Pressure profiles tongue resistance training 5 Authors ... · Tongue-palate pressures were 9...
Transcript of Pressure profiles tongue resistance training 5 Authors ... · Tongue-palate pressures were 9...
Pressure profiles tongue resistance training
Title page part 1
Running head: Pressure profiles tongue resistance training 1
2
Title: Pressure profile similarities between tongue resistance training tasks and liquid swallows 3
4
Authors: Catriona M. Steele, Ph.D.1-5 5
Gemma L. Bailey, M.H.Sc.1 6
Sonja M. Molfenter, M.H.Sc. 1 7
Erin M. Yeates, M.H.Sc. 1 8
Karen Grace-Martin, M.A.6 9
10
Affiliations: 1) Toronto Rehabilitation Institute, Toronto, Canada 11
2) Dept. of Speech-Language Pathology, University of Toronto, Toronto, Canada 12
3) Institute of Biomaterials and Biomedical Engineering, University of Toronto, 13
Toronto, Canada 14
4) Graduate Department of Rehabilitation Sciences, University of Toronto, 15
Toronto, Canada 16
5) Bloorview Kids Rehab, Toronto, Canada 17
6) The Analysis Factor, Ithaca, NY, USA 18
19
Clinical Trials Registration 20
Not applicable 21
22
23
Pressure profiles tongue resistance training
Title page part 2
Previous publication or presentation of this content: 1
A portion of these data, namely the pressure data on water and nectar-thick juice swallows, has 2
been reported in a related manuscript in the Journal of Speech-Language, Hearing Research, 3
53(2), 273-283. 4
5
Funding support: 6
Funding for this study was provided through operating and career award grants from the 7
Canadian Institutes of Health Research (Grants 69521, 82668, 84534 and 83888). Additional 8
funding support was provided by the Toronto Rehabilitation Institute and an Ontario Ministry of 9
Research and Innovation Early Researcher Award to the first author. The authors acknowledge 10
the support of Toronto Rehabilitation Institute which receives funding under the Provincial 11
Rehabilitation Research Program from the Ministry of Health and Long-term Care in Ontario. 12
The views expressed do not necessarily reflect those of the ministry. 13
14
Conflicts of Interest: 15
The first author discloses that KayPentax, the manufacturer of equipment discussed in this 16
manuscript, has provided sponsorship for a previous series of workshops that she has instructed. 17
Otherwise, the authors have no conflicts of interest to disclose. 18
19
20
Pressure profiles tongue resistance training
Title page part 3
Contact Information for Primary Author (and for offprint requests): 1
Catriona M. Steele, Ph.D. 2
Toronto Rehabilitation Institute, 3
550 University Avenue, #12030, 4
Toronto, ON, M5G 2A2, Canada 5
Tel: 416-597-3422 ext. 7603 6
E-mail: [email protected] 7
8
9
Key words: 10
Dysphagia; exercise; oral-motor; pressure; rehabilitation; resistance; swallowing; tongue. 11
Pressure profiles tongue resistance training
2
Pressure profile similarities between tongue resistance training tasks and liquid swallows 1
Abstract 2
Tongue-pressure resistance training is known to increase tongue strength in seniors and 3
individuals with stroke-related dysphagia. However, evidence of associated functional 4
improvements in swallowing is equivocal. We investigated similarities in pressure waveform 5
profiles between swallowing and several of tongue-palate pressure tasks to identify tasks that 6
may be best-suited for inclusion in tongue-pressure resistance training protocols for patients who 7
are unable to safely perform real bolus swallows in treatment. Tongue-palate pressures were 8
recorded in twenty healthy, young adults. Participants performed water and nectar-thick juice 9
swallows, effortful and non-effortful saliva swallows, and “half-maximum” tongue-palate 10
partial-pressure tasks emphasizing either anterior or posterior tongue-palate contact at different 11
speeds. Pressure slopes (amplitude change over time) during the pressure application (rise) and 12
withdrawal (release) phases were analyzed. A subset of four tasks with the greatest similarity in 13
slope characteristics to those seen in bolus swallows was identified: anterior half-maximum 14
tongue-presses; posterior maximum tongue-presses; posterior half-maximum slow tongue-15
presses; and effortful saliva swallows. We propose that future research should explore the degree 16
to which swallowing improvements are obtained from treatment protocols that emphasize these 17
tasks. 18
19
Pressure profiles tongue resistance training
3
Pressure profile similarities between tongue resistance training tasks and liquid swallows 1
Introduction 2
Tongue pressure resistance training has recently emerged as a treatment approach with 3
potential to yield positive outcomes in adults with swallowing impairment involving tongue 4
