Renal physiology bpums
-
Upload
khalil-pourkhalili -
Category
Health & Medicine
-
view
118 -
download
1
Transcript of Renal physiology bpums

Renal physiology- Dr. Kh. Pourkhalili
1
Renal physiology
Presented by: Dr. Khalil Pourkhalili
Bushehr University of Medical Sciences(BPUMS)
Faculty of medicine
Bushehr University of Medical Sciences

Renal physiology- Dr. Kh. Pourkhalili
2
B.P.U.M.S
Regulation of water and electrolyte balance Excretion of metabolic waste Excretion of bioactive substances (Hormones and many
foreign substances, specifically drugs) Regulation of arterial blood pressure Regulation of red blood cell production Regulation of vitamin D production Gluconeogenesis Acid-base balance
Renal functions

Renal physiology- Dr. Kh. Pourkhalili
3
B.P.U.M.S
Position: the kidneys are paired organs that lie on the posterior wall of the abdomen behind the peritoneum
Weight: 115-170 g (Mean 150 g) Size: 11 cm long, 6 cm wide, and 3 cm thick
Anatomy of the kidneys and urinary system

Renal physiology- Dr. Kh. Pourkhalili
4
B.P.U.M.S
Major parts: Cortex Medulla Outer medulla Inner medulla
Minor calyx Major calyx Pelvis

Renal physiology- Dr. Kh. Pourkhalili
5
Two parts in kidneyB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
6
B.P.U.M.S
Blood flow to the two kidneys is equivalent to about 22% (1.1 L/min) of the cardiac output in resting individuals.
Renal artery → interlobar artery → arcuate artery → interlobular artery (cortical radial arteries) → afferent arteriole → glomerular capillaries (glomerulus) → efferent arteriole → peritubular capillaries, which supply blood to the nephron.
Interlobular vein → arcuate vein → interlobar vein → renal vein.
Blood flow to the kidneys

Renal physiology- Dr. Kh. Pourkhalili
7
B.P.U.M.S
Blood flow to the kidneys

Renal physiology- Dr. Kh. Pourkhalili
8
B.P.U.M.S
Number of nephrons in each human kidney: 1-1.2 million nephrons, which are hollow tubes composed of a single cell
layer.
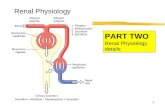
The nephron consists of two parts1. Renal corpuscle (glomerular capillaries and Bowman's capsule)
2. A long tubule which consists of: Proximal tubule Loop of Henle (DTL, ATL & TAL) Distal tubule Collecting duct system.
Nephron as functional unit in the kidney

Renal physiology- Dr. Kh. Pourkhalili
9
B.P.U.M.S
Macula densa
Near the end of the thick ascending limb, the nephron passes between the afferent and efferent arterioles of the same nephron. This short segment of the thick ascending limb is called the macula densa.
Nephron as functional unit in the kidney

Renal physiology- Dr. Kh. Pourkhalili
10
B.P.U.M.S
Nephron as functional unit in the kidney
Distal tubule
Cortical collecting tubule
Medullary collecting tubule
Collecting duct

Renal physiology- Dr. Kh. Pourkhalili
11
B.P.U.M.S
The nephron

Renal physiology- Dr. Kh. Pourkhalili
12
B.P.U.M.S
Cortical nephrones (70-80 %)
Juxtamedullary nephrons (20-30 %) (longer loop of Henle and the efferent arteriole forms not only a network of peritubular capillaries but also a series of vascular loops called the vasa recta).
The juxtamedullary nephrons are important for urine concentration.
Types of nephrons

Renal physiology- Dr. Kh. Pourkhalili
13
Two types of nephronsB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
14
Two types of nephronsB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
15
B.P.U.M.S
Less than 0.7% of the renal blood flow (RBF) enters the vasa recta
Functions of vasa recta:
Conveying oxygen and important nutrients to nephron segments Delivering substances to the nephron for secretion Serving as a pathway for the return of reabsorbed water and solutes to the
circulatory system Concentrating and diluting the urine
Role of vasa recta

Renal physiology- Dr. Kh. Pourkhalili
16
B.P.U.M.S
Vasa recta

Renal physiology- Dr. Kh. Pourkhalili
17
B.P.U.M.S
Proximal tubule cells: have an extensively amplified apical membrane called the brush border (due to the presence of many microvilli) , which is present only in the proximal tubule. The basolateral membrane (the blood side of the cell) is highly invaginated. These invaginations contain many mitochondria.
Cells of descending and ascending thin limbs of Henle's loop: have poorly developed apical and basolateral surfaces and few mitochondria.
Cells of the thick ascending limb and the distal tubule: have abundant mitochondria and extensive infoldings of the basolateral membrane.
The collecting duct cells: principal cells (P cells)and intercalated cells (I cells).
Nephron cells

Renal physiology- Dr. Kh. Pourkhalili
18
B.P.U.M.S
Principal cells have a moderately invaginated basolateral membrane and contain few mitochondria. Principal cells play an important role in reabsorption of NaCl and secretion of K+.
Intercalated cells, which play an important role in regulating acid-base balance, have a high density of mitochondria.
- One population of intercalated cells secretes H+ (i.e., reabsorbs HCO3-), and a second population secretes HCO3- .
Inner medullary collecting duct cells: Cells of the inner medullary collecting duct have poorly developed apical and basolateral surfaces and few mitochondria.

