Safety Surfactant in Sepsis-Induced Respiratory Distress Syndrome · 2010. 5. 17. ·...
Transcript of Safety Surfactant in Sepsis-Induced Respiratory Distress Syndrome · 2010. 5. 17. ·...

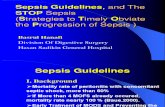
Safety and Potential Efficacyof an Aerosolized Surfactantin Human Sepsis-InducedAdult Respiratory Distress SyndromeJohn G. Weg, MD; Robert A. Balk, MD; R. Steven Tharratt, MD; Stephen G. Jenkinson, MD; Jagdip B. Shah, MD;David Zaccardelli, PharmD; John Horton; Edward N. Pattishall, MD; for the Exosurf ARDS Sepsis Study Group
Objective.\p=m-\Toevaluate the safety and potential efficacy of aerosolized surfac-tant in intubated patients with adult respiratory distress syndrome (ARDS).
Design.\p=m-\Aprospective, double-blind, placebo-controlled, randomized, parallel,mutlicenter pilot clinical trial.
Patients.\p=m-\Atotal of 51 patients with sepsis-induced ARDS were entered into thestudy within 18 hours of developing sepsis or sepsis syndrome.
Intervention.\p=m-\Patientswere randomized into four treatment groups in a 2:1:2:1ratio, as follows: 12 hours of surfactant per day, 12 hours of 0.6% saline per day,24 hours of surfactant per day, and 24 hours of 0.6% saline per day. Surfactant orsaline was aerosolized continuously for up to 5 days using an in-line nebulizer thataerosolized only during inspiration.
Main Outcome Measures.\p=m-\Ventilatorydata, arterial blood gases, and hemo-dynamic parameters were measured at baseline, every 4 or 8 hours during the 5days of treatment, 24 hours after treatment, and 30 days after treatment, at whichtime mortality was also assessed. Safety was evaluated throughout the 30 days ofthe study.
Results.\p=m-\Surfactantwas administered safely in ventilated patients when givencontinuously throughout the 5 days using the nebulizer system. Although there wereno differences in any physiological parameter between the treatment groups, therewas a dose-dependent trend in reduction of mortality from 47% in the combinedplacebo group to 41% and 35% in the groups treated with 12 hours and 24 hoursof surfactant per day, respectively.
Conclusions.\p=m-\Aerosolizedsurfactant was well tolerated when administered ona continuous basis for up to 5 days; however, at the doses given, it did not resultin significant improvements in patients with sepsis-induced ARDS.
(JAMA. 1994;272:1433-1438)
From the Pulmonary and Critical Care Medicine Di-vision, Department of Internal Medicine, University ofMichigan Medical Center, Ann Arbor (Dr Weg); theDepartment of Pulmonary and Critical Care Medicine,Rush-Presbyterian-St Luke's Medical Center, Chicago,Ill (Dr Balk); the Division of Pulmonary and Critical CareMedicine, University of California\p=m-\DavisMedical Cen-ter, Sacramento (Dr Tharratt); the Pulmonary DiseaseSection, Audie L. Murphy Veterans Affairs Hospital,San Antonio, Tex (Dr Jenkinson); the Department ofAnesthesiology, Medical College of Virginia, Richmond
(Dr Shah); and the Clinical Research Division, Bur-roughs Wellcome Co, Research Triangle Park, NC (DrsZaccardelli and Pattishall and Mr Horton).
A complete list of members of the Exosurf ARDSSepsis Study Group appears at the end of this article.
Reprint requests to the Pulmonary and Critical CareMedicine Division, Department of Internal Medicine,University of Michigan Medical Center, Room B1H245\x=req-\0026,1500 E Medical Center Dr, Ann Arbor, Ml 48109\x=req-\0026 (Dr Weg).
ALTHOUGH partially described by a
variety of names for many years, adultrespiratory distress syndrome (ARDS)first was described clearly in 1967.1 Thissyndrome has been associated with ex¬
traordinarily diverse predisposing andetiologic factors, including sepsis or sep¬sis syndrome, gastric aspiration, trauma,heroin and other drug overdose, mul¬tiple transfusions, fat emboli, chemicalor smoke inhalation, burns, disseminatedintravascular coagulation, viral pneumo¬nia, pancreatitis, drug reactions, andnear drowning.2 Following insult to thepulmonary capillary endothelium and/or the alveolar epithelium, high perme¬ability pulmonary edema develops, thechest roentgenogram shows diffuse bi¬lateral infiltrates, lung compliance falls,and extravascular lung water increasesin the absence of left-sided heart fail¬ure.3 Hypoxemia persists despite highconcentrations of supplemental oxygendue to intrapulmonary shunting.4 Al¬though intrapulmonary shunting can bedecreased with various ventilatory ma¬
nipulations, including positive end-ex¬piratory pressure, this often leads to adiminished cardiac output, which can im¬peril tissue oxygen delivery and utili¬zation.6 Despite increasingly complexmodes ofmechanical ventilation, sophis¬ticated respiratory and hemodynamicmonitoring, and a continually expand¬ing array ofpotent antibiotics, the over¬all mortality is estimated to have re¬mained at 40% to 50% for the last twodecades, and mortality increases pre¬cipitously with each organ that fails.6"9
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from

Even use of extracorporeal membraneoxygénation in prospective randomizedtrials has failed to reduce mortality.9·10
The similarity between ARDS andneonatal respiratory distress syndrome(NRDS) was noted in the first descrip¬tion of ARDS, and surfactant deficiencywas postulated as a common mechanismof dysfunction.1 In both disorders, thereis refractory hypoxemia, decreased lungcompliance, bilateral infiltrates on chestroentgenogram, hyaline membrane for¬mation, and surfactant dysfunction.11 Ithas already been demonstrated that sur¬factant replacement therapy reducesmortality and morbidity in NRDS.1213There is compelling evidence that sur¬factant replacement has a role in treat¬ment of ARDS.
