Atopic dermatitis(Eczema)
-
Upload
dr-raza -
Category
Health & Medicine
-
view
194 -
download
1
Transcript of Atopic dermatitis(Eczema)

Dr Muhammad Raza
PG Trainee MCPS

1. To know about basic concept of atopic dermatitis.
2. Signs and symptoms of the disease
3. Etiology and pathogenesis.
4. Diagnosis, management and referral of the disease.
By the end of my presentation each participant should be able to:

Atopic Dermatitis(Eczema)
• Atopic dermatitis (eczema) is a condition that makes your skin cracked, swollen, red and itchy. It's common in children but can occur at any age.
• Atopic dermatitis is long lasting (chronic)and tends to flare periodically.
• It may be accompanied by asthma or hay fever

People with atopic dermatitis
• More than 50% develop asthma
• 75% develop allergic rhinitis


Signs and symptoms
Dry skin
Itching , especially at night
Red to brownish-gray patches, especially on the hands, feet,
ankles, wrists, neck, upper chest, eyelids, inside the bend of the
elbows and knees, and in infants, the face and scalp
Small, raised bumps, which may leak fluid and crust
over when scratched
Thickened, cracked, scaly skin
Raw, sensitive, swollen skin from scratching.


UK Diagnostic criteria
Itchy skin and at least three of the
followings:
History of itch in skin creases or
cheeks(if < 4yrs)
Dry skin
(Xeroderma)
Visible flexural
eczema(cheeks,fore
head,outer limbs if
< 4yrs
History of
asthma/hay fever(in
1st-degree relatives
if < 4yrs)
Onset in first 2
years of life

Infancy
• Often acute and involves the face and trunk
sparing of napkin area
Childhood
• Back of the knees, front of the elbows, wrists and
ankles
Adults
• Face and trunk, lichenification is common
Distribution and character of rash

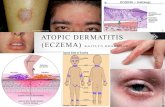
Typical AD for Infants and Toddlers
Erythematous, ill-
defined plaques on
the lateral lower
with overlying scale
Erythematous, ill-
defined plaques on
the cheeks with
overlying scale and

More Examples of Atopic Dermatitis
• Note the distribution of AD on face and extensor surfaces

Affects flexural areas of neck, elbows, knees,
wrists, and ankles
• Antecubital fossa • Lichenified, erythematous plaques behind the knees

Acute
• Redness and
swelling,usually
with ill defined
margins
• Papules,vesicles
and large blisters
• Exudation and
cracking
Chronic
• Usually less
vesicular and
exudative.
• Lichenification,
secondary to
rubbing and
scratichng
• Fissures, scratch
marks
Continue….

EPIDEMIOLOGY
Age Of Onset 60% develop in 2 months to 1 year of life. 30% are seen for the first time by age 5, and 10% develop AD between 6
20 years of age. Rarely AD has an adult onset
Gender Slightly More Common in males than females

The cause of AD is multifactorial and not completely understoodThe following factors are thought to play varying roles:
Genetics
Skin Barrier Dysfunction
Impaired Immune Response
Eliciting factors
Exacerbating factors



• Mutation in filaggrin gene(FLG), which encodes a
protein that aggregates keratin filaments during
terminal differentiation of the epidermis
• Filaggrin is an important component of barrier of
the skin
Filaggrin

Atopic Dermatitis: Cause

ELICITING FACTORS
Inhalants Specific aeroallergens, especially dust mites and pollens.
Microbial Agents Exotoxins of Staphylococcus aureus may act as super-antigents and stimulate the T cells and macrophages
Auto-allergens IgE antibodies directed at human proteins cause release of auto-
allergens from damaged tissue which trigger IgE or T cell responses.
Foods Eggs, milk, soya-beans, fish and wheat

Exacerbating Factors
Skin Barrier Disruption Increase transepidermal water loss by frequent bathing, handwashing and dehydration
Infections S.aureus present in severe cases; rarely fungus (dermatophytosis, candidiasis)
Season AD improves in summer, flares in winter
Clothing Wool is an important trigger; wool clothing or blankets.
Emotional Stress is an exacerbating factor in flares of the disease

Diagnosis
Skin biopsy elevated
numbers of a certain type of
white blood cells
(eosinophils) and elevated
serum IgElevel)
Skin scratch/prick
test which involve
scratching or pricking the skin with a needle that contains a
small amount of a suspected
allergen)
Patch test is performed in
suspected cases of contact allergic
dermatitis
Bacterial and viral
swabs are useful in
suspected secondary infections
Total & specific IgE antibodies
to determine specific
environmental allergens.
RAST
(Radioallergosorbenttest may
suggest dust mite allergy)
Atopic dermatitis is typically diagnosed
clinically by UK diagnostic criteria ,
however further labs are helpful in
diagnosing AD.