Renal physiology- Dr. Kh. Pourkhalili
19
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
20
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
21
B.P.U.M.S
Ultrastructure of the renal corpuscle The renal corpuscle consists of:
1 -Glomerulus or glomerular capillaries2 -Bowman's capsule

Renal physiology- Dr. Kh. Pourkhalili
22
B.P.U.M.S
Juxtaglomerular apparatus consists of: The macula densa of the thick ascending limb Extraglomerular mesangial cells Renin producing granular cells of the afferent arteriole
The juxtaglomerular apparatus is one component of the tubuloglomerular feedback mechanism that is involved in the autoregulation of RBF and GFR.

Renal physiology- Dr. Kh. Pourkhalili
23
B.P.U.M.S
1. The capillary endothelium of the glomerular capillaries
2. Basement membrane (The total area of glomerular capillary endothelium across which filtration occurs in humans is about 0.8 m2)
3. A single-celled layer of epithelial cells (podocytes)
Filtration barrier

Renal physiology- Dr. Kh. Pourkhalili
24
B.P.U.M.S
Filtration barrier

Renal physiology- Dr. Kh. Pourkhalili
25
B.P.U.M.S
Filtration barrier

Renal physiology- Dr. Kh. Pourkhalili
26
B.P.U.M.S
The endothelium is fenestrated (contains 700-Å holes) and freely permeable to water, small solutes (such as Na+, urea, and glucose), and most proteins but is not permeable to red blood cells, white blood cells, or platelets.
Because endothelial cells express negatively charged glycoproteins on their surface, they may retard the filtration of very large anionic proteins into Bowman's space.
In addition to their role as a barrier to filtration, the endothelial cells synthesize a number of vasoactive substances (e.g., nitric oxide [NO], a vasodilator, and endothelin-1 [ET-1], a vasoconstrictor) that are important in controlling renal plasma flow (RPF).
Role of endothelial cells

Renal physiology- Dr. Kh. Pourkhalili
27
B.P.U.M.S
The basement membrane, which is a porous matrix of negatively charged proteins, including type IV collagen, laminin, proteoglycans and fibronectin, is an important filtration barrier to plasma proteins.
The basement membrane is thought to function primarily as a charge-selective filter in which the ability of proteins to cross the filter is based on charge.*
Role of basement membrane

Renal physiology- Dr. Kh. Pourkhalili
28
B.P.U.M.S
The podocytes, have long finger-like processes that completely encircle the outer surface of the capillaries.
The processes of the podocytes interdigitate to cover the
basement membrane and are separated by apparent gaps called filtration slits (slit pores).
Each filtration slit is bridged by a thin diaphragm that contains pores with a dimension of 40 × 140 Å.
Filtration slits, which function primarily as a size-selective filter, keep the proteins and macromolecules that cross the basement membrane from entering Bowman's space.
Role of podocytes

Renal physiology- Dr. Kh. Pourkhalili
29
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
30
Mesangial cellsB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
31
B.P.U.M.S
Nephrotic syndrome: is produced by a variety of disorders and is characterized by an increase in permeability of the glomerular capillaries to proteins
Proteinuria Hypoalbuminemia Generalized edema
IN THE CLINIC

Renal physiology- Dr. Kh. Pourkhalili
32
Filterability through the filtration barrier Effect of size Filterability of solutes is inversely related to their size
Effect of charge Negatively charged large molecules are filtered less easily than positively
charged molecules of equal molecular size
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
33

Renal physiology- Dr. Kh. Pourkhalili
34
B.P.U.M.S
Filtration Reabsorption Secretion
Basic renal processes involved in urine formation
Excretion= Filtration – reabsorption + secretion

Renal physiology- Dr. Kh. Pourkhalili
35
B.P.U.M.S
Filtration, is the process by which water and solutes in the blood leave the vascular system through the filtration barrier and enter Bowman's space.
Secretion, is the process of moving substances into the tubular lumen from the cytosol of epithelial cells that form the walls of the nephron.
Reabsorption, is the process of moving substances from the lumen across the epithelial layer into the surrounding interstitium.
Excretion, means exit of the substance from the body (ie, the
substance is present in the final urine produced by the kidneys). Excreted= Filtered – Reabsorbed + Secreted
Basic renal processes

Renal physiology- Dr. Kh. Pourkhalili
36
B.P.U.M.S
Creatinine Sodium

Renal physiology- Dr. Kh. Pourkhalili
37
B.P.U.M.S
Glucose PAH

Renal physiology- Dr. Kh. Pourkhalili
38
Glomerular filtration-the first step in urine formation
Composition of the glomerular filtrate
Filtrate is essentially protein-free and devoid of cellular elements, including red blood cells.
Most salts and organic molecules, are similar to the concentrations in the plasma.
Exceptions include calcium and fatty acids, that are not freely filtered because they are partially bound to the plasma proteins.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
39
GFR is about 20 % of RPF
RBF → 1100 - 1200 ml/min
About 5–10% of RBF, flows down into the medulla
RPF → 650 ml/min
GFR → 125 ml/min (180 L/day)
Filtration fraction = GFR/RPF (20 %)
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
40
Determinants of GFR Ultrafiltration occurs because the starling forces Rate of filtration = Kf x NFP Rate of filtration = Kf x (PGC – ΠGC) – (PBC – ΠBC) Kf = hydraulic permeability x surface area NFP = (PGC – ΠGC) – (PBC – ΠBC) The portion of filtered plasma is termed the filtration fraction and is
determined as: FF=GFR/RPF
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
41
B.P.U.M.S
Determinants of GFR

Renal physiology- Dr. Kh. Pourkhalili
42
1. Increased PBS decreases GFR2. Increased glomerular capillary Kf increases GFR3. Increased ΠGC decreases GFR Two factors that influence the glomerular capillary colloid osmotic
pressure:
The arterial plasma colloid osmotic pressure The filtration fraction
B.P.U.M.S
Determinants of GFR

Renal physiology- Dr. Kh. Pourkhalili
43
4. Increased glomerular capillary hydrostatic pressure increases GFR (PGC is the primary regulator of GFR)
PGC is determined by three variables, each of which is under physiologic control:
Arterial pressure Afferent arteriolar resistance Efferent arteriolar resistance
B.P.U.M.S
Determinants of GFR

Renal physiology- Dr. Kh. Pourkhalili
44
B.P.U.M.S
In normal individuals, the GFR is regulated by alterations in PGC that aremediated mainly by changes in afferent or efferent arteriolar resistance.

