1 Randomized controlled trial of short bursts of a potent topical corticosteroid versus more...
Transcript of 1 Randomized controlled trial of short bursts of a potent topical corticosteroid versus more...

The Eleventh Meeting of BEES (British Epidermo-EpidemiologySociety)
Programme and Abstracts
09:00 Coffee and registration
09:45 The BEES Guest Overseas Lecture Atopic disease: should we be looking within?
Prof. Bengt Bjorksten, Sweden
10:30 *Randomized controlled trial of short bursts of a potent topical corticosteroid versus more prolonged use of a mild preparation for childrenwith atopic eczema
Dr Kim Thomas, Nottingham
10:45 *Are patients satisfied with a teledermatology consultation?Dr John English, Nottingham
11:00 Tea/Coffee
11:30 Complexity theory and dermatology waiting listsDr. Dominic Smethurst, Nottingham
12:15 *Severe cutaneous adverse reactions: time latency between beginning of drug use and onset of reaction
Dr Maja Mockenhaupt, Germany
12:30 Lunch
14:00 Action on dermatology past and future
Mr Nicholas Evans, NHS Modernisation Agency
14:45 *A cost-effectiveness rationale for the selection of antimicrobial therapy in acne: a randomized controlled trial
Ms Mara Ozolins, Nottingham
15:00 The future of electronic publishing
Dr. Richard Smith, British Medical Journal
15:45 Meeting ends
15:45 AGM for BEES Members Only
Lunchtime/coffee breaks: Poster/database presentation
Use of an electronic cancer registry in a district general hospital
Dr Tessa Frost and Dr Andrew Warin
*Denotes submitted abstract.
British Journal of Dermatology 2002; 146: 541–543.
Ó 2002 British Association of Dermatologists 541

Abstracts
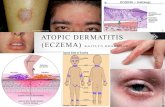
1Randomized controlled trial of short bursts of a potent topical
corticosteroid versus more prolonged use of a mild prepara-
tion for children with atopic eczema
K.THOMAS, H.WILLIAMS, S.ARMSTRONG, C.O’NEILL,* T.AVERY,A.LI WAN PO, J.THOMAS
University of Nottingham U.K.
School of Public Policy, Law and Economics, University of Ulster, U.K.*Centre for Evidence-Based Pharmacotherapy, Aston University, U.K.
Aims This study aimed to determine whether a 3-day burst of a potent
steroid is more effective than a weak preparation used for 7 days in
treating disease exacerbations and in maintaining remissions inchildren with atopic eczema.
Methods A randomized, double-blind, parallel group study of
18 weeks’ duration. 174 patients with mild or moderate atopic
eczema were recruitment from 13 general practices in the Notting-ham area. Two primary outcomes were evaluated: (i) the total
number of scratch-free days and (ii) the number of disease relapses.
Secondary outcomes included the median duration of the 1st diseaserelapse; the number of nights when sleep was not disturbed; disease
severity (SASSAD), two quality-of-life measures (CLQI and DFI) and
the number of treatment ÔfailuresÕ in each arm. Skin thickness was
measured using B-mode ultrasound.Results We found no differences between the two groups for any of
the outcome measures used. The median number of scratch free days
was 118.0 for the hydrocortisone group and 117.5 for the beta-
methasone valerate group (95% CI median difference )2–4,P ¼ 0.53). The median number of relapses for both groups was 1.
Both groups showed clinically significant improvements in disease
severity and quality-of-life compared to baseline. No significantchanges in skin thickness were observed.
Conclusions For children with mild or moderate atopic eczema in the
community, both 1% hydrocortisone used for 7 days, or betameth-
asone valerate 0.1% used for 3 days, are effective in controlling dis-ease symptoms.
2Are patients satisfied with a teledermatology consultation?
R.STOCKLEY, J.ENGLISH, A.MORRIS AND R.EMERSON
Department of Dermatology, Queen’s Medical Centre, Nottingham NG7
2UH, U.K.Background Many dermatologists have expressed concerns about the
development of teledermatology. It is a radical shift from the tradi-
tional face-to-face consultation with the dermatologist as the GPtakes digital images of the patient’s skin condition and emails them
with the history to the consultant dermatologist for his or her opin-
ion. The dermatologist emails the opinion back to the GP who then
informs the patient. The objective of this study was to see if thepatients who had undergone a teledermatology consultation were
satisfied with the service. This was an attempt to involve patients in
the decision-making process regarding the development of a new
health care service.Methods A postal questionnaire was sent to the first 180 patients of
the teledermatology pilot service. 114 (64% response rate) were
returned, 52 (46%) of patients did not require a hospital attendance
and 62 (54%) did.
