Barrett’s Esophagus: Review of Diagnostic Issues …€™s Esophagus: Review of Diagnostic Issues...
Transcript of Barrett’s Esophagus: Review of Diagnostic Issues …€™s Esophagus: Review of Diagnostic Issues...
Barrett’s Esophagus: Review of Diagnostic Issues and Pre-
Neoplastic Lesions
Robert Odze, MD, FRCPCChief, Gastrointestinal PathologyAssociate Professor of PathologyBrigham and Women’s Hospital
Harvard Medical SchoolBoston, MA
Barrett’s Esophagus:Metaplasia and Dysplasia
• Metaplasia - Def’n/types- Pathogenesis- Differential Diagnosis
• Dysplasia - Incidence/risk factors- Pathologic features- Adjunctive Diagnostic tests- Natural History- Treatment
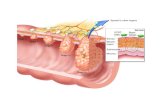
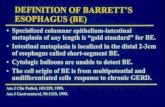
Barrett’s EsophagusDefinition
• Columnar metaplasia of esophageal squamous epithelium (any length)
• Recognized at endoscopy• Goblet cell metaplasia
Barrett’s EsophagusGross Types
• Long segment (>3cm)• Short segment (1-3cm)• Ultrashort segment (0-1cm)
Barrett’s EsophagusEpithelial Types
• Intestinal (“specialized”) type (99%>2cm)
• Cardia type (“junctional”)• Fundic type
Short (Ultrashort ) BE vs. Chronic Carditis
• Distinction important• Different clinical, etiologic,
pathologic, outcome, risk of malignancy
Summary of Factors That Impede the Ability to Separate the True Gastric Cardia from the Distal Esophagus at Endoscopy
__________________________________________________________________________
Hiatal Hernia (which causes obliteration of the proximal gastric folds)Irregular Z line
Erosions in Distal Esophagus (which mimicks BE)Respiratory Movements
Sampling ErrorSimilar Histology
__________________________________________________________________________
Table 1. Frequency of significant morphologic parameters in biopsies from patients with BE or CIM
_______________________________________________________________________________________________Disease Squamous Crypt Crypt Incomplete Diffuse IM HG MEP EG/EDCategory over IM Disarray Atrophy IM (>50%)_______________________________________________________________________________________________
BE 8/14 17/20 12/20 20/20 12/20 8/20 14/20 6/20(%) 57 85 60 100 60 40 70 30
CIM 0/7 10/20 5/20 10/20 2/20 0/20 3/20 0/20(%) 0 50 25 50 10 0 15 0
P value 0.01 0.04 0.05 <0.001 0.02 0.01 0.03 0.02_______________________________________________________________________________________________
BE: Barrett’s esophagus; CIM: carditis with intestinal metaplasia; IM: intestinal metaplasia; MEP: Multilayered epithelium; HG: Hybrid glands; EG/ED: esophageal glands/ducts
Mucin Histochemistry
______________________________________________________Stain Esoph Cardia
Goblet Non-Goblet Goblet Non-Goblet______________________________________________________Alcian blue + + + +(acid mucin
High Iron diamine + + + -(sulphomucin) _____________________________________________________
Multilayered Epithelium
1. Hybrid epithelium (squam/colum)- EM, cytokeratins
2. Biologically active3. Phenotypically similar to Barrett’s
Esophagus4. Highly associated with Barrett’s
esophagus and GERD
Esophageal versus Cardia Intestinal Metaplasia__________________________________________
Feature Esophagus IM Cardia IM(BE)
___________________________________________________________1. GERD clinical profile + -2. Irregular Z line + -3. Esophagitis (histologic) + -4. Gastritis (histologic) - +5. H. Pylori - +6. Eosinophils ++ +7. Neut, Plasma, Lymphocytes + ++8. Multilayered epithelium + -9. HID stain positive + -10. MUC 1, 6 positive + -11. BE CK 7/20 pattern + +/-12. Complete > incomplete IM - +__________________________________________________________
Barrett’s EsophagusDysplasia: Definition
• “Neoplastic epithelium that remains confined within the basement membrane”
• not reactive• not synonymous with “atypical”• unlikely to spontaneously regress
• Both a marker and a precursor of adenocarcinoma
Barrett’s Dysplasia/CarcinomaRisk
Prevalence : 6-8%
Incidence : 0.2 – 3% (1/52 – 1/208 patient years)
Relative Risk: 30-125x
Incidence Rate of Adenocarcinoma in Barrett’s Esophagus
__________________________________________________________________Incidence Follow-up
Series Patients Cases (Patient Incidence(No.) (No) Years) Rate
__________________________________________________________________Haammeeteman et al 50 5 260 1/52Bonelli et al 71 2 110 1/55Roberston et al 56 4 224 1/56Miros et al 81 3 289 1/96Iftikhar et al 107 4 462 1/115Drewitz et al 170 4 834 1/208O’Connor et al 136 2 570 1/285Sepchler et al 108 4 1037 1/259Sharma et al 618 12 2546 1/212_________________________________________________________________
Barrett’s Dysplasia/CarcinomaRisk Factors
Length of BESeverity of RefluxHiatus Hernia size
GenderEthnicity
AgeSmoking?Alcohol?
