ACLS Lecture
-
Upload
gotsunshyne -
Category
Health & Medicine
-
view
15.836 -
download
7
Transcript of ACLS Lecture

2005 AHA Guideline Changes
BLS for Healthcare ProvidersACLS Updates


Purpose of BLS Changes
To improve survival from cardiac arrest by increasing the number of victims of cardiac arrest who receive early, high-quality CPR
Planned, practiced response with CPR/AEDs yields survival rates of 49-74%

What Have We Learned About CPR? 330,000 die annually from coronary heart
disease CDC
60% from Sudden cardiac event @ home or en route
85-90% in VF/VT arrest 2-3 x greater survival if CPR is immediate,
with defib <5 min. EMS relies on trained, willing, equipped
public

Less than 1/3 get bystander CPREven pros don’t do good CPR! Too slow Too shallow No CPR x 24-49% of the arrest!

Most significant changes 2005
IT’S ALL ABOUT BLOOD FLOW!
Emphasis on effective CPR Fast; deep; 50/50; minimal interruption
Single compression-to-ventilation ratio 30:2 single rescuer adult, child, infant, excluding
newborns

Most significant changes (cont.)
Each shock from an AED should be followed by 2 minutes of CPR (5 cycles of 30:2) starting with compressions
Each rescue breath should take one second and produce visible chest rise
Reaffirmation that AEDs should be used for kids 1-8 y.o.

Why change compressions?
When compressions stop, blood flow stops! Universal compression ratio easier to
learn/retain Higher ratio yields more blood flow; keeps
pump “primed”

Why shorten breaths?
Large volume breaths increase ITP; decrease venous return to heart
Long breaths interrupt compressions Hyperventilation decreases coronary and
cerebral perfusion pressures Over-ventilation increases air in stomach;
regurgitation/aspiration

Why from 3 shocks to 1?
Biphasic defibrillators eliminate VF 85% on first shock
Current AED sequence can delay CPR 37 seconds Long CPR interruptions decrease likelihood of
subsequent successful shocks Myocardial “stunning” (O2, ATP depletion)

Chest Compressions
2005 (New): Push hard, fast, rate of 100 per minute Allow full chest recoil after each compression Minimize interruptions (no more than 10 seconds
at a time) except for specific interventions (advanced airway/AED)

Chest Compressions cont’d
2000 (Old): Less emphasis was given to need for adequate
depth, complete chest recoil, and minimizing interruptions

Chest Compressions cont’d
Why: If chest not allowed to recoil:
less venous return to heart reduced filling of heart Decreased cardiac output for subsequent chest
compressions When chest compressions are interrupted,
blood flow stops and coronary artery perfusion pressure falls

Chest Compressions cont’d
Why: Study of CPR performed by healthcare
providers found that: ½ of chest compressions too shallow No compressions provided during 24% to
49% of CPR time

Changing Compressors Every 2 Minutes 2005 (New):
If more than 1 rescuer present, change “compressor” roles every 2 minutes
2000 (Old): Rescuers changed when fatigued-usually did not report
feeling fatigued until 5min. or more Why:
In manikin studies, rescuer fatigue developed in as little as 1-2minutes(as demonstrated by inadequate chest compressions)

Rescue Breathing without Compressions 2005 (New):
10-12 breaths per minute (adults) 1 every 5-6 seconds
12-20 breaths per minute for infant or child 1 every 3-5 seconds
2000 (Old): 10-12 breaths for adults 20 breaths for infant or child

Rescue Breathing without Compressions cont’d
Why: Wider range of acceptable breaths for infant and
child will allow the provider to tailor support to patient
Note: If you are assisting lay rescuer-they are not taught to deliver rescue breaths without chest compression

Rescue Breaths with Compressions
2005 (New): Each rescue breath should be given over 1
second and produce visible chest rise Avoid breaths that are too large or too forceful Manikins configured so that visible chest rise
occurs at 500-600ml 2000 (Old):
Rescue breaths over 1-2 seconds Recommended tidal volume for adult rescue
breaths was 700ml-1000ml

Rescue Breaths with Compressions cont’d
Why: Oxygen Delivery
Oxygen delivery is product of oxygen content in the arterial blood and cardiac output (blood flow)
During first minutes of CPR for VF SCA, initial oxygen content in blood adequate/ cardiac output is reduced
Effective chest compressions more important than rescue breaths immediately after VF SCA

Rescue Breaths with Compressions cont’d
Why: Ventilation-Perfusion Ratio
The best oxygenation of blood and elimination of CO2 occur when ventilation (volume of breaths x rate) closely matches perfusion
During CPR , blood flow to lungs is about 25-33% of normal
Less ventilations needed during cardiac arrest than when patient has perfusing rhythm

Rescue Breaths with Compressions cont’d
Why: Hyperventilation leads to:
Increased positive pressure in the chest Decreased venous return to the heart Limited refilling of heart Decreased cardiac output during
subsequent compressions Gastric distention/vomiting


