Syncope
-
Upload
smsraza -
Category
Health & Medicine
-
view
2.083 -
download
0
description
Transcript of Syncope

SYNCOPE: WHAT SYNCOPE: WHAT HAPPENS WHEN YOUR HAPPENS WHEN YOUR
LIGHTS GO OUT LIGHTS GO OUT ??
Syed RazaSyed RazaMD,MRCP (UK),FCCP, Dip.Card (UK)MD,MRCP (UK),FCCP, Dip.Card (UK)

COMMON SCENARIO !COMMON SCENARIO !
Elderly lady Elderly lady Lives aloneLives alone Collapse at home Collapse at home ? LOC? LOC No eye witnessNo eye witness Patient does not remember the eventPatient does not remember the event

Mrs L, 64yo F
66yo F
,
Mrs K, 59yo F
Case Case Mrs M, 85yo F









ObjectivesObjectives
DefinitionDefinition PrevalencePrevalence Diagnostic Work UpDiagnostic Work Up ManagementManagement Implications on drivingImplications on driving

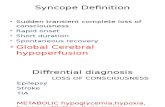
Syncope:Syncope:A Symptom, Not a DiagnosisA Symptom, Not a Diagnosis
Syncope:Syncope:A Symptom, Not a DiagnosisA Symptom, Not a Diagnosis
Self-limited loss of consciousness and Self-limited loss of consciousness and postural tonepostural tone
Relatively rapid onsetRelatively rapid onset Variable warning symptomsVariable warning symptoms Spontaneous, complete, and usually prompt Spontaneous, complete, and usually prompt
recovery without medical or surgical recovery without medical or surgical interventionintervention
Lipsitz 1983Lipsitz 1983
Underlying mechanism: Underlying mechanism: transient global cerebral hypoperfusion.transient global cerebral hypoperfusion.

Impact of SyncopeImpact of Syncope
1Kenny RA, Kapoor WN. In: Benditt D, et al. eds. The Evaluation and Treatment of Syncope. Futura;2003:23-27.2Kapoor W. Medicine. 1990;69:160-175.
3Brignole M, et al. Europace. 2003;5:293-298.4 Blanc J-J, et al. Eur Heart J. 2002;23:815-820.5Campbell A, et al. Age and Ageing. 1981;10:264-270.
40% will experience syncope at least once in a lifetime1
1-6% of hospital admissions2
1% of emergency room visits per year3,4
10% of falls by elderly are due to syncope5
Major morbidity reported in 6%1
eg, fractures, motor vehicle accidents
Minor injury in 29%1
eg, lacerations, bruises

THE COSTTHE COST
More than 1 billion pounds per year spent More than 1 billion pounds per year spent by NHS for managing falls and syncope.by NHS for managing falls and syncope.
Significant portion of the budget is spent Significant portion of the budget is spent onon
clinical conditions which have been clinical conditions which have been misdiagnosed ( i.e. 10% of syncope misdiagnosed ( i.e. 10% of syncope diagnosed as epilepsy)diagnosed as epilepsy)

Incidence Rates of Syncope According to Age and Sex
Soteriades, E. et al. N Engl J Med 2002;347:878-885


ClassificationClassification
Syncope
Neurally Mediated 34%VasovagalCarotid SinusSituationalGlossopharyngeal NeuralgiaCerebrovascularAutonomic Failure
Cardiac Mediated 18%ArrythmiaSrtructural Heart DiseaseCardiopulmonary Disease
Others 47%Orthostatic HypotensionIdiopathicMedicationsPsychiatric

Causes of syncope*
Neurally mediated 50%
Cardiac arrhythmia 11%
Orthostatic hypotension 6%
Structural cardiopulmonary 3%
Unknown 9%
* Data pooled from 4 population studies n=1640 patients

Neurally Mediated Neurally Mediated SyncopeSyncope
Neuro cardiogenic syncope Neuro cardiogenic syncope Carotid sinus hypersensitivityCarotid sinus hypersensitivity Visceral syncope (micturition, Visceral syncope (micturition,
cough, defecation etc.)cough, defecation etc.) Glossopharyngeal neuralgia Glossopharyngeal neuralgia

Neurally Mediated Neurally Mediated SyncopeSyncope
(autonomic failure)(autonomic failure) Orthostatic /Postural HypotensionOrthostatic /Postural Hypotension
Postural Orthostatic Tachycardia Postural Orthostatic Tachycardia Syndrome (POTS)Syndrome (POTS)