Numerous animal models of ARDSthat examined a variety of injuriesclearly demonstrate that surfactant dys¬function is present.14"16 Rapid injury, suchas with antilung serum infusion, andmore prolonged injury, such as oxygentoxicity, result in physiological changessimilar to those seen in ARDS, and bothare also associated with surfactant dys¬function.1718 Surfactant replacementtherapy improves physiology and sur¬vival in these animal models similar tothat seen in NRDS.15,19
Surfactant dysfunction is also presentin humans with ARDS. Patients withtrauma-induced ARDS have surfactantdysfunction in proportion to the sever¬
ity of their disease.20 Surfactant dys¬function is also present in patients atrisk of developing ARDS, and increas¬ing dysfunction is seen in patients whoproceed to develop ARDS.21
Surfactant therapy for ARDS in hu¬mans has been limited to a few case
reports where surfactant was used innonrandomized, open-label fashion.2224These anecdotal reports describe re¬markable benefits in some patients.These results are encouraging and ingeneral support the role of surfactantdysfunction as a component of ARDS.
The purpose of this pilot study was toevaluate aerosolized surfactant replace¬ment therapy in a multicenter, random¬ized, double-blind, placebo-controlleddose comparison in patients with sepsis-induced ARDS. The objectives were toevaluate the safety and potential effi¬cacy of continuously aerosolized syn¬thetic surfactant in intubated patientswith ARDS in preparation for a larger,definitive trial.
METHODSDesign
This study was a double-blind, pla¬cebo-controlled, multicenter, random¬ized, parallel-design, pilot-dose compari-
son of the effect of aerosolized surfac¬tant or saline on sepsis-induced ARDS.Patients were randomized in a 2:1:2:1ratio, respectively, into the following fourtreatment groups: 12 hours of aerosol¬ized surfactant per day (Surf-12), 12hours of aerosolized 0.6% saline per day(placebo), 24 hours of aerosolized sur¬factant per day (Surf-24), and 24 hoursof aerosolized 0.6% saline per day (pla¬cebo). Randomization was performed bya central office at the time of entry,using an interactive computer programthat maintained comparable numbers en¬tered into all groups at each site andacross all sites. The study consisted of a
screening phase, a 5-day treatmentphase, a 24-hour posttreatment phase,and a 30-day follow-up. The study wascarried out in 20 tertiary care medicalcenters throughout the United Statesand was approved by the institutionalreview board of each institution.
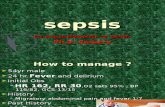
PatientsPatients who met the following cri¬
teria were eligible for the study: (1) malesor females age 5 years or older; (2) in¬tubation and mechanical ventilation; (3)presence of a pulmonary balloon-flota¬tion catheter; (4) clinical evidence ofARDS as defined by both a hypoxemiaratio (partial pressure of oxygen, arte¬rial/fraction of inspired oxygen [PacVFl02]) from 50 through 299 and diffusebilateral infiltrates on chest roentgeno-gram; and (5) sepsis as documented bya positive blood culture, or sepsis syn¬drome as recently defined25 as high clini¬cal suspicion of infection, core tempera¬ture greater than 38.3°C (not requiredif receiving antipyretics) or less than35.6° C, heart rate greater than 90 beatsper minute (not required if the patientwas receiving beta blockers or calciumchannel blockers) and respirations great¬er than 20 breaths per minute, and evi¬dence of inadequate perfusion by oneof the following: hypoxemia, Pa02 lessthan 75 mm Hg with an Fi02 of 21% notdue to chronic lung disease, elevatedserum lactate, change in mental status,or decrease in urine output to less than30 mL/h for 2 hours despite fluid re¬
placement. Patients were required toenter the study within 18 hours of theidentification of sepsis or sepsis syn¬drome.
Patients were excluded from the studyfor any of the following reasons: (1) elec-trocardiographic evidence of coronaryartery ischemia or infarction, or a pul¬monary capillary wedge pressure great¬er than 22 mm Hg; (2) bacterial pneu¬monia, Pneumocystis carinii infection,or other compromising pulmonary in¬fections; (3) renal failure defined as se¬rum creatinine level of 220 prnol/L (2.5
mg/dL) or more or sustained oliguria forgreater than 2 hours (urine output <30mL/h for adults and <0.5 mL per kilo¬gram of body weight per hour for chil¬dren <18 years old); (4) hepatic failuredefined as a bilirubin level greater than86 µ /L (5.0 mg/dL), or alanine ami-notransferase or aspartate aminotrans-ferase greater than five times the upperlimit of normal; (5) patients known tohave acquired immunodeficiency syn¬drome; (6) pregnancy; (7) chronic medi¬cation for chronic obstructive lung dis¬ease, asthma, or emphysema; and (8)any physiological or psychological con¬dition other than ARDS that contrain-dicated the administration ofsurfactant.