Patient Characteristics__________________________________________________________________Variable GERD Barrett’s HGD/CA
(N=2170) (N=1189) (N=131)__________________________________________________________________Male sex 98% 99% 99%Age (yr*) 59+13 61+11 63+10White ethnicity 76% 83% 89%Ethanol Consumption 40% 37% 42%Smoking 34% 25% 27%Hiatal hernia 24% 65% 84%Hiatal hernia size (cm*) 0.4+1.1 2.4+1.9 3.5+2.3Barrett’s length (cm*) 2.6+2.1 5.0+4.4__________________________________________________________________
Avidan et al. Am J Gastroenterol2002;97(8) 1930-1936
DysplasiaPathologic Features
1. Gross - Flat- Elevated (plaque, nodule, polyp)
2. Microscopic - Adenoma-like- Non-adenoma like
Dysplasia in the GI Tract
NegativeIndefinite
Positive (low, high)Intramucosal AdenoCa
Submucosal (Invasive) AdenoCa
Vienna System and Dysplasia Morphology Study GroupClassification of Dysplasia in IBD
_________________________________________________________________
Vienna DMSG_________________________________________________________________
1. Negative for neoplasia/dysplasia Negative for dysplasia2. Indefinite for neoplasia/dysplasia Indefinite for dysplasia3. Non-invasive low-grade neoplasia Low-grade dysplasia
(low-grade adenoma/dysplasia)4. Non-invasive high-grade neoplasia High-grade dysplasia
4.1 High-grade adenoma/dysplasia4.2 Non-invasive carcinoma
(carcinoma in situ)4.3 Suspicious of invasive carcinoma
5. Invasive Neoplasia Adenocarcinoma*5.1 Intramucosal Adenocarcinoma Intramucosal5.2 Submucosal carcinoma or beyond Invasive
__________________________________________________________________*not described by DMSG
Crypt Dysplasia with surface maturation. A clinical,
pathologic and molecular study of a Barrett’s Cohort
L. Lomo, P. Blount, R. Sanchez, P. Galipeau, D. Cowan, D. Ayub, P. Rabinovitch, B. Reid, R. Odze
Am J Surg Pathol (In Press)
Pathologic Features of the Study Cohort1983-2003 (N=206)
_________________________________________________________
Feature BCDA Controls (N=15) (N=191) p value
_________________________________________________________
Maximum diagnosisAssociated neoplasia (total) 13/15 (87%) 112/191 (59%) 0.052Low-grade dysplasia 2/15 (13%) 70/191 (37%) 0.09High-grade dysplasia 8/15 (53%) 35/191 (18%) 0.004Adenocarcinoma 3/15 (20%) 7/191 (4%) 0.03
_________________________________________________________________________________________________
Summary of Molecular Biomarkers of the
Study Cohort______________________________________________________________________
Feature BCDA Controls (N=15) (N=191) p value
______________________________________________________________________
> 1 Molecular abnormality 12/15 (80%) 100/191 (52%) 0.057
9p LOH 8/9 (89%) 67/116 (58%) 0.0817p LOH 4/9 (44%) 12/116 (10%) 0.016?4N 2/15 (13%) 11/191 (5.8%) 0.24Aneuploidy 5/15 (33%) 12/191 (6.3%) 0.004Any flow abnormality 6/15 (40%) 15/191 (7.9%) 0.001
______________________________________________________________________
Barrett’s Esophagus_________________________Feature Regeneration Dysplasia__________________________________________