Renal physiology- Dr. Kh. Pourkhalili
45
B.P.U.M.S
Determinants of GFR
Kf can be altered by the mesangial cells, with contraction of these cells producing a decrease in Kf that is largely due to a reduction in the
area available for filtration .

Renal physiology- Dr. Kh. Pourkhalili
46
Factors affecting the GFRB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
47
B.P.U.M.S
The following pressure measurements were obtained from within the glomerulus of an experimental animal:Glomerular capillary hydrostatic pressure = 50 mm HgGlomerular capillary oncotic pressure = 26 mm HgBowman’s space hydrostatic pressure = 8 mm HgBowman’s space oncotic pressure = 0 mm Hg
Calculate the glomerular net ultrafiltration pressure (positivepressure favors filtration; negative pressure opposes filtration).A. +16 mm Hg B. +68 mm Hg C. +84 mm HgD. 0 mm Hg E. −16 mm Hg F. −68 mm HgG. −84 mm Hg
Question

Renal physiology- Dr. Kh. Pourkhalili
48
B.P.U.M.S
RBF: 22-25% of the cardiac output or near 1100-1200 ml/min, 4 ml/min/gr Blood flow is higher in the renal cortex and lower in the renal medulla. About 5–10% of RBF, flows from efferent arterioles down into the
medulla.
Renal blood flow
(ml/min/gr)

Renal physiology- Dr. Kh. Pourkhalili
49
B.P.U.M.S
1. Pressure difference across renal vasculature2. Total renal vascular resistance
RBF= Like most other organs, the kidneys regulate their blood flow by
adjusting vascular resistance in response to changes in arterial pressure.
The afferent arteriole, efferent arteriole, and interlobular artery are the major resistance vessels in the kidneys and thereby determine
renal vascular resistance
Determinants of renal blood flow

Renal physiology- Dr. Kh. Pourkhalili
50
B.P.U.M.S
Renal resistance vessels

Renal physiology- Dr. Kh. Pourkhalili
51
Physiologic control of GFR and RBF
The determinants of GFR that are most variable and subject to physiologic control include:
PGC ΠGC
These variables, in turn, are influenced by:
Sympathetic nervous system Hormones and autacoids Feedback controls that are intrinsic to the kidneys
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
52
Sympathetic nervous system activation decreases GFR
Strong activation of the renal sympathetic nerves can constrict the renal arterioles (α1) and decrease renal blood flow and GFR.
Severe hemorrhage Brain ischemia
Moderate or mild sympathetic stimulation has little influence on renal blood flow and GFR.
Reflex activation of the sympathetic nervous system resulting from moderate decreases in pressure
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
53
Hormonal and autacoid control of renal circulation
1. Norepinephrine, epinephrine (a1 receptors) and endothelin constrict renal blood vessels and decrease GFR.
2. Angiotensin II preferentially constricts efferent arterioles, thus:
Increased angiotensin II levels raise glomerular hydrostatic pressure while reducing renal blood flow.
It should be kept in mind that increased angiotensin II formation usually occurs in circumstances associated with decreased arterial pressure or volume depletion, which tend to decrease GFR.
In these circumstances, the increased level of angiotensin II, by constricting efferent arterioles, helps prevent decreases in glomerular hydrostatic pressure and GFR
At the same time, though, the reduction in renal blood flow caused by efferent arteriolar constriction contributes to decreased flow through the peritubular capillaries, which in turn increases reabsorption of sodium and water
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
54
3. Endothelial-derived nitric oxide decreases renal vascular resistance and increases GFR.
4. Prostaglandins and bradykinin tend to increase GFR.
Under stressful conditions, such as volume depletion or after surgery, the administration of nonsteroidal anti-inflammatory drugs (NSAIDS), such as aspirin, that inhibit prostaglandin synthesis may cause significant reductions in GFR.
B.P.U.M.S
Hormonal and autacoid control of renal circulation

Renal physiology- Dr. Kh. Pourkhalili
55
B.P.U.M.S
Hormones affect on RBF and GFR

Renal physiology- Dr. Kh. Pourkhalili
56
B.P.U.M.S
The phenomenon whereby RBF and GFR are maintained relatively constant (despite blood pressure changes), named autoregulation, to allow precise control of renal excretion of water and solutes.
Autoregulation, is achieved by changes in vascular resistance, mainly through the afferent arterioles of the kidneys.
Importance of GFR autoregulation in preventing extreme changes in renal excretion
Autoregulation of GFR and RBF

Renal physiology- Dr. Kh. Pourkhalili
57
B.P.U.M.S
1. Tubuloglomerular feedback (role of adenosine and ATP) ATP and adenosine constricts the afferent arteriole, thereby returning GFR to
normal levels. ATP and adenosine also inhibit renin release by granular cells in the afferent
arteriole
2. Myogenic mechanism (role of pressure and stretch activated cationic channels)
Importance of autoregulation Autoregulation of GFR and RBF provides an effective means for uncoupling renal
function from arterial pressure, and it ensures that fluid and solute excretion remain constant.
Mechanisms for autoregulation of RBF and GFR