General AssessmentsThe following general assessments to
evaluate safety and potential efficacywere obtained on entrance into thestudy: a thorough medical history, thor¬ough physical examination, electrocar¬diogram, hématologie evaluation (hemo¬globin, hematocrit, white blood cell countand differential, platelet count, and redblood cell count and composition), bloodchemistries (albumin, alkaline phos¬phate, calcium, carbon dioxide, chloride,cholesterol, creatinine, glucose, lacticacid, lactic dehydrogenate, phosphorus,potassium, sodium, total protein, triglyc¬éride, -glutamyltransaminase, alanineaminotransferase, aspartate aminotrans-ferase, total bilirubin, urea, and uricacid), urinalysis (pH, glucose, ketones,protein, bilirubin, and blood), APACHEII (Acute Physiology and Chronic HealthEvaluation II) score, a chest roentgeno¬gram, and cultures of blood and otherappropriate sites. These assessmentswere repeated within the 24-hour pe¬riod after aerosolization had been dis¬continued and 30 days after the studybegan. The number of days of hospital-ization were evaluated at hospital dis¬charge or at 30 days. Chest roentgeno-grams were evaluated by a single radi¬ologist blinded to the treatment group.Mortality was assessed 30 days aftertreatment began, and the cause ofdeathwas documented.
The patient was continuously moni¬tored for any adverse experiences, whichwere rated according to intensity, seri¬ousness, and causality to study drug. Anadverse experience was defined as anyuntoward outcome and was rated as at¬tributable to the study if, in the inves¬tigator's judgment, it might be relatedto the study drug or its delivery or wouldnot be expected in patients with ARDSrelated to sepsis. The investigator re¬corded each adverse event, including anestimate of duration, intensity, serious¬ness, causality, and interventions un¬dertaken.
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from

Respiratory and HemodynamicAssessments
Respiratory and hemodynamic assess¬ments were also obtained to evaluatesafety and potential efficacy. At base¬line, every 4 hours, and when the nebu¬lizer was turned off and on throughoutthe 5-day treatment period, the follow¬ing ventilatory data were obtained: in¬tubation status, Fl02, ventilator mode,positive end-expiratory pressure, peakinspiratory pressure, tidal volume, pla¬teau pressure, and respiratory rate.From these data, the dynamic and staticrespiratory system compliance was cal¬culated. The number of days the patientwas on mechanical ventilation duringthe 30 days of the study was also re¬corded.
At baseline and every 4 hours duringthe treatment period, the following wereobtained: hypoxemia ratio (Pa02/Fl02),temperature, hemodynamic data (heartrate, pulmonary capillary wedge pres¬sure, mean right atrial pressure, andthe systolic, diastolic, and mean arterialand pulmonary artery blood pressures),arterial blood gas, and mixed venousblood gas. From these data, the alveolar-arterial oxygen gradient (P[A-a]02), ar¬terial/alveolar oxygen ratio (PaC>2/PA02),shunt fraction, arteriovenous oxygen dif¬ference, and lung injury score were cal¬culated. Thermodilution cardiac outputwas determined every 8 hours duringtreatment and used in determining thesystemic oxygen transport.
All hemodynamic and respiratory pa¬rameters were repeated every 4 hoursfor 24 hours after discontinuation oftreatment. These parameters were re¬
peated at the 30-day follow-up if thepatient was still being ventilated and a
pulmonary balloon-flotation catheterwas in place. If not ventilated, spirom-etry, lung volumes, and single breathcarbon monoxide diffusing capacity wereobtained.
Surfactant AdministrationThe surfactant administered in this
study (Exosurf, Burroughs WellcomeCo, Research Triangle Park, NC) is a
synthetic surfactant developed by Clem¬ents.26 It is a mixture ofdipalmitoyl phos-phatidylcholine (DPPC), cetyl alcohol(hexadecanol), tyloxapol, and sodiumchloride, with a ratio of 13.5:1.5:1.0:5.8,respectively. The surfactant was formu¬lated as a sterile lyophilized powder andcontains 13.5 mg of DPPC per milliliterafter reconstitution with sterile water.
After randomization, the pharmacistplaced 175 mL of surfactant or 0.6% sa¬line in an opaque nebulizer (TriNeb, Vor-tran Medical Technology Ine, Sacra¬mento, Calif); a new canister was used
every 4 hours and was weighed beforeand after use. The nebulizer producesparticles with a mass median diameterof approximately 2.2 µ . Surfactant orsaline was aerosolized continuously forup to 5 days using an in-line nebulizer(VISAN, Vortran Medical TechnologyIne) that aerosolized only during inspi¬ration.27 The air flow through the nebu¬lizer was set to deliver approximatelyone half of the tidal volume.
Statistical MethodsThe objectives of this study were to
evaluate the safety and potential effi¬cacy of continuously aerosolized syn¬thetic surfactant in preparation for a
larger, definitive trial. Thus, no samplesize or power calculations were done a
priori.There were no differences in results
between the two placebo groups (12- and24-hour administration of 0.6% saline perday). Thus, the placebo groups were com¬bined for all subsequent analyses.
