Pyroelectric-Based Sleep Apnea Detection System for ... · FIGURE 8 Voltage Amplifier Charge...
Transcript of Pyroelectric-Based Sleep Apnea Detection System for ... · FIGURE 8 Voltage Amplifier Charge...

FIGURE 8
Voltage Amplifier Charge Amplifier
Pyroelectric-Based Sleep Apnea Detection System for Premature Infants
Alexandria Carter 1, Rhea Charles 2 , Samira Shamsir 3 Knoxville Catholic High School 1, Webb School of Knoxville 2, University of Tennessee, Knoxville 3
INTRODUCTION RESULTS
METHODOLOGY
CONCLUSION
This work was supported primarily by the ERC Program of the National Science Foundation and Department of Energy under NSF Award Number EEC-1041877.
Much thanks to Dr. Anne Skutnik and Dr. Chien-fei Chen for this opportunity and to Samira Shamsir for her time and dedication.
REFERENCES
Sleep apnea is a fairly common condition in which an individual temporarily ceases breathing for a few seconds to a minute in his or her sleep. These interruptions may occur upwards of thirty times per hour, seriously disturbing the sleep of the individual and contributing to the future development of afflictions caused by a lower quality of sleep, including high blood pressure and heart disease. There are three types of sleep apnea: obstructive, caused by the blockage of the airway when the throat muscles relax, central, which occurs when the brain does not send the correct signal to allow breathing, and mixed, a combination of both. [1]
Premature infants (born three weeks or more before estimated due date) are at greater risk for sleep apnea than those born full-term due to their underdeveloped lungs, one of the last organs to mature. Although this problem fixes itself as the baby continues to grow and develop, a temporary solution is necessary to detect and monitor apnea. [2]
Currently, both contact and non-contact based methods to detect apnea exist, such as polysomnography, an overnight sleep study with the ability to accurately monitor the patient’s sleep pattern. However, the wires and patches that are used for this screening are bulky and uncomfortable for the fragile anatomy of neonatal infants. Other systems also compromise the convenience, comfort, or cost of the device. The solution is to utilize a minimally-invasive, lightweight, and low-cost pyroelectric sensor inside the nasal cannula to detect apnea and trigger a Vibrating Mini Motor Disc [3] to wake the infant.
To conclude, final tests were conducted to ensure the safety, comfort, and controllability of our device. The purpose of this technology is to improve the currently uncomfortable monitoring conditions, which NICU apnea patients might experience during procedures such as a plethysmography, and create a system which is optimally non-invasive. Many enhancements are already in formulation for this technology as well. First, to reduce invasive technology used on premature infants, a reusable hospital bracelet (see Figure 9) with the Mini Vibrating Motor Disc [2] enclosed will be implemented.
This effort is to make the baby’s bracelet multifunctional and reduce weight and contact devices located on and in the baby’s body and skin. Next, there is potential opportunity to use adhesives, such as hydrogel and hydrocolloids (see Figure 10), currently being used on NICU
patients to improve the sensor placement and increase its efficiency. By developing a patch (see FIgure 11) which encloses the sensor (see Figure 12) to place inside the baby’s nose, the sensor becomes permanent for as long as necessary. This creates continuity for the monitor system even if the oxygen source must be replaced or switched between a face mask and nasal cannula over the course of a day (see Figure 13). Finally, to make the former ideas possible, this system will require wireless technologies which, to our advantage, our counterpart Samira has already succeeded in doing. Our desire is for this technology to improve, grow, save money, and most importantly, save lives.
[1] American Sleep Apnea Association (2017). Sleep Apnea Information for Individuals. Retrieved from https://www.sleepapnea.org/learn/sleep-apnea/ [2] Shamsir, S.; Hesari, S.H.; Islam, S.K.; et al. “Instrumentation of a Pyroelectric Transducer Based Respiration Monitoring System with Wireless Telemetry.” 2017. [3] Robotics and CNC. (16 July 2015). Vibrating Mini Motor Disc [Data Sheet]. Retrieved from http://www.adafruit.com/products/1201 on 10 July 2018. [4] Texas Instruments. (2002). TLC272 LinCMOS Precision Dual Operational Amplifier [Data Sheet]. Retrieved on 10 July 2018. [5] Texas Instruments. (1988). SN54190 Synchronous Up/Down Counter with Down/Up Mode Control [Data Sheet]. Retrieved on 10 July 2018. [6] Texas Instruments. (1988). SN5474 Dual D-Type Positive-Edge-Triggered Flip-Flop with Preset and Clear [Data Sheet]. Retrieved on 10 July 2018. [7] Microchip. (2002-2011). MCP6541 Push-Pull Output Sub-Microamp Comparator [Data Sheet].
