings.
In addition, when a pharmaceutical company invents a new active chemical substance,
acquiring an ATC might greatly help in obtaining a patent, as it demonstrates the novelty of the
drug, or at least the active substance, in question. However, in this regard, two elements should
be kept in mind. Firstly, pharmaceutical companies will probably apply for a patent, before
trying to obtain a new ATC classification so as not to risk missing the chance to obtain a patent.
Secondly, a pharmaceutical product does not require a new ATC per se to be considered
novel. A new combination of different active chemical substances, which already have ATCs,
could equally be the basis for a patent. In a similar fashion, pharmaceutical companies could
attempt to find a new ATC classification for their existing pharmaceutical products in their
attempt to “evergreen” the product.516 This trending concept of “evergreening” refers to
attempts by pharmaceutical industries to increase the lifespan of their mature branded drugs’
economic rentability, e.g. through obtaining new patents and thusly increasing the length of
their monopoly.517
With regard to registration and marketing authorization, the main programmes of the WHO
concern the moving of pharmaceutical products in international commerce. These rules will be
discussed below, as we consider them to mainly concern export, and thus the next phase.
Finally, with regard to the pricing and reimbursement of pharmaceutical products, the WHO
has also provided guidance.518 It even has a Collaborative Centre on Pharmaceutical Pricing
and Reimbursement Information (PPRI),519 and recently, a third conference in a series of
conferences on the topic has been organized by the European region.520
3.4.4 Manufacturing and distribution
Once a pharmaceutical products has been patented and accorded marketing authorization, it
will be manufactured on a large scale and distributed, which includes instances of export. After
distribution, there remains a certain follow-up, in order to detect any possible safety risks (e.g.
by-effects) which might have been overlooked during the first three clinical trial phases; the
distribution amongst a larger population might uncover some rare instances which could not
514 The WHO’s system is substance-based as it aims to allow for comparative research of drug use, and the EphMRA is product-based as it aims to provide market segments. See EphMRA, ‘Comparison of the WHO ATC Classification & EphMRA/PBIRG Anatomical Classification: Version January 2013’, available at http://www.ephmra.org/user_uploads/who-atc%202013%20final.pdf, 3. 515 Ibid. 516 Kate S Gaudry, ‘Evergreening: A Common Practice to Protect New Drugs’ (2011) 29 Nature Biotechnology 876. 517 See Marcus Healey and Krithika Venkataraman, ‘Drug Evergreening: Does Economic Value Outweigh Therapeutic Value?’ (Prescient Healthcare Group 2015) Working Paper 2. 518 WHO, ‘WHO Guideline on Country Pharmaceutical Pricing Policies’ (2015), available at http://apps.who.int/iris/bitstream/10665/153920/1/9789241549035_eng.pdf?ua=1. 519 Gesundheit Österreich GmbH, ‘PPRI: Pharmaceutical Pricing and Reimbursement Information’, http://whocc.goeg.at/About/PPRI. 520 See WHO/Europe, ‘Third International Pharmaceutical Pricing and Reimbursement Information (PPRI) Conference’, http://www.euro.who.int/en/health-topics/Health-systems/medicines/news/news/2015/11/third-international-pharmaceutical-pricing-and-reimbursement-information-ppri-conference