Renal physiology- Dr. Kh. Pourkhalili
58
B.P.U.M.S
Tubuloglomerular feedback

Renal physiology- Dr. Kh. Pourkhalili
59
B.P.U.M.S
Tubuloglomerular feedback

Renal physiology- Dr. Kh. Pourkhalili
60
B.P.U.M.S
Autoregulation is absent when arterial pressure is less than 80 mm Hg.
Autoregulation is not perfect; RBF and GFR do change slightly as arterial blood pressure varies.
Despite autoregulation, RBF and GFR can be changed by certain hormones and by changes in sympathetic nerve activity.
Three points concerning autoregulation

Renal physiology- Dr. Kh. Pourkhalili
61
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
62
B.P.U.M.S
A novel drug aimed at treating heart failure was tested in experimental animals. The drug was rejected for testing in humans because it caused an unacceptable decrease in the glomerular filtration rate (GFR). Furtheranalysis showed that the drug caused no change in mean arterial blood pressure but renal blood flow (RBF) was increased. The filtration fraction was decreased.
What mechanism is most likely to explain the observed decrease in GFR?
A. Afferent arteriole constriction B. Afferent arteriole dilationC. Efferent arteriole constriction D. Efferent arteriole dilation
Question

Renal physiology- Dr. Kh. Pourkhalili
63
Urine formation by the kidneys tubular processing of the
glomerular filtrate
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
64
Reabsorption and secretion by the renal tubules
Urinary excretion = Glomerular filtration - Tubular reabsorption + Tubular secretion
Tubular reabsorption is selective and quantitatively large
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
65
Reabsorption of filtered water and solutes from the tubular lumen across the tubular epithelial cells, through the renal interstitium, and back into the blood
Transcellular route Paracellular rute
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
66
Transport
Passive transport Simple diffusion Facilitated diffusion (glucose in
basolateral membrane) Active transport Active reabsorption Primary active transport
(sodium-potassium ATPase pump) Secondary active transport Secondary active reabsorption
(glucose by sodium in PT) Active secretion Primary active secretion Secondary active secretion (H+
by sodium in PT) Osmosis Pinocytosis
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
67
Basic mechanisms of transmembrane transport
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
68
Transport maximum
Transport maximum for substances that are actively reabsorbed
B.P.U.M.S
375 mg/min
250
375 mg

Renal physiology- Dr. Kh. Pourkhalili
69
• The renal threshold for glucose is the plasma level at which the glucose first appears in the urine in more than the normal minute amounts. One would predict that the renal threshold would be about 300 mg/dL, that is, 375 mg/min (TmG) divided by 125 mL/min (GFR). However, the actual renal threshold is about 200 mg/dL of arterial plasma, which corresponds to a venous level of about 180 mg/dL. Figure 38–10 shows why the actual renal threshold is less than the predicted threshold. The "ideal" curve shown in this diagram would be obtained if the TmG in all the tubules was identical and if all the glucose were removed from each tubule when the amount filtered was below the TmG. This is not the case, and in humans, for example, the actual curve is rounded and deviates considerably from the "ideal" curve. This deviation is called splay. The magnitude of the splay is inversely proportionate to the avidity with which the transport mechanism binds the substance it transports.

Renal physiology- Dr. Kh. Pourkhalili
70
Transport maximum
Transport maximum for substances that are actively secreted
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
71
Reabsorption and secretion along nephron Proximal tubular reabsorption Normally, about 65 per cent of the filtered load of sodium and water and a
slightly lower percentage of filtered chloride are reabsorbed by the proximal tubule
Cells of the proximal tubule also secrete organic cations and organic anions
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
72
In the first half of the proximal tubule, Na+ uptake into the cell is coupled with either H+ (HCO3-) or organic solutes (glucose and AA)
B.P.U.M.S
First half of the proximal tubule

Renal physiology- Dr. Kh. Pourkhalili
73
In the second half of the proximal tubule, sodium is reabsorbed mainly with chloride ions (para and transcellular) because of higher chloride concentration (around 140 mEq/L compared to 105 in first half)
B.P.U.M.S
Oxalate HCO3- Sulfate
Second half of the proximal tubule

Renal physiology- Dr. Kh. Pourkhalili
74
Osmotic reabsorption of water across the PT B.P.U.M.S
An important consequence of osmotic water flow across the proximal tubule is that some solutes, especially K+ and Ca++, are entrained in the reabsorbed fluid and thereby reabsorbed by the process of solvent drag.

Renal physiology- Dr. Kh. Pourkhalili
75
B.P.U.M.S
Concentrations of solutes along the PT

Renal physiology- Dr. Kh. Pourkhalili
76
Reabsorption and secretion along nephron Solute and water transport in loop of henle Henle's loop reabsorbs approximately 25% of the filtered NaCl and 15-20 % of
the filtered water
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
77
Distal Tubule The very first portion of the distal tubule forms part of the juxtaglomerular
complex The next part of the distal tubule referred to as the diluting segment
because it also dilutes the tubular fluid. It is virtually impermeable to water and urea.
Approximately 5 percent of the filtered load of sodium chloride is reabsorbed in the early distal tubule.
B.P.U.M.S
Reabsorption and secretion along nephron

Renal physiology- Dr. Kh. Pourkhalili
78
Late distal tubule and cortical collecting tubule Principal cells Reabsorb sodium and water from the lumen and secrete potassium ions
into the lumen (sites of action of the potassium-sparing diuretics) Reabsorption of Na+ generates a negative luminal voltage, which provides
the driving force for reabsorption of Cl- across the paracellular pathway
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
79
Reabsorb potassium ions and secrete H+ ions into the tubular lumen
Reabsorption of K+ is mediated by an H+,K+-ATPase located in the apical cell membrane.
B.P.U.M.S
Intercalated cells