Questionnaire
Prefer to use the telederm service or wait to see the dermatologist face to face?
Prefer to wait for hospital consultation rather than use the telederm service if
this meant a much longer wait?
Would you use the telederm service again?
Satisfied or very satisfied with the telederm service (had to choose one of five
options)
Did NOT require hospital visit
64% yes
21% yes
98% yes
80%
Did require hospital visit
49% yes
19% yes
87% yes
64%
Results and Conclusions There were some differences in the responses
between those patients that required a hospital visit and those that
did not. A traditional face-to-face consultation would have beenpreferred by 20% of patients . The patients that did attend hospital
seemed to have a preference for traditional face-to-face consultation
compared those that did not attend hospital but nearly 90% of all
patients returning the questionnaire would use the service again.
3
Severe cutaneous adverse reactions time latency betweenbeginning of drug use and onset of reaction
M.MOCKENHAUPT, J.SCHLINGMANN AND E.SCHOPF
Dokumentationszentrum schwerer Hautreaktionen (dZh), Department ofDermatology, University of Freiburg, Germany
Background Toxic epidermal necrolysis (TEN) and Stevens–Johnson
syndrome (SJS) are acute life-threatening severe cutaneous adverse
reactions (SCAR) with an unclear pathogenesis mainly caused bydrugs. Allopurinol and trimethoprim ⁄ sulphamethoxazole (TMS) are
both well known to be associated with these conditions. In addition,
TMS is known to induce generalized bullous fixed drug eruption
(GBFDE), a less severe condition with a very short induction periodthat is clinically often confused with SJS or TEN.
Aim We want to further investigate the risk profile of allopurinol and
TMS for inducing SCAR, as the hazard functions of these substances
are different. Furthermore, the re-review of cases using more specificcriteria to differentiate between SCAR and GBFDE should allow us to
detect misclassification of cases.
Methods 984 cases of SJS, SJS ⁄ TEN overlap and TEN were ascertainedby a population-based registry between 1990 and 1999. The fol-
lowing analysis is based on a random sample of 115 cases earlier
accepted as SJS or TEN, which were exposed to either allopurinol or
TMS, and 38 cases excluded in the previous review. An independentexpert committee blinded for possible causes re-reviewed these
cases in clinical terms, as the original review process took place
over a period of 10 years. In this analysis special emphasis is given
to the time latency between beginning of drug use and onset ofSCAR.
5 4 2 A B S T R A C T S
Ó 2002 British Association of Dermatologists, British Journal of Dermatology, 146, 541–543

Results Before re-review 162 ⁄ 984 patients with SCAR reported the
use of allopurinol and 131 ⁄ 984 the use of TMS within 2 weeks priorto the onset of the adverse reaction. After the re-review the per-
centage of doubtful cases was higher for TMS (28 ⁄ 57) than for
allopurinol (30 ⁄ 83). For definite cases of SJS or TEN the range
between the lower and upper quartile of the time latency betweenbeginning of drug use and onset of SCAR was 14–34 days for allo-
purinol, in contrast to 5–15 days for TMS. The time latency for
doubtful and excluded cases after the use of TMS was much shorter(2.5 and 2 days, respectively).
Conclusions The high numberof doubtful cases after the re-review
reveals the difficulty of applying approved detailed definitions to the
variety of clinical patterns of cutaneous adverse reactions. We couldconfirm a high correlation of time latency between beginning of drug
use and onset of SCAR and GBFDE for allopurinol and TMS, which
may have an important impact on the risk profile of these and other
suspected drugs, as well as on pathogenetic and therapeutic consid-erations of severe adverse events. When drug exposure occurs outside
the relevant interval of time latency for SJS and TEN, other risk fac-
tors and ⁄ or differential diagnoses such as GBFDE should be consid-ered.
4A cost-effectiveness rationale for the selection of antimicro-
bial therapy in acne: a randomized controlled trial
M.OZOLINS,* E.A.EADY, A.AVERY,* W.J.CUNLIFFE, A.LI WAN
PO,à C.O’NEILL,** N.B.SIMPSON,– C.E.WALTERS, E.CARNEGIE, J.B.LEWIS, J.DADA, M.HAYNES,* K.WILLIAMS* AND
H.C.WILLIAMS
*University of Nottingham, U.K.
