Renal Physiology Lecture 2012
-
Upload
farida-maksum-lz -
Category
Documents
-
view
20 -
download
1
description
Transcript of Renal Physiology Lecture 2012
-
Renal & Body Fluids Module:PHYSIOLOGY OF THE UROPOIETIC SYSTEMMinarma SiagianBagian Ilmu FaalIKDU-FKUI
-
Why?
-
Overview of functionsRegulation of body fluid osmolality & volume:Excretion of water and NaCl is regulated interacting with CV, endocrine, CNSRegulation of electrolyte balance:Daily intake of inorganic ions (Na+, K+, Cl-, HCO3-, H+, Ca2+, Mg+ & PO43-) should be matched by daily excretion through kidneys.Regulation of acid-base balance:Kidneys work in concert with lungs to regulate the pH in a narrow limits of buffers within body fluids.
-
Overview of functionsExcretion of metabolic products & foreign substances:
urea from amino acid metabolismuric acid from nucleic acidscreatinine from musclesend products of hemoglobin metabolismhormone metabolitesforeign substances (e.g., drugs, pesticides, & other chemicals ingested in the food)
-
Production and secretion of hormones:renin (activates the renin-angiotensin-aldosterone system, thus regulating blood pressure & Na,K balance)prostaglandins/kinins (bradykinin = vasoactive, leading to modulation of renal blood flow & along with angiotensin II affect the systemic blood flow)1,25-dihydroxyvitamin D3 (stimulates Ca2+ resorption & bone deposit)erythropoietin (stimulates red blood cell formation by bone marrow).Overview of functions
-
STRUCTUREMACROSCOPICCortexMedulla
MICROSCOPIC
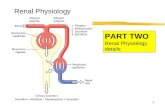
Funtional unit : NEPHRONCortical nephronJuxtamedullary nephronGlomerulus (Bowman caps. + glomerular capillary)Tubules (Proximal T. + Loop of Henle + Distal T. )Collecting DuctsJuxtaglomerular apparatusAfferent + efferent arteriolesPeritubular capillary - vasa recta
-
NEPHRON
-
Structure of Tubular Cells
-
Juxtaglomerular Apparatus
-
Renal VascularizationAbd Ao renal a interlobar a arcuate a interlobular a (cort radial a) afferent ale glomerular cap afferent ale peritubule kap (vasa recta) venules veins renal v IVC RA
How does this system affect PGC?
-
Autoregulationlocal & fast regulation of afferent/efferent ale :miogenicTubuloglomerular feedbackonly effective within a certain rangeNot completeNot effective if BP < 70 or > 200 mmHgRPF can still change through sympathetic control or A II
-
Autoregulation0.54080120160200240(mmHg)1.01.5RPF (L/min)Range of autoregulation
-
renal press. P GC renal a press. GFR flow thru prox tub & AH distal delivery of fluid (macula densa) [Na] in mac densa secr vasoconst (?) by JGA to aff ale constr aff aleTUBULOGLOMERULAR FEEDBACK
-
Three general processes determine the composition and volume of urine:Glomerular filtration (cf. renal clearance)Reabsorption of the substance from the tubular fluid into bloodSecretion of the substance from the blood into the tubular fluid
-
Plasma in glomerular cap Glomerular Membrane Ultrafiltrate ( plasma protein)Membran Filtrasi:Endothelial cells of glomerular cap (fenestra, mesangial cells)Lamina basalis (extracell matrix - glikoprotein negatively charged)Epithelial cells of Bowmans caps (podocytes - filtration slits) Affected by:Filtration PressureFiltration surface areaPermeability of filtration membraneGlomerular Filtration
-
FILTRATIONsel mesangial
-
Systemic blood vessels:artery capillary veinRenal vessels portal system: afferent ale capillary efferent alePGC (BP) maintained high afferent ale > efferent ale
Filtration without reabsorptionGlomerular Filtration
-
.arteriolevenulecapillaryFiltration
-
PCap Filtr press arteriolevenulecapillaryfiltr reabsorb Filtration
