Facial nerve injury and reanimation
-
Upload
mohamed-rahil -
Category
Health & Medicine
-
view
1.339 -
download
1
Transcript of Facial nerve injury and reanimation


Embriology of facial nerve
• The facial nerve is the 7th cranial nerve .
• formation of facial nerve began at the 3rd week of embryonic life from the 2nd pharangeal arch .
• The complexity of the nerve's course, its branching patterns, and its anatomic relationships are completed at the end of 3rd month of prenatal life.
• During this period, the muscles of facial expression also differentiate, become functional, and actively contract.

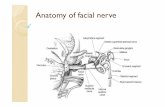
Anatomy of facial nerve
• emerges from the brainstem between the pons and the medulla
• controls the muscles of facial expression, and taste sensations from the anterior two-thirds of the tongue .
• also supplies preganglionic parasympathetic fibers to several head and neck ganglia .
• The motor part of the facial nerve arises from the facial nerve nucleus in the pons while the sensory part of the facial nerve arises from the nervus intermedius.

Intracranial part
• The portion of the nerve from the brainstem to the internal auditory canal
• Carries preganglionic parasympathetic fibers and special afferent sensory fibers

(( Intra tem poral part ))
Important branches of facial nerve in this part :
1. Greater superfacial petrosal nerve :
Carries parasympathetic fibers to lacrimal gland and glands of the nose and palate.
2. Nerve to Stapedius muscle3. Chorda tympani carries parasympathetics to the
submandibular and sublingual glands & Taste to anterior 2/3 of the tongue .

Extracranial part
Main trunk ( 15 – 20 mm) :1. Give branches to the posterior
belly of the digastric and stylohyoid muscles.
2. Postauricular to occipitofrontalis muscles
Branching of the extracranial segments in the parotid gland that splitting it into a superficial and deep lobe :
• Temporal• Zygomatic • Buccal • Marginal mandibular • Cervical

Component of nerve
• Endoneurium :• Surrounds each nerve fiber• Provides endoneural tube for
regeneration
• Perineurium :• Surrounds a group of nerve fibers
(fascicle).• Provide tensile srtength• Protect nerve from infection
• Epineurium :• Surrounds the entire nerve • Provides nutrition to the nerve

Sunderland Nerve Injury Classification
Class I (Neuropraxia)• Axon remain intact• Conduction block caused by cessation of axoplasmic flow• Full recovery
Class II (Axonotmesis)• Axons are disrupted• Endoneural tube still intact• Full recovery expected
Class III (Neurotmesis)• Neural tube is disrupted• Poor prognosis• If regeneration occurs, high incidence of synkinesis (involuntary movement
of muscles associated with voluntary movement other muscles )

Sunderland Nerve Injury Classification
Class IV• Epineurium remains intact• Perineurium, endoneurium, and axon disrupted• Poor functional outcome with higher risk for synkinesis
Class V• Complete disruption• Little chance of regeneration• Risk of neuroma formation


Causes of Facial nerve paralysis supranuclear lesions :
• Congenital abnormalities, stroke , malignancies, trauma , vascular conditions and other causes .
• only lower part of the opposite side of the face is paralyzed.
• The upper part with the frontalis and orbicularis oculi escapes due to bilateral representation in the cerebral cortex.
infranuclear lesions :• Malignancy (parotid gland as well as tumors of adjacent
structures) , trauma, infections, Bell’s palsy, osteopetrosis and iatrogenic causes .
• the whole of the face of the same side gets paralyzed.


Signs and symptoms of facial nerve paralysis
• The symptoms according to the level of injury of facial nerve.
At internal auditory meatus; loss of lacrimation, stapedial reflex, taste
from most of anterior two-third of tongue, lack of salivation and paralysis of muscles of facial expression.
Below geniculate ganglion; loss of stapedial reflex, taste from
anterior two third of tongue, lack of salivation and paralayis of facial expression muscles.
Region below stylomastoid foramen paralysis of facial expression muscles.


House-Brackmann Grading System
used for clinical assessment of patient with facial nerve paralysis.

