Lecture 2 Esophagus
Transcript of Lecture 2 Esophagus
-
LECTURE 2
DISORDERS OF THE ESOPHAGUS
ESOPHAGEAL FUNCTION
INSERTION BY HYPOPHARYNX & INSERTION BY HYPOPHARYNX & RELAXATION OF THE UPPER ESOPHAGEAL SPHINCTER (UES) TRANSPORT BY ESOPHAGEAL PERISTALSIS DELIVERY BY PERISTALSIS AND RELAXATION OF THE LOWER ESOPHAGEAL SPHINCTER (LES)
LES pressure is about 15 mmHg above intragastric pre ssure
-
59-y.o. male
History of chest pain Intermittent heartburn Intermittent dysphagia Normal exam Labs: normal Normal cardiac evaluation
-
CASE
UPPER ENDOSCOPY: EROSIVE ESOPHAGITIS ESOPHAGEAL
STRICTURE
TREATMENT ESOPHAGEAL DILATION HEALTH HABITS and
DIETARY PRECAUTIONS PROTON PUMP INHIBITOR
-
ESOPHAGEAL SYMPTOMS HEARTBURN DYSPHAGIA
OROPHARYNGEAL 32 muscles involved with swallowing
ESOPHAGEAL NEUROMUSCULAR DYSFUNCTION NEUROMUSCULAR DYSFUNCTION MECHANICAL
REGURGITATION CHEST PAIN ODYNOPHAGIA PSEUDOPHAGIA GLOBUS
-
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
PATHOPHYSIOLOGY: REFLUXATE OVERCOMES THE ANTIREFLUX BARRIERS OF THE
GASTROESOPHAGEAL JUNCTION (LES @ GEJ)
INAPPROPRIATE, PATHOLOGIC, SPONTANEOUS TRANSIENT RELAXATION OF THE LOWER ESOPHAGEAL SPHINCTER
REDUCED LES PRESSURE INCREASED ABDOMINAL PRESSURE
OBESITY PREGNANCY
INCREASED NOCTURNAL HCL (EATING LATE )
-
GERD PATHOPHYSIOLOGY
INCREASED ESOPHAGEAL:HCL (acid) CONTACT (at night) WITH DECREASED CLEARING OF REFLUXATE
DELAYED GASTRIC EMPTYING HIATAL HERNIA (sliding) HIATAL HERNIA (sliding)
TRANSIENT RELAXATION OF THE LES IMPAIRED LES FUNCTION
SMOKING, ALCOHOL, CAFFEINE, CHOCOLATE NEGATIVE H. PYLORI STATUS
POSITIVE H. pylori STATUS IS PROTECTIVE EMOTIONAL STRESS
INCREASES SUBJECTIVE SEVERITY OF REFLUX SYMPTOMS BUT NOT THE NUMBER OR DURATION OF REFLUX EVENTS
-
LESP & HIATAL HERNIA GERD
Size of Hiatal Hernia
-
HIATAL HERNIASLIDING
-
PROGRESSIVELY INCREASING LAXITY OF THE PHRENOESOPHA GEAL MEMBRANE, , LEADING TO HIATAL HERNIA AND GROSS INCOMPETENCE
-
HIATAL HERNIA PARAESOPHAGEAL
MOST (SMALL) AREASYMPTOMATIC
LARGER PARAESOPHAGEALHERNIA CAN CAUSE:EPIGASTRIC PAINEPIGASTRIC PAINNAUSEA/VOMITINGGASTRIC OBSTRUCTIONBLEEDINGPERFORATIONGASTRIC VOLVULUS
REQUIRE SURGICALREPAIR
-
PULMONARYGERD NOT A COMMON CAUSE OF THESE
CONDITIONS
ASTHMA CHRONIC BRONCHITIS ATELECTASIS ATELECTASIS PULMONARY FIBROSIS CHRONIC COUGH
-
EAR-NOSE-THROATGERD NOT A COMMON CAUSE OF THESE
CONDITIONS:
THROAT CLEARING CHRONIC HOARSENESS DENTAL DISEASE HALITOSIS HALITOSIS NOCTURNAL CHOKING GLOBUS VOCAL CORD ULCERS SUBGLOTTIC STENOSIS PHARYNGITIS NAUSEA
-
DIAGNOSIS GERD
HISTORY - SYMPTOMS UGI SERIES (BARIUM)
DEMONSTRATE REFLUX INSENSITIVE INSENSITIVE