weakness. Both healthy seniors and individuals with stroke-related dysphagia have been found to 5
experience significant gains in measures of maximum isometric tongue strength following an 8-6
week course of resistance exercise in which treatment focused on achieving strength targets in 7
the range of 60-80% of maximum isometric pressure capacity1, 2. However, evidence that these 8
improvements generalize to swallowing remains equivocal. In a small sample of 10 stroke 9
patients, Robbins and colleages2 reported faster oral transit times and improvements in 10
penetration-aspiration scores on thin liquid swallowing tasks at post-treatment videofluoroscopy, 11
but changes in other impairments, such as pharyngeal residue remained elusive. 12
Within the speech-language pathology literature, interest in exercise-based approaches to 13
speech and swallowing rehabilitation has been growing1-8. Proponents of an exercise-based 14
approach advise that the basic tenants of exercise-based physical rehabilitation must be applied 15
to speech and swallowing goals, to afford the best chance of successful outcomes4, 8. Treatment 16
should employ tasks that are highly specific to the task for which functional outcomes are 17
desired (i.e., swallowing). Secondly, exercises must be practiced with sufficient intensity to 18
induce fatigue. Finally, exercise must be practiced with sufficient frequency for sufficient 19
duration to be likely to induce muscle changes. The previous studies by Robbins and colleagues1, 20
2 adhere to the latter two of these principles; tongue strength changes are targeted by including 21
60 task repetitions daily, in the 60-80% range of maximum capacity, on non-consecutive days 22
over an 8-week period. Furthermore, the Robbins protocol addresses the possibility that 23
Pressure profiles tongue resistance training
4
resistance exercises should selectively target different regions of the tongue by dividing the 1
exercise tasks equally into anterior-emphasis and posterior-emphasis tongue-palate press tasks. 2
For the anterior-emphasis tasks, patients are instructed to place a pressure bulb in the front of the 3
mouth and squeeze the bulb using the front of the tongue. For the posterior-emphasis tasks, the 4
pressure bulb is positioned further back in the mouth, and patients are instructed to squeeze the 5
bulb using the back of the tongue. However, the Robbins exercise protocol focuses exclusively 6
on strength and does not include actual swallowing tasks, or other possible tongue-press tasks, 7
such as those emphasizing precision, endurance or speed. The fact that swallowing pressures are 8
known to fall well short of those pressures registered in maximum isometric tasks9 calls the into 9
question the emphasis on strength goals and outcomes in this approach. 10
In our laboratory, we have been studying patterns of tongue-pressure application in 11
swallowing and exploring tongue-pressure resistance training as a method for effective swallow 12
rehabilitation. Our primary goal is to restore functional swallowing with thin liquids. We have 13
been particularly interested in the possible contribution of motor skill to tongue pressure 14
application, inspired by evidence from other rehabilitation literature that skill training (involving 15
the repeated practice of goal-oriented tasks) can lead to faster and more sustainable changes in 16
motor function than strength training alone10. Skilled movements are defined as those movement 17
tasks that require the modification and organization of muscle synergies into effective movement 18
sequences11. Our interest in this concept led us to develop a tongue resistance training protocol 19
that involves repeated practice of sub-maximal partial pressure generation tasks, with an 20
emphasis on pressure precision12. The lack of clear evidence of generalization from improved 21
pressure outcomes to improved swallowing outcomes in these cases, prompted us to investigate 22
pressure profiles more closely and to explore the role of timing13, 14 (and temporal modulation) as 23
Pressure profiles tongue resistance training
5
a factor in tongue-pressure behavior in swallowing. Systematic variations in the temporal 1
aspects of tongue-pressure onset and withdrawal between water and nectar-thick juice swallows 2
have recently been described in healthy young adults13. The rise and release phases of tongue-3
palate pressure behavior may logically be considered to have primary salience for propulsion of a 4
bolus through the mouth towards the pharynx in swallowing14-16. This observation supports the 5