77
have been detected in the first three phases. This process of ex-post monitoring of
pharmaceutical products is known as pharmacovigilance.
First of all, since 1977, the WHO has developed a Model List of Essential Medicines, defending
the point that some medicines are more essential than others.521 The objective of making such
a list was to help governments make decisions when steering or coordinating pharmaceutical
production.522 However, the pharmaceutical industry cracked down on this initiative as it
considered this technique of essential medicines lists to hamper market mechanisms, and at
best only be useful for the poorest countries.523 Nevertheless, the WHO has continued this
initiative, and pleaded for more investment in the production of these essential medicines.524
At the same time, the WHO/Europe has been cooperating with social institutes of both Austria
and Belgium in order to facilitate the introduction and accessibility of high-priced medicines
into the European market, which represents the other kind of the spectrum.525
In the framework of the manufacturing process, the WHO has developed good manufacturing
practices (GMP) guidelines, which are meant to ensure the quality of the output of the
manufacturing process both in terms of safety as in terms of efficacy.526 These guidelines,
which are developed by the WHO Expert Committee on Specifications for Pharmaceutical
Preparations527, are widely recognized. The EMA, for example, explicitly states on its website
that ‘[a]lthough EU and WHO GMP guidance documents do differ in some details, the main
principles remain the same. EU requirements fulfil all the recommendations of WHO.’528 In
addition, certain private certification schemes require producers to at least have knowledge of
the WHO GMP guidance documents.529 As such, the WHO’s recommendations indirectly affect
Belgian and Flemish regulation, although the concrete impact is difficult to discern as the WHO
recommendations are filtered by the European level. In addition, the WHO has developed
guidelines on good distribution practices (GDP).530 These guidelines are referred to in the
certification scheme developed by the International Air Transport Association, which
521 WHO, ‘WHO Model Lists of Essential Medicines’, http://www.who.int/medicines/publications/essentialmedicines/en/. 522 In this regard, a 2013 WHO report on Priority Medicines for Europe and the World which serves as a basis for EU decisions on Horizon 2020 research investments is undoubtedly equally relevant. The report is available online at http://www.who.int/medicines/areas/priority_medicines/en/. 523 Richard Laing and others, ‘25 Years of the WHO Essential Medicines Lists: Progress and Challenges’ (2003) 361 The Lancet 1723. 524 In this regard, this initiative resembles the WHO’s efforts to secure more investment in research towards type II and type III diseases, as it also combats the pharmaceutical industry’s focus on profitable diseases, albeit here with regard to production. 525 WHO/Europe, ‘WHO/Europe partners with Austria and Belgium to address new, high-priced medicines in Europe’, http://www.euro.who.int/en/health-topics/Health-systems/medicines/news/news/2015/10/whoeurope-partners-with-austria-and-belgium-to-address-new,-high-priced-medicines-in-europe. 526 A list of WHO GMP guidelines can be found at http://www.who.int/medicines/areas/quality_safety/quality_assurance/production/en/. 527 See WHO, ‘WHO Expert Committee on Specifications for Pharmaceutical Preparations: How Does It Work?’ (2013), available at http://www.who.int/medicines/services/expertcommittees/pharmprep/WHO_ECSPP_2014.pdf. 528 See EMA, ‘Questions and Answers: Good Manufacturing Practices’, available at http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/q_and_a/q_and_a_detail_000027.jsp (Question answered July 2006). 529 “This certification procedure also requires participants to be informed of WHO guidelines in the field of GMP.” See http://asq.org/cert/resource/pdf/certification/inserts/CPGP%20Insert%202013%20.pdf 530 WHO, ‘WHO good distribution practices for pharmaceutical products’ (2010) WHO Technical Report Series, No. 957, available at http://www.who.int/medicines/areas/quality_safety/quality_assurance/GoodDistributionPracticesTRS957Annex5.pdf.

78
represents the global airline industry.531 This scheme requires compliance with the WHO GDP
in order for certification to be obtained, and has been endorsed by both Belgian and EU
regulators.532
In the distribution phase, the WHO is mainly concerned with the quality of pharmaceutical
products moving in international commerce. Central to its quality assessment framework in this
field, are its certification scheme on the quality of pharmaceutical products moving in
international market,533 as well as the prequalification programme, which is intended to ensure
the quality of products used by UN agencies.534 The WHO GMP guidelines are an integral part
of this scheme.535 For pharmaceutical products produced in the EU but intended exclusively
for markets outside of the EU, the EMA must consult with the WHO before granting an
authorization.536 Indeed, “Article 58 of Regulation (EC) No 726/2004 allows the Agency's
Committee for Medicinal Products for Human Use (CHMP) to give opinions, in co-operation
with the World Health Organization (WHO), on medicinal products for human use that are
intended exclusively for markets outside of the European Union (EU).”537 Furthermore, article
127 of the Medicines Directive requires Member States to “have regard to the prevailing
administrative arrangements of the World Health Organization” when issuing certificates to
manufacturers, exporters or the authorities of an importing third country that the manufacturer
has obtained a manufacturing authorization. Indeed, the WHO has both established
substantive and administrative guidelines and regulations for pharmaceutical products moving
in international commerce.
Finally, the WHO operates (at least) two programmes which concern the safety of
pharmaceutical products moving in international commerce, after the first authorization
phases. Firstly, the WHO intervenes in the global pharmaceutical market in order to combat
the spread of ‘substandard, spurious, falsely labelled, falsified and/or counterfeit’ (SSFFC)
pharmaceutical products.538 In this fight, it has established a partnership with the EU539, which
has itself driven up the fight against fake pharmaceuticals since 2008,540 and which refers in
its Directive 2011/62/EU on fake pharmaceuticals to WHO’s initiatives in this area.541 Next,
531 IATA, ‘CEIV Pharma – Putting pharmaceuticals back in the air’, http://www.iata.org/whatwedo/cargo/pharma/Pages/ceiv-pharma.aspx. 532 See IATA, ‘How to become CEIV Pharma certified’, available at http://www.iata.org/whatwedo/cargo/pharma/Documents/ceiv-pharma-specifications.pdf 533 See WHO, ‘Essential medicines and health products - Certification scheme on the quality of pharmaceutical products moving in international commerce’, http://www.who.int/medicines/areas/quality_safety/regulation_legislation/certification/en/. 534 See WHO, ‘Prequalification programme – A United Nations Programme managed by WHO’, http://apps.who.int/prequal/ 535 Jaya Bir Karmacharya, Good Manufacturing Practices (GMP) for Medicinal Products (2014) <http://library.umac.mo/ebooks/b28113378.pdf#page=111> accessed 21 December 2015. 536 Article 58 Pharmaceuticals Regulation. 537 EMA, ‘Article 58 applications: Regulatory and procedural guidance’, http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/document_listing/document_listing_000157.jsp&mid=WC0b01ac05800240d1 538 ‘WHO Project for the Surveillance and Monitoring of SSFFC Medical Products’ (2013) 27 WHO Drug Information 97. See also ‘Substandard/spurious/falsely-labelled/falsified/counterfeit medical products’ (Report by the Director-General, 3 January 2014) WHO Docs. EB134/25, available at http://apps.who.int/gb/ebwha/pdf_files/EB134/B134_25-en.pdf. 539 WHO, ‘EU/ACP/WHO Renewed partnership: tackling dangerous pharmaceuticals’, http://who.int/medicines/areas/coordination/dangerous_pharm/en/. 540 European Commission, ‘Safe, innovative and accessible medicines: a renewed vision for the pharmaceutical sector’ (10 December 2008), http://ec.europa.eu/health/human-use/package_en.htm. 541 Directive 2011/62/EU of the European Parliament and of the Council of 8 June 2011 amending Directive 2001/83/EC on the Community code relating to medicinal products for human use, as regards

