FACIAL REANIMATION BY MEANS OF THE YPOGLOSSAL NERVE: … Anatomia NS.pdf · 2019-11-20 · FACIAL...
Transcript of FACIAL REANIMATION BY MEANS OF THE YPOGLOSSAL NERVE: … Anatomia NS.pdf · 2019-11-20 · FACIAL...
FACIAL REANIMATION BY MEANS OF THEHYPOGLOSSAL NERVE: ANATOMIC COMPARISONOF DIFFERENT TECHNIQUES
OBJECTIVE: The goal of this study was to determine the various anatomical and surgi-cal relationships between the facial and hypoglossal nerves to define the required lengthof each for a nerve transfer, either by means of a classical hypoglossal-facial nerve anas-tomosis or combined with any of its variants developed to reduce tongue morbidities.METHODS: Five adult cadaver heads were bilaterally dissected in the parotid and sub-maxillary regions. Two clinical cases are described for illustration.RESULTS: The prebifurcation extracranial facial nerve is found 4.82 � 0.88 mm fromthe external auditory meatus, 5.31 � 1.50 mm from the mastoid tip, 15.65 � 0.85 mmfrom the lateral end of C1, 17.19 � 1.64 mm from the border of the mandible condyle,and 4.86 � 1.29 mm from the digastric muscle. The average lengths of the mastoid seg-ment of the facial nerve and the prebifurcation extracranial facial nerve are 16.35 �1.21 mm and 18.93 � 1.41 mm, respectively. The average distance from the bifurca-tion of the facial nerve to the hypoglossal nerve turn is 31.56 � 2.53 mm. For a directhypoglossal-facial nerve anastomosis, a length of approximately 19 mm of the hypoglos-sal nerve is required. For the interposition nerve graft technique, a 35 mm-long graft isrequired. For the technique using a longitudinally dissected hypoglossal nerve, an aver-age length of 31.56 mm is required. Exposure of the facial nerve within the mastoidprocess drilling technique requires 16.35 mm of drilling.CONCLUSION: This study attempts to establish the exact graft, dissection within thehypoglossal nerve, and mastoid drilling requirements for hypoglossal to facial nervetransfer.
KEY WORDS: Facial reanimation, Hypoglossal-facial anastomosis, Hypoglossal nerve
Neurosurgery 61:ONS-41–ONS-50, 2007 DOI: 10.1227/01.NEU.0000279996.11201.FD www.neurosurgery-online.com
NEUROSURGERY VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 | ONS-41
TUMOR
Alvaro Campero, M.D.Department of Neurosurgery,Hospital de Clínicas,University of Buenos AiresSchool of Medicine,Buenos Aires, Argentina
Mariano Socolovsky, M.D.Department of Neurosurgery,Hospital de Clínicas,University of Buenos AiresSchool of Medicine,Buenos Aires, Argentina
Reprint requests:Mariano Socolovsky, M.D.,1175 La Pampa Street,5th Floor, Apt A,Buenos Aires, 1428, Argentina.Email: [email protected]
Received, April 22, 2006.
Accepted, January 5, 2007.
Functional preservation of the facial nerve during removalof lesions along its course has been of considerable concernfor surgeons approaching tumors at the base of the cra-
nium. In spite of the striking development in surgical tech-niques during the second half of the 20th century and theremarkable improvement in morbidity and mortality of manytumor excision procedures, facial paralysis is not an uncom-mon postoperative event.
Since 1904, when Korte (10) performed the first facial reani-mation surgery (Fig. 1A), multiple techniques have beendescribed with the same purpose, the most widely used to datebeing the classical hypoglossal-facial nerve anastomosis (11,12, 15–18, 20, 23). Basic morbidities of this technique are relatedto hypoglossal nerve section, producing moderately severeswallowing and speech disorders. Over the past two decades,however, many variants of this procedure have been specifi-cally developed to reduce morbidity after complete hypoglos-sal nerve section (1, 4, 6, 13, 14, 19) (Fig. 1, B–D).
Other facial reanimation techniques, such as cross-facial anas-tomosis and variants (including the “babysitting” procedure),gracillis free-transfer, masseteric-facial nerve transfer, and staticmuscle transfers (23, 25, 26, 27) exist, but these do not involve theuse of the XIIth cranial nerve as the only axon donor and, thus,are beyond the scope of this study. Our focus in this study is onthe anatomic and surgical relationships of the facial andhypoglossal nerves given their relevance to determine the expo-sure length required in each technical variant. This would stan-dardize the hypoglossal-facial nerve transfer and its variants,allowing for an easier performance of these procedures.
MATERIALS AND METHODS
Laboratory DissectionFive adult cadaver heads providing 10 facial nerves (Cranial Nerve
[CN] VII) and 10 hypoglossal nerves (CN XII) were fixed in formalin
Surgical Anatomy and Technique
and injected with colored silicone. This cadaver material was providedby the Anatomy Department of the University of Buenos Aires Schoolof Medicine. The technique applied for the injection of arteries andveins was taught to one of the authors (AC) at the University of FloridaAnatomy Laboratory, directed by Professor Rhoton. Dissections of theparotid and submaxillary regions were carried out in each specimenunder 6� to 20� magnification. Then, the different techniques of nervetransfer from CN XII to CN VII were performed on the specimens. Theclassical hypoglossal-facial nerve technique and the partial hypoglos-sal section were combined with interposition nerve graft, longitudinaldissection of CN XII, or drilling of the facial nerve at the mastoid por-tion of the temporal bone. A precision caliber was used for measure-ments during and after dissections.