UPPER ENDOSCOPY NORMAL (NERD) ESOPHAGITIS BARRETTS ESOPHAGUS EVALUATE AND TREAT
COMPLICATIONS
-
WHEN TO DO ENDOSCOPY ?ALARM SYMPTOMS
DYSPHAGIA GI BLEEDING ANEMIA WEIGHT LOSS WEIGHT LOSS INADEQUATE THERAPEUTIC
RESPONSE POSSIBLE BARRETTS ESOPHAGUS
with LONG HISTORY OF UNDER TREATED GERD, SYMPTOMS > 5 YRS although there is questionable benefit with routine screening
-
OTHER DIAGNOSTIC TESTS ESOPHAGEAL MOTILITY
POSITION pH PROBE EVALUATE ESOPHAGEAL FUNCTION
BEFORE SURGERY
24-hour pH STUDY WHEN DIAGNOSIS IS IN DOUBT NON RESPONSE TO THERAPY
ESOPHAGEAL IMPEDANCE MEASURES REFLUX; ACID AND
NONACID REFLUX
-
ESOPHAGTITIS
-
ESOPHAGEAL STRICTURE
-
THERAPY GERD IS CHRONIC & RECURRENT
THERAPY IS LONG TERM IN MODERATE TO SEVERE DISEASE
DIET AND HEALTH HABITS ELEVATION - HEAD OF THE BED
(NIGHTTIME SYMPTOMS)(NIGHTTIME SYMPTOMS) TITRATE TO DISEASE SEVERITY
PPIs when ALARM SYMPTOMS PRESENT STEP UP THERAPY
UNTIL CONTROLLED
STEP DOWN THERAPY UNTIL BREAK-THROUGH
-
H-2 BLOCKERS
CIMETIDINE (TAGAMET) RANITIDINE (ZANTAC) FAMOTIDINE (PEPCID) FAMOTIDINE (PEPCID) NIZATIDINE (AXID)
-
PROTON PUMP INHIBITORS
OMEPRAZOLE (PRILOSEC)* LANSOPRAZOLE (PREVACID, DEXILANT) REBEPRAZOLE (ACIPHEX) PANTOPRAZOLE (PROTONIX) PANTOPRAZOLE (PROTONIX) ESOMEPRAZOLE (NEXIUM)** OMEPRAZOLE + Na Bicarb
IMMEDIATE RELEASE (ZEGERID)
-
LIMITATIONS OF PPI TREATMENT GERD
SPECIFIC GERD Sx ARE NOT EQUALLY RESPONSIVE Heartburn > Regurgitation > Chest pain > Cough
NO SYMPTOM IS 100% SPECIFIC FOR GERD Nonresponsive to treatment make sure there is refl ux
24 hour pH monitoring or Esophageal impedance testi ng 24 hour pH monitoring or Esophageal impedance testi ng
HYPERSENSITIVITY PPIs do not directly treat GERD; it is a neuromuscu lar
dysfunctional disorder that leads to pathological r eflux
-
TYPICAL GERD SYMPTOMS
ALARM SX / SIGNS PRESENTDYSPHAGIAFOOD IMPACTIONWEIGHT LOSSGI BLEEDINGANEMIAADVANCED AGE (>50)FAMILY HX OF UGI CANCERODYNOPHAGIA
ALARM SX / SIGNS ABSENT
LIFESTYLE CHANGESOTC AA or H2RA prn
PERSISTENT SXSNO
CONTINUE RX
YESUPPER ENDOSCOPY
H2RA BID or PPI QD
YES
PERSISTENT SXS
CONTINUE TX, DECREASING TOLOWEST EFFECTIVE ACID SUPPRESSION TO CONTROL SXS
NO
UPPER ENDOSCOPY
YES
EROSIVE ESOPHAGITISESOPHAGEAL ULCERBARRETTS ESOPHAGUSNORMAL
PPI BID or for NORMAL QD
PERSISTENT SXS
24-HOUR pH or IMPEDANCE STUDY ANTIREFLUX PROCEDURE
NO
YES REFLUX CONFIRMED
CANCERDYSPHAGIAWT LOSS
EOSINOPHILIC ESOPHAGITIS
-
COMPLICATIONSGERD
STRICTURE - DYSPHAGIA ULCER PAIN, BLEEDING INTRACTABLE
TROUBLESOME SYMPTOMS TROUBLESOME SYMPTOMS MICROASPIRATION BARRETTS ESOPHAGUS
-
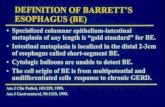