speculation that treatment tasks that most closely match the slope characteristics (i.e., amplitude 6
changes over time) of both tongue-pressure application and release in healthy swallowing may 7
be optimal tasks to include in a program of swallowing rehabilitation. Although true task-8
specificity for swallowing would require actual swallows, the idea that some non-swallowing 9
tongue-press tasks might closely mirror critical aspects of the tongue-pressure motor pattern seen 10
in swallowing is important, given that many patients who aspirate may be unable to safely 11
include bolus swallows in their swallowing rehabilitation regime. 12
The goal of the current study was to explore similarities in tongue-pressure profile 13
between liquid swallowing tasks and various tongue-press tasks in healthy adults, based on 3 14
specific criteria: a) whether pressures are registered in the same locations on the palate; b) the 15
rate of amplitude change at the anterior palate during the pressure onset phase (rise slope); and c) 16
the rate of amplitude change at the posterior palate during the pressure release phase (release 17
slope) (see Figure 1). For the current study, we studied partial-pressure amplitude targets in the 18
range of 50% of each participant’s maximum isometric pressure capacity (henceforth called 19
“half-maximum tongue-press” tasks). The choice of this target range was motivated by previous 20
evidence showing that habitual swallowing pressures typically fall in or below this half-21
maximum range9. 22
Pressure profiles tongue resistance training
6
Discrete liquid swallowing tasks were performed with two stimuli: water (DSW) and 1
nectar-thick apple juice (DSANEC). Comparator tasks included both anterior-emphasis tasks, for 2
which the front of the tongue is pressed up against the front of the palate (the alveolar ridge, just 3
behind the upper incisors), and posterior-emphasis tasks, for which the back of the oral tongue is 4
pressed up against the back of the palate (targeting the anatomical region around the transition 5
from the hard to soft palate). Task instructions for the following comparator tasks are detailed in 6
Table 1: anterior emphasis half-maximum tongue-press tasks (AHMAX); posterior-emphasis 7
maximum effort tongue-press tasks (PMAX); posterior emphasis half-maximum tongue-press 8
tasks (PHMAX); non-effortful saliva swallows (NESS)13, 15, and effortful saliva swallows 9
(ESS)13, 15. The half-maximum tongue-press tasks were conducted at habitual (AHMAX; 10
PHMAX), fast (AHMAXFAST; PHMAXFAST) and slow (AHMAXSLOW; PHMAXSLOW) 11
rates. 12
Methods 13
Participants 14
Twenty healthy adults (10 male, 10 female), under the age of 40, provided written 15
consent for participation in the study. Participants attended an intake session in which an oral 16
mechanism examination and a swallow screening were performed to rule out clinical signs of 17
swallowing difficulty. Participants with known histories of swallowing difficulties, stroke, brain 18
injury, neurodegenerative disease, or head and neck cancer were excluded. The study was 19
approved by the Toronto Rehabilitation Institute Research Ethics Board. 20
Data were collected using the orolingual manometry module of the KayPentax Digital 21
Swallow Workstation (KayPentax, Lincoln Park, NJ). A soft plastic strip containing 3 silicon air 22
bulbs (diameter: 13 mm; inter-bulb spacing: 8 mm) was adhered to each participant’s palate in 23
Pressure profiles tongue resistance training
7
midline using a small amount of a cyanoacrylate dental adhesive (Iso-Dent, Ellman International 1
Inc., Oceanside, NY). The strip was positioned such that the anterior bulb was located 2
immediately behind the front teeth. Pressures from the anterior, medial and posterior palatal 3
bulbs were registered on a monitor in a window with a 500 mm Hg maximum, and sampled at 4
250 Hz. For a few participants, it became obvious that maximum pressures exceeded 500 mm 5
Hg, in which case the equipment was adjusted to allow a maximum of 750 mm Hg. Equipment 6
was calibrated at the beginning of each recording session as per manufacturer’s instructions. 7
Prior to attaching the tongue-bulb array, task-training was provided. Participants were taught to 8
perform maximum emphasis anterior and posterior emphasis tongue presses and immediate 9
feedback regarding pressure values was provided using the Iowa Oral Performance Instrument 10
(IOPI). Participants were then instructed in the performance of half-maximum tongue-press 11
tasks, again using the IOPI for biofeedback. The experiment then proceeded using the KayPentax 12
equipment to register tongue-palate pressures. Participants were instructed to perform the 10 13