Renal physiology- Dr. Kh. Pourkhalili
80
Medullary collecting duct
Medullary collecting ducts reabsorb less than 10 % of the filtered water and sodium
They are the final site for processing the urine and, therefore, play an extremely important role in determining the final urine output of water and solutes.
Special characteristics MCD:
The permeability of the medullary collecting duct to water is controlled by the level of ADH.
Unlike the cortical collecting tubule, the medullary collecting duct is permeable to urea.
The medullary collecting duct is capable of secreting H+ against a large concentration gradient, as also occurs in the cortical collecting tubule. Thus, the medullary collecting duct also plays a key role in regulating acid-base balance.
B.P.U.M.S
Reabsorption and secretion along nephron

Renal physiology- Dr. Kh. Pourkhalili
81
B.P.U.M.S
Medullary collecting duct

Renal physiology- Dr. Kh. Pourkhalili
82
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
83
Summary of concentrations of solutes in the tubular segments
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
84
Regulation of tubular reabsorption Glomerulotubular balance
The ability of the tubules to increase reabsorption rate in response to increased tubular load
If GFR increases from 125 ml/min to 150 ml/min, the absolute rate of proximal tubular reabsorption also increases from about 81 ml/min (65 per cent of GFR) to about 97.5 ml/min (65 percent of GFR).
Some degree of glomerulotubular balance also occurs in other tubular segments, especially the loop of Henle.
The importance of glomerulotubular balance:
It helps to prevent overloading of the distal tubular segments when GFR increases. And acts as a second line of defense to buffer the effects of spontaneous changes in GFR on urine output. (The first line of defense, tubuloglomerular feedback, which help prevent changes in GFR.)
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
85
Regulation of tubular reabsorption Hormonal control of reabsorption
Aldosterone AII ADH ANP PTH Sympathetic stimulation (E, NE)
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
86
Dilates the AA, constricts the EA and relaxes the mesangial cells, Thus this increases pressure in the glomerular capillaries, thus increasing the glomerular filtration rate (GFR), resulting in greater excretion of sodium and water.
Increases blood flow through the vasa recta which will wash the solutes (NaCl and urea) out of the medullary interstitium.
Decreases sodium reabsorption in the distal convoluted tubule (interaction with Na-Cl cotransporter) and cortical collecting duct of the nephron via cGMP dependent phosphorylation of Na channels.
Inhibits renin secretion Reduces aldosterone secretion Relaxes vascular wall by elevation of cGMP
Regulation of tubular reabsorption- role of ANPB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
87
Peritubular capillary and renal interstitial fluid physical forces
Reabsorption =Kf x Net reabsorptive force
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
88
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
89
Regulation of peritubular capillary physical forces The determinants of peritubular capillary reabsorption1. Hydrostatic pressure of the peritubular capillaries which is
influenced by arterial pressure and resistances of the afferent and efferent arterioles.
↑ Arterial pressure tend to raise peritubular capillary hydrostatic pressure and decrease reabsorption rate.
Increase in resistance of either the afferent or the efferent arterioles reduces peritubular capillary hydrostatic pressure and tends to increase reabsorption rate.
2. Colloid osmotic pressure of the plasma in peritubular capillaries ↑ Colloid osmotic pressure increases peritubular capillary reabsorption. The colloid osmotic pressure of peritubular capillaries is determined by: Systemic plasma colloid osmotic pressure Filtration fraction
3. Kf (Increases in Kf raise reabsorption)
4. Hormones (Aldosterone, AII, ADH, ANP, PTH)
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
90
B.P.U.M.S
Regulation of peritubular capillary physical forces

Renal physiology- Dr. Kh. Pourkhalili
91
Renal interstitial hydrostatic and colloid osmotic pressures
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
92
B.P.U.M.S
The amount of substance that is filtered per unit time.
For freely filtered substances, the filtered load is just the product of GFR and plasma concentration.
Sodium filtered load: 0.14 mEq/mL x 125 mL/min = 17.5 mEq/min.
Filtered load

Renal physiology- Dr. Kh. Pourkhalili
93
B.P.U.M.S
The volume of plasma from which that substance has been removed and excreted into urine per unit time (volume/time).
If a substance is present in urine at a concentration of 100 mg/mL and the urine flow rate is 1 mL/min, the excretion rate for this substance is calculated as follows:
If this substance is present in plasma at a concentration of 1 mg/mL, its clearance is as follows:
Clearance

Renal physiology- Dr. Kh. Pourkhalili
94
B.P.U.M.S
A healthy 25-year-old woman was a subject in an approved research study. Her average urinary urea excretion rate was 12 mg/min, measured over a 24-hour period. Her average plasma urea concentration duringthe same period was 0.25 mg/mL.
What is her calculated urea clearance?A. 0.25 mL/min B. 3 mL/minC. 48 mL/min D. 288 mL/min
Question

Renal physiology- Dr. Kh. Pourkhalili
95
B.P.U.M.S
GFR is an index of kidney function. Knowledge of the patient's GFR is essential in evaluating the severity of kidney disease.
The substance used for measuring GFR must: Be freely filtered across the glomerulus into Bowman's space Not be reabsorbed or secreted by the nephron Not be metabolized or produced by the kidney Not alter the GFR
Inulin and creatinine can be used to measure GFR.
Using clearance to estimate GFR

Renal physiology- Dr. Kh. Pourkhalili
96
B.P.U.M.S
Using clearance to estimate GFR Inulin clearance can be used to estimate GFR
Other substances that have been used clinically to estimate GFR include radioactive iothalamate and creatinine.