BARRETTS ESOPHAGUSSPECIALIZED INTESTINAL METAPLASIA IN THE
DISTAL ESOPHAGUS1.7% OF ADULT POPULATION IN US
CHRONIC SEVERE REFLUX of both Acid and Bile salts a nd esophageal exposure time
ENDOSCOPY AND BIOPSIES STRICTURE (MID-ESOPHAGUS) STRICTURE (MID-ESOPHAGUS) RISK FOR PROGRESSION TO CANCER
LARGE HIATAL HERNIA LONG BARRETTS SEGMENT DYSPLASIA (high grade) MALES > FEMALES AGE > 70 SMOKING
ADENOCARCINOMA RISK ~ 0.3% /year
1/3 OF PATIENTS ARE ACID INSENSITIVE
-
BARRETTS ESOPHAGUS
-
BARRETTS ESOPHAGUS ULCER
-
ESOPHAGEAL STRICTURE BARRETTS ESOPHAGUS
-
63-year-old male presents with a history of
progressive dysphagia
Dysphagia associated with a 15 lb weight loss over the last 3 months
Has to eat softer food to get it to go down 40 year history of smoking 1 pack of cigarettes/day Exam: height was 70 inches and he weighed 155 lbs Exam: height was 70 inches and he weighed 155 lbs
(weight 6 months ago 170 lbs) The remainder of the examination was normal except
for reduced breath sounds on chest exam
WHAT IS THE MOST LIKELY CAUSE OF THIS PATIENT S DYSPHAGIA?
-
Downloaded from: Gastrointestinal and Liver Disease 8e (on 24 September 2006 03:28 PM)
2005 Elsevier
GERD EoE
-
OBSTRUCTIVE LESIONSDYSPHAGIA
CARCINOMA DYSPHAGIA with WEIGHT LOSS SQUAMOUS CELL CARCINOMA
ALCOHOL AND SMOKING ALCOHOL AND SMOKING
ADENOCARCINOMA GASTROESOPHAGEAL REFLUX DISEASE
ALSOLUTE RISK IS LOW< 10,000 CASES/YEAR IN USINCIDENCE IS INCREASING
-
ESOPHAGEAL ADENOCARCINOMA PATHOGENESIS
GERD CHRONIC ESOPHAGITIS INTESTINAL METAPLASIA INTESTINAL METAPLASIA
(BARRETTS)* (ALL CASES?)DYSPLASIA ADENOCARCINOMA
Enzinger, PC and Mayer, RJ; Medical Progress: Esop hageal Cancer. NEJM; 2003, 349:2241-2252
-
TNM STAGING ESOPHAGEAL CANCER
CT CHEST / UPPER ABDOMEN / ENDOSCOPIC ULTRASOUND
PRIMARY TUMOR (T 1 - 4) REGIONAL LYMPH NODES (N0, N1) DISTANT METASTASIS (M0, M1) T1 OR T2, NO, MO - CURATIVE SURGERY T4 OR M1 - CHEMORADIATION T2 OR T3, N1 - CHEMORADIATION +/-
SURGERY
-
ESOPHAGOGASTRECTOMYCANCER OF THE DISTAL ESOPHAGUS
5-YEAR SURVIVAL: 20-25%
-
ESOPHAGEAL CANCERADENOCARCINOMA
-
ESOPHAGEAL CANCER SQUAMOUS CELL
OBSTRUCTIVE DYSPHAGIAALCOHOL & SMOKING
-
ESOPHAGEAL CANCER SQUAMOUS CELL
RADIOGRAPHIC APPEARANCE
-
ESOPHAGEAL CANCER ADENOCARCINOMA
-
26-year-old male dysphagia associated with an
esophageal food impaction
Occurred while eating chicken History of intermittent heartburn and on occasion d ysphagia
over the last 3 years. The heartburn has not been helped with the use of r anitidine The patient was thin otherwise the examination was normal
Labs including a CBC were normal Labs including a CBC were normal
WHAT DOES IMPACTION SUGGEST?