Presenting medical histories andphysical examinations were tabulatedand compared for intergroup differences.Changes in physiological parametersduring the treatment period were com¬
pared using an average area under thecurve (AAUC). The AAUC was derivedby plotting the physiological data col¬lected repeatedly every 4 hours duringthe treatment period, baseline (hour 0)through hour 120, with the parameteron the y-axis and time on the x-axis.Area under the curve (AUC) was thencalculated for each patient's data. Sincethe AUC values would be large and notmeaningful to the clinician, the individualpatient AUCs were then divided by 120hours of treatment to yield a more fa¬miliar and meaningful value (AAUC).For patients not receiving the full 120hours of treatment, the last recordedvalue was carried forward to lessen theimpact on the AUC for patients whodid not complete the entire 5 days oftreatment and to better represent theirultimate status (success or failure)throughout the study. Change from base¬line AAUC was calculated by subtract¬ing each patient's baseline values fromtheir AAUC. Nonparametric confidenceintervals (CIs) based on Wilcoxon'sRank-Sum Test28 were constructed forthe comparison ofthe change from base¬line AAUC values between the com¬bined placebo groups and the surfactant-treated groups. Nonparametric inter¬vals based on Wilcoxon's Sign-Rank Testwere constructed on the change frombaseline AAUC data to detect changeover time.
Mortality was assessed using Fish¬er's Exact Test for survival at 30 days.This analysis was selected because the
hypothesis of choice is a change in sur¬vival rate rather than an increase insurvival time. Roentgenograms were
categorized according to the degree ofconsolidation, atelectasis, hyperinflation,and effusion using a numeric score from0 (none) to 3 (severe) in all five lobes. Inaddition, a general overall score of im¬provement or worsening was comparedbetween groups. The number of days onmechanical ventilation, in the intensivecare unit, receiving supplemental oxy¬gen, and in the hospital were displayedusing Kaplan-Meier plots.
In addition to evaluation of all physi¬ological parameters for worsening,safety was also evaluated by the inci¬dence of adverse experiences, expectedcomplications of ARDS, and new physi¬cal examination abnormalities or newdiseases identified during treatment orthe follow-up period, using 95% CIs.Changes from baseline for hematologyand clinical chemistry parameters were
compared using nonparametric 95% CIsand on difference between treatmentgroups and the placebo group.
RESULTSPatient Demographics,Accountability, andSurfactant Dosage
Fifty-one patients were entered intothe study: 17 in the combined placebogroup, and 17 in each surfactant-treatedgroup. Other than a preponderance offemales in the placebo group and malesin the Surf-24 group, there were no no¬table differences between groups in age,smoking history, body temperature,mean systemic arterial blood pressure,or APACHE II score (Table 1). Atscreening, blood cultures with gram-positive organisms were found in twopatients in the placebo group, none inthe Surf-12 group, and one in the Surf-24 group; gram-negative organisms werefound in three patients in the Surf-24group. The major pulmonary physiologi¬cal parameters were not statistically dif¬ferent between all groups at baseline(Table 2).
There were 10,12, and 12 patients inthe placebo, Surf-12, and Surf-24 groups,respectively, who completed a full 5 daysof treatment. Reasons for not complet¬ing the full course of therapy includedmechanical ventilation discontinued insix patients (two in each group), deathin three patients (one in each treatmentgroup), adverse experiences unrelatedto the study in three patients (one in theplacebo group and two in the Surf-12group), attending physician clinical de¬cision to change to a ventilation mode orventilator incompatible with the nebu¬lizer in two patients (one each in the
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from

Table 1.—Demographic and Baseline Characteristics
Characteristic
Treatment Group*Placebo Surf-12
Surf-24
No. of Patients 17
SexFemaleMale 14
Mean (±SD) age, y 51 (±19) 51 (±20) 53 (±17)Current smokers, % 41 53 41Mean (±SD) body temperature, °C 38.0 (±0.7) 38.4 (±0.8) 38.2 (±1.0)Mean (±SD) systemic arterial blood pressure,
mm Hg 80.0 (±21) 79.7 (±15.2) 75.0 (±12.0)Mean APACHE lit score 14.2 (±6.4) 16.5 (±6.7) 15.7 (±6.6)
The placebo group received 0.6% saline for 12 or 24 hours per day; Surf-12 and Surf-24 indicate patients whoreceived surfactant for 12 and 24 hours per day, respectively.
+APACHE II indicates Acute Physiology and Chronic Health Evaluation II.
Table 2.—Mean Values and Average Area Under the Curve for Change From Baseline for Major PhysiologicParameters*
ParameterTreatmentf
GroupBaseline,Mean (SE)
AAUCChange From Baseline,
Mean (SE)Shunt fraction, % Placebo
Surf-12Surf-24
32.6 (3.8)34.1 (2.8)31.5(3.4)
-3.9 (3.7)-8.1 (2.3)+.-3.7(1.9)
Fl02, % Placebo
Surg-12Surf-24
66.5 (5.6)68.2 (3.5)68.8 (4.9)
-7.6 (5.0)-10.6(4.5)+.-12.9(4.6)+
PaOz/Fio2 ratio Placebo
Surf-12Surf-24
146.5(20.4)124.2(11.8)161.5(16.2)
44.0(17.1)+42.2 (9.3)+.22.8(13.6)
P(A-a)o2, mm Hg
P(a/A)o2, mm Hg
Placebo
Surf-12Surf-24Placebo
Surf-12Surf-24
352.3 (43.6)357.2 (25.0)335.1 (33.2)
0.2 (0.04)0.2 (0.02)0.3 (0.03)
-81.7(36.8)+.-70.3 (32.8)-82.5 (29.6)+.