Grade CharacteristicsI. Normal facial function in all areasII. Mild dysfunction
Slight weakness noticeable on close inspection• Forehead - Moderate-to-good function• Eye - Complete closure with minimal effort• Mouth - Slight asymmetry
III. Moderate dysfunction
Obvious asymmetry.• Forehead - Slight-to-moderate movement• Eye - Complete closure with maximum effort• Mouth - Slightly weak with maximum effort
IV. Moderately severe dysfunction
• Obvious weakness and/or disfiguring asymmetry• Forehead – No motion• Eye - Incomplete closure• Mouth - Asymmetric with maximum effort
V. Severe dysfunction
Only minimal motion seen. • At rest, asymmetry • Forehead – No movement• Eye - Incomplete closure• Mouth - Slight movement
VI. Total paralysis No movement

Grade Definition
I Normal
II Very mild weakness
III Obvious weakness, asymmetry of mouthComplete eye closure
IV Obvious weakness, asymmetry of mouthIncomplete eye closure
V Very slight movement only
VI No movement at all

Preoperative evaluation
• History : focusing on the onset and duration of weakness.
• complete physical exam of the head and neck including a cranial nerve examination .
• The muscles of facial expression are evaluated for symmetry and function—both statically and dynamically.
• electrical testing is performed to determine the
physiological status of the facial nerve branches and the muscles of the face.
(EMG & ENG)

electrical testing of facial nerve ELECTRONEUROGRAPHY (ENOG)• measure of the amount of intact axons relative to the
healthy side .• used to determine prognosis pre-operatively• Degeneration greater than 90% is correlated with a
poor prognosis .
ELECTROMYOGRAPHY (EMG)• Electromyography is often used as an adjunct to
ENOG• EMG can be used to identify false positive ENOG
results
NERVE EXCITABILITY TEST (NET)• determine prognosis for facial nerve
recovery• A threshold difference of greater than 3.5 mAmps
correlates with a poor prognosis.

Rehabilitation of the Paralyzed Face
Goals– Functional
• EYE PROTECTION• Oral competence
– Cosmetic• Symmetry at rest• Volitional movement
– Facial expressions

MANAGEMENT of facial nerve paralysis
Treatment of facial nerve weakness or paralysis may be : supportive medical surgical eye care combination of all four .
Selection of the type of management depend on :
• The cause of the facial paralysis• Type of injury and its location• The duration of deficit

Medical Treatment• Medical treatment is instituted to decrease the swelling.• It often involves the use of steroids. This treatment may be continued until the
nerve shows sign of recovery.
Prednisolone 60-80 mg/day in divided doses intial 4-5 days,then taper over next 7-10 days.– Decreases the possibility of permanent paralysis .– From swelling of facial nerve in facial canal .– Decreases the severe pain .
Antiviral may be effective in some cases of paralysis (bells palsy). • Acyclovir 400mg 5 times a day –10 days• Valacyclovir 1000mg /day 5-7 days .

Surgical Reanimation Techniques Broadly classified into: I . Neural methods: • Facial Nerve Decompression• Micro-neurological surgery to re-suture the damaged nerve.• Nerve graft (to overcome gaps)• Cross-Facial Nerve Grafting
• Nerve Transfers • Hypoglossal to facial • Spinal accessory to facial • Phrenic to facial II . Musculofascial transpositions:• Move new muscles and nerves into the face to take the place of the injured facial nerve.III . Facial plastic procedures.IV. Prosthetics.

OTHER CLASSIFICATION
• Static– Slings– Gold weight– Tarsorrhaphy– Lower lid
shortening
• Dynamic– Nerve grafting– Muscle transfer
• Regional• Free flap

Facial Nerve Decompression• Performed in severe cases when the facial nerve is seriously
deteriorating.• Patients are at risk of permanent paralysis and have a poor
prognosis without aggressive intervention. • To be effective, the surgery must be performed within 2 weeks of
the onset of symptoms.
• Most common approach for facial nerve decompression : Retrosigmoid facial nerve decompression Translabyrinthine facial nerve decompression


Direct nerve repair• the most effective procedure for reanimating the
paralyzed face.
• should be done as soon as possible, before significant muscle degeneration occurs (preferably < 6 months).
• If the stumps of the nerve have a neuroma or appear crushed, the nerve ends should be “freshened” until normal appearing nerve is evident.
• The nerve stumps should be realigned in
fascicular groups without tension.
• The perineurium is sutured together followed by the epineurium using 9-0 or 8-0 monofilament nonresorbable nylon suture .