79
WHO acts as an important coordinator when it comes to pharmacovigilance. The main
coordinating centre for the WHO in this issues is the Uppsala Monitoring Centre, which
monitors post-distribution adverse effects of pharmaceutical products.542 In recognition of this
role, article 28c of the Medicines Regulation requires the EMA to “collaborate with the [WHO]
in matters of pharmacovigilance and [to] take the necessary steps to submit to it, promptly,
appropriate and adequate information regarding the measures taken in the Union which may
have a bearing on public health protection in third countries.”
the prevention of the entry into the legal supply chain of falsified medicinal product, OJ L174/74, consideration (4). 542 UMC, ‘The WHO Programme’, http://www.who-umc.org/.

80
4. The impact of the WHO in Flanders
In this conclusory chapter, we will discuss the two sides of the impact story: the impacting and
the impacted side, or in other words, the rule-makers and the rule-takers. We will look at some
of the specific characteristics of the WHO as a rule-maker, but will also discuss how the WHO
is more and more engaged in a rule-making network. Indeed, WHO has seized to be the only
relevant global health actor for some time. By expanding on the rule-makers, we hope to give
Flemish policy-makers an insight in the processes of non-traditional law-making at work here.
As a consequence, they should be better equipped to weigh in on this processes. At the same
time, we will also discuss how the rules developed by the WHO and its network make it to the
Flemish level. We will focus on the variety and complexity of ways in which this happens.
Particular attention will be paid to the role of the EU, which is difficultly categorized as either a
rule-taker or rule-maker as it fits both descriptions543, in several fields of global health
governance.
4.1 Rule-maker
4.1.1 The WHO’s choice for soft law
The most obvious observation to be made about the WHO’s exercise of its normative function
is its reliance on non-binding instruments over binding instruments. Although the WHO has a
strong mandate to develop legally binding agreements and regulations in articles 19-22 of its
Constitution, it has generally opted not to make use of this ability. It has adopted only one
Convention, the FCTC, in addition to two regulations, the IHR and the Nomenclature
Regulations. Proposals for new conventions have continued to be made, but resistance
remains strong, both within the WHO Secretariat, and among Member States.
Not only have few binding instruments been adopted, most of these instruments have
moreover been implemented or specified through non-binding instruments. This has been,
most notably, the case for the FCTC, which is, as the name suggests, a framework convention.
Under normal circumstances, such a convention would be further developed through the
adoption of (binding) protocols. However, the WHO has not had much success in developing
such protocols, as only one protocol has yet been adopted, which currently only has a limited
amount of ratifications.544 Instead, the FCTC has been further implemented through non-
binding guidelines, mainly in the framework of the MPOWER-project. The Nomenclature
Regulations have encountered a similar fate, as they have been further developed through the
ICD and its associated classification families.
In contrast with these two instruments, strong and specific obligations flow from the IHR, but
these obligations lack strong enforcement mechanisms, as has become painfully clear during
the Ebola crisis. Not only have states parties to the IHR in general insufficiently developed
national capacities to surveil and handle cases falling under these regulations, the WHO has
543 Neither does it fit the bill of the newly introduced concept of ‘rule-intermediary’ nicely. See David Levi-Faur and Shana M Starobin, ‘Transnational Politics and Policy: From Two-Way to Three-Way Interactions’ (The Hebrew University of Jerusalem 2014) Working Paper 62 <http://din-online.info/pdf/jf2.pdf> accessed 13 January 2016. 544 Note that several states have ratified the protocol rather recently, and that ratifications keep occurring so that the protocol might still become an effective and important instrument.