Retrieved on 10 July 2018. [8] Texas Instruments. (1973-2014). NA555 xx555 Precision Timer [Data Sheet]. Retrieved on 10 July 2018.
To complete this apnea detection circuit and board (see Figures 1 and 2), an intricate and detail-oriented process ensued. First, each component was built on a breadboard and tested multiple times. These components included a dual operational amplifier (op-amp) [4], a synchronous up/down counter [5], a dual D-type flip flop [6], a sub-micro amp comparator [7], a vibrating mini motor disc [3], and an xx555 timer [8]. Each component was then placed on the circuit board and soldered to finalize placement and allow inducement of current. As each component was soldered,the board was tested multiple times to ensure accurate results were produced. Our mentor Samira helped us with this by checking the consistency of the wavelength and amplitude of each unit as displayed on the oscilloscope.
We also used tools such as the multimeter and function generator to measure current or produce an artificial signal for testing. The issue with the component was usually the misplacement of a connection or incorrect wiring to the ground or power source.
As a complete circuit, this system uses a pyroelectric (heat-perceptive) sensor to detect the temperature difference between human inhalation and exhalation (see Figure 3). This signal is then sent to the op-amp (which contains both a charge and voltage amplifier) in series to heighten the signal. Then, once the signal has passed through the comparator, the timer is activated. If the breath signal is not detected for 15 seconds or more, the counter is triggered, and it induces the vibration of the motor disc (see Figure 4). This disc is encased in a compartment, such as a bracelet, which is attached to the infant’s body. If this vibration is activated, it will wake up the apnea patient in effort to regulate breathing. After a time of being exposed to this technology, we hypothesize the human body will adapt to correcting apnea signs before the machine has an opportunity to, and apnea events will reduce in number or even disappear.
(Fig. 12) pyroelectric sensor(Fig. 13) infant attached to breathing
machine; no direct access to nasal canal
(Fig. 11) nasal cannula; what our current technology relies on
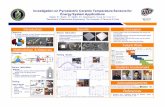
When all the components (see Methodology) were assembled and soldered onto the circuit board, the device was ready to test. The pyroelectric sensor was attached to the input of the op-amp to set up a simulation of an breathing apnea patient. The infant’s breathing cycle was represented by a series of waves (see Figures 6-8) displayed on an oscilloscope (see Figure 5). The signal was always kept above 0 volts and below 5 Volts. The respiration frequency was also around 1 Hertz.
In a successful run of the detection device, a simulated apnea episode (fifteen seconds or longer without breathing) should trigger a pulse (seen in Figure 6 as a sudden dip in the counter output), for the flip-flop to signal an LED to illuminate and for a vibrating motor to wake up the infant. This alarm signal will continue until the infant awakens and returns to his or her regular respiration cycle. Then, the flip-flop has to be manually cleared, or reset, to begin monitoring again. Our results show that the product succeeded in terms of accuracy, compactness, and affordability.
FIGURE 6
Counter Comparator Charge Amplifier
Timer
FIGURE 7
Comparator
Charge Amplifier
Combined Outputs: Apnea Simulation (Fig. 6)
Time 5 10 15 20
5 10 15 20
5 10 15 20 Time
Time
4
8
1
2
2
0
2
4
6
8
10
Vo
ltage
Volta
ge
Volta
ge
Comparator and Charge Amplifier Outputs (Fig. 7)
Charge and Voltage Amplifier Outputs (Fig. 8)
(Fig. 5) Tektronix Oscilloscope, quad-channel
apnea
(Fig. 9) reusable multiple function bracelet.smooth surface
for comfort
(Fig. 10) hydrogel adhesive patches
(Fig. 1) circuit diagram
(Fig. 2) completed board with components
(Fig. 4) mini vibrating motor disc
15 seconds without breathing
(Fig. 3) pyroelectric sensor (our temperamental baby)