ACLS CE -Part III of III -Defibrillation and ACLS Drug Therpy
-
Upload
imhotep-virtual-medical-school -
Category
Documents
-
view
350 -
download
2
Transcript of ACLS CE -Part III of III -Defibrillation and ACLS Drug Therpy
Defibrillation and ACLS Drug Therapy
Prepared and presented by
Marc Imhotep Cray, M.D.
ACLS CE Part III of III
http://en.wikipedia.org/wiki/Defibrillation
Defibrillation
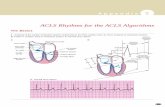
•Defibrillation is a common treatment for life-threatening cardiac dysrhythmias, ventricular fibrillation and pulseless ventricular tachycardia •Defibrillation consists of delivering a therapeutic dose of electrical energy to the heart with a device called a defibrillator •External depolarization of the heart to stop Vfib or Vtach that has not responded to other maneuvers
Defibrillation
• Know your AED*
• Universal steps:
1. Power ON
2. Attach electrode pads
3. Analyze the rhythm
4. Shock (if advised)
3
*Automated External Defibrillator
Defibrillation
• Most frequent initial rhythm in witnessed sudden cardiac arrest is ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) which rapidly deteriorates into VF
• The only effective treatment for VF is electrical defibrillation
• Probability of successful defibrillation diminishes rapidly over time
• VF rapidly converts to asystole if not treated
5
• Outcomes of Rapid Defibrillation by Security Officers after Cardiac Arrest in Casinos
• NEJM Vol 343 (17) October 26, 2000
• Used AEDs on 105 patients with Ventricular Fibrillation
• 53% survived to discharge (back to casino)
• Previously, less than 5% survive
7
Also see: Use of Automated External Defibrillators by a U.S. Airline Page LA et al. N Engl J Med 2000; 343:1210-1216
Example of deploying AEDs in a highly populated and
monitored environment…Still debates about cost effectiveness
Do AEDs work?
An AED at a railway station in Japan. The AED box has information on how to use it in Japanese, English, Chinese and Korean,
and station staff are trained to use it. http://en.wikipedia.org/wiki/File:AED_Oim
achi_06z1399sv.jpg
Public-Access Defibrillation and Survival after Out-of-Hospital Cardiac Arrest
http://www.nejm.org/doi/full/10.1056/NEJMoa040566
• Community based trial of AED deployment and layperson training.
• 30 in AED group versus 15 survivors in CPR only group to hospital discharge
• Average age of survivor - 69.8 years
• Study cost - $9.5 million
8
Study Conclusions “Training and equipping volunteers to attempt early defibrillation within a structured response system can increase the number of survivors to hospital discharge after out-of-hospital cardiac arrest in public locations. Trained
laypersons can use AEDs safely and effectively.”
Defibrillation Procedure
• Position paddles
• “Clear” the patient
• Shock and then resume CPR for 5 cycles then re-analyze after each shock
• Prepare drug therapy
– Next slides
ACLS Drug Therapy
N.B. Following is only a outlined capsule ACLS drugs,
for a details see
ACLS Core Drugs American Heart Association 2006, pdf
Routes of Administration
• Peripheral IV – easiest to insert during CPR
• Central IV – fast onset of action
• Intratracheally (down an ET tube)
• Intraosseous – alternative IV route in peds
IV Fluids
Volume Expanders
• crystalloids , e.g. Ringer’s lactate, N/S, or colloids, e.g. Albumin or Hetastarch
• TKO – D5W, N/S
Morphine Sulfate
• Drug of choice for pain
• Also decreases pre-load
• IV dose – 2-4 mg as often as every 5 minutes
• Precautions
– May cause respiratory depression
Lidocaine
• Indications:
– PVCs, Vtach, Vfib
– Can be toxic so no longer given prophylactically
• IV dose :
– 1-1.5 mg/kg bolus then continuous infusion of 2-4 mg/min
– Can be given down ET tube
• Signs of toxicity:
– slurred speech, seizures, altered consciousness
Amiodarone (Cordarone)
• Indications: – Like Lidocaine – Vtach, Vfib
• IV Dose: – 300 mg in 20-30 ml of N/S or D5W – Supplemental dose of 150 mg in 20-30 ml of N/S or
D5W – Followed with continuous infusion of 1 mg/min for 6
hours than .5mg/min to a maximum daily dose of 2 grams
• Contraindications: – Cardiogenic shock, profound Sinus Bradycardia, and
2nd and 3rd degree blocks that do not have a pacemaker
Procainamide (Pronestyl)
• Indications: – Like lidocaine (is usually a second choice) – Uncontrolled Afib or Atrial flutter if no signs of
heart failure • Dose :
– continuous IV infusion. Initially 20mg/min then titrated down to 1-4 mg/min
• Side effects – Hypotension – Widening of the QRS
Bretylium Tosylate (Bretylol)
• Indications:
– Same as lidocaine and procainamide (usually when condition doesn’t respond to these two)
• IV dose:
– 5-10mg/kg bolus followed by continuous infusion of 1-2 kg/min
• Side Effects:
– N & V
– Hypotension
Atropine • Indications:
– Symptomatic sinus bradycardia
– Second Degree Heart Block Mobitz I
– May be tried in asystole
– Organophosphate poisoning
• IV Dose:
– .5 – 1 mg every 3-5 minutes
– Max dose is .04mg/kg
– Can be given down ET tube
• Side Effects:
– May worsen ischemia
Isoproterenol (Isuprel)
• Indications: – Temporary stimulant prior to pacemaker
– Bradycardia refractory to atropine
– Torsades de Pointes refractory to magnesium sulfate
• IV dose: – Continuous infusion of 2-10 micrograms/ml of
infusion fluid
Adenosine • Indication:
– PSVT
• IV Dose:
– 6 mg bolus followed by 12 mg in 1-2 minutes if needed
• Side Effects:
– Flushing
– Dyspnea
– Chest Pain
– Sinus Brady
– PVCs
Verapamil
• Indications:
– Is a calcium channel blocker that may terminate PSVT (is a backup to Adenosine) as well as atrial flutter and uncontrolled atrial fib
• IV Dose:
– 2.5-5 mg over 2 minutes up to 20 mg
• Side Effects:
– Hypotension
– N & V
Magnesium
• Used for refractory Vfib or Vtach caused by hypomagnesemia and Torsades de Pointes
• Dose:
– 1-2 grams over 2 minutes
• Side Effects
– Hypotension
– Asystole!