RESULTS
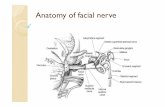
Surgical AnatomyThe peripheral facial nerve consists of six portions: cisternal,
meatal, labyrinthine, tympanic, mastoid, and extracranial (fromproximal to distal). The extracranial portion begins where thenerve exits the skull through the stylomastoid foramen intothe parotid gland to branch into the temporo- and cervicofacial
divisions. The portion of the facial nerve between the stylo-mastoid foramen and its bifurcation, referred to as prebifurca-tion extracranial facial nerve (PBEF), is inferior to the externalauditory meatus (EAM), medial and anterior to the mastoidprocess, lateral to the styloid process, superior and anterior tothe atlas, and posterior to the mandible condyle (Fig. 2C).
Position of the PBEF Relative to the EAMThe EAM comprises two portions: an osseous internal por-
tion and a fibrocartilaginous external portion. The fibrocarti-laginous portion has two membranes, a cartilaginous and afibrous one. These are joined by their borders, forming acomplete canal. The cartilaginous membrane fills the infe-rior and anterior portions of the canal. In the samples stud-ied, the average distance from the inferior border of the EAMcartilage to the PBEF was 4.82 mm (range, 3.3–5.2 mm) (Fig.3A, Line 1; Table 1).
Position of the PBEF Relative to the Mastoidand Styloid Processes
The temporal bone (os temporale) consists of five parts: thesquama (Squama temporalis), the petrous (Pars petrosa), the mas-toid (Pars mastoidea) and the tympanic (Pars tympanica) parts,and the styloid process (Processus styloideus). The mastoid part,whose air cells vary in number between individuals, projectsdownwards, forming the mastoid process. This projection ofthe temporal bone serves for the attachment of such muscles asSternocleidomastoideus, Splenius capitis, Longissimus capitis, andthe posterior belly of the digastric muscle (from superficial todeep). The occipital artery is located medial to the digastricmuscle. The average distance from the tip of the mastoidprocess to the PBEF is 5.31 mm (range, 3.1–7.9 mm) (Fig. 3A,Line 2; Table 1).
The styloid process constitutes a part of the hyoid systemand is a downward- and forward-pointed projection. This pro-vides attachment to three muscles (Stylohyoideus, Styloglossus,and Stylopharyngeus muscles) and two ligaments (the stylohy-oid and stylomandibular ligaments). There is a shallow groovebehind and slightly outside the styloid process, and the stylo-mastoid foramen can be found at the back. After its emergencefrom the stylomastoid foramen, the facial nerve has a down-ward and forward course through the styloid process.
Position of the PBEF Relative to the AtlasGiven the absence of a body and a spinous process, the
atlas (i.e., the first cervical vertebra) differs from the othercervical vertebrae. It consists of two lateral masses joined bothanteriorly and posteriorly by the anterior and posteriorarches, respectively. Two transverse processes are formedfrom the external aspect of these lateral masses, whose func-tion is to provide an attachment surface for powerful muscles.It is mainly by virtue of this condition that these transverseprocesses are relatively more developed here than in the othercervical vertebrae. The transverse foramen (foramen transver-sarium), which is found at the base of the atlantal transverseprocesses, provides a groove for the vertebral artery. Many
ONS-42 | VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 www.neurosurgery-online.com
CAMPERO AND SOCOLOVSKY
FIGURE 1. A–D, illustrations showing different hypoglossal-facial nervetransfer techniques. A, classical hypoglossal-facial nerve anastomosis. B,interposition sural nerve graft between the hypoglossal and facial nerves.C, longitudinal partial hypoglossal nerve dissection. D, facial nervedrilling at the mastoid process and facial nerve transposition to thehypoglossal nerve.
Position of the PBEF and CN XII Relative tothe Digastric Muscle
The digastric muscle, alsoknown as digastricus, is along muscle consisting oftwo bellies, an anterior and aposterior one, joined by anintermediate tendon. It has a downward and forwardc u r v e d c o u r s e f ro m t h emedial aspect of the mastoidprocess, within the mastoidnotch, to the lower border ofthe mandible body, withinthe digastric fossa, with ananteriorly and inferiorlyoblique direction. The supe-rior border of the digastricmuscle is parallel to thePBEF, and the average dis-tance between them is 4.86mm (range 2.3–6.4 mm) (Fig.3B, Line 5 and Fig. 4C; Table1). In its proximal course,the hypoglossal nerve (CNXII ) i s loca ted par t ia l lyunderneath the posteriorbelly of the digastric muscle.Distally, at the level of thedigastric muscle tendon, itturns anteriorly toward thetongue. At that level, theaverage distance betweenthe digastric muscle and the
hypoglossal nerve is 5.05 mm (range, 3.2–7 mm) (Fig. 3B,Line 6 and Fig. 4C; Table 1).