Renal physiology- Dr. Kh. Pourkhalili
97
Example
B.P.U.M.S

98
Creatinine clearance can be used to estimate GFR
B.P.U.M.S
Using clearance to estimate GFR

Renal physiology- Dr. Kh. Pourkhalili
99
B.P.U.M.S
Correlation between plasma creatinine concentration and GFR

Renal physiology- Dr. Kh. Pourkhalili
100
B.P.U.M.S
If we know the GFR (as assessed from inulin clearance) and the clearance of a given substance, then any difference between clearance and GFR represents net secretion or reabsorption (or, in a few rare cases, renal synthesis).
If the clearance of a substance exactly equals the GFR (inulin clearance), then there has been no net reabsorption or secretion.
If the clearance is greater than the GFR, there must have been net secretion.
Finally, if the clearance is less than the GFR, there must have been net reabsorption.
What can the clearance of a substance tell us?

Renal physiology- Dr. Kh. Pourkhalili
101
B.P.U.M.S
If a substance is completely cleared from the plasma, the clearance rate of that substance is equal to the total renal plasma flow thus:
Amount of the substance delivered to the kidneys by RPF equals to amount of the substance excreted in the urine
RPF x Ps = Us x V
PAH clearance can be used to estimate RPF
The characteristics of the substance used for measuring RPF: Its concentration in arterial and renal venous plasma should be measureable. It is not metabolized, stored, or produced by the kidney Does not itself affect blood flow
Using clearance to estimate RPF

Renal physiology- Dr. Kh. Pourkhalili
102
PAH clearance can be used to estimate RPFB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
103
ExampleB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
104
Effective renal plasma flow (ERPF) ERPF= Clearance of PAH (CPAH)
Example UPAH: 14 mg/mL V urine: 0.9 mL/min PPAH: 0.02 mg/mL
ERPF=?
B.P.U.M.S
PAH
PAH
PVUERPF .
Estimating renal plasma flow by PAH clearance
min/63002.0
9.014 mlERPF

Renal physiology- Dr. Kh. Pourkhalili
105
ERPF can be converted to actual renal plasma flow (RPF)
Average PAH extraction ratio: 0.9
Actual RPF=ERPF/extraction ratio=630/0.9=700 ml/min
RBF = RPF ÷ (1 − Hct) = 700 ÷ (1-0.45)= 700 ÷ 0.55 = 1273
B.P.U.M.S
PAH
PAHPAHPAH P
VPE
Conversion of ERPF to actual RPF
ExtractionERPFActualRPF
%

Renal physiology- Dr. Kh. Pourkhalili
106
Regulation of extracellular fluidosmolarity and sodium
concentration
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
107
Importance of osmolarity regulation Extracellular fluid sodium concentration and
osmolarity are regulated by the amount of extracellular water.
The body water in turn is controlled by: Fluid intake (thirst) Renal excretion of water
In this chapter, we discuss specifically: Mechanisms that cause the kidneys to eliminate excess water by excreting
a dilute urine Mechanisms that cause the kidneys to conserve water by excreting a
concentrated urine Renal feedback mechanisms that control the extracellular fluid sodium
concentration and osmolarity Thirst and salt appetite mechanisms
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
108
Kidneys excrete excess water by forming a dilute urine
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
109
Tubular fluid remains isosmotic in the proximal tubule Tubular fluid becomes dilute in the ascending loop of henle Tubular fluid in distal and collecting tubules is further diluted in the absence
of ADH.
B.P.U.M.S
Renal mechanisms for excreting a dilute urine

Renal physiology- Dr. Kh. Pourkhalili
110
Kidneys conserve water by excreting a concentrated urine
The human kidney can produce a maximal urine concentration of 1200 to 1400 mOsm/L.
Some desert animals, such as the Australian hopping mouse, can concentrate urine to as high as 10,000 mOsm/L
This allows the mouse to survive in the desert without drinking water; sufficient water can be obtained through the food ingested and metabolism.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
111
B.P.U.M.S
The fact that the large amounts of water are reabsorbed into the cortex, rather than into the renal medulla, helps to preserve the high medullary interstitial fluid osmolarity.
Renal mechanisms for excreting a concentrated urine

Renal physiology- Dr. Kh. Pourkhalili
112
Requirements for excreting a concentrated urine
1. High ADH Levels Osmoreceptors and ADH secretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
113
Requirements for excreting a concentrated urine
1. High ADH Levels Osmoreceptors and ADH secretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
114
Requirements for excreting a concentrated urine
2. Hyperosmotic renal medulla The process by which renal medullary interstitial fluid becomes
hyperosmotic:
a. Countercurrent mechanism (50 %) The countercurrent mechanism depends on the special anatomical arrangement of
the loops of Henle and the vasa recta
b. Urea recycling (40-50 %)
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
115
a. Countercurrent mechanism
Countercurrent mechanism produces a hyperosmotic renal medullary interstitium
The major factors that contribute to the buildup of solute concentration into the renal medulla are as follows:
1. Active transport of sodium ions and co-transport of potassium, chloride, and other ions out of the thick portion of the ascending limb of the loop of Henle into the medullary interstitium
2. Active transport of ions from the collecting ducts into the medullary interstitium
3. Facilitated diffusion of large amounts of urea from the inner medullary collecting ducts into the medullary interstitium
4. Diffusion of only small amounts of water from the medullary tubules into the medullary interstitium, far less than the reabsorption of solutes into the medullary interstitium
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
116
Steps involved in causing hyperosmotic renal medula
B.P.U.M.S
Countercurrent multiplier system in the loop of Henle for producinga hyperosmotic renal medulla

Renal physiology- Dr. Kh. Pourkhalili
117
Role of distal tubule and collecting ducts in excreting a concentrated urine
B.P.U.M.S
The fact that the large amounts of water are reabsorbed into the cortex, rather than into the renal medulla, helps to preserve the high medullary interstitial fluid osmolarity.