Neuro-Cardiogenic Neuro-Cardiogenic SyncopeSyncope
Commonest cause of syncope Commonest cause of syncope Most frequently in 30 - 50 age groupMost frequently in 30 - 50 age group Typical triggers - pain, fear, blood etcTypical triggers - pain, fear, blood etc Prodromal symptoms- warmth, nausea, Prodromal symptoms- warmth, nausea,
sweatingsweating Good history is key to diagnosisGood history is key to diagnosis Usually does not require fancy Usually does not require fancy
investigationsinvestigations Patient may be discharged the same dayPatient may be discharged the same day

PathophysiologyPathophysiology
Neuro-cardiovascular reflexes severely Neuro-cardiovascular reflexes severely impaired or absent.impaired or absent.
Pooling of 500-800 ml blood in distensible Pooling of 500-800 ml blood in distensible blood vessels of legs on prolonged standing.blood vessels of legs on prolonged standing.
Reduced venous return and cardiac output.Reduced venous return and cardiac output. Reduced brain perfusion.Reduced brain perfusion. Warning signals to brain impairedWarning signals to brain impaired Patient presents with pre syncope or Patient presents with pre syncope or
syncopesyncope

Carotid Sinus SyndromeCarotid Sinus Syndrome
Common in elderly/atherosclerotic ds.Common in elderly/atherosclerotic ds. Sensitive baro receptors at carotid bodySensitive baro receptors at carotid body Any pressure i.e. sudden neck turningAny pressure i.e. sudden neck turning
or tight collar /shavingor tight collar /shaving slowing of heart rate and fall in blood slowing of heart rate and fall in blood
pressurepressure Poor brain perfusion → SyncopePoor brain perfusion → Syncope

Carotid Sinus Syncope and Autonomic Dysfunction
Freeman, M. Neurogenic Orthostatic Hypotension. NEJM 2008; 358: 616


POSTURAL BPPOSTURAL BP


Postural Blood PressurePostural Blood Pressure
Sadly NOT accurately measuredSadly NOT accurately measured Supine position –at least 10 minutesSupine position –at least 10 minutes Standing/SittingStanding/Sitting Measure BP immediately, 1 minute , 3 Measure BP immediately, 1 minute , 3
minutesminutes
Symptoms of pre-syncope or syncopeSymptoms of pre-syncope or syncope Fall in systolic BP by 30 mmHg AND Fall in systolic BP by 30 mmHg AND
diastolic BP by 20 mmHgdiastolic BP by 20 mmHg..

Orthostatic HypotensionOrthostatic Hypotension
Common in elderlyCommon in elderly
most vulnerablemost vulnerable ↓ ↓ Baro receptor sensitivityBaro receptor sensitivity Reduced thirst mechanismReduced thirst mechanism Poly pharmacyPoly pharmacy
Peripheral sympathetic tone Peripheral sympathetic tone impairmentimpairment
Diabetic neuropathy, antihypertensive Diabetic neuropathy, antihypertensive medicationmedication

POSTURAL ORTHOSTATIC POSTURAL ORTHOSTATIC TACHYCARDIA SYNDROME TACHYCARDIA SYNDROME
(POTS)(POTS)Patients ( women 15-50)Patients ( women 15-50)
dizziness or faint on acquiring sudden erect dizziness or faint on acquiring sudden erect postureposture
Reduced volume of blood reaches the heartReduced volume of blood reaches the heart Stimulation of mechano receptors causes Stimulation of mechano receptors causes
tachycardiatachycardia Heart rate increases by more than 30 Heart rate increases by more than 30
beats/min.beats/min. Heart rate usually above 120 /minute.Heart rate usually above 120 /minute.

Initial evaluation: HistoryInitial evaluation: History
Prior to eventPrior to event
Position, activity, situation (urinating etc)Position, activity, situation (urinating etc)
predisposing factors (crowded, warm place etc)predisposing factors (crowded, warm place etc)
precipitating events (fear, pain, neck movements)precipitating events (fear, pain, neck movements)
Onset of eventOnset of event
nausea, vomiting, sweating, aura, nausea, vomiting, sweating, aura,
About event (eye witness)About event (eye witness)
Colour, duration, movements, tongue bitingColour, duration, movements, tongue biting
After the eventAfter the eventnausea, vomiting, sweating, confusion, muscle ache, skin nausea, vomiting, sweating, confusion, muscle ache, skin colour, woundscolour, wounds