81
encountered great difficulties in convincing non-affected countries to abide by the temporary
recommendations they had adopted. Indeed, the WHO’s consensual and non-conflictual
approach to decision-making “has resulted that both the [IHR] and the FCTC, the two legally
binding WHO agreements, do not include dispute settlements.”545 Recent proposals to reform
WHO emergency response programmes thus logically target inter alia the WHO’s capacity to
enforce the IHR.
Despite this lack of binding instruments, it would be wrong to claim that the WHO has
(completely) failed in the exercise of its normative functions. To the contrary, the WHO has
been quite successful and prolific in the development of non-binding guidelines and
recommendations. Indeed, as several authors have noted, this has been one of its most
successful activities. The development of these guidelines and recommendations happens at
different levels and in a variety of ways. The WHO has adopted Global Strategies and
developed these into more concrete action plans, both at the global and at the regional level.546
This is, for example, the case for the WHO Global Strategy on Diet, Physical Activity and Health
(see section 3.2). These Global Strategies lead to, and are supported by, more specific
guidelines, such as the Sugar Guideline. Sometimes, such guidelines do not form part of a
greater Global Strategy, but simply provide an overview of the state-of-the-art of the research
and policy recommendations based thereon. These guidelines can be endorsed by the WHA,
in which case they become “recommendations” in the sense of article 23 WHO Constitution.
However, even without such formal endorsement – which is indeed rarely given, these
guidelines or other documents can often be impactful. How these instruments can then be
impactful will be further discussed in section 4.2.2.
4.1.2 WHO as an expert organization
The impact of the WHO’s soft norms depends to a large extent on the WHO’s reputation as an
expert organization. Indeed, despite the great variety in types of instruments, there seems to
be one constant which is the involvement of experts, often in a leading role. It is this expertise
which grants WHO the legitimacy necessary to play an influential role in global health
governance, and which ensures the implementation of its instruments, even more so than with
most other international organizations.
Consequently, when several scholars challenged the WHO guidelines’ scientific soundness in
2008, the WHO has reacted swiftly and decisively. It did so through the establishment of a
Guideline Review Committee, which prepared a Guideline Development Handbook (see
section 3.1.2). Through this Committee and this Handbook, the guideline development
procedure of the WHO has become much more formalized and institutionalized, as well as
clearly evidence-based. These evolutions have remained largely overlooked and under-
debated outside of the circles of medical experts. Still, in time, they might prove quite influential.
Indeed, as the Guideline Review Committee carries the final responsibility for the scientific
soundness of the WHO’s guidelines, it will most likely only increase in importance over the
coming years. Moreover, the streamlining of the guideline development procedure might lead
to more clarity, transparency and accessibility with regard to this process, which cannot but be
applauded.
545 van de Pas and van Schaik (n 43) 197. 546 See this interview for an example of how such global strategies can be implemented. Boytsov (n 388).

82
As such, the Guideline Review Committee should be a body of interest to Flemish policy-
makers. Staying informed about further developments in the guideline development procedure
should allow the Flemish government and parliament to engage more actively with the
guideline development processes.547 Moreover, to ensure engagement with these processes,
the government should interact regularly with the Flemish scientific community548, which could
lead to a reinforced role for both partners in WHO guideline development. At least, it would
allow Flanders to follow the development of guidelines more closely.
In addition to corroborating its reputation as an evidence-based norm-setter, the WHO has
been increasingly realizing that expertise alone will not suffice to protect its claim to legitimacy.
More and more, it has started involving stakeholders in the different steps of the exercise of its
normative function. Partly, such reforms are inspired by the critique that the WHO is overly
dominated by the medical community.549 This is, for instance, the case in the development of
the new version of the ICD, ICD-11, which has taken a long time, exactly because so many
stakeholders have been involved. Similarly, the Guideline Development Handbook requires
the consultation of relevant stakeholders whenever a guideline is developed. Nevertheless,
debate persists with regard to the involvement of private actors in the WHO’s work, which
remains one of the hot topics of the WHO current reform programme.
With regard to this final point, there are two relevant remarks for Flanders. Firstly, if the Flemish
government would prefer that Flemish civil society organizations (and other non-state actors)
participate whenever consultation rounds are organized or feedback from private actors is
requested by WHO, it can contribute thereto by disseminating information on ongoing
consultative processes within the WHO and by promoting active contribution.550 A joint Flemish
contribution, based on internal debate between Flemish state and non-state actors, could even
be considered in important cases. Secondly, Flanders should reflect, within the context of its
external multilateral policies, what role it sees for private actors in global governance. These
reflections could feed into the Belgian and European negotiating mandate for the reform of the
non-state actor framework of the WHO.
4.1.3 The WHO’s multiple roles
Thanks to its recognition as an expert organization, the WHO is most famous for its technical
leadership. On the basis of sound scientific evidence, it provides global standards in its
guidelines, which national or regional standards are expected, although rarely legally required,
547 The Guideline Review Committee is, however, not responsible for the content of the guidelines, which remains the responsibility of the separate expert committees. Still, the GRC acts as a gatekeeper. As such, a lot of information at least passes through this committee. 548 This could happen, for example, through interaction with the Flemish WHO Collaborating Centres. Currently, there are 6 such institutes in Flanders, three of which are based at Ghent University (WHO Collaborating Centres for Research on Sexual and Reproductive Health, for the monitoring of anthelminthic drug efficacy for soil-transmitted helminthiasis, and on Primary Health Care), two of which are based at the Institute of Tropical Medicine in Antwerp (WHO Collaborating Centres for HIV/AIDS Diagnostics and Laboratory Support and for Research and Training on human African trypanosomiasis diagnostics), and the final one being based at the University of Antwerp (the WHO Collaborating Centre for the Prevention and Control of Infectious Diseases). 549 Kelley Lee even dubbed the WHO Secretariat ‘the medical mafia’. See Kamradt-Scott (n 253) 76. referring to Kelley Lee’s Historical Dictionary of the World Health Organization. 550 Sometimes non-state actors might even be better informed about ongoing consultative processes within WHO. In these cases, the information might cycle back towards the Flemish government rather than the other way around. A strong partnership with civil society, at least with regard to information-sharing, could thus be highly beneficial for both state and non-state parties.