-
afferent aleefferent aleglom capGlomerular Filtration
-
PGCFiltr press afferent aleefferent aleglom capFiltration Glomerular Filtration
-
Forces Involved in Glomerular Filtration
Glomerular CapillaryBlood Pressure+55Plasma Colloid Osmotic Pressure-301510Bowmans CapsuleHydrostatic Pressure -Net Filtration Pressure+
-
604020001glomerular capPP (mmHg)Hydrostatic Pressure (P) and Oncotic Pressure () in glomerular capillary
-
Glomerular FiltrationFILTRATION PRESSURE (STARLING FORCES)Drives filtration:Glom cap hydrostatic pressure (PGC)Bowmans caps oncotic pressure (BC = 0)
Against filtration:Bowmans caps hydrostatic pressure (PBC)Glom cap oncotic pressure ( GC)
-
Glomerular FiltrationKf(filtration coefficient)
-
Glomerular Filtration RateVolume of plasma (ml) going through the glomerulus (filtered) each minuteIntrinsic control (AUTOREGULATION) miogenic tubuloglomerular feedbackExtrinsic control (Sympathetic nerves)
-
Tubular Reabsorption & SecretionBy passive diffusionFacillitated diffusionBy primary active transport: SodiumBy secondary active transport: Sugars and Amino AcidsHormonal control
-
Tubular ReabsorptionA transepithelial process whereby most tubule contents are returned to the bloodAll organic nutrients are normally reabsorbedWater and ion reabsorption is hormonally controlled
-
Tubular Reabsorption
-
Tubular SecretionWhere substances move from peritubular capillaries or tubule cells into filtrateTubular secretion is important for:Disposing of substances not already in the filtrate Eliminating undesirable substances such as urea and uric acidRidding the body of excess potassium ionsControlling blood pH
-
Tubular Secretion
-
Reabsorption & Secretionproximal tubules(60-70%)ion sodiumObligatory reabsorptioniso-osmotic reabsorptiondistal tubulesfacultative reabsorptionPeritubule capillariesluminal & basolateral membranes
-
Transport Na+ sepanjang nefron
-
Transepithelial Glucose Transport
-
Osmolality of medullary Interstitium 4 X plasma (1200 1400 mOsm)3 solutes involved: Na+(Cl-)K+ureaPurpose:passive reabsorption of water (osmosis) in collecting ducts if ADH present
-
Osmolality of medullary InterstitiumProx tub isoosmotic reabsDescend A.H. water reabs w/o solutes; filtrate becomes increasingly hypertonicAscend A.H. solute reabs w/o water; filtrate becomes increasingly hypotonicDist tub & coll d. water reabs (osmosis) if ADH present
-
Osmolality of medullary InterstitiumFiltrate at end of descend AH osm adequate solutes for ascend AH to pumpFiltrate at end of ascent AH osm (diluting segment) insures osmotic gradient between filtrate and interstitiumIf diluting segment unable to form hypotonic fluid no osmotic gradient osmotic diuresis
-
Osmolality of medullary InterstitiumCountercurrent Multiplier System (ansa Henle juxtamed nephron pars ascend) thin passive thick Na+(Cl-)-K+-ATPase pumpCountercurrent Exchanger System (vasa recta)descend water exits; solutes enterascend air enter; solutes exit
-
countercurrent multiplier & exchanger mechanisms in the juxtamedullary nephrons
-
Formation of Dilute UrineFiltrate is diluted in the ascending loop of HenleDilute urine is created by allowing this filtrate to continue into the renal pelvisCollecting ducts remain impermeable to water; no further water reabsorption occursThis will happen as long as antidiuretic hormone (ADH) is not being secreted Urine osmolality can be as low as 50 mOsm (one-sixth that of plasma)
-