WHAT ARE THE POSSIBLE CAUSES OF THE DYSPHAGIA?
HOW SHOULD THIS PATIENT BE EVALUATED?
-
MEAT (CHICKEN) IMPACTION IMPACTION REMOVED
EOSINOPHILIC ESOPHAGTITIS
-
EOSINOPHILIC ESOPHAGITIS (EoE ) AFFECTS ALL AGE GROUPS including children MEN > WOMEN SHARES CLINICAL and HISTOLOGIC FEATURES with GERD
CHILDREN: vomiting, feeding intolerance, failure to thrive ADULTS: chest pain, heartburn, epigastric pain, dysp hagia, food
impactions, refractory GERD
EoE AND GERD ARE NOT MUTUALLY EXCLUSIVE PPI-responsive EoE (do not have GERD) exhibit a clinical PPI-responsive EoE (do not have GERD) exhibit a clinical
response to PPIs PPI may have an anti-inflammatory effect
TREATMENT of SUSPECTED EoE: Trial of PPI for 2 months Swallowed topical steroids Empiric elimination diets Esophageal dilation for dysphagia
-
EOSINOPHILIC ESOPHAGITISFOOD ALLERGY or AEROALLERGEN
ANTIGEN
ACTIVATED IMMUNE SYSTEM
Th2 (IL-4, IL-5, IL-13)
EOTAXIN-3 secretion from the esophageal
squamous cells
Eosinophilshome to the esophagus
Omeprazole blocks IL-13 Induced Eotaxin-3 secretionIn sq. cells from EoE patients
-
69-YEAR OLD MALE PRESENTS TO THE EMERGENCY DEPARTMENT AT 11:00 PM WITH THE INABILITY TO
SWALLOW HIS OWN SALIVA
He was eating a steak at 7:00 pm which lodged in his throat
Has been unable to swallow since that time Normally has no difficulty eating, but has noted tha t Normally has no difficulty eating, but has noted tha t
meat has had a tendency to hang-up on occasion. Except for drooling the exam was normal
WHAT IS THE CAUSE OF THIS PATIENT S DYSPHAGIA?HOW SHOULD THIS PROBLEM BE EVALUATED AND TREATED?
-
Downloaded from: Gastrointestinal and Liver Disease 8e (on 24 September 2006 03:28 PM)
2005 Elsevier
GERDEoE
-
OBSTRUCTIVE LESIONSRINGS
SCHATZKIS RING 10% OF POPULATION LUMEN < 13 mm: DYSPHAGIA LUMEN < 13 mm: DYSPHAGIA
14-18 mm MAY HAVE DYSPHAGIA
-
SCHATZKIS RING
-
FOOD IMPACTION SCHATZKIS RING
RELATED TO GERD
-
55-YEAR OLD MALE WHO HAS A HISTORY OF PROGRESSIVE DYSPHAGIA TO BOTH
LIQUIDS AND SOLIDS
15 lbs loss over the last 6 months Notes regurgitation but not heartburn. He tried
Prilosec but it was not helpful The patient was somewhat thin but the
examination was otherwise normal Labs including a CBC were normalPOSSIBLE CAUSES OF THIS PATIENT S DYSPHAGIA?