Renal physiology- Dr. Kh. Pourkhalili
118
Recirculation of urea from collecting duct to loop of henle contributes to hyperosmotic renal medulla
B.P.U.M.S
b. Role of urea recycling

Renal physiology- Dr. Kh. Pourkhalili
119
Countercurrent exchange in the vasa recta preserves hyperosmolarity of the renal medulla
There are two special features of the renal medullary blood flow that contribute to the preservation of the high solute concentrations:
1. The medullary blood flow is low, accounting for less than 5 per cent of the total renal blood flow. This sluggish blood flow is sufficient to supply the metabolic needs of the tissues but helps to minimize solute loss from the medullary interstitium.
2. The vasa recta serve as countercurrent exchangers, minimizing washout of solutes from the medullary interstitium
B.P.U.M.S
Countercurrent exchange in the vasa recta

120
Countercurrent exchange in the vasa rectaB.P.U.M.S
Increased medullary blood flow can reduce urine concentrating ability

Renal physiology- Dr. Kh. Pourkhalili
121
AntiduresisB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
122
Summary of urine concentrating mechanism and changes in osmolarity in different segments of the tubules
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
123
Obligatory urine volume A normal 70-kilogram human must excrete about 600 milliosmoles
of solute each day.
Maximal urine concentrating ability is 1200 mOsm/L
Drinking 1 liter of seawater with a concentration of 1200 mOsm/L would provide a total sodium chloride intake of 1200 milliosmoles.
If maximal urine concentrating ability is 1200 mOsm/L, the amount of urine volume needed to excrete 1200 milliosmoles would be 1200 milliosmoles divided by 1200 mOsm/L, or 1.0 liter.
Why then does drinking seawater cause dehydration?
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
124
Osmolar clearances When the urine is dilute, water is excreted in excess of solutes. Conversely, when the urine is concentrated, solutes are excreted in
excess of water.
Osmolar clearance (Cosm): The volume of plasma cleared of solutes each minute.
For example: If Posm= 300 mosm/L, Uosm= 600 mosm/L, urine flow rate is 1 ml/min
(0.001 L/min)
Osmolar clearance is 0.6 mosm/min divided by 300 mosm/L, or 0.002 L/min (2.0 ml/min).
This means that 2 milliliters of plasma are being cleared of solute each minute.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
125
Free-water clearance (CH20) is calculated as the difference between water excretion (urine flow rate) and osmolar clearance:
Thus, the rate of free-water clearance represents the rate at which solute-free water is excreted by the kidneys.
When free-water clearance is positive, excess water is being excreted by the kidneys
When free-water clearance is negative, excess solutes are being removed from the blood by the kidneys and water is being conserved.
Thus: When urine osmolarity is greater than plasma osmolarity, free-water
clearance will be negative, indicating water conservation When urine osmolarity is lower than plasma osmolarity, free-water
clearance will be positive, indicating that water is being removed from plasma.
B.P.U.M.S
Free water clearances

Renal physiology- Dr. Kh. Pourkhalili
126
Disorders of urinary concentrating ability
Inappropriate secretion of ADH (Either too much or too little ADH secretion)
Impairment of the countercurrent mechanism. A hyperosmotic medullary interstitium is required for maximal urine
concentrating ability. No matter how much ADH is present, maximal urine concentration is limited by the degree of hyperosmolarity of the medullary interstitium.
Inability of the distal tubule, collecting tubule, and collecting ducts to respond to ADH.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
127
Failure to Produce ADH (Central diabetes insipidus) The treatment for central diabetes insipidus is administration of a synthetic
analog of ADH, desmopressin.
Inability of the kidneys to respond to ADH (Nephrogenic diabetes insipidus)
The treatment for nephrogenic diabetes insipidus is to correct, if possible, the underlying renal disorder.
B.P.U.M.S
Disorders of urinary concentrating ability

Renal physiology- Dr. Kh. Pourkhalili
128
Control of ECF osmolarity and Na+ concentration
Estimating plasma osmolarity from plasma sodium concentration
Because sodium and its associated anions (Cl-, HCO3-) account for about 94 per cent of the solutes in the extracellular compartment, plasma osmolarity can be roughly approximated as:
Posm=2.1 x Plasma sodium concentration Posm=2.1 x 142= 298 mosm/L
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
129
Two primary systems regulating the concentration of sodium and osmolarity of extracellular fluid:
1. The osmoreceptor-ADH system2. The thirst mechanism
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
130
1. The osmoreceptor-ADH systemB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
131
CNS centers for thirst1. Anteroventral wall of the third ventricle (AV3V) Subfornical organ OVLT
2. A small area located anterolaterally in the preoptic nucleus
Stimuli for thirst
B.P.U.M.S
2. Role of thirst in controlling ECF osmolarity and Na cocentration

Renal physiology- Dr. Kh. Pourkhalili
132
Integrated responses of osmoreceptor-ADH and thirst mechanisms in controlling extracellular fluid osmolarity and sodium concentration
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
133
Role of AII and aldosterone in ECF osmolarity and Na concentration
Angiotensin II and aldosterone have little effect on sodium concentration, because:
Although these hormones increase the amount of sodium in the ECF, they also increase the ECF volume by increasing reabsorption of water along with the sodium.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
134
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
135
B.P.U.M.S
Regulation of potassium excretion