Management
Primary preventionMoisturize your skin at least twice a day (Creams,
ointments and lotions)
Identify and avoid triggers that worsen the condition (sweat, stress, obesity, soaps, detergents, dust and pollen)
Take shorter baths or showers (Limit your baths and showers to 10 to 15 minutes. And use warm, rather than hot, water)

Continue….
Take a bleach bath (A diluted-bleach bath with household bleach for 10 minutes decreases bacteria on the skin and related infections)
Use only gentle soaps (Choose mild soaps,Because deodorant soaps and antibacterial soaps can remove more natural oils and dry your
skin.)
Dry yourself carefully (After bathing gently pat your skin dry with a soft towel and apply moisturizer
while your skin is still damp)

Atopic Dermatitis
Irritants
Wool Clothing
Winter Chapping
Excessive Heat
Sweating
Airborne allergens
Food allergens
Skin infections
Stress
Habitual scratching
Supportive Care

• Emollients (Moisturizers)
• (Alpha-Hydroxy acid) is made up of glycolic
acid(8%) + lactic acid(12%) + Urea (6%).
• Vanicream,Eucerin,Lubiderm,Curel and vaseline
petroleum jelly.
• Urea creams
• Oils
• Apply emollients once in a day after bathing
and the times when the skin is usually dry.
1st line treatment
( Emollients+ Topical steroids)

Topical steroids
• Hydrocortisone 1-2.5% applied to all skin
• Quite safe and often use for months
• Use intermittently on thin areas(face and
• Stronger potency topical steroids for non
facial/genital regions.
• Avoid potent/ultrapotent topical steroid
preparations on face,armpit,groins & bottom.

2nd line treatment
• Topical immunosuppresants and topical calcineurin
inhibitors like tacrolimus and pimecrolimus.
Use when the continued use of topical steroids is
ineffective or inadvisable
3rd line treatment
• Phototherapy with ultraviolet (UV) light can be an effective treatment for severe atopic dermatitis.
Combined UVA and UVB light have a more beneficial
effect than UVA or UVB light alone. UV light may also
help to prevent bacterial infections.

Systemic Treatment
→Antihistamines for itching
Linoleic acid and linoleic gamma for pruritis
→Macrolide and cephalosporin for secondary bacterial infection
→Acyclovir for “Herpeticumeczema”

Advance Therapies
Cyclosporine Methotrexate AzathioprineBiologics(Anti-
IgE i-e omaltizumab)

Differential Diagnosis
• seborrheic dermatitis
• Scabies
• Drug reactions
• Psoriasis
• Allergic contact dermatitis
• Cutaneous T-cell lymphoma
• Lichen planus
• Palmoplanter pustulosis

• Staph areus is most commonBacterial
• Herpes simplex virus cause a widespread severe eruption( eczema herpeticum)
• Papillomavirus and moluscum contagiosum.Viral
• Defective barrier functionIrritant reaction
• Loss of schooling and behavioural difficultiesSleep disturbance
• Eggs, cow’s milk, protein, fish, wheat and soya may cause an immediate urticarial eruption.Food allergy
Complications of atopic eczema

When to Refer
Patients should be referred to a
dermatologist when:→Patients have recurrent skin
infections
→Patients have extensive and/or
severe disease
→Herpeticum eczema
→Symptoms are poorly controlled
with topical steroids



Resources
• http://www.nhs.uk/conditions/pregnancy-and-baby/pages/eczema-in-children.
• https://nationaleczema.org/eczema/child-eczema/
• https://www.allergyuk.org/atopic-dermatitis-and-eczema-in-children/atopic-dermatitis-eczema-in-children