Facial Nerve (CN VII)
CN VII, also referred to as the facial nerve, is a mixed nerveconsisting of a main part (the facial nerve proper) and anaccessory part (nervus intermedius or pars intermedii of Wrisberg).From its apparent origin at the pontomedullary sulcus, itcourses laterally toward the internal auditory canal (IAC) (cis-ternal part). After exiting this canal (meatal part), it runsbetween the cochlea and the vestibule (labyrinthine part) andon the medial aspect of the tympanic cavity (tympanic part) toemerge from the skull through the mastoid process (mastoidpart). The average length of the mastoid facial nerve is 16.35mm (range, 15.2–18.6 mm) (Fig. 3B, Line 7; Table 1). It exits theskull through the stylomastoid foramen into the parotid gland.From the stylomastoid foramen to its bifurcation (PBEF), thefacial nerve has a deep to superficial and downward course.The average length of the PBEF is 18.93 mm (range, 16–20.6mm) (Fig. 3B, Line 8; Table 1). The average distance from the
NEUROSURGERY VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 | ONS-43
FACIAL REANIMATION BY MEANS OF THE HYPOGLOSSAL NERVE
A
1
2
3
4
12
3
4
B
C
muscles attach to the transverse processes, including thesuperior oblique and inferior oblique portions of the Longuscolli, Rectus capitis lateralis, Levator scapulae, and Splenius cervi-cis. The average distance from the lateralmost end of theatlantal transverse process to the PBEF is 15.85 mm (range,14.3–16.8 mm) (Fig. 3A, Line 3; Table 1).
Position of the PBEF Relative to the Mandible Condyle
The mandible, also known as inferior maxillary, consists oftwo parts: a body and two lateral ends or rami. The superiorends of the rami comprise two very large processes, an anteriorprocess known as the coronoid process, which serves as theattachment for the temporal muscle, and a posterior processknown as the mandible condyle. The condyle is an elipsoid emi-nence with a long axis obliquely directed medialward and back-ward. The mandible condyle and the glenoid fossa of the squa-mous temporal bone form the temporomandibular joint. Theaverage distance from the posterior border of the mandiblecondyle to the PBEF is 17.19 mm (range, 14.9–20.7 mm) (Fig. 3A,Line 4; Table 1).
FIGURE 2. A and B, auditory-mastoid polygon. Thispolygon is formed by four lines. 1, anterior vertical linerunning by the anterior border of the EAM cartilage. 2,posterior vertical line running by the tip of the mastoidprocess. 3, superior horizontal line, obliquely placedfrom anterior to posterior and superior to inferior, rep-resenting the lower end of the EAM cartilage and thetip of the mastoid process. 4, inferior horizontal line, 2cm below the inferior border of the EAM cartilage. C,right lateral view. The skin, subcutaneous tissues andpart of the temporal bone have been removed to exposethe facial and hypoglossal nerves. The auditory-mas-toid polygon is useful to locate the hypoglossal nerveimmediately proximal to the parotid gland, especiallywhen a preauricular approach is used for a classicalhypoglossal-facial nerve anastomosis. A., artery; Car.,carotid; CN, cranial nerve; Ext., external; Int., internal;Jug., jugular; M., muscle; Mand., mandibular.
skin to the PBEF, just below the EAM cartilage, is 21.16 mm(range, 14.3–27.7 mm) (Table 1).
We have drawn a polygon consisting of four lines (auditory-mastoid polygon). The first line is an anterior vertical line run-ning by the anterior border of the EAM cartilage. The secondline is a posterior vertical line running by the tip of the mastoidprocess. The third line, a superior horizontal line, obliquelyplaced from anterior to posterior and superior to inferior, rep-resents the lower end of the EAM cartilage and the tip of the
mastoid process. Thr fourth line is an inferior horizontal lineplaced 2 cm below the lower border of the EAM cartilage (Fig.2, A and B). In 100% of the facial nerves sampled in this study,the PBEF was found within this polygon.
Hypoglossal Nerve (CN XII)CN XII, also known as the hypoglossal nerve, is an exclu-
sively motor nerve supplying the tongue muscles. From thepreolivary sulcus, the hypoglossal nerve fascicles meet andcourse outwardly. Once out of the skull through the anteriorcondyle foramen (hypoglossal canal), CN XII has a forwardand downward oblique course. It runs posterior and thenmedial to the internal jugulary vein and lateral to the carotidartery (Fig. 2C). The extracranial course of the hypoglossalnerve is parallel to the course of the PBEF and the digastricmuscle. At the level of the digastric intermediate tendon, itturns anteriorly towards the tongue. The average distance fromthe bifurcation of the facial nerve to the place where thehypoglossal nerve turns towards the tongue is 31.56 mm(range, 27.6–35.8 mm) (Fig. 3B, Line 9; Table 1).
DISCUSSION
Hypoglossal-facial Nerve AnastomosisHypoglossal-facial nerve anastomosis is the most widely
used technique for facial nerve neurotization (11, 15, 16, 17,18, 22). It requires the complete section of the hypoglossal
ONS-44 | VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 www.neurosurgery-online.com
CAMPERO AND SOCOLOVSKY
FIGURE 3. A and B, right lateral view. 1, the distancefrom the EAM to CN VII. 2, the distance from the mas-toid process to CN VII. 3, the distance from the trans-verse process of the atlas to CN VII. 4, the distancefrom the mandible condyle to CN VII. 5, the distancefrom the digastric muscle to CN VII. 6, the distancefrom the digastric muscle to CN VII. 7, the length of themastoid portion of CN VII. 8, the distance from thestylomastoid for amen to the CN VII bifurcation. 9, thedistance from CN VII to CN XII.