2 Rescuer CPR with Advanced Airway
2005 (New): No pause for ventilation when there is an
advanced airway in place 8-10 breaths per minute

2 Rescuer CPR with Advanced Airway cont’d
2000 (Old): Recommended “asynchronous” compressions
and ventilations Ventilation rate of 12-15 per minute Rescuers taught to re-check for signs of
circulation “every few minutes”

2 Rescuer CPR with Advanced Airway cont’d Why:
Ventilations can be delivered during compressions
Avoid excessive number of breaths During CPR, blood flow to lungs decreased, so
lower than normal respiratory rate will maintain adequate oxygenation

Airway/Trauma Victims
2005 (New): In patients with suspected cervical spine injuries-if
unable to open airway using the jaw thrust, use the head-tilt chin lift
2000 (Old): Jaw thrust without head tilt taught to both lay
rescuers and healthcare providers

Airway/Trauma Victims cont’d
Why: Jaw thrust difficult maneuver to learn,may not
effectively open airway and it can cause spinal movement
Opening the airway is a priority in an unresponsive trauma victim
Manual stabilization preferred over immobilization devices during CPR

“Adequate” vs.Presence or Absence of Breathing 2005 (New): BLS healthcare provider checks for:
adequate breathing in adult victims presence or absence of breathing in children
and infants Advanced healthcare provider (with ACLS
and PALS/PEPP) will assess for adequate breathing in victims of all ages

Adequate vs. Presence or Absence of Breathing cont’d 2000 (Old):
Healthcare provider checked for adequate breathing for victims of all ages
Why: Children may demonstrate breathing patterns
(rapid, grunting) which are adequate but not normal
Assessment for adequate breathing is more consistent with advanced provider skill

Infant/Child: Give 2 Effective Breaths 2005 (New):
Attempt “a couple of times” to deliver 2 effective breaths (that cause visible chest rise)
2000 (Old): Healthcare providers were taught to move head
through a variety of positions to obtain optimal airway opening

Infant/Child: Give 2 Effective Breaths cont’d
Why: Most common mechanism of cardiac arrest in
infants and children is asphyxial Rescuer must be able to provide effective breaths

Lone Healthcare Provider-”phone first” vs. “CPR first”
2005 (New): Tailor sequence to most likely cause of
cardiac arrest “Phone First” Sudden witnessed collapse (adult or
child)-likely to be cardiac in origin. Call 9-1-1 and get the AED
“CPR First” Hypoxic Arrest (adult or child)- give 5 cycles or about 2 minutes of CPR before leaving victim to call 9-1-1 and get the AED

Lone Healthcare Provider cont’d 2000 (Old): Tailoring response to likely cause
of arrest was not emphasized in training Why:
Sudden collapse-likely cardiac and early CPR and defibrillation needed
Victims of hypoxic arrest need immediate CPR

“Child” BLS Guidelines
2005 (New): Child CPR guidelines for healthcare providers
apply to victims from 1 year of age to onset puberty (about 12-14 years old)
2000 (Old): Child CPR age 1-8

“Child” BLS cont’d
Why: No single anatomic or physiologic characteristic that
distinguishes a “child” victim from an “adult” victim No scientific evidence that identifies a precise age to begin
adult techniques

Symptomatic BradycardiaInfants/Children
2005 (New): Chest compressions indicated if HR <60 and
signs of poor perfusion, despite adequate ventilation
2000 (Old): Same recommendation in 2000 guidelines but it
was not incorporated into the BLS training

Symptomatic BradycardiaInfants/Children cont’d
Why: Bradycardia is common terminal rhythm in infants
and children
Do not want to wait for development of pulseless arrest to begin chest compressions if there are signs of poor perfusion and no improvement with 02 and ventilatory support

Child Chest Compressions
2005 (New): Use heel of 1 or 2 hands
2000 (Old): Use heel of 1 hand
Why: Child manikin study showed that rescuers
performed better chest compressions using the “adult” technique

Infant Chest Compressions
2005 (New): Use the 2 thumb-encircling technique-sternum
compressed with thumbs and use fingers to squeeze thorax
2000 (Old): Use of fingers to compress chest wall was not
described Why:
This technique results in higher coronary artery perfusion pressure

Compression to Ventilation Ratios Infants/Children
2005 (New): Lone rescuer:Compression to ventilation ratio
30:2 for infants, children and adults for 2 Rescuer CPR: 15:2 ratio for infants and
children 2000 (Old):
15:2 adults 5:1 infants/children

Compression to Ventilation Ratios Infants/Children cont’d Why:
Simplify training Reduce interruptions in chest compressions 15:2 ratio for 2 rescuer CPR for infants/children
will provide additional ventilations


Foreign Body Airway Obstruction 2005 (New):
Airway obstructions classified as mild or severe
Rescuers should act only if signs of severe obstruction present poor air exchange Increased respiratory distress Silent cough Cyanosis Inability to speak or breath

Foreign Body Airway Obstruction cont’d 2005 (New) cont’d
If victim becomes unresponsive ACTIVATE 9-1-1 and begin CPR When airway opened during CPR, look in
mouth and remove object if seen No blind finger sweeps