Department of Microbiology, University of Leeds, U.K.àCentre forEvidence-Based Pharmacotherapy, Aston University, U.K.
§School of Public Policy Law and Economics, University of Ulster, U.K.
–Department of Dermatology, Royal Victoria Infirmary, Newcastle, U.K.
** Dermatology, Leeds General Infirmary U.K.Background This NHS ⁄ HTA-funded study aimed to rank five com-
monly used antimicrobial therapies for acne in order of their clinical
effectiveness and cost-effectiveness. We also wanted to identify which
agents are less likely to promote resistance and those which areeffective in patients who harbour high numbers of resistant Propi-
onibacterium acnes strains.
Methods From surgeries and colleges in the Nottingham and Leedsareas, 649 patients with mild to moderate facial acne were recruited.
The two primary outcome measures were patient self-assessment of
improvement in overall acne severity and reduction in inflamed
lesion count, measured at 18 weeks. Secondary outcome measuresincluded two acne severity scores, assessors’ global estimation of
improvement, quality of life and utility scores, enumeration of anti-
biotic resistant propionibacteria, and the incidence of adverse events.
Results and Conclusions The most effective treatments (percentagewith at least moderate improvement according to patients, mean
change in lesion count) were the topical BenzamycinÒ b.d. (66%,
) 27) and its components given separately (topical erythromycino.d. + 5% benzoyl peroxide o.d.) (63%, ) 26), followed by 5% benzoyl
peroxide b.d. (60%, ) 23). The least effective were oral oxytetracy-
cline (55%, ) 18) and minocycline (54%, ) 22). The most cost-
effective treatment was benzoyl peroxide and least cost-effective wasminocycline. In terms of quality of life, benzoyl peroxide moved down
the rankings and minocycline moved up. The two topical erythro-
mycin-containing regimens produced the largest reductions and the
oral treatments the smallest in the prevalence and population densityof cutaneous propionibacteria. Prior bacterial colonisation did not
affect outcome in the topical groups. Efficacy of both oral preparations
was influenced by tetracycline resistant P. acnes strains.
Disclaimer The views and opinions expressed are those of the authorsand do not necessarily reflect those of the Department of Health.
Poster/database presentation
5
Use of an electronic cancer registry in a district general hos-
pitalT.A.FROST AND A. WARIN
Dermatology Department, Royal Devon & Exeter Hospital, Barrack Road,
Exeter EX2 5DW, U.K.Background Skin cancers from a large proportion of UK Dermatologists’
work are inaccurately recorded. Increasingly we are expected to audit
our work for quality and timeliness of diagnosis and treatment.
Methods Since the beginning of 2000 we have incorporated the use ofa database in our day-to-day work to record clinical and management
details of all nonmelanoma skin cancers treated in the Dermatology
outpatients clinic. Malignant melanoma detected in our Health
Authority area have been recorded since 1987. The same databasesystem can be used as an epidemiological tool or to follow the progress
of individual patients through follow-up data. Whenever a person is
alive as defined through a confirmed R D & E contact this fact is
automatically entered onto the database, allowing our mortalitytables to be reasonably accurate. We are in control of the data entry
and are able to check for accuracy against histological records on a
regular quarterly basis, demonstrating unequivocally how in-
accurate are Regional Cancer Registries. We monitor waiting timesof patients, numbers and types of procedures and activity of different
doctors.
Results Since 1987 malignant melanoma has increased from 20 per100 000–30 per 100 000 with a marked change in gender inci-
dence. The major increase has been in early and in situ melanoma,
except in men where we show a disturbing increase in invasive
lesions. In Exeter half the nonmelanoma skin cancers come to us withthe site and age range as expected. As time goes on we should get a
good idea of our recurrence rate. Thus far, this is not a large pro-
portion of our work, but we have no idea how much goes to the
plastic surgeons. In addition, there are fairly small numbers needingflaps, grafts, second procedures or referral on to surgeons.
Results The case for increased resourcing can be easily supported by
reports generated in a timely manner by such a system.
A B S T R A C T S 5 4 3
Ó 2002 British Association of Dermatologists, British Journal of Dermatology, 146, 541–543