A
B
TABLE 1. Measurements of the extracranial portion of CranialNerve VIIa
MeasurementsAverage Range
(mm) (mm)
Distance from the EAM to CN VIIb 4.82 3.3–5.2
Distance from the mastoid 5.31 3.1–7.9
process to CN VIIb
Distance from the atlas to CN VIIb 15.85 14.3–16.8
Distance from the mandibular 17.19 14.9–20.7
condyle to CN VIIb
Distance from the digastric 4.86 2.3–6.4
muscle to CN VIIc
Distance from the digastric 5.05 3.2–7.0
muscle to CN XIIc
Length of the mastoid portion of CN VIIc 16.35 15.2–18.6
Distance from the EMF to the 18.93 16.0–20.6
CN VII bifurcationc
Distance from CN VII to CN XIIc 31.56 27.6–35.8
Distance from the skin to CN VII 21.16 14.3–27.7
a EAM, external auditiory meatus; CN, cranial nerve; EMF, estylomastoid foramen.b See Figure 2A.c See Figure 2B.
tongue atrophy is a directconsequence of hypoglossaln e r v e s e c t i o n ( F i g . 7 E ) .Immediately after surgery,patients find difficulty inproducing sounds such as“d” or “r,” but with appro-priate speech therapy reha-bilitation, this situation canbe controlled within 2 to 3months. In addition, swal-l o w i n g , e s p e c i a l l y f o o dmanipulation in the mouth,is affected in the immediatepostoperative period; how-ever, most patients get usedto this and quickly learn tocope with the difficulty. Inmost cases, patients felt com-fortable with the sacrificeimplied by the denervatedhemiglossal to obtain facialreanimation, and all of themexpressed that they wouldundergo the procedure againif required (11, 16, 17, 18, 22).
As far as the results of theprocedure are concerned, 564hypoglossal-facial nerveanastomoses were performedbetween 1954 and 1992, asrecorded in the literature.According to Pitty and Tator(16), positive results accountfor approximately 65% of the
cases, whereas 22% showedpoor results and 13% had acomplete lack of reinnerva-tion. More importantly, spe-cialized literature shows totalconsensus (11, 15, 16, 17) re-garding the maximum intervalbetween resection and anasto-mosis procedures , whichshould not exceed 1 year.
Longer intervals are associated with significant atrophy of thefine mimetic muscles, as they are histologically replaced by fattissue after 2 years. Beyond that period, the rate of success ofany kind of facial reanimation by neurotization is significantlyhindered.
Furthermore, according to the literature, specialists agreethat hemiglossal atrophy is not reduced by joining the ansahypoglossi to the distal stump of the hypoglossal nerve, as sug-gested by Kempe (9). This technical variant, widely advocatedin the 1960s and 1970s, has been practically abandoned becauseof the lack of good results (16).
nerve, resulting in hemiglossal atrophy. With appropriatetraining in the rehabilitation period, a conscious use of thosemuscles may be regained (7), but reflex gestures, such asemotions, cannot be recovered. When this is the case, eyelidand mouth closure become appropriate, and facial symmetryand voluntary function of the compromised side of the faceare restored; however, mobility of each separate muscle ispoor and facial hypertonicity can sometimes occur (16) (Fig.7, C and D).
Disorders produced by hemiglossal denervation tend totranslate into speech and swallowing difficulties. Severe
NEUROSURGERY VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 | ONS-45
FACIAL REANIMATION BY MEANS OF THE HYPOGLOSSAL NERVE
FIGURE 4. A–D, right-sided classical hypoglossal-facial nerve anastomosis. A, skin incision. The incision beginsbefore the tragus, skirts the earlobe, and follows the anterior border of the sternocleidomastoid muscle, ending at thelevel of the mandibular angle. B, the superficial planes have been dissected, exposing the parotid gland, the sternoclei-domastoid muscle and superficial vessels and nerves. The facial nerve should be searched for within the parotid glandusing the auditory-mastoid polygon (as reference). C, deeper planes have been dissected, exposing the facial andhypoglossal nerves. The digastric muscle is found between the facial nerve and the turn where the hypoglossal nervechanges its course. D, the hypoglossal-facial nerve anastomosis has been carried out. The hypoglossal nerve has beentransferred in the search for the facial nerve underneath the digastric muscle. Auric., auricular; CN, cranial nerve;Ext., external; Gr., greater; Int., internal; Jug., jugular; M., muscle; N., nerve; V., vein.
A B
C D
Anatomic Considerations Regardingthe Classical Technique
For the classical technique, in which CN XII is redirectedcranially to CN VII, enough release of CN XII is required toreach the facial nerve and perform a tensionless anastomosis atthe suture site. The facial nerve can be found at the level of thestylomastoid foramen, where it exits the skull, or more distallyif a preauricular approach is used. In this article, all measure-ments and procedures regarding the classical hypoglossal-facial nerve anastomosis are based on a preauricular approachrather than on an incision over the mastoid process. With thislatter approach, the distance between the anastomosis and thetarget organ is longer. In order to simplify the facial nerve dis-section proximal to the parotid gland, this article describes the
auditory-mastoid polygon,where the PBEF is found in100% of cases.
More than half of the distancebetween both nerves is requiredfor a tensionless suture, assum-ing that the whole sectionedlength of the hypoglossal nervewill be moved toward the facialnerve. Thus, the hypoglossalnerve should cover approxi-mately 60% of this distance atleast, so the stump of CN XII canreach CN VII without tension.The average distance from thebifurcation of the facial nerve towhere the hypoglossal nerveturns and becomes horizontal is31.56 mm (range, 27.6–35.8 mm)according to our measurements.Consequently, approximately 19mm of the hypoglossal nerve isrequired because it turns, whichimplies that the ansa hypoglossishould be sectioned to performa major nerve trunk transposi-tion. In our specimens, the ansahypoglossi was found distal tohalf the distance between CNsVII and XII.
Classical Hypoglossal-facialAnastomosis:Technical Variants
Various new techniques havebeen described over the pastdecade in an attempt to mini-mize the most severe morbidi-ties after hypoglossal-facialnerve anastomosis. Sequelae ofthis procedure include the
swallowing and speech disorders described previously, whichare secondary to hypoglossal nerve section.