Foreign Body Airway Obstruction cont’d
2000 (Old): Rescuers taught to recognize
Partial obstruction with good air exchange Partial obstruction with poor air exchange Complete airway obstruction
Rescuers taught to ask 2 questions Are you choking? Can you speak?
Sequence for unresponsive choking victim was a complicated sequence/included abdominal thrusts

Foreign Body Airway Obstruction cont’d Why:
Simplification Compressions during CPR may increase
intrathoracic pressure more than abdominal thrusts
Blind finger sweeps may injure victims mouth/throat or rescuers finger

Shock /Immediate CPR
2005 (New): Delivery of single shock for VF and pulseless VT
followed by immediate CPR Perform 2 minutes of CPR before checking for
signs of circulation

Shock /Immediate CPR cont’d 2000 (Old):
3 stacked shocks recommended Why:
3 shocks were based on use of monophasic waveforms
New biphasic defibrillators have a higher first-shock success rate
3-shock sequence can result in delays up to 37 seconds or longer from delivery of shock and delivery of first post-shock compression

Monophasic Defibrillation dose 2005 (New):
Initial and subsequent shocks for VF/pulseless VT in adults 360J
2000 (Old): 200, 200-300J, 360J
Why: One dose to simplify training

Biphasic Defibrillation Dose
2005 (New): Initial shock for adults:150-200J for biphasic
truncated exponential waveform 120J for rectilinear biphasic waveform The second dose should be the same or
higher Rescuers should use the device-specific
defibrillation dose. If rescuer unfamiliar with device-specific dose-use default dose of 200J

Biphasic Defibrillation Dose cont’d 2000 (Old):
200J, 200-300J, 360J Why:
Simplify defibrillation Support use of device-specific doses

Use of AED’s in Children
2005 (New): Recommended use of AED’s in children 1-8
years old 2000 (Old):
Insufficient evidence to recommend for or against use of AED’s in children under 8 years old
Why: Evidence published since 2000 shows AED’s
safe and effective for use in infants and children

Community/Lay Rescuer AED Programs 2005 (New):
CPR/AED use by public safety first responders recommended to increase SCA survival rates
Insufficient evidence to recommend for or against AED’s in homes
2000 (Old): Key elements of an AED program included:
Physician oversight Training of rescuers Integration with EMS Process of CQI

Community/Lay Rescuer AED Programs cont’d
2005 (Why): The North American PAD trial reinforced the
importance of planned and practiced response.
Even at sites with AED’s in place- the AED’s were deployed for less than half the of the cardiac arrests at those sites indicating the need for frequent CPR


Tx of ArrhythmiasAHA 2005 Guidelines

CPR Algorithm

Pulseless Algorithm

Brady-Arryhthmias

Tachy-Arryhthymias

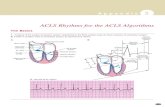
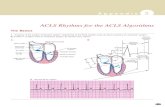
Pulseless Arrest4 Basic RhythmsShockable
V-fib
V-Tach
Non-Shockable
Asystole
PEA

Shockable Rhthyms Ventricular Tachycardia V-Fib
Shock early ABC’s
Tx of VT/VF Shock- biphashic 200j, monophasic 360j (one x) CPR-IV, ETT Shock CPR-epi/vasopressin Shock CPR-Lido/amiodarone Shock CPR-epi Shock CPR- lido/amio

NON-Shockable PEA Asystole Tx of Asystole & PEA
CPR-IV,airway Meds-vasopressin/epi CPR-2 min Meds-epi,atropine* CPR Meds-epi,atro CPR
*Atropine used in PEA, only for HR < 60

Contributing Factors H’s and T’s
Hypovolemia Hypoxia Hydrogen ion (acidosis) Hypo/hyperkalemia Hypoglycemia Hypothermia Toxins (drugs) Tamponade (cardiac) Tension PTX Thrombosis (coronary or pulmonary) Trauma

Tachycardia’sStable vs. Unstable Stable
MI 12 lead Narrow complex Wide complex Treat causes
H’s and T’s
Unstable Altered MS CP Hypotension Signs of shock

Tx of Stable Tachycardias
A-fib/flutter Vagal maneuvers Diltiazem (Ca++ channel blocker)
SVT Adenosine
V-Tach (WITH PULSE) Antiarrhythmic: Lido, Amio, (Mg+ for torsades)

Tx of Unstable Tachycardias
Perform immediate synchronized cardioversion MI Sedate if conscious DO NOT DELAY CARDIOVERSION

BradycardiasTx of Bradycardias
Stable MI Adequate perfusion? Monitor BP!!
Unstable Poor perfusion Immediate transcutaneous pacing Consider atropine while awaiting pacer Consider epi or dopamine if pacing ineffective

ACLS Class Recommendations Class I – Always do this! Class IIa – Intervention of choice. Class IIb – Give careful consideration. Class Indeterminate – Clinical judgment Class III – Not recommended!