Inflammation ++ +/-Ulceration ++ +/-Surface Maturation + -Pleomorphism - +/-Loss of Polarity - +/-Atypical Mitoses - +/-Surface Proliferation +/- ++Villiform Change +- +/-Mucin Depletion +/- ++__________________________________________
Barrett’s-related DysplasiaInterobserver Agreement__________________________________________
Category % agreement__________________________________________HGD + IMC vs. others 85-87%Negative vs. others 71-72%Negative + Ind vs. others 75-77%Neg vs. Ind/LGD vs. HGD/IMC 58-61%__________________________________________
Reid BJ et al. Hum Pathol 1988
Barrett’s-related DysplasiaInterobserver Variation
__________________________________________Category Set 1 Set 2__________________________________________No dysplasia 0.44 (mod) 0.58Indefinite 0.13 (slight) 0.15Low grade 0/23 (fair) 0.31High grade/cancer 0.63 (substantial) 0.64__________________________________________
Montgomery EA et al. Hum Pathol 2001
Adjunctive TechniquesProliferation Markers
DNA content (aneuploidy)Telomerase
Genetic mutations (p53, p16, Kras, APC, B catenin)
Growth FactorsApoptosis InhibitorsCyclooxygenase 2
AMACR Immunostaining is Useful in Detecting Dysplastic Epithelium in BE, UC and CD
R Dorer, J Glickman, RD OdzeAm J Surg Pathol (In Press)
Dorer et alResults__________________________________________
AMACR PositiveDysplasia BE UC/CD__________________________________________
Negative 0% 0%Indefinite 21% 14%Low Grade 38% 96%High Grade 81% 80%AdenoCa 72% 71%__________________________________________
A CB
Figure 2. AMACR expression in colitis without dysplasia (A), with high-grade dysplasia (B), and invasive adenocarcinoma (C).
Natural History_____________________________________Dysplasia (%) n Cancer (%)_____________________________________None 382 9 (2)Low grade 72 5 (7)High grade 170 37 (22)_____________________________________
Sampliner. Am J Gastroenterol 2002:97(8);1888-1895
Esophagectomy forHigh-Grade Dysplasia__________________________________________
Series Unsuspected Carcinoma__________________________________________Edwards (1996) 8/11 (73%)Heimiller (1996) 13/30 (43%)Cameron (1997) 2/19 (10.5%)Ferguson (1997) 8/15 (53%)Falk (1997) 4/12 (33%)
Total 35/87 (40%)_________________________________________
Natural History of High-Grade DysplasiaProspective Studies
Schnell et al, Schnell et al, GastroenterolGastroenterol 2001; 120:16072001; 120:1607--1619 1619 Reid et al, Am J Reid et al, Am J GastroenterolGastroenterol 2000; 95:16692000; 95:1669--16761676
Weston et al, Am J Weston et al, Am J GastroenterolGastroenterol 2000; 95: 18882000; 95: 1888--1893 1893
Seattle (Incident HGD)Seattle (Incident HGD)N=27N=27
Seattle (Baseline HGD) Seattle (Baseline HGD) N=76N=76
Pro
po
rtio
n w
ith
Can
cer
Pro
po
rtio
n w
ith
Can
cer
YearsYears
Hines VA, N=75Hines VA, N=75(Excluded 4 cancers in 1(Excluded 4 cancers in 1stst
year)year)
Kansas VA, N=15Kansas VA, N=15
Low-Grade Dysplasia
103 (66%)12 (75%)
5 (3%)1 (6%)
15616
Sharma et al.Conio et al.
20 (3%)
1 (2%)
Progress to Cancer (%)
ND758Schnell et al.
31 (65%)48Weston et al.