Asaoka et al. (3) established that the number of axons in anormal hypoglossal nerve (9778 � 1516) (11) exceeds the axonscontained in a normal facial nerve (7228 � 950), and that thecross-sectioned area of the normal facial nerve (0.948 mm2)accounted for 61.5% of the area of the hypoglossal nerve (1.541mm2), whereas that of the injured facial nerve (0.66 mm2) wasless than 50% of the area of the hypoglossal nerve. Accordingly,in theory, sectioning only part of the hypoglossal nerve, ratherthan its entire diameter, should be enough to achieve goodfacial reinnervation. This procedure could also reduce the post-operative occurrence of severe synkinesis (2).
If the hypoglossal nerve is partially sectioned, however, itcannot be moved towards the facial nerve distal stump to per-
ONS-46 | VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 www.neurosurgery-online.com
CAMPERO AND SOCOLOVSKY
FIGURE 5. A–D, right-sided hypoglossal-facial nerve anastomosis with interposition jump graft. A, this techniqueuses an incision similar to the classical technique. B, superficial and deeper planes have been dissected, exposingthe facial and hypoglossal nerves. C, the graft has been sutured to the facial nerve superiorly and to the superiorhalf of the hypoglossal nerve inferiorly. The donor nerve should be longer than 31.56 mm. D, magnified view of thesuture. CN, cranial nerve; Int., internal; Jug., jugular; M., muscle; V., vein.
A B
C D
form the anastomosis, as is the case of the classical technique.Many different methods have been applied to overcome thisproblem, including intratemporal transposition of the facialnerve or graft interposition.
May et al. (14), who describe the use of a graft between thefacial nerve and the partially sectioned hypoglossal nerve (Figs.1B, 4, and 6), have observed only three cases of hemiglossalatrophy among the 20 samples they have analyzed. The effec-tiveness of this technique has been questioned as a result of thefact that the donor axons have to move along a path and tocourse through two unions and the whole length of the graft. Inother words, the success rate of midface reanimation is uncer-
tain (7). Manni et al. (13) andGuntinas-Lichius et al. (8),however, report extensiveexperience with this tech-nique with results similar tothe ones obtained with theclassical technique. Cusimano(6) published a case reportpresenting similar results,although with no interposi-tion jump graft. Our anatomicstudy, however, suggests thatCusimano’s technique isextremely difficult to performb e c a u s e o f t h e d i s t a n c ebetween both nerves, whichprecludes good nerve coapta-tion without tension.
Arai et al. (1) introducedsome changes to the proce-dure: they dissected thehypoglossal nerve longitudi-nally to later perform theanastomosis with the facialnerve, thereby avoiding theuse of an interposition jumpgraft (Fig. 1C). This techniquehas also been questionedthroughout the specialized lit-erature (7) because any longi-tudinal fascicle nerve dissec-tion, regardless of whetherthe nerve is monofascicular asis the case of the hypoglossalnerve, injures a certain num-ber of axons owing to the factthat they have a plexal struc-ture and intercross along thecourse of the nerve (24).
Sawamura and Abe (19)suggest the drilling of thefacial nerve at the Fallopiancanal up to the stapedialnerve. This technique pro-
vides some further centimeters of facial nerve, which is sec-tioned and rotated to be anastomosed with the partially sec-tioned hypoglossal nerve (Figs. 1D, 5, and 8). Sawamura andAbe report a series of four patients whose facial paralysis pro-gression is longer than 2 years. Positive outcomes correspondto three cases, especially regarding facial symmetry at rest.Atlas and Lowinger (4) report three cases of intratemporalfacial nerve transposition using a similar technique, with func-tion recovery in all cases and a dramatic reduction of the onlypartial hemiglossal weakness.
Petrous bone drilling, although involving a more complextechnique and a longer operative time, would apparently pre-
NEUROSURGERY VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 | ONS-47
FACIAL REANIMATION BY MEANS OF THE HYPOGLOSSAL NERVE
FIGURE 6. A–D, right-sided hypoglossal-facial nerve anastomosis with mastoid process drilling. A, the parotid andmastoid regions have been dissected, exposing the mastoid process and the facial and hypoglossal nerves. B, the mas-toid process has been drilled, with the supramastoid crest as upper limit. The whole mastoid facial nerve has beenexposed, avoiding the need of entering or breaking the semicircular canals. C, the facial nerve has been sectioned at thebeginning of the mastoid portion and then moved towards the hypoglossal nerve. The superior half-diameter of thehypoglossal nerve has been sectioned. Thus, the free stump of the facial nerve has been sutured to the superior portionof the hypoglossal nerve. D, magnified view of the suture. A., artery; Car., carotid; CN, cranial nerve; Int., internal;Jug., jugular; M., muscle; Prox., proximal; Seg., segment; V., vein.
A B
C D
serve a greater degree of tongue function without compromis-ing the quality of the axons received by the facial nerve.Therefore, on the basis of both theory and the limited experi-ence reported throughout the specialized literature, and inaccordance with our own experience with six cases (21) (Fig. 8),the classical hypoglossal-facial nerve anastomosis is likely to bereplaced with this promising technique.