Propranolol
• Beta blocker that may be useful for Vfib and Vtach that has not responded to other therapies
– Very useful for patients whose cardiac emergency was precipitated by hypertension
– Also used for Afib, Aflutter, & PSVT
Epinephrine
• Because of alpha, beta-1, and beta-2 stimulation, it increases heart rate, stroke volume and blood pressure – Helps convert fine vfib to coarse Vfib – May help in asystole – Also PEA and symptomatic bradycardia
• IV Dose: – 1 mg every 3-5 minutes – Can be given down the ET tube – Can also be given intracardiac – May increase ischemia because of increased O2
demand by the heart
Vasopressin (ADH)
• Similar effects to Epinephrine without as much cardiovascular side effects!
• IV dose = 40 IU
• Can be given down ET tube
• May be better for asystole
Norepinephrine (Levarterenol)
• Similar in effect to epinephrine
• Used for severe hypotension that is NOT due to hypovolemia
• Cardiogenic shock
• Administered as a continuous infusion
– Adult rate is usually 2-12 micrograms/min
– Range is .5-1 microgram up to 30!
• Side effects:
– Like epinephrine, it may worsen ischemia
– Extravasation causes tissue necrosis
Dopamine
• Used for hypotension (not due to hypovolemia)
– Usually tried before norepinephrine
– Has alpha, beta, and dopaminergic properties
• Dopaminergic dilates renal and mesenteric arteries
• Second choice for bradycardia (after Atropine)
• IV Dose:
– 1-20 micrograms/kg
• Side effects:
– Ectopic beats
– N & V
Dobutamine
• Actions similar to Dopamine
• Used for CHF with hypotension
• IV Dose:
– 2-20 micrograms/minute
• Side effects:
– Tachycardia
– N & V
– Headache
– Tremors
Amrinone
• Similar to dobutamine
• Used for refractory CHF
• IV Dose:
– 2-15 micrograms/kg/min
• Side effects:
– May worsen ischemia
– N & V
– Thrombocytopenia
Digitalis (Digoxin)
• Slows conduction through A-V node and increases force of contraction
• Used in CHF and chronic atrial fib/flutter
• Can be given orally or IV
• Side effects:
– Arrhythmias
– N & V, diarrhea
– Agitation
Nitroglycerin
• Vasodilator that helps relieve pain from angina pectoris
• Can be given IV, sublingually, as an ointment or a slow release patch
• Side effects:
– Headache
– Hypotension
– Syncope
– V/Q mismatch
Sodium Nitroprusside (Nipride)
• Vasodilator used for hypertensive crisis
• IV dose:
– Loading dose of 50 –100 mg followed by infusion of .5-8 micrograms/kg/min
– Is light sensitive so IV bag must be wrapped in tin foil
• Side effects:
– Hypotension so patient must have continuous hemodynamic monitoring
Sodium Bicarbonate
• Used for METABOLIC acidosis hyperkalemia – H + HCO3 >H2CO3>H2O and CO2 – Airway and ventilation have to be functional!
• IV Dose: – 1 mEq/kg – If ABGs, [BE] x wt in kg/6
• Side effects: – Metabolic alkalosis – Increased CO2 production
Thrombolytics
• Used to improve coronary blood flow by lysing clots, ie coronary thrombosis – Best if given within six hours of onset of chest pain
– Examples: TPA/Alteplase(Activase), Streptokinase
• Side effects: – Bleeding
Further study: http://www.uptodate.com/contents/advanced-cardiac-
life-support-acls-in-adults
End of ACLS CE Part III THANK YOU FOR YOUR ATTENTION