83
to conform to.551 This is, for example, the case for the GMP and GDP guidelines (see section
3.4.4), which have found their way into European guidelines and even private certification
systems. Because of the WHO’s technical expertise, their technical guidelines are often taken
as a basis for standards in the field of public health.
However, the WHO has not limited itself to a strictly technical role. To the contrary, through its
rights-based approach which is codified in the preamble of its Constitution, the WHO has been
trying to steer global health research in order to make up for the skewed priorities stemming
from the market incentives system. For some years, it has been trying to increase the amount
of R&D spending towards type II and type III diseases which have historically largely been
neglected. In this light, the WHO shows itself as a normative actor. Through the GSPA-PHI
and the Model List of Essential Medicines, for example, it tries to promote certain policies, not
because these policies are scientifically more sound per se, but rather because they might
contribute to a more equitable world order. As the main global health actor, it tries to convince
developed states that terms like ‘global health’ should indicate more engagement towards
developing states. As such, it has become a pivotal player in the development discourse.
Indeed, Flanders has already collaborated on several occasions with the WHO in the field of
development through the financing of certain programmes.552
Still, it is a common misconception that the WHO is only relevant for developing countries.
Although developed countries often have already attained the global standard set out in WHO
guidelines, this is not always the case. Think, for example, of the Sugar Guidelines. Indeed,
the entire combat against NCDs has reaffirmed the importance of the WHO for developed
countries also. Moreover, as it often manages to attract the best experts in different fields, the
WHO can still manage to provide technical guidance of a quality which (developed) states
acting alone could not (or at least not on such a wide array of topics as WHO). In other words,
it would be wrong for Flemish policy-makers (or even private actors) to disregard WHO
guidelines as irrelevant, as it also produces relevant guidance for Flemish policies, such as its
policies on nutrition and physical activity.553 In these cases, dissemination of the scientific
knowledge provided in these guidelines might be a task for the Flemish government.
Another function which the WHO fulfills at times, is that of counterweight to industrial
interests.554 Indeed, some industries have become so multinational that single states or even
regional groups might have little control over them. In these cases, refuge is sometimes sought
with the WHO, since it is still able to counter industry tactics when it places its full weight behind
a certain issue. The most evident example of this would be the FCTC, where the WHO has
explicitly been attempting to counter industry tactics. However, one could also think of the
attitude the WHO sometimes takes vis-à-vis the pharmaceutical industry, where it tries to
promote a more equitable division of attention among different diseases. Think, for example,
of the GSPA-PHI or the Model List of Essential Medicines. Nevertheless, the WHO’s
551 We have noted above that close engagement with the Flemish scientific community should allow the Flemish government to engage more actively with the WHO when it is developing more technical guidelines. This engagement might even consist of critical reflection ex post on the practical usefulness of the WHO’s technical guidelines. 552 See section 1.2.1. 553 Think, for example, also of the WHO’s guidance on social determinants for health. See footnote 11. 554 Burci has identified the regulation of the food, tobacco and beverage industries, which have strongly resisted such regulation, as one of the major challenges for global health in the coming decades. As was the case with the tobacco industry, the WHO will be quintessential to provide a counterweight to these anti-regulation interests. Gian Luca Burci, ‘The Next One Hundred Years of Global Health’ (2015) 39 Fletcher F. World Aff. 87, 88.