Renal physiology- Dr. Kh. Pourkhalili
136
Normal K intake, distribution and output from the body
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
137
Regulation of potassium excretion
ECF K concentration: 4.2 ±0.3 mEq/L
This precise control is necessary because many cell functions are very sensitive to changes in extracellular fluid potassium concentration.
For instance, an increase in plasma potassium concentration of only 3 to 4 mEq/L can cause cardiac arrhythmias, and higher concentrations can lead to cardiac arrest or fibrillation.
Total ECF K → (14×4.2)→ 59 milliequivalents Total ICF K → (28×140)→ 3920 milliequivalents
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
138
Effect of adding or removing K to ECF
The potassium in a single meal → as high as 50mEq Daily intake of K → 50 - 200 mEq/day
Therefore: Failure to rapidly rid the extracellular fluid of the ingested potassium could
cause life-threatening hyperkalemia.
Likewise, a small loss of potassium from the extracellular fluid could cause severe hypokalemia.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
139
Factors that can influence the distribution of K between the intra- and extracellular compartments
Insulin stimulates k uptake into cells by activating Na-K ATPases in many cells
Aldosterone increases potassium uptake into cells
↑ K intake → ↑ secretion of aldosterone → ↑ cell potassium uptake.
↑ Aldosterone secretion (Conn's syndrome) → hypokalemia.
↓ Aldosterone secretion (Addison's disease) → hyperkalemia due to accumulation of potassium in ECF as well as to renal retention of K.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
140
Factors that can influence the distribution of K
B-adrenergic stimulation increases cellular uptake of potassium probably by (up-regulating the activity of the sodium-potassium pump)
Acid-base abnormalities can cause changes in potassium distribution
Metabolic acidosis increases extracellular potassium concentration, in part by causing loss of potassium from the cells.
Metabolic alkalosis decreases extracellular fluid potassium concentration.
↑ H+ → ↓ activity Na-K ATPase pump → ↓cellular uptake of K and raises extracellular K
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
141
Factors that can influence the distribution of K
Cell lysis causes increased extracellular K concentration As occurs with severe muscle injury or with red blood cell lysis
Strenuous exercise can cause hyperkalembia by releasing potassium from skeletal muscle.
Increased ECF osmolarity causes redistribution of K from the cells to ECF.
In diabetes mellitus, large increases in plasma glucose raise extracellular osmolarity, causing cell dehydration and movement of potassium from the cells into the extracellular fluid
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
142
Overview of renal potassium excretionB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
143
Overview of renal potassium excretionB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
144
Most of the day-to-day variation of potassium excretion is not due to changes in reabsorption in the proximal tubule or loop of Henle but:
Most daily variation in potassium excretion is caused by changes in potassium secretion in distal and collecting tubules
Thus, most of the day-to-day regulation of potassium excretion occurs in the late distal and cortical collecting tubules, where potassium can be either reabsorbed or secreted, depending on the needs of the body.
B.P.U.M.S
Overview of renal potassium excretion

Renal physiology- Dr. Kh. Pourkhalili
145
Potassium secretion by principal cellsB.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
146
Intercalated cells reabsorb k during potassium depletion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
147
Factors that regulate k secretion by principal cells
Plasma potassium concentration
Aldosterone
Tubular flow rate
Hydrogen ion concentration
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
148
1. Increased ECF K concentration stimulates potassium secretion by 3 mechanisms:
a. Increased ECF K concentration stimulates the Na-K ATPase pump, thereby increasing K uptake across the basolateral membrane.
b. Increased ECF K concentration increases the K gradient from the renal interstitial fluid to the interior of the epithelial cell; this reduces backleakage of potassium ions from inside the cells through the basolateral membrane.
c. Increased K concentration stimulates aldosterone secretion, which further stimulates potassium secretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
149
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
150
2. Aldosterone stimulates potassium secretion by principal cells
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
151
Increased extracellular potassium concentration stimulates aldosterone secretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
152
Increased plasma k concentration directly and indirectly raises k secretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
153
Blockade of aldosterone feedback system greatly impairs control of potassium concentration
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
154
3. Increased distal tubular flow rate stimulates potassium secretion.
A rise in distal tubular flow rate, as occurs with: Volume expansion High sodium intake Diuretic drug treatment
Conversely, a decrease in distal tubular flow rate, as caused by sodium depletion reduces potassium secretion.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
155
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
156
4. Acute acidosis decreases potassium secretion
The primary mechanism by which increased hydrogen ion concentration inhibits potassium secretion is:
Decreased activity of the Na-K ATPase pump. This in turn decreases intracellular potassium concentration and subsequent passive diffusion of potassium across the luminal membrane into the tubule.
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
157
Chronic acidosis, lasting over a period of several days, increases urinary potassium excretion.
The mechanism for this effect is: Chronic acidosis inhibit proximal tubular sodium chloride and water
reabsorption, which increases distal volume delivery, thereby stimulating the secretion of potassium.
This effect overrides the inhibitory effect of hydrogen ions on the Na-K ATPase pump. Thus, chronic acidosis leads to a loss of potassium, whereas acute acidosis leads to decreased potassium excretion
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
158
B.P.U.M.S

Renal physiology- Dr. Kh. Pourkhalili
159
Micturition reflexB.P.U.M.S
Physiologic anatomy and nervous connections of the bladder

Renal physiology- Dr. Kh. Pourkhalili
160
Filling of the bladder and cystometrogram B.P.U.M.S