Formation of Concentrated UrineIn the presence of ADH, water permeable channels are added to the cell membranes of cells lining the DCT and collecting duct, and 99% of the water in filtrate is reabsorbedThis equalizes the osmolality of the filtrate and the interstitial fluidADH is the signal to produce concentrated urineThe kidneys ability to respond depends upon the high medullary osmotic gradient
-
Osmolality of medullary InterstitiumADH: neurohormone produced by NSO & PV (stored in posterior hypophysis)stimulus osmolarity of EF aquaporins on luminal membr of distal tubules & collecting ducts
-
ADH secretion
-
Effects of ADH
-
Osmolality of medullary InterstitiumWater reabs in collecting ducts:passive through water channels ADHNeed osmotic gradient between lumen (filtrate) and interstitium (EF) setup by countercurrent multiplier & maintained by countercurrent exchanger
-
GLUCOSE[glucose]plasma under hormonal controlGlucose: freely filtered100% reabsorbed by prox tub if < Tm (375 mg/min)[glucose]plasma > 300 mg/ml urine = renal thresholdGlucose reabsorption curve splay
-
CLEARANCEVolume of plasma (ml) cleared of a substance in one minuteIf substance x is freely filtered, not reabsorbed, not secreted, then:CX = Glomerular Filtration Rateexample: INULINCX < CIN : substance filtered and reabsorbedCX > CIN : substance filtered and secretedCCREATININE Renal Function Index ( GFR)CPAH Renal Plasma Flow
-
Solute Clearance: Rate of removal from the BloodInformation on Kidney FunctionGFRReabsorption ratesSecretion rates
-
Reabsorption of substances by renal tubule
-
GLUCOSEC = UV P Glucose < threshold completely reabsorbed Cgluc = 0Glucose > threshold glucosuria(+ osmotic diuresis)
-
C = UV 0 Pall filtered glucose will be reabsorbed, if < Tm
-
Glucose handling by nephron
-
GLUCOSEGlucose reabsorption by secondary active transport linked to Na+ reabsorption:cotransport on the luminal membrane facilitated diffusion on the basolateral membranesaturated, specific, competetion (limited!)
-
Asidosis: pH plasmaProtein damage CNS functionAlkalosis: pH plasma neuronal sensitivityCNS & heartBuffer: HCO3- & plasma proteinH+ from dietary intake & metabolismH+ excretion by lungs & kidneysACID BASE BALANCE
-
Acid-base Homeostasis
-
ACID-BASE BALANCEKidneys excrete metabolic (fixed) acids:HCO3- reabsorptionH+ secretion (limiting pH 4.5 must be buffered in lumen)
-
ACID BASE BALANCEProximal Tub.:antiport Na+-H+ luminal membr.antiport Na+-NH4+ luminal membr.simport Na+-HCO3- basolateral membr.carbonic anhydrase on the brush border Distal Tub.:H+-ATPase & H+-K+-ATPase luminal membr.antiport HCO3-Cl- basolateral membr.
-
ACID BASE BALANCE
H+-K+-ATPase pump in distal tub. K+ imbalance frequently accompany acid base imbalance & v.v.
-
HCO3 reabsorption in proximal tubules
-
New HCO3 reabsorption in proximal tubules
-
H+ Balance in kidney: the role of proximal tub. Secretion of H+ & NH4+ into lumen for excretionReabsorption of HCO3-, (Na+)
-
New HCO3 reabsorption in distal tubules & collecting ducts
-
Role of the intercalated cell in acidosis and alkalosis
-
Type A intercalated cells excrete H+ and reabsorb HCO3-Type B intercalated cells reabsorb H+ and secrete HCO3-H+ Balance in kidney: the role of the collecting duct
-
MicturitionWall of urinary bladder: Visceral smooth muscle plasticityReflex:Stretch Reflex:rec afferent center efferent effectorControl:unconsciousconscious cerebral cortex (inhibition) conditioned reflexEfferent:Parasympathetic bladder wallSomatic external sphincter (skeletal muscle)
-
Intravesical pressure (CYSTOMETROGRAM)IaIbIIIa = small press caused by 50 mlIb = no press up to 400 ml (the urge to void first felt 150 ml)II = press caused by bladder contraction
-
Urine storage in VU
-
Micturition
-
*