84
relationship with the pharmaceutical industry is more ambiguous as the pharmaceutical
industry sometimes also serves the WHO’s goals of enhancing global health.
Finally, we would also like to make mention of the administrative function the WHO sometimes
fulfills. One example thereof can be found in the administrative arrangements it has designed
for the movement of pharmaceutical products in international commerce. Another example
would be the generalized naming systems and classification systems it maintains, such as the
Nomenclature Regulations, and its implementing norms, and the INN and ATC system. At the
same time, we have also discussed the WHO playing a more active role on another occasion.
During the Ebola crisis, the WHO has attempted to speed up the clinical trials process for
promising pharmaceutical products (both medicines and vaccines) to combat Ebola. As it has
generally proven difficult in the past to sufficiently test Ebola vaccines and medicines for lack
of sufficient human test subjects for clinical trials, the (almost) past Ebola crisis provided a
critical change for some extensive tests. Consequently, the WHO lobbied to ensure an
accelerated procedure for these clinical trials, in the hope a vaccine or medicine might be
developed. As it does not control the authorization procedures itself, here, it acted more as a
coordinator and facilitator.
4.1.4 The global health network
Despite all the previous discussions about the WHO, one of the most important things to note
is that, although the WHO is generally mentioned as the most important actor in the field of
global health governance, it is by no means the only one. Indeed, around and besides the
WHO, an entire network of global health governance has developed with different actors
exercising different, and sometimes even overlapping, competences.555 These new actors
have increasingly challenged the WHO’s centrality.556 In addition, actors from other domains
have also been encroaching on the field of global health governance, to the extent that Burci
has stated that “[t]he main policy challenges for the century ahead will center on how to
preserve the distinctiveness of global health as its own critical policy matter-without being
subsumed under different policy agendas such as security-while also securing its prominent
role in the world as an effective balance for other interests and policy issues.”557
A sketch of the whole field of global health governance and its different networks is outside of
the scope of this paper, but some examples can still be drawn from what has been described
above.558 Firstly, in the field of health emergencies, we have noted the existence of several
555 The WHO has acknowledged this itself in its draft framework for engagement with non-state actors. See ‘[Draft] Framework of engagement with non-state actor’ (Appendix to WHA resolution, 26 May 2015), WHO Docs. WHA68.9, available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R9-en.pdf?ua=1, para 2: “The global health landscape has become more complex in many respects; among other things, there has been an increase in the number of players including non-State actors. WHO engages with non-State actors in view of their significant role in global health for the advancement and promotion of public health and to encourage non-State actors to use their own activities to protect and promote public health.” An interesting schematic overview of some of the new actors is provided at page 13 of Charles Clift’s report on the role of the WHO in the international system. See Clift (n 141) 13. 556 Burci (n 554) 89. 557 ibid 88. 558 Additionally, we would like to note that individuals may greatly affect the outcomes of certain projects. Indeed, the success of the FCTC largely depended on the continued engagement by Taylor and Roemer, as well as the support by Brundtland. Additionally, the WHO’s campaign with regard to hygiene and health has been largely inspired by the work of Pittet. This was confirmed during our interview at Gasthuisberg. See also Kamradt-Scott (n 253).

85
relevant actors besides the WHO at the end of section 2.3.1. The WHO is, for example, not an
operational international organization, and thus relies heavily on other organizations, both
governmental and non-governmental, to provide “boots on the ground.” Here, we can refer to
the importance of Médicins Sans Frontières. However, we can also refer to the Centers for
Disease Control, whose mandate seems to overlap (partly) with that of the WHO. Secondly, in
the field of pharmaceutical products, we can refer to the ICH, which has been developing
standards for clinical trials, an activity which falls squarely within the WHO’s mandate. Although
the WHO has been closely involved in the ICH, it has not occupied a leading role here. In
addition, there are several private certification schemes, which have gained importance in the
pharmaceutical sector, as they have in other sectors. These certification schemes often refer
to the WHO’s guidelines.559 In the field of nutrition, finally, the WHO has often had to share the
leadership role with the FAO, for instance, when they jointly established the Codex
Alimentarius Commission.560 It would benefit the Flemish government to maintain an overview
of the evolving global health governance network. Indeed, it could help in discerning which are
the most appropriate organizations to complete certain tasks (which might inform decisions on
which organizations to fund).
At the European level, the EU has of course created quite a large gravitational pull for regional
networks, even with regard to public health. Indeed, the EU has been involved in nearly every
initiative at the regional level in this field, and has closely collaborated with the WHO (both at
the HQ and at the regional level). It established (independent) agencies, such as the ECDC
and EMA, and developed regulatory initiatives translating global standards, which are often
non-binding, into binding EU law documents. With regard to the FCTC, for example, the
European Commission is deemed to translate guidelines developed in the framework of this
convention, into EU instruments, which are generally binding on the member states. Another
example can even be found in the area of “diet, physical activity, and health”, in which the
European Commission has also collaborated with WHO/Europe. Given this prominent role of
the EU, active engagement in the European health policy debate might well serve a twofold
purpose. On the one hand, the EU can help translate Flemish (or Belgian) concerns to the
international level. On the other hand, the EU provides a filter for relevant guidelines, which
can help maintain an overview of relevant actors and guidelines coming from the international
level. As such, we would argue that any Flemish external multilateral policy requires a strong
European component, not only because of the European level an sich, but also because of the
recognition the EU enjoys globally.
Finally, in the light of this argument, it is relevant to shortly refer again to the current reform the
WHO is undergoing. Undoubtedly, the continued perception of the WHO as the leading
organization in global health governance, at the centre of the network, will depend highly on
its continued capacity to act as such. This, in turn, will depend on the success of the reform.
Not only should the reform lead to greater financial stability, it should also help restore the
reputation WHO has been losing over the last years through, for example, tardy and
inadequate responses to global health emergencies (think of the Ebola crisis), but also, for
example, in 2008, when its guideline development system was criticized for being insufficiently
evidence-based. Essentially, the reform should allow the WHO to act as the coordinating and
leading authority it was meant to be.
559 One example can be found in the IATA guidelines on the aerial transport of pharmaceuticals which have been discussed in section 3.4.4. 560 We have not yet mentioned this Commission in this report, but it featured in our earlier report as one of six case studies. See Vanstappen and others (n 4).