-
Downloaded from: Gastrointestinal and Liver Disease 8e (on 24 September 2006 03:28 PM)
2005 Elsevier
GERDEoE
-
ESOPHAGEAL NEUROMUSCULAR (MOTILITY)
DISORDERS
ACHALASIA SCLERODERMA SCLERODERMA MOTILITY DISORDERS
DISTAL (DIFFUSE) ESOPHAGEAL SPASM
HYPOMOTILITY
-
ACHALASIAFAILURE TO RELAX
DEGENERATION OF NEURONS (MYENTERIC PLEXUS) NITRIC OXIDE NEURONS
(INHIBITION)(INHIBITION) VIP NEURONS
REDUCED RELAXATION of the LES WITH SWALLOWING INCREASED LES PRESSURE
LOSS OF PERISTALSIS IN THE LOWER 2/3 OF THE ESOPHAGUS
-
ACHALASIA
DYSPHAGIA TO BOTH LIQUIDS AND SOLIDS
WEIGHT LOSS ASPIRATION ASPIRATION INCREASED RISK OF SQUAMOUS
CARCINOMA AFTER AGE 50 IF UNTREATED
-
ACHALASIA DIAGNOSIS
UPPER ENDOSCOPY ESOPHAGEAL MOTILITY STUDY
TREATMENT PNEUMATIC BALLOON DILATION PNEUMATIC BALLOON DILATION SURGICAL MYOTOMY BOTOX INJECTION MEDICATION NOT VERY USEFUL
NITRATES CALCIUM CHANNEL BLOCKER VIAGRA
-
ACHALASIA
BIRDS BEAK ENDOSCOPIC VIEW
-
ACHALASIA PNEUMATIC BALLOON DILATION
-
19-YEAR OLD FEMALE COMPLAINS OF
ODYNOPHAGIA
She has a history of acne for which she takes doxycycline which she typically takes at night
She woke up in the morning with severe odynophagia when she drank a glass of orange juice. juice.
Examination was normal. Labs including a CBC were normal
WHAT IS THE MOST LIKELY CAUSE OF THIS PATIENT S ODYNOPHAGIA?
-
PILL ESOPHAGITIS ODYNOPHAGIA
-
ESOPHAGEAL INFLAMMATORY LESIONS
EOSINOPHILIC ESOPHAGITIS PILL ESOPHAGITIS CANDIDA ESOPHAGITIS HERPETIC ESOPHAGITIS HERPETIC ESOPHAGITIS IDIOPATHIC ULCER - AIDS
CANDIDA CMV HERPES
-
CANDIDA ESOPHAGITIS ODYNOPHAGIA
-
HERPETIC ESOPHAGITIS ODYNOPHAGIA
-
IDIOPATHIC ULCER - AIDS ODYNOPHAGIA
-
ESOPHAGEAL DISORDERS KEY POINTS
GERD COMMON, RECURRENT, CHRONIC WIDE SPECTRUM OF SYMPTOMS TAILOR THERAPY TO SEVERITY STRICTURES 10%
EXCLUDE CARDIAC CAUSES OF CHEST PAIN PRIOR TO CONSI DERING THE DIAGNOSIS OF NON-CARDIAC CHEST PAIN
ALARM SYMPTOMS WARRANT UPPER ENDOSCOPY PPIs ARE EFFECTIVE AND SAFE FOR APPROPRIATE INDICAT IONS AND USING
LOWEST EFFECTIVE DOSELOWEST EFFECTIVE DOSE ESOPHAGEAL ADENOCARCINOMA IS ON THE RISE (OBESITY, LONG HISTORY OF
GERD, BARRETTS ESOPHAGUS) SQUAMOUS CELL CARCINOMA RELATED TO TOBACCO AND ALCO HOL USE
(DECREASING) ACUTE ODYNOPHAGIA - PILL ESOPHAGITIS INFLAMMATORY ESOPHAGITIS
EOSINOPHILIC ESOPHAGITIS (CHILDREN, ADULTS MALE > FEMALE) SHARES SYMPTOMS WITH GERD ENDOSCOPY WITH BIOPSIES PPI, TOPICAL STEROID, ELIMINATION DIET
HEALTHY PEOPLE: HSV AIDS, DM, CHEMO: CANDIDA, CMV, HSV, IEU (AIDS)
SCHATZKIS RINGS INTERMITTENT DYSPHAGIA
-
LARGE ESOPHAGEAL ULCER WITH TRACHEOESOPHAGEAL FISTU LA
ESOPHAGEAL STENT PLACED
TRACHEOESOPHAGEAL FISTULA