0.08 (0.03)+.0.07 (0.02)+.0.05 (0.02)
PEEP, mm Hg PlaceboSurf-12
Surf-24
9.1 (1.0)10.0(1.4)11.3(1.1)
1.0 (0.9)1.4(0.8)0.5(1.3)
PIP, mm Hg PlaceboSurg-12Surf-24
42.4(3.1)47.0 (3.2)42.3 (2.5)
3.7 (2.3)1.9(2.4)0.8 (2.2)
Compliance, mlVcm H20Static Placebo
Surf-12Surf-24
32.0 (2.6)30.8(3.1)37.1 (2.7)
-0.2(1.4)1.3(2.2)0.2(2.1)
Dynamic PlaceboSurf-12
Surf-24
26.0 (2.2)23.8(1.8)29.4 (2.4)
-1.9(1.4)0.3(1.2)
-0.3(1.8)*AAUC indicates average area under the curve; Fio2, fraction of inspired oxygen; Pao2, partial pressure of oxygen,
arterial; Pao2, partial pressure of oxygen in the alveoli; P(A-a)o2, alveolar-arterial difference in partial pressure ofoxygen; P(a/A)o2, arterial/alveolar oxygen ratio; PEEP, positive end-expiratory pressure; and PIP, peak insplratorypressure.
tThe placebo group recleved 0.6% saline for 12 or 24 hours per day; Surf-12 and Surf-24 indicates patients whoreceived surfactant for 12 and 24 hours per day, respectively.
¿Statistically significant change from baseline ( P<.05).
placebo and Surf-24 groups), nebulizer/ventilator malfunction in two patients(both in the placebo group), and a timingerror after 4.5 days in one patient in theSurf-24 group.
The mean (±SD) amount of surfactantaerosolized (based on nebulizer weightchanges) over the entire 5 days was 568.4(±53.6) g in the Surf-12 group and 1128.4(±99.3) g in the Surf-24 group. This is
the equivalent ofapproximately 21.9 and43.5 mg per kilogram per day of DPPCin the Surf-12 and Surf-24 groups, re¬
spectively. The amount of aerosol actu¬ally deposited would be a small fractionof that aerosolized.29
SafetyIn general, the continuous nebuliza-
tion of surfactant or 0.6% saline for up
Survival of the patient groups treated with 0.6% sa¬line for 12 and 24 hours per day (Placebo), surfac¬tant for 12 hours per day (Surf-12), and surfactantfor 24 hours per day (Surf-24) throughout the 30days of the study.
to 5 days for either 12 or 24 hours perday was extremely well tolerated. How¬ever, pneumothorax occured in one pa¬tient in the Surf-12 group, presumablydue to partial occlusion of the ventilatorexhalation bacteria filter with aerosolparticles. Another patient in the Surf-24 group had clonus of unknown causethat resolved spontaneously while con¬
tinuing surfactant therapy.Comparisons within the placebo group
given 0.6% saline for 12 hours per dayshowed no changes in any parameterswhile on or off therapy.30 In addition,there were no differences between pa¬tients in the placebo group treated 12hours per day compared with those givenplacebo 24 hours per day. Thus, nebu-lization of 0.6% saline appeared to haveno adverse effects.
There were no consistent deteriora¬tions in blood chemistry and hémato¬logie values during treatment within or
among the placebo, Surf-12, or Surf-24groups. There also were no differencesbetween groups in use of concomitantdrug therapy, including acetaminophen,antibacterials, antifungals, antihyperten-sives, antivirals, aspirin, bronchodilators,glucocorticoids, mineralocorticoids, ibu-profen, indomethacin, paralytic agents,sedatives, or vasopressive agents. Re¬sults of most electrocardiograms wereabnormal at baseline, and there were noconsistent changes during treatmentwithin or among treatment groups. Simi¬larly, there were no consistent changesin physical findings or medical historiesduring treatment among treatmentgroups.
EfficacyAlthough the major objective was to
assess safety, potential efficacy was alsoevaluated. There was a rank order de¬crease in mortality at 30 days with a
mortality of 47%, 41%, and 35% in theplacebo, Surf-12, and Surf-24 groups, re¬
spectively (Figure). At 14 days, mortal¬ity was 35%, 24%, and 24% in the pla¬cebo, Surf-12, and Surf-24 groups, re-
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from

spectively. At 10 days, the mortality was
29%, 18%, and 6% in the placebo, Surf-12, and Surf-24 groups, respectively.These changes were not statistically sig¬nificant. With the number of patients ineach treatment group, there was 10%power (ß=.9, =.05) to detect a differ¬ence in mortality between 47% in theplacebo group and 37% in each treat¬ment group. The causes of death werenot notably different between groups,with multisystem organ failure and over¬
whelming sepsis with cardiovascular col¬lapse as the most common causes ofdeath. Respiratory failure was listed asthe cause of death in one patient fromthe placebo group and two patients fromthe Surf-24 group.