Diagnostic testsDiagnostic tests
Carotid sinus massageCarotid sinus massage
Tilt testingTilt testing
Others; EP testing, signal averaged (V) Others; EP testing, signal averaged (V) ECG, Echocardiography, ETT, cardiac ECG, Echocardiography, ETT, cardiac catheterisation, neurological/psychiatric catheterisation, neurological/psychiatric evaluation,evaluation,

Carotid Sinus Massage Carotid Sinus Massage ProtocolProtocol
Massage longitudinally, site of maximal impulse, Massage longitudinally, site of maximal impulse, anterior margin SCM muscle level of cricoid anterior margin SCM muscle level of cricoid cartilagecartilage
5 –10 seconds, right first, then left after 1-2 5 –10 seconds, right first, then left after 1-2 minute break (minute break (Newcastle protocol 10secsNewcastle protocol 10secs))
Continuous ECG and BP monitoring mandatoryContinuous ECG and BP monitoring mandatory
Neurological complication in 0.45% in a series of Neurological complication in 0.45% in a series of 1600 patients (5secs massage)1600 patients (5secs massage)

Carotid Sinus MassageCarotid Sinus Massage
Stimulation of hypersensitive carotid body can produce 3 main responses
Cardio-inhibitory response (70%)
Vasodepressor response (10%)
Mixed (20%)

Positive CSM TestPositive CSM Test
Significant brady /more than 3 s Significant brady /more than 3 s pause on the ECG pause on the ECG
More than 50 mmHg fall in systolic More than 50 mmHg fall in systolic BP BP
Mixed response Mixed response

TILT TABLE TESTTILT TABLE TEST

Tilt Table Test In ActionTilt Table Test In Action

Indications for Tilt Table Indications for Tilt Table TestingTesting
Unexplained recurrent syncopeUnexplained recurrent syncope
Assessment of recurrent, unexplained Assessment of recurrent, unexplained fallfall
Syncope with suspected autonomic Syncope with suspected autonomic failurefailure
After a cardiac cause for syncope has After a cardiac cause for syncope has been excludedbeen excluded

Upright Tilt Table TestUpright Tilt Table Test
Measure HR and Measure HR and BP while tilting BP while tilting them uprightthem upright
Attempt to elicit Attempt to elicit symptomssymptoms

Tilt Table TestingTilt Table Testing
Supine at least 20 minutes prior to tiltSupine at least 20 minutes prior to tilt Tilt angle 70 degreesTilt angle 70 degrees Passive phase min 20 to 45 minutesPassive phase min 20 to 45 minutes Use either intravenous isoprenaline or Use either intravenous isoprenaline or
sublingual GTN if passive phase is sublingual GTN if passive phase is negativenegative
Pharmacological phase – 15 to 20 minutesPharmacological phase – 15 to 20 minutes End-point: induction syncope End-point: induction syncope

Normal test

Cardioinhibitory response Cardioinhibitory response

Vasodepressor responseVasodepressor responseBP drops from 150/70 to 50/30 but BP drops from 150/70 to 50/30 but
heart rate stays sameheart rate stays same

Mixed responseMixed responseBP drops from 150/60 to 50/20 BP drops from 150/60 to 50/20
while HR drops from 65 to 30bpmwhile HR drops from 65 to 30bpm


Orthostatic hypotensionOrthostatic hypotensionsteady drop in BP and rise in HRsteady drop in BP and rise in HR

Heart Monitoring OptionsHeart Monitoring OptionsSyncope Occurs Infrequently, Syncope Occurs Infrequently,
Long-term Monitoring is Likely to be Most Long-term Monitoring is Likely to be Most EffectiveEffective
Heart Monitoring OptionsHeart Monitoring OptionsSyncope Occurs Infrequently, Syncope Occurs Infrequently,
Long-term Monitoring is Likely to be Most Long-term Monitoring is Likely to be Most EffectiveEffective
ILRILR
MCOT MCOT ExternalExternal
Loop Loop RecorderRecorder
Typical EventTypical EventRecorderRecorder
Holter Holter MonitorMonitor
12-Lead12-Lead
2 Days2 Days
7 Days7 Days
30+ Days30+ Days
36 Months36 Months
10 Seconds10 Seconds
ILR = insertable loop recorderILR = insertable loop recorder
MCOT= mobile cardiac outpatient telemetryMCOT= mobile cardiac outpatient telemetry