Anatomic Queries Regarding Variantsto the Classical Technique
Interposition Jump Graft TechniqueGiven the results of our cadaver study, the distance between
CNs VII and XII is 31.56 mm. Consequently, a sural nerve graft ofthat length will be required for a tensionless anastomosis at theborders of the suture. Since the graft tends to retract after harvest-
ing, it should be at least 25% longer than the distance betweenboth stumps; as a result, the graft should be at least 35 mm longon average. As we see it, the case reported by Cusimano andSekhar (6) proves difficult to perform in most patients because,according to our study, the distance between both nerves is suf-ficiently long to preclude a direct graftless reapproximation,unless a long enough longitudinal dissection CN XII is carriedout, thereby leading to the technique described below.
Hypoglossal Nerve Longitudinal DissectionThe principle considered in the previous technique should be
applied for this one. A portion of the hypoglossal nerve is lon-gitudinally dissected. The minimal length of nerve to bereleased is the distance between CNs VII and XII (i.e., an aver-age of 31.56 mm) plus some additional millimeters to performa tensionless reapproximation.
ONS-48 | VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 www.neurosurgery-online.com
CAMPERO AND SOCOLOVSKY
FIGURE 8. A–B, a 52-year-old woman with a huge cerebellopontinetumor (meningioma) presented with a complete facial paralysis aftertumor resection. The patient was offered different alternatives as facialreinnervation in the postoperative period and decided to undergo afacial drilling surgery at the petrous bone in order to reduce postoper-ative tongue morbidity. C–D, 6 months after the procedure, facial sym-metry and eye closure were regained. E–F, observe the complete tonguefunction preservation after this procedure. The only tongue morbiditywas a slight movement weakness, referred by the patient as “clumsi-ness,” but the symptoms were completely resolved in 3 weeks.
A B
C D
E F
FIGURE 7. A–B, complete facialparalysis in a 38-year-old manafter cerebellopontine angle tumorresection. Three months after thatsurgery, a classical hypoglossal-facial nerve anastomosis was per-formed. C–D, 1 year after the pro-cedure, facial symmetry and eyeclosure were regained. E, completepostoperative tongue hemiatrophysecondary to hypoglossal nervesection is observed.
A B
C D
E
Facial Nerve Drilling at the Temporal BoneFor drilling the mastoid process, the whole length of the
mastoid CN VII, measuring 16.35 mm, should be released. Ifthe distance from the stylomastoid foramen to the CN VIIbifurcation, measuring 18.93 mm, is added to that figure, a totallength of 35.28 mm is obtained. This length is longer than thedistance between CNs VII and XII (31.56 mm), and it should beenough for a tensionless nerve anastomosis.
CONCLUSION
Our study describes the hypoglossal-facial nerve anastomo-sis, includes a literature review of the results achieved withthis technique, and explains several of the variants introducedin recent years. It also describes the anatomic parameters andthe length of the hypoglossal nerve sectioning that may stan-dardize the site where the common trunk of the facial nerve atthe infraauricular level should be identified and illustrates theprocess by means of two cases. By virtue of this study, it ispossible to precisely establish the type of graft, the dissectionwithin the hypoglossal nerve, and the extent of mastoid drillingrequired for a nerve transfer from the facial to the hypoglossalnerve in any of the classical technique variants described,whose aim is to achieve better tongue function. Future con-trolled clinical trials will determine which of those variants canoffer the best outcome with less morbidity compared with the“gold standard,” which continues to be the classical hypoglos-sal-facial nerve anastomosis.
REFERENCES1. Arai H, Sato K, Yanai A: Hemihypoglossal-facial nerve anastomosis in treat-
ing unilateral facial palsy after acoustic neurinoma resection. J Neurosurg82:51–54, 1995.
2. Asaoka K, Sawamura Y: Hypoglossal-facial nerve side-to-end anastomosis.J Neurosurg 91:163–164, 1999 (letter).
3. Asaoka K, Sawamura Y, Nagashima M, Fukushima T: Surgical anatomy fordirect hypoglossal-facial nerve side-to-end “anastomosis.” J Neurosurg91:268–275, 1999.
4. Atlas MD, Lowinger DS: A new technique for hypoglossal-facial nerve repair.Laryngoscope 107:984–991, 1997.
5. Deleted in proof.6. Cusimano MD, Sekhar LN: Partial hypoglossal to facial nerve anastomosis for
reinnervation of the paralyzed face in patients with lower cranial nervepalsies: Technical note. Neurosurgery 35:532–534, 1994.
7. Fernandez E, Pallini R, Palma P, Lauretti L: Hypoglossal-facial nerve anasto-mosis. J Neurosurg 87:649–650, 1997 (comment).
8. Guntinas-Lichius O, Streppel M, Stenert E: Postoperative functional evalua-tion of different reanimation techniques for facial nerve repair. Am J Surg191:61–67, 2006.
9. Kempe L: Operative Neurosurgery. New York, Springer Verlag, 1970, vol 2.,pp 233–239.
10. Korte W: A case of nerve transfer from the facial nerve to the hypoglossalnerve. Dtsch Med Wochenschr 29:293, 1903.
11. Linnet J, Madsen FF: Hypoglosso-facial nerve anastomosis. Acta Neurochir133:112–115, 1995.
12. Love JG, Cannon BW: Nerve anastomosis in the treatment of facial paralysis.Special consideration of the etiologic role of total removal of tumors of theacoustic nerve. Arch Surg 62:379–390, 1951.
13. Manni JJ, Beurskens C, van de Velde C, Stokroos RJ: Reanimation of the par-alyzed face by indirect hypoglossal-facial nerve anastomosis. Am J Surg182:268–273, 2001.
14. May M, Sobol SM, Mester SJ: Hypoglossal-facial nerve interpositional-jumpgraft for facial reanimation without tongue atrophy. Otolaryngol Head NeckSurg 104:818–825, 1991.