The mean baseline and mean AAUCchange from baseline for the major physi¬ological values are shown in Table 2.Comparingwithin each treatment group,there were statistically significant im¬provements from baseline in Pa02/Fl02,P(A-a)02, and P(a/A)o2 in the placebogroup, shunt fraction, Pa02/Fl02, Fl02,and P(a/A)02 in the Surf-12 group, andP(A-a)02 and Fl02 in the Surf-24 group.In comparison between treatmentgroups, there were no significant dif¬ferences seen. All groups had similarchanges in positive end-expiratory pres¬sure and compliance, and although notshown in the table, there were no dif¬ferences in other pulmonary and hemo-dynamic assessments, such as peak in-spiratory pressure, arteriovenous oxy¬gen difference, pulmonary capillarywedge pressure, and cardiac output.
The number of days in the hospitalwas not significantly different betweenthe treatment groups. Similarly, therewere no significant differences in im¬provement ofchest roentgenograms be¬tween the treatment groups.COMMENT
This first placebo-controlled clinicaltrial of the effects of surfactant replace¬ment therapy in patients with ARDSindicates that aerosolized surfactant issafe when given to intubated, mechani¬cally ventilated patients. The safety ofaerosolized surfactant therapy givenwith each breath continuously for up to5 days is evident by the lack of anydetrimental laboratory changes and thefew adverse events recorded duringtherapy. There was one pneumothoraxcaused by increased airway pressuresdue to partial occlusion of the ventilatorexhalation bacteria filter. Caution mustbe taken when aerosolizing largeamounts of drug into a ventilatory cir¬cuit; use ofspecially designed equipmentis required.31
Although improvement in the surfac¬tant-treated groups was not dramatic,
the trends in mortality in this pilot studyare encouraging. The trends appear tobe greater when evaluated earlier aftertreatment. The difference between the10-day and 30-day mortality may indi¬cate the importance of late, nonrespi-ratory causes of death, although therewere no differences in causes of mor¬
tality identified in the study.The mechanism of action for a poten¬
tial reduction in mortality includes thesurface tension-lowering capability andthe antiedemic effects of surfactant.However, other mechanisms of actionmay also play a role. For example, sur¬factant causes a dose-dependent inhibi¬tion of interleukin-1, interleukin-6, andtumor necrosis factor release from stimu¬lated human macrophages in vitro.32 Amarked concentration-dependent sup¬pression ofphytohemagluttinin-inducedimmunoglobulin has also been demon¬strated.33 These and as yet unreportedmediations of the ongoing systemic in¬flammatory reaction that underliesARDS or multiple organ dysfunctionsyndrome may account for an importantcomponent of the potential therapeuticefficacy of surfactant replacement.
The lack ofeffect on physiology in thispilot trial could be attributed to the lackof a role of surfactant in ARDS, use ofan inappropriate surfactant, use of aero¬sol delivery, or an inappropriate doseachieved. The rationale for surfactantreplacement in ARDS is supported bymany human and animal studies.11·15"24The surfactant used has proven to besafe and effective in extensive studiesin NRDS.12·13 Aerosol delivery of sur¬factant was chosen because it is lessinvasive than delivering a large intra-tracheal bolus. After aerosolization, sur¬factant remains functional, and in ani¬mal models, aerosolized surfactant hasbeen more efficacious than liquid bolusdelivery in an adult lung model.34 Thenebulizer used in this study produces a
relatively homogenous particle size dis¬tribution with a mass median diameterof approximately 2.2 pm.27 This particlesize should give adequate deposition tothe alveolar regions of the lung.
Most studies in animal models ofARDS have used a bolus of 100 mg ofDPPC per kilogram as an effective dose;however, aerosolization may be moreefficient than bolus instillation and thebeneficial dose required for aerosol ap¬plication has not been established. Theamount aerosolized in this study was
approximately 44 mg of DPPC per ki¬logram per day. The actual amount de¬posited in the lung would be expected tobe similar to other aerosolized drugs inintubated patients, or 2% to 5% of thataerosolized.28 Thus, a likely reason forlack of effectiveness is the small dose
delivered to the alveolar space. Inacti-vation by serum proteins can be over¬come by increasing the dose of surfac¬tant:0 Therefore, more profound effectson mortality and pulmonary physiologymay be seen with higher doses of sur¬factant.
Patients with sepsis-induced ARDSwere used in this study because sepsisis one of the most common causes ofARDS, results in a high mortality rate,and decreases the variability that wouldoccur by including multiple causes ofARDS. Although patients with sepsismay not be homogeneous, the variabil¬ity in response would be increased fur¬ther using patients with other causes ofARDS. The definition used meets re¬cent American College of Chest Physi¬cians-Society of Critical Care MedicineConsensus Conference guidelines for thedefinitions of sepsis for the use of inno¬vative therapies in sepsis.36 The PaOVFl02 ratio and the pulmonary capillarywedge pressure criteria used were pur¬posefully chosen to be more inclusivethan those used in previous studies, sincesurfactant therapy should be useful inmilder forms of ARDS or ARDS com¬
plicated with mildly elevated pulmonarycapillary wedge pressure.