86
4.2 The multi-layered and complex nature of the rule-taker
4.2.1 Implementation in a multi-layered and complex context
If the rule-maker side of the implementation matrix could be considered complex, this is
certainly no less true for the rule-taker side. Admittedly, as was evident from our attempts to
define the rule-taker side, “Flanders”, in our introduction, we were already aware of this
complexity at the outset of this report. Nevertheless, the report confirmed and reinforced our
assumptions in this regard.
The complexity of the Flemish context flows from different elements. Firstly, there is the
national, federal context. In a national context with a high degree of autonomy for several
subnational entities, defining homogenous competence packages, one of the goals of the past
state reforms, is certainly not evident.561 Belgian federalism further corroborates these
difficulties by distinguishing between Communities and Regions, with competences (material
and territorial) which may overlap. Because of the federal context, different entities are often
responsible for the implementation of certain norms. In the context of the FCTC, for example,
the Flemish Community and the Belgian federal government share the responsibility of
implementation. The coordination this requires, is not always simple, as was noted in
discussing the Belgian score in the IHR implementation report (see section 2.3.4.1).
The European context further compounds the situation. As we noted already in section 1.2.1,
the WHO often cooperates directly with the EU, rather than with its member states, which may
result in legal obligations for these member states. As such, as we mentioned above, the EU
has become more of a go-between between the national and the global level, often directly
affecting the norms adopted at the global level, or adapting to the European regional context.
We have encountered this role for the EU especially in our section on the FCTC and on
pharmaceutical companies. Indeed, the EU’s position is not neatly captured by the distinction
between rule-makers and rule-takers.
4.2.2 Different ways and levels of impact
A second note with regard to the rule-taker side of the discussion is the divergent levels of
impact the WHO’s different norms have in Flanders, and the different ways they can have
impact. As we have noted in our earlier reports, and have noted again throughout this report,
there are several different methods for an organization as the WHO to have impact in Flanders.
In a limited number of cases, the WHO has developed binding norms itself. The main examples
in this regard are, of course, the single convention and the two regulations the WHO has
adopted in the course of its 70-year existence. However, in addition, the WHO’s non-binding
norms can equally become binding in the course of the implementation process. In this context,
it is important to refer again to the judgment by the Constitutional Court, which confirmed that
the (non-binding) guidelines which implement the FCTC, are equally to be considered when
implementing the FCTC, and these could be fall under the protection article 23 of the Belgian
Constitution offers. Another important mechanism for norms to become binding is through the
561 Ruth Boone, ‘“In een federale staat bestaan homogene bevoegdheidspakketten eigenlijk niet”’, interview with professor Jan Velaers (5 December 2013), available online at http://www.legalworld.be/legalworld/In-een-federale-staat-bestaan-homogene-bevoegdheidspakketten-eigenlijk-niet.html?LangType=2067.

87
transposition of these norms into EU legislation, which has occurred at regular intervals, for
example, with regard to pharmaceutical products, as well as with regard to the WHO guidelines
which have further implemented the FCTC.
In the absence of legal obligation, non-binding norms can still have an important impact. They
can inspire changes in policy, by either presenting new ideas, new research or by pointing out
existing deficiencies in health systems. Here, we would like to stress again that it is generally
difficult to discern which amount of impact the norm has had. Firstly, a WHO guideline can be
the direct inspiration for a change in policy, either because the WHO defends a normative claim
which the state supports, or because the WHO presents new research which might require a
change in existing policies, or for any other reason. In our research, we have encountered no
clear examples of such cases, although the rules on the registration of clinical trials might come
close. In addition, the WHO’s changing focus from traditional health topics to NCDs, social
determinants of health, a healthy environment, and the debate it has started with regard to
intellectual property rights in the pharmaceutical industry, might continue to trigger more of
these moments. Indeed, “in the wake of the global alert concerning NCDs, the WHO is
expected to take a more active role in regulating key issues baring an impact on health,
including alcohol beverages, food safety and nutrition.”562 Secondly, in the words of
Easterbrook in a recent interview, “WHO guidelines can often be a catalyst in driving a policy
change that a country is already contemplating.”563 Thirdly, policy-makers often fall back on
internationally accepted guidelines and norms when contemplating policy changes. In this
case, WHO guidelines will certainly be carefully read and analyzed if a policy change in the
field of public health is considered, and will thus affect the outcome of the policy change.
4.2.3 Impact on private actors directly
Although governments and policy-makers remain the WHO’s partner of choice in the
implementation of its guidelines, they are by no means the sole target public of its guidelines
or recommendations. Indeed, several recommendations are designed thusly that they can be
applied directly by private actors. This is, for example, the case for the Clean Care is Safer
Care programme, but equally for the GMP designed for pharmaceutical manufacturers. Even
guidelines aimed mainly at policy-makers, such as the Sugar Guidelines, might be picked up
by private actors. Indeed, dietary specialists may take over the recommendations put forward
in these guidelines, or, as we have seen, newspapers may base their web surveys on these
guidelines.
As we have noted in section 3.3, the WHO often goes through great efforts in making the
guidelines accessible for the target public it is intended for. It has translated its guidelines on
hand hygiene into a one-sheet infogram on My Five Moments of Hand Hygiene, a phrase which
now sounds familiar to many doctors. It has undertaken a similar effort in developing a Surgical
Safety Checklist. The spread of its guidelines to private actors is further simplified by the
attendance of several groups representing doctors, patients with certain diseases, the
pharmaceutical industry, etc. at WHO meetings. These groups are generally as well, if not
better, aware of the changes going on at the level of WHO, and can communicate these to the
people they represent. As such, these guidelines might more quickly reach private actors
through their representative bodies than through implementation or dissemination by
governments.
562 van de Pas and van Schaik (n 43) 198. 563 Shetty (n 311) 779.