Direct nerve repair
More recently, tissue engineering has provided nerve conduits, which function as guides for axonal growth.
Depending on the materials used for their construction, they can be classified as natural, when based on laminin, collagen or even vessels and decellularized nerves, or artificial, usually made of polymers .
The major limitation for use of nerve conduits is the low rate of axonal growth, which may not yield full repair within the available time and chronic inflammtion which should be removed after period of time
Studies have shown that the conduits are effective in promoting repair of nerve gaps measuring up to 3 cm, while nerve autografts are required for bridging of larger distances
Recently,Wakao et al. used biodegredable collagen nerve conduits filled with autologous bone marrow MSC differentiated into Schwann cells to promote repair

Nerve Grafting
• Integrity of proximal and distal nerve stumps and facial muscles.
• There is a gap in the facial nerve that cannot be primarily repaired.
• The length of the graft should be about 20% longer than the gap.
• The graft must also be placed in a tissue bed that is free of scar.

Nerves most commonly used for grafting ;
• Great auricular nerve– Usually in surgical field.– Can only harvest 7-10cm of this nerve.– Loss of sensation to lower auricle &
skin over the angle.• Sural nerve– Located 1 cm posterior to the lateral
malleolus.– Can provide 35cm of length.– Very useful in cross facial anastomosis.– Loss of sensation to lateral calf and
foot.

Nerve transfers
• Nerve transposition is also known as facial-hypoglossal transfer
• This technique is employed when direct repair or grafting is not possible.
• This may be due to the absence of the main trunk of the facial nerve or in cases of intracranial nerve damage.
• may be performed immediately or up to several years after the injury
• Requires that the patient have an intact distal nerve segment and facial musculature suitable for reinnervation which determined by EMG .
• Facial appearance may be nearly normal at rest. There will be some persistent weakness of the face at movement .

Nerve transfers
• Hypoglossal nerve– Direct hypoglossal-to-facial graft• Distal branch of facial nerve is attached
to hypoglossal nerve.• Complications – atrophy of ipsilateral
tongue, difficulties with chewing, speaking, and swallowing.
– Partial hypoglossal-to-facial jump graft• Uses a nerve cable graft, to connect
the distal end of the facial nerve to a notch in the hypoglossal nerve
• Much fewer complications, but increased recovery time.


Cross-Facial Nerve Grafting• This technique employs a nerve graft (typically
the sural nerve) that acts as a conduit for motor axons from the normal side, contralateral facial nerve.
– Options
• Single contralateral branch to distal nerve anastomosis.
• Multiple anastomoses from segmental branches to segmental branches
• disadvantages : • Additional donor site in the leg.• Violating the normal side of the face.• Two or more suture lines for the axons to cross.• Long interval until return of function

Static Suspension Procedures It is used for suspension of the forehead , eyelids, nares, oral commissure,
upper and lower lip. used to achieve symmetry at rest . They provide no dynamic return of function. It can be used alone or in combination with muscle transfers.• Autologous materials• Tensor fasciae lata.• Temporalis fascia. • Synthetic materials• Silastic rods.• Gore-Tex.
• Dynamic transfers . Local Muscle Transposition Free functioning muscle transfer.


Static slings before and after the operation

Dynamic transfers
Local Muscle Transposition Free functioning muscle transfer.

Dynamic transfers
• Local Muscle Transposition• It is employed when there has been
long standing paralysis and the muscles of facial expression have atrophied.
• The masseter and temporalis muscles are the two most commonly used.
• can activate it by clenching the teeth.
• These may be transposed to the upper and lower eyelids and the ala and the upper and lower lips.


Dynamic transfers
• Free muscle transfer• It is appropriate for those with
intracranial or congenital causes of facial paralysis.
• A variety of donor muscles have been described. These include the gracilis, latissimus dorsi, pectoralis minor.
• The procedure is performed in two steps ;
• In the first step, a cross-face nerve graft is performed.
• The second stage is the muscle transfer which is done 9 to 12 months later.



Eye Care• Glasses should be worn whenever the patient outside . • Contact lenses should not be worn in this situation . • If the eye is dry, we can use eye drops (artificial tears ) .• Ointment may be prescribed for use at bedtime .
• The best protection for night/sleep hours is to place a clear eye guard over the eye. This can be secured in place with tape.
• Any eye problems or irritation which does not quickly pass should warrant consultation with ophthalmologist as soon as possible.
• If facial weakness is anticipated following surgery, a silk thread is sometimes
placed in the lid to help close it. When lid closure is adequate this easily removed.
• In some cases of long-standing paralysis, it may be necessary to insert a weight ( gold plate) into the eyelid to close the eye or perform some other procedure to help the eyelid close (i.e. tarsorrhaphy).