Everything is spinningEverything is spinning

MANAGEMENTMANAGEMENT
Patient education and counsellingPatient education and counselling Avoid triggersAvoid triggers Increase in salt and fluid intakeIncrease in salt and fluid intake Sleeping with the head of the bed Sleeping with the head of the bed
raised (6-12 inches.raised (6-12 inches. Elastic stockingsElastic stockings Preventing LOC or InjuryPreventing LOC or Injury
Assume supine position upon onset of prodromeAssume supine position upon onset of prodrome Avoid driving or other activities that could lead Avoid driving or other activities that could lead
to injuryto injury

Pharmacological therapyPharmacological therapy
Beta blockersBeta blockers DysopyramideDysopyramide FludrocortisoneFludrocortisone SSRIsSSRIs MidodrineMidodrine

Management of Neurally Management of Neurally Mediated SyncopeMediated Syncope
Grubb BP. NEJM. 2005. 352(10): 1004-1010

INDICATION FOR INDICATION FOR PACEMAKER PACEMAKER
Syncope with cardio inhibitory or Syncope with cardio inhibitory or
mixed (cardio-inhibitory plus mixed (cardio-inhibitory plus vasodepressor).vasodepressor).
Severe brady cardia, AV or SA Severe brady cardia, AV or SA blockblock
Over drive pacing for some tachy Over drive pacing for some tachy arrhythmia.arrhythmia.

• Non-random, observational
• RCTs comparing vs
• RCTs comparing vs
What are the indications for What are the indications for pacemaker therapy in pacemaker therapy in
neurocardiogenic syncope?neurocardiogenic syncope?

2727 dual-chamber dual-chamber pacemakerspacemakers
with rate-drop with rate-drop responseresponse
54 pts54 pts2727 No pacemaker No pacemaker
Included• >6 lifetime episodes• + tilt-table test
– (relative bradycardia)
Primary outcome: first recurrence of syncope
Pacemaker No pacemaker
Recurrence of Syncope
6/27 (22%) 19/27 (70%)
Time to recurrence
112 days 54 days
Excluded• Vascular, coronary,
myocardial or conduction system disease
The North American The North American Vasovagal Pacemaker Study Vasovagal Pacemaker Study
(VPS)(VPS)
J. Am. Coll Cardiol. 1999;33:16-20

Soteriades E et al. N Engl J Med 2002;347:878-885
Overall Survival of Participants with Syncope, According to Cause, and Participants without Syncope

Driving ImplicationsDriving ImplicationsGroup 1 EntitlementGroup 1 Entitlement Group 2 EntitlementGroup 2 Entitlement
Simple faint –definite Simple faint –definite provocation with provocation with prodromal symptomsprodromal symptoms
No driving restrictionsNo driving restrictions No driving restrictionsNo driving restrictions
Unexplained syncope Unexplained syncope with low risk of with low risk of recurrencerecurrence
Can drive 4 weeks after Can drive 4 weeks after the eventthe event
Can drive 3 months Can drive 3 months after the eventafter the event
Unexplained syncope Unexplained syncope & high risk of & high risk of recurrencerecurrence
A abnormal ECGA abnormal ECG
B structural heart B structural heart diseasedisease
C syncope at the C syncope at the wheel or results in wheel or results in injuryinjury
D more than 1 D more than 1 episode in last 6 episode in last 6 monthsmonths
Can drive 4 weeks after Can drive 4 weeks after the event if cause the event if cause identified and treatedidentified and treated
If no cause – 6 months If no cause – 6 months offoff
Can drive after 3 Can drive after 3 months if the cause months if the cause identified and treatedidentified and treated
If no cause, licence If no cause, licence revoked for yearrevoked for year
Loss of Loss of consciousness with consciousness with no clinical pointersno clinical pointers
Full neuro/cardiac Ix Full neuro/cardiac Ix with no pointerswith no pointers
Licence revoked for 6 Licence revoked for 6 monthsmonths
Licence revoked for 1 Licence revoked for 1 yearyear
Cough syncopeCough syncope Stop driving until Stop driving until symptoms controlledsymptoms controlled
Stop drivingStop driving
If smokes or If smokes or respiratory disease respiratory disease have to be controlled have to be controlled for 5 yearsfor 5 years

SUMMARYSUMMARY
Syncope is not an uncommon problemSyncope is not an uncommon problem The diagnosis of syncope is often The diagnosis of syncope is often
missed or it is misdiagnosedmissed or it is misdiagnosed Thorough history from eye witness can Thorough history from eye witness can
be very helpfulbe very helpful Syncope can be fatalSyncope can be fatal Further training to identify the Further training to identify the
problem and formulating a plan of problem and formulating a plan of management is needed.management is needed.


ANY QUESTION ??ANY QUESTION ??