Previous studies have not been ran¬domized or placebo-controlled. Random¬ization to a concurrent control groupwas essential for comparisons in thisstudy. The control group received 0.6%saline through the same nebulizer sys¬tem to control for potential effects fromthe nebulizer, to help maintain the blind¬ing of treatment group assignment, andto have a similar salt content as thesurfactant suspension. Although aero-solization of saline may have some ef¬fects on pulmonary function, the 30-daymortality of47% in the placebo group issimilar to other studies ofsepsis-inducedARDS or sepsis,37 and there were noeffects of aerosolization of 0.6% salineseen in the placebo groups when ana¬
lyzed separately.30Although surfactant therapy in pa¬
tients with sepsis-induced ARDS did notresult in any statistically significant dif¬ferences in this pilot study, it is likelythat the dose achieved was not largeenough to counteract the inhibitors pre¬sent in the lungs in patients with ARDS.A controlled trial with more patientsusing larger doses of surfactant may bemore effective.
The members of the Exosurf ARDS SepsisStudy Group were as follows: Timothy E. Albert-son, MD, University of California-Davis MedicalCenter, Sacramento; EdgarJ. Caldwell, MD, MaineMedical Center, Portland; Stephen G. Jenkinson,MD, Audie L. Murphy VA Hospital, San Antonio,Tex; Robert A. Balk, MD, Rush-Presbyterian-StLuke's Medical Center, Chicago, 111; Neil R. Mac-Intyre, MD, Duke University, Durham, NC; An-
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from

thony A. Meyer, MD, University ofNorth Carolina,Chapel Hill; John G. Weg, MD, University ofMichigan Medical Center, Ann Arbor; AnthonyKillian, MD, West Pennsylvania Hospital, Pitts¬burgh; Spencer K. Koerner, MD, Cedars SinaiMedical Center, Los Angeles, Calif; Henry J.Silverman, MD, University of Maryland Hospital,Baltimore; Paul N. Lanken, MD, University ofPennsylvania Hospital, Philadelphia; Daniel P.
Schuster, MD, Washington University School ofMedicine, St Louis, Mo; John H. Siegel, MD, Mary¬land Institute of Emergency Medical Systems Ser¬vices, University of Maryland, Baltimore; John A.Weigelt, MD, University of Texas, SouthwesternMedical Center, Dallas; James H. Williams, MD,University of California-Irvine Medical Center,Orange; Warren R. Summer, MD, Louisiana StateUniversity School of Medicine, New Orleans; Leo
C. Roteilo, MD, SUNY Health Science Center,Syracuse, NY; Steven G. Peters, MD, Mayo Clinic,Rochester, Minn; Donald J. Schölten, MD, Butter-worth Hospital, Grand Rapids, Mich; Paul A. Kear¬ney, MD, University of Kentucky Chandler Medi¬cal Center, Lexington; and H. David Reines, MD,Medical College of Virginia, Richmond.
Support for this project was provided by Bur¬roughs Wellcome Co, Research Triangle Park, NC.
References1. Ashbaugh DG, Bigelow DB, Petty TL, LevineBE. Acute respiratory distress in adults. Lancet.1967;2:319-323.2. Fowler AA, Hamman RF, Good JT, et al. Adultrespiratory distress syndrome: risk with common
predispositions. Ann Intern Med. 1983;98:593-597.3. Rinaldo JE, Rogers RM. Adult respiratory dis-tress syndrome: changing concepts of lung injuryand repair. N Engl J Med. 1982;306:900-909.4. Dantzker DR, Brook CJ, DeHart P, Lynch JP,Weg JG. Ventilation perfusion distribution in theadult respiratory distress syndrome. Am Rev RespirDis. 1979;120:1039-1052.5. Weg JG. Oxygen transport in adult respiratorydistress syndrome and other acute circulatory prob-lems: relationship of oxygen delivery and oxygenconsumption. Crit Care Med. 1991;19:650-657.6. Montgomery AB, Stager MA, Carrico CJ, Hud-son LD. Causes of mortality in patients with adultrespiratory distress syndrome. Am Rev RespirDis.1985;132:485-489.7. Bernard GR, Bradley RB. Adult respiratory dis-tress syndrome: diagnosis and management. HeartLung. 1986;15:250-255.8. Hyers TM, Fowler AA. Adult respiratory dis-tress syndrome: causes, morbidity and mortality.Fed Proc. 1986;45:25-29.9. National Heart, Lung, and Blood Institute, Di-vision of Lung Diseases. Extracorporeal Supportfor Respiratory Insufficiency. Bethesda, Md: Na-tional Institutes of Health; 1979:243-245.10. Morris AH, Wallace CJ, Clemmer TP, et al.Final report: computerized protocol controlled clini-cal trial ofnew therapy which includes ECCO2R forARDS. Am Rev Respir Dis. 1992;145:A60.11. Merritt TA, Hallman M, Spragg R, Heldt GP,Gilliard N. Exogenous surfactant treatments forneonatal respiratory distress syndrome and theirpotential role in the adult respiratory distress syn-drome. Drugs. 1989;38:591-611.12. Long W, Corbet A, Cotton R, et al. A controlledtrial of synthetic surfactant in infants weighing1250 g or more with respiratory distress syndrome.N Engl J Med. 1991;325:1696-1703.13. Horbar JD, Wright EC, Onstad L, et al. De-creasing mortality associated with the introductionof surfactant therapy: an observational study of