Lid Gold Weights
46

Miniature Micro Chip Technology and Artificial Muscle Implant
47

The Nose
• The collapse of the nasal sidewall can be corrected either from the outside or the inside of the nose.
• Outside techniques involve placing strips of suspension material from the cheekbone, under the skin, to the nasal sidewall, and suspending the nasal sidewall in its anatomic position.
• To widen the nasal cavity from the inside, small cartilage grafts can be inserted into the framework of the nose.
48

Adjunctive Procedures
Soft-tissue procedures to improve symmetryo Rhytidectomyo Excision of redundant intraoral mucosa.o Blepharoplastyo Brow lift
Procedures for droolingo Wilkie procedureo Submandibular gland resection with parotid duct ligation
Modification of normal side to improve symmetry:o Neurectomy.o Myectomy.


Modern studies about facial nerve reanimation

Daily Facial stimulation to Improve Recovery after Facial Nerve Repair in rats
By Robin W. Lindsay and colleagues , in 2010
• The slow rate of facial nerve regeneration following certain injury and even surgical management of paralysed facial nerve can lead to degeneration of the motor end organ and permanent loss of function.
• A variety of pharmacologic agents have been shown to
improve motor nerve regeneration in animals, including ; angiotensin II, nitric oxide,and brain-derived neurotropic factor but due to it is adverse effects and the difficulties with drug delivery and bioavailability,none of these drugs is in clinical use.
• So this study came to improves recovery of facial nerve after transection and repair depending on daily mechanical whisker stimulation via either protraction or retraction .
Full recovery occure 4 months after complete nerve transection .

Peripheral Nerve Repair with Cultured Schwann CellsMaria Carolina O. Rodrigues and her colleages
26 January 2012
• The bone marrow is a rich source of mesenchymal cells, which can be differentiated in vitro into Schwann cells and subsequently engrafted into the damaged nerve.
• Experimental studies provide evidence of functional, histological, and electromyographical improvement following transplantation of bone-marrow-derived mesenchymal cells in animal models of peripheral nerve injury which can be diffrentiated in to Schwann cells that have a central role in nerve repair,
• Activated Schwann cells produce collagen and laminin, creating a tunnel of extracellular matrix, and express cell adhesion molecules and receptors, including IL-1, N-cadherin, gamma integrins, and the neural cell adhesion molecule
• other alternative sources of mesenchymal stromal cells are :• the adipose tissue and skin• Also, the bulge area of the hair and whisker follicles

Stem cells could help regenerate facial nerve José Tadeu Arantes . August 14, 2013
• Nerve regeneration depends critically on Schwann cell structure which provide support and growth factors that is essential for nerve growth . The problem is that Schwann cells are scarce in an organism. So the ulternative is the use of stem cells to bridge this gap
• The study was conducted in animals (rats) subjected to neurotmesis .The animals were split into four groups. In the first, the two remaining parts of the selected nerve were connected by a hollow silicon tube; in the second, the tube was filled with an acellular gel; in the third, it was filled with undifferentiated stem cells; and finally, in the fourth, in was filled with Schwann-like differentiated stem cells .
• The result was that all animals that received stem cells (undifferentiated or differentiated) had a much more significant improvement than those that received an empty tube or a tube filled with gel. Which confirme the rule of stem cells in nerve regeneration .
• the experiment brought one surprise: undifferentiated stem cells had a better performance than differentiated (schwann cells) .

Effect of Platelet Rich Plasma on Facial Nerve Regeneration
Platelets contain various growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-, and vascular endothelial growth factor.
When platelets are activated,they release these factors, which play important biological roles in various conditions.
It has been demonstrated that neurons express PDGF receptors, PDGF- has been proven to be a survival factor for Schwann cells . Also, an augmented PDGF- expression in peripheral neurons has been found after peripheral nerve injury, suggesting a role in peripheral nerve regeneration These findings have led some authors to investigate the effects of PDGF, which has been found to improve regeneration and remyelination of the nervous system.
suturing of the nerve and application of PRP demonstrated the greatest increase in the axon counts after treatment than application of PRP without suturing .

Georgiade Plastic, maxillofacial and reconstructive surgery
Peterson's Principles of Oral and Maxillofacial Surgery ,2012
Grabb___Smith_s_Plastic_Surgery__6th_Ed.2007
Facial_Plastic_Reconstructive_and_Trauma_Surgery
Articles from internet
references

THANK YOU FOR LISTENING