15. Pellat JL, Bonnefille E, Zanaret M, Cannoni M: Hypoglossal-facial anastomo-sis. A report of 60 cases. An Chir Plast Esteth 42:37–43, 1997.
16. Pitty LF, Tator CH: Hypoglossal-facial nerve anastomosis for facial nervepalsy following surgery for cerebellopontine angle tumors. J Neurosurg77:724–731, 1992.
17. Rosenwasser RH, Liebman E, Jimenez DF, Buchheit WA, Andrews DW: Facialreanimation after facial nerve injury. Neurosurgery 29:568–574, 1991.
18. Samii M, Matthies C: Indication, technique and results of facial nerve recon-struction. Acta Neurochir 130:125–139, 1994.
19. Sawamura Y, Abe H: Hypoglossal-facial nerve side-to-end anastomosis forpreservation of hypoglossal function: Results of delayed treatment with anew technique. J Neurosurg 86:203–206, 1997.
20. Shah SB, Jackler RK: Facial nerve surgery in the 19th and early 20th cen-turies: The evolution from crossover anastomosis to direct nerve repair. AmJ Otol 19:236–245, 1998.
21. Socolovsky M: Modern concepts in peripheral nerve surgery. Part II: Facialreanimation techniques. Rev Arg Neurocir 18:85–93, 2004.
22. Sood S, Anthony R, Homer JJ, Van Hille P, Fenwick JD: Hypoglossal-facialnerve anastomosis: Assessment of clinical results and patient benefit for facialnerve palsy following acoustic neuroma excision. Clin Otolaryngol25:219–226, 2000.
23. Spector JG: Neural repair in facial paralysis: Clinical and experimental stud-ies. Eur Arch Otorhinolaryngol 254 [Suppl 1]:S68–S75, 1997.
24. Sunderland S: Nerve and Nerve Injuries. New York, Churchill-Livingstone,1979, ed 2, pp 134–136.
25. Terzis JK: “Babysitters”: An exciting new concept in facial reanimation, inCastro D (ed): Proceedings of the Sixth International Symposium on the FacialNerve. Rio de Janeiro, Kygler and Ghedini Publications, 1988, p 525.
26. Terzis JK, Noah ME: Analysis of 100 cases of free-muscle transplantation forfacial paralysis. Plast Reconstr Surg 101:554–555, 1997.
27. Yoleri L, Songur E, Mavioglu H, Yoleri O: Cross-facial nerve grafting as anadjunct to hypoglossal-facial nerve crossover in reanimation of early facialparalysis: clinical and electrophysiological evaluation. Ann Plast Surg46:301–307, 2001.
COMMENTS
In this study, the authors nicely illustrate the different techniques ofhypoglossal to facial transfer by anatomic dissections. Fortunately,
the number of patients needing this technique is now very low becauseof better facial nerve preservation after acoustic neuroma surgery,radiosurgery for a number of acoustic neuromas, and the improvedtechniques of direct facial nerve repair.
When needed, I prefer to get as long a facial nerve as possible bymobilizing the mastoid segment of the nerve, and then suturing it tohalf of the hypoglossal nerve split for a very short length. I do not pre-fer to split the hypoglossal nerve over a long distance because many ofthe fascicles could be disrupted.
When the facial nerve starts to show recovery, the patient can begiven specific mimic exercises to improve the functional recovery, ashas been shown by Nedzelski at the University of Toronto (J Nedzelski,personal communication, 1998).
Laligam N. SekharSeattle, Washington
This is an excellent demonstration of the relevant anatomy for perform-ing any of the facial reanimation techniques that involve anastomosis
with the hypoglossal nerve. One of the key points in my experienceinvolves the length of hypoglossal nerve that is required to reach thestump of the facial nerve at the pes anserinus. The hypoglossal nervemust be dissected far anterior in this circumstance, as discussed in thisarticle. This article should serve as solid preparation for those faced with
NEUROSURGERY VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 | ONS-49
FACIAL REANIMATION BY MEANS OF THE HYPOGLOSSAL NERVE
performing this procedure. Knowledge and some experience with thespecific techniques of microanatomosis of peripheral nerves are equallyimportant components to obtain before performing in the operating room.
The patients presented provide illustrations of the best expectationsof these techniques. However, we must remember that these representthe absolute best that can be hoped for by the patient and surgeon.Historically speaking, less than half of these patients will realize sucha nice result. In general, the failure rate is 50% in terms of any func-tional return. Of those who do gain some improvement, only half ofthose will reach a House-Brackmann Grade 3 result, with eye closureand muscular tone. These realities must be kept in mind when counsel-ing patients before commencement of such a procedure.
J. Diaz DaySan Antonio, Texas
This is a very nice anatomic presentation that also reviews the vari-ous types if Cranial Nerve XII–VII anatamoses in use. The points
are made very well, with good examples. The discussions of the prob-lems and results that are encountered with the different techniques arewell done. I believe this will be an asset to practicing neurosurgeonswho encounter interruption of the VIIth nerve without the ability of adirect anastamosis or interposition graft.
There is a tendency to discount the disability of tongue hemiatro-phy when compared with facial dysfunction. The hypoglossal splitwith a facial nerve mobilization procedure may avoid that deficit. Italso minimizes the need for an interposition graft with two anasta-moses to traverse.
When there is a complete VIIth nerve section and a lack of a proxi-mal stump for performing a direct repair or interposition graft, I likethis technique.