88
Finally, certain guidelines might also indirectly reach private actors, for example, through
private certification schemes. In section 4.1.4, we have referred to IATA’s certification scheme
which requires compliance with WHO’s guidelines on GDP. This indirect route for guidelines
to reach private actors is, of course, reinforced by the growing number of relevant global health
actors. Indeed, most actors dealing with global health refer in some way or another to WHO’s
guidelines, since, as it stands, the WHO is still the main actor in global health, from which other
actors are not afraid to learn or borrow.

89
Annexes Annex I: Organigram of the WHO
Source: http://www.who.int/about/structure/who-organigram.pdf

90
Annex II: The core functions of the WHO
Source: http://who.int/country-cooperation/what-who-does/core-functions-big.jpg

91
Annex III: Dietary guideline development process
Source: http://www.who.int/elena/about/guidelines_process/en/

92
PARTNERS
NEDERLANDS
Het Leuven Centre for Global Governance Studies (www.globalgovernancestudies.eu) coördineert de derde generatie van het Steunpunt “Buitenlands beleid, internationaal
ondernemen en ontwikkelingssamenwerking” voor de Vlaamse Regering. Een
Steunpunt heeft als doel de wetenschappelijke ondersteuning van Vlaams beleid.
Het project brengt 17 promotoren en 10 junior onderzoekers (waarvan acht
doctoraatsstudenten) samen. Het Steunpunt doet aan (a) dataverzameling en -
analyse, (b) korte termijn beleidsondersteunend wetenschappelijk onderzoek, (c)
fundamenteel wetenschappelijk onderzoek en (d) wetenschappelijke dienstverlening.
We werken samen met een aantal partners: het Antwerp Centre for Institutions and
Multilevel Politics, de Vlerick Leuven Gent Management School en H.U.Brussel.
Binnen de KU Leuven maken ook collega’s verbonden aan de Faculteit Economie, het
Instituut voor Internationaal en Europees Beleid, de Onderzoekseenheid Internationaal
en Buitenlands Recht, het Instituut voor Internationaal Recht, het Instituut voor
Europees Recht en HIVA - Onderzoeksinstituut voor Arbeid en Samenleving deel uit
van het project.
Het onderzoek is verdeeld over vier thematische pijlers: (i) Internationaal en Europees
Recht; (ii) Internationaal en Europees Beleid; (iii) Internationaal Ondernemen; en (iv)
Ontwikkelingssamenwerking.
Bezoek onze website voor meer informatie: www.steunpuntiv.eu
ENGLISH
The Leuven Centre for Global Governance Studies coordinates a Policy Research
Centre on "Foreign Affairs, International Entrepreneurship and Development
Cooperation" for the Flemish Government. A Policy Support Centre aims to
scientifically support Flemish regional policies. The project brings together 17 senior
and 10 junior researchers (including eight PhD students).
The Centre conducts (a) data collection and analysis, and provides (b) short-term
policy supporting research, (c) fundamental scientific research and (d) scientific
services.
The Policy Research Centre is based on an inter-university consortium led by the
Leuven Centre for Global Governance Studies (www.globalgovernancestudies.eu) in
cooperation with the Antwerp Centre for Institutions and Multilevel Politics, the Vlerick
Leuven Gent Management School and the H.U.Brussel. Within the KU Leuven,
colleagues from the Faculty of Business and Economics, the HIVA - Research Institute
for Work and Society, the Institute for International and European Policy, the Research
Unit International and Foreign Law, the Institute for International Law, and the Institute
for European Law are also involved in the project.
Research is structured in four thematic pillars: (i) International and European Law; (ii)
International and European Policy; (iii) International Entrepreneurship; and (iv)
Development Cooperation.
For more information, see our website: www.steunpuntiv.eu