Regression (%)No. LGDStudy
Weston et al, Am J. Weston et al, Am J. GastroenterolGastroenterol 2001; 96:13552001; 96:1355--13621362Schnell et al, Gastroenterology 2001; 120:1607Schnell et al, Gastroenterology 2001; 120:1607--16191619
Sharma et al, Gastroenterology 2002; 122:A20Sharma et al, Gastroenterology 2002; 122:A20ConioConio et al, Am J et al, Am J GastroenterolGastroenterol 2003; 19312003; 1931--19391939
Prospective StudiesProspective Studies
ACG guidelines for Surveillance in Barrett’s esophagus: (Sampliner et al, Am J Gastroenterol 97:1888,2002)
Chronic GERD Symptoms
Screening Endoscopy with Biopsies
Negative for dysplasia Low grade dysplasia High-grade dysplasiax2 endoscopies
Repeat endoscopy with biopsyExpert pathologist opinion
3 year surveillance Repeat x 1Focal Mucosal Multifocal
Annual surveillance irregularityUntil no dysplasia 3 months Intervention
surveillance EMR (surgical)
The Case for Barrett’s Surveillance5-year Survival of Surveyed and Non-surveyed Cases
73.3%
52.9%
90.0%
0.0%
20.0% 20.0%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Corley Streitz Peters
5-ye
ar S
urv
ival
Surveyed cases
Non-surveyed cases
Corley et al, Gastroenterology 2002; 122:633Corley et al, Gastroenterology 2002; 122:633StreitzStreitz et al, J et al, J ThoracThorac CardiovascCardiovasc SurgSurg 1993; 105:3831993; 105:383Peters et al, J Peters et al, J ThoracThorac CardiovascCardiovasc SurgSurg 1994; 108:8131994; 108:813
Ideal Biopsy Protocol• Jumbo forceps• 4 quadrant Q2 cm in BE• 4 quadrant Q1 cm in dysplasia• All nodules/polyps/masses• Confirm with experienced GI
pathologist
Management ConsiderationsSurveillance vs. Esophagectomy
Extent of HGDExtent of LGDNodularityPatient ageComorbiditiesLength of BE
Extent of dysplasia in BEButtar et al, Gastro 2001;120:1630-1639
_________________________________________________________________________
# 1 year 3 year RRPatients survival survival Carcinoma Cancer
_________________________________________________________________________
Focal HGD 33 93% 86% 12% -Diffuse HGD* 67 62% 66% 42% 5.36Nodularity 25 - - 60% 3.98Lack of acid suppression 100 - - 42% 2.48_________________________________________________________________________
Focal <5 crypts, diffuse >5 crypts or >1 biopsy
Extent of Low Grade Dysplasia is a Significant Risk Factor for
Cancer in Barrett’s EsophagusOdze et al, Mod Pathol 2005;18(1):119
Table 3: Mean number of crypts/biopsy in each diagnostic category___________________________________________________________________________Maximum Diagnosis Non-Progressors Progressors___________________________________________________________________________
Negative for dysplasia 23.29 20.38(range; SD) (7.6548.65; 9.51) (5.74-52.40; 9.07)
Indefinite for dysplasia 0.005 0.0166(range; SD) (0-0.205; 0.0320 (0-0.463; 0.088)
LGD 2.595 5.802(range; SD (0-22.32; 4.98) (0-20.32; 6.25)
HGD 0.835 1.294(range; SD) (0-10.08; 2.27) (0-11.17; 2.4)___________________________________________________________________________
Flow Cytometry: Prospective StudiesFlow Cytometry: Prospective StudiesPatients without HighPatients without High--Grade DysplasiaGrade Dysplasia
TeodoriTeodori et alet alN=30 patientsN=30 patients
NormalNormalCytometryCytometry
(N=17)(N=17)
AbnormalAbnormalCytometryCytometry
(N=13)(N=13)
0% cancer0% cancer 23% cancer23% cancer
Reid et al, Am J Gastro 2000; 95:1669Reid et al, Am J Gastro 2000; 95:1669TeodoriTeodori et al, Cytometry 1998; 34:254et al, Cytometry 1998; 34:254
p<0.01 for dysplasia or cancer (46%)p<0.01 for dysplasia or cancer (46%)
Pro
bab
ility
of C
ance
rP
rob
abili
ty o
f Can
cer
Aneuploid and/or 4N
Diploid, normal 4N
N=247 patientsN=247 patientsReid et al
p < 0.001p < 0.001
½ biopsy every 2 cm½ biopsy every 2 cm
28%28%
0%0%
Ulcers in BE(Montgomery et al, Am J Gastro 2002;97(11):27-31)
_________________________________________________________________________
Ulcer-relatedDysplasia # cases Ulcers CA onGrade (35/138) follow-up______________________________________________________
Neg 44 7% 0%Indef 22 9% 0%LGD 26 0% 0%HGD 33 33% 8/10 (80%)*CA 13 54% -______________________________________________________*8/10 vs 12/23 p<.05
Barrett’s Esophagus:New Surveillance Strategies
• Balloon cytology• Fluorescence spectroscopy• Chromoendoscopy• Flow cytometry