Kalmon D. PostNew York, New York
Reanimation of a permanently injured facial nerve when the proxi-mal stump is unavailable is most commonly performed using a
hypoglossal-facial nerve anastomosis or one of its variations. In partic-ular, the hypoglossal to facial cranial nerve jump graft, in which half ofthe hypoglossal nerve is joined to the extracranial facial nerve by asingle cable nerve graft, has become the procedure of choice for mostsurgeons, given that improved facial and maintained hypoglossalnerve function have been reported in several studies (1, 2).
In this study, the authors perform a cadaveric analysis (with fivecadavers analyzed bilaterally) of the microanatomic relationshipsbetween the facial and hypoglossal nerves, and measure the distancesbetween the prebifurcation extracranial facial nerve and various rele-vant surrounding structures. They conclude that 1) 19 mm of thehypoglossal is required for a classic anastomosis, 2) longitudinal dissec-tion requires approximately 31.5 mm of nerve, 3) a 35-mm-long graft isrequired for the jump-graft technique, and 4) approximately 16.3 mmof facial nerve can be exposed by drilling the mastoid process.Furthermore, descriptions of the classic hypoglossal-facial nerve anas-tomosis and interposition jump-graft technique are included, as are apartial literature review of technical variations and results. Finally, theauthors illustrate two representative cases in which these anastomotictechniques were used.
The cadaveric measurements of various facial nerve relationships (assummarized in Table 1) represent an original contribution to the neuro-surgical literature on facial hypoglossal anastomosis. Along with thereview of regional microanatomy, readers will find the description ofthese interrelationships (along with the corresponding figures) of gen-eral interest. Specifically, the authors’ description of the auditory mas-
toid quadrilateral space for locating the hypoglossal and facial nervesthrough a pre-auricular approach is particularly noteworthy. The mas-toid drilling technique for mobilizing the proximal facial nerve andallowing direct coaption (without need for intervening nerve graft) tothe superior half of the hypoglossal nerve is well illustrated. One case(Fig. 8) highlights the clinical outcome of the latter technique with sat-isfactory facial function and no significant tongue-muscle dysfunction.By contrast, another case (Fig. 7) illustrates the striking tongue atrophythat is attributable to taking the entire hypoglossal nerve.
I like this technique, especially because it provides a means of per-forming a tension-free repair without the need for an intervening nervegraft. The importance of avoiding tension for nerve repair (8) with theliberal use if nerve grafts as appropriate (7) is well established (6).However, the avoidance of a nerve graft ensures that regeneratingaxons only have to cross one and not two suture lines, so that axonalloss and misdirection are minimized (3, 4). With other transfer tech-niques, such as the intercostal to musculocutaneous, the series withdirect repairs demonstrate improved functional outcome (5) as com-pared with those where interpositional grafts are placed. We hope theseauthors will similarly collect and publish a larger series in the future todocument the clinical outcome from the innovative technical variationdescribed in this article.
Rajiv MidhaCalgary, Canada
1. Arai H, Sato K, Yanai A: Hemihypoglossal-facial nerve anastomosis in treatingunilateral facial palsy after acoustic neurinoma resection. J Neurosurg82:51–54, 1995.
2. Cusimano MD, Sekhar L: Partial hypoglossal to facial nerve anastomosis forreinnervation of the paralyzed face in patients with lower cranial nerve palsies:Technical note. Neurosurgery 35:532–533, 1994.
3. Hudson AR, Hunter D, Kline DG, Bratton BR: Histological studies of experi-mental interfascicular graft repairs. J Neurosurg 51:333–340, 1979.
4. Kim DH, Connolly SE, Voorhies RM, Beuerman RW, Kline DG: Initial evalua-tion of variable graft lengths and lesion lengths in the repair of nerve gaps.J Reconstr Microsurg 6:311–316, 1990.
5. Malessy MJ, Thomeer RT: Evaluation of intercostal to musculocutaneous nervetransfer in reconstructive brachial plexus surgery. J Neurosurg 88:266–271, 1998.
6. Matsuyama T, Mackay M, Midha R: Peripheral nerve repair and grafting tech-niques: A review. Neurol Med Chir (Tokyo) 40:187–199, 2000.
7. Millesi H, Meissl G, Berger A: The interfasicular nerve-grafting of the medianand ulnar nerves. J Bone Joint Surg Am 54:727–750, 1972.
8. Miyamoto Y: Experimental study of results of nerve suture under tension vs.nerve grafting. Plast Reconstr Surg 64:540–549, 1979.
This article describes the anatomic relationship between the relevantstructures encountered during extracranial facial nerve repair.
Cadaver dissections and caliper measurements provide the study data,and two illustrative cases are provided to clarify the clinical points. Thetechniques of 1) hypoglossal-facial direct anastomosis, 2) hypoglossal-facial end-to-side anastomosis with interposition grafting, 3) partialhypoglossal-facial direct anastomosis with longitudinal dissection, and4) hypoglossal-facial end-to-side anastomosis with temporal bonedrilling are well illustrated, adequately described, and well referenced.The anatomic data presented will be useful for those performing thesetypes of procedures. Specifically, the lengths of nerve that need to bedissected to permit tension-free anastomosis, which is crucial for suchrepairs to work, are described. The authors correctly point out thatonly a randomized comparison trial will establish the superiority ofone approach over the others.
Christopher J. WinfreeJeffrey N. BruceNew York, New York
ONS-50 | VOLUME 61 | OPERATIVE NEUROSURGERY 1 | SEPTEMBER 2007 www.neurosurgery-online.com
CAMPERO AND SOCOLOVSKY