neonates weighing 601 to 1300 grams at birth. Pe-diatrics. 1993;92:191-196.14. Hallman M. Lung surfactant in respiratory dis-tress syndrome. Acta Anaesthesiol Scand. 1991;35(suppl 95):15-21.15. Lewis JF, Jobe AH. Surfactant and the adultrespiratory distress syndrome. Am Rev RespirDis.1993;147:218-233.16. Holm BA, Matalon S. Role of pulmonary sur-factant in the development and treatment of adultrespiratory distress syndrome. Anesth Analg. 1989;69:805-818.17. Lachmann B, Hallman M, Bergmann KC. Res-piratory failure following anti-lung serum: study onmechanisms associated with surfactant system dam-age. Exp Lung Res. 1987;12:163-180.18. Holm BA, Notter RH, Leary JF, Matalon S.Alveolar epithelial changes in rabbits after a 21-dayexposure to 60% O2. J Appi Physiol. 1987;62:2230\x=req-\2236.19. Holm BA, Notter RH. Surfactant therapy inadult respiratory distress syndrome and lung in-jury. In: Holm BA, Notter RH, eds. SurfactantReplacement Therapy. New York, NY: Alan R LissInc; 1989:273-304.20. Pison U, Obertacke U, Brand M, et al. Alteredpulmonary surfactant in uncomplicated and septi-cemia-complicated courses ofacute respiratory fail-ure. J Trauma. 1990;30:19-26.21. Gregory TJ, Longmore WJ, Moxley MA, et al.Surfactant chemical composition and biophysicalactivity in acute respiratory distress syndrome.J Clin Invest. 1991;88:1976-1981.22. Richman PS, Spragg RG, Robertson B, MerrittTA, Curstedt T. The adult respiratory distress syn-drome: first trials with surfactant replacement. EurRespir J. 1989;2(suppl 3):109S-111S.23. Lachmann B. Animal models and clinical pilotstudies of surfactant replacement in adult respira-tory distress syndrome. Eur Respir J. 1989;2(suppl3):98S-103S.24. Chan CYJ, Barton TL, Rasch D. Colfosceril inan infant with adult respiratory distress syndrome.Clin Pharm. 1992;11:880-882.25. Bone RC, Fisher CJ Jr, Clemmer TP, et al.Sepsis syndrome: a valid clinical entity. Crit CareMed. 1989;17:389-393.
26. Durand DJ, Clyman RI, Heymann MA, et al.Effects of a protein-free, synthetic surfactant onthe survival and pulmonary function of pretermlambs. J Pediatr. 1985;107:775-780.27. Raabe OG, Lee JIC, Wong GA. A signal actu-ated nebulizer for use with breathing machines.J Aerosol Med. 1989;2:201-210.28. Hollander M, Wolfe DA. Nonparametric Sta-tistical Method. New York, NY: John Wiley & SonsInc; 1973.29. MacIntyre NR, Silver RM, Miller CW, SchulerF, Coleman E. Aerosol delivery in intubated, me-
chanically ventilated patients. Crit Care Med. 1985;13:81-84.30. Pattishall E, Williams J, Zaccardelli D, et al.The effect of exposure to intermittent vs continu-ous nebulization of 0.6% saline in patients withARDS. Am Rev Respir Dis. 1992;145:A79.31. Haas CF, Weg JG, Kettell CW, Caldwell EJ,Zaccardelli DS, Brown DL. Effects of dense, high\x=req-\volume, artificial surfactant aerosol on a heatedexhalation filter system. Crit Care Med. 1993;21:125-130.32. Thomassen MJ, Meeker DP, Antal JM, Con-nors MJ, Wiedemann HP. Synthetic surfactant (Exo-surf) inhibits endotoxin-stimulated cytokine secre-tion by human alveolar macrophages. Am J RespirCell Mol Biol. 1992;7:257-260.33. Bartmann P, Gortner L, Pohlandt F, Jaeger H.In vitro lymphocyte functions in the presence ofbovine surfactant and its phospholipid fractions.J Perinat Med. 1992;20:189-196.34. Lewis J, Ikegami M, Higuchi R, Jobe A, Ab-solom D. Nebulized vs instilled exogenous surfac-tant in an adult lung injury model. J Appl Physiol.1991;71:1270-1276.35. Fuchimukai T, Fujiwara T, Takahashi A, En-horning G. Artificial pulmonary surfactant inhib-ited by proteins. J Appl Physiol. 1987;62:429-437.36. Bone RC, Balk RA, Cerra FB, et al. Definitionsfor sepsis and organ failure and guidelines for theuse of innovative therapies in sepsis. Chest. 1992;101:1644-1655.37. Bone RC. Toward an epidemiology and naturalhistory of SIRS (systemic inflammatory responsesyndrome). JAMA. 1992;268:3452-3455.
at University of British Columbia Library on May 6, 2010 www.jama.comDownloaded from