different experimental tasks in randomized order, with 5 repetitions per task, to enable the 14
calculation of representative task mean data values for each participant. Previous literature 15
regarding intra-participant variability in swallowing suggests that at least 3 repetitions of a given 16
swallowing task are required to obtain representative tongue-pressure measures17. 17
Instructions were displayed in front of the participant on a computer monitor, so that 18
mandatory quiet rest periods could be interspersed between tasks. For the saliva swallow tasks, 19
one swallow was cued every 30 seconds, for a total signal recording time of 2 minutes, 30 20
seconds per task. This ensured a rest period between swallows to allow for saliva replenishment. 21
The bolus swallow and tongue-press tasks were peformed at a natural pace, unless the task 22
instructions specifically indicated that the participant was to perform rapid or slow half-23
Pressure profiles tongue resistance training
8
maximum tongue-presses. For the bolus swallow tasks, participants were provided with a cup 1
containing approximately 150 ml of water or nectar-thick apple-juice (Resource™, Nestlé 2
Nutrition, Highland Park, MI) and cued to take 5 comfortably-sized sips of liquid in a row from 3
the cup, performing one discrete swallow per sip, and then removing the cup from their lips 4
before the next swallow. Precise sip-volume measurement techniques cannot easily be employed 5
during the collection of natural reiterated discrete swallowing data. However, based on previous 6
studies using these same tasks, it can be assumed that sip size in this study fell between 5 and 10 7
ml per swallow, and likely varied less than 2 ml from swallow to swallow within a participant18. 8
Data Processing 9
The first step in data processing was to index important events in the pressure 10
waveforms. This task was completed by two trained research associates who aligned a cursor in 11
the KayPentax manometry software with the onset, peaks and offsets of pressure events in each 12
pressure waveform. For each event, the timepoint (in milliseconds) and pressure amplitude (in 13
mm Hg) was recorded in a spreadsheet for subsequent analysis. Ten percent of the data were 14
indexed in duplicate for the purposes of calculating inter-rater agreement, which was excellent 15
(Intra-class correlation = 1.00). Due to a technical problem with the pressure measurement 16
equipment, data for one male participant could not be included in the analysis. Pressure 17
amplitude differences in mm Hg (henceforth called range), durations (in milliseconds) and slopes 18
(range divided by duration, in mm Hg per second) were calculated for the anterior pressure bulb 19
rise-phase (pressure onset to pressure peak at the anterior bulb) and posterior pressure bulb 20
release-phase (pressure peak to pressure offset at the posterior bulb) of each pressure event. Prior 21
to further analysis, all range data were normalized relative to a standardized value of 600 mm Hg 22
Pressure profiles tongue resistance training
9
assigned to the peak maximum anterior isometric pressure rise-range value registered at the 1
anterior pressure bulb for each participant: 2
3
Normalized pressure range = Pressure range X 600 4 Maximum Isometric Pressure range 5 6
Normative values for maximum isometric pressures at the anterior palate have previously been 7
reported to fall at approximately 600 mm Hg for healthy young adults9. 8
9
Analysis 10
The analysis for this study was conducted in a stepwise fashion. First, chi-square 11
statistics were used to compare the frequency with which activation of both the anterior and 12
posterior pressure bulbs occurred in the different tasks included in the study. Descriptive 13
statistics for rise slope and release slope were then examined, and Forest Plots showing 95% 14
confidence interval overlap across tasks were prepared (Figures 2 and 3). To further examine 15
task differences statistically, two mixed model analysis of variance models (rise slope; release 16
slope) were run using the mixed procedure in SPSS 16.0 (SPSS, Inc., 2007). Both models 17
controlled for the within-subjects nature of the eleven tasks by including random effects for 18
participant and the participant X task interaction, with a variance components covariance 19
structure and restricted maximum likelihood estimation. Furthermore, rather than using the mean 20
response of the five replicate trials for each swallowing task as the experimental unit, which 21
ignores variability among replications, we captured the variation among the trials directly by 22
modelling the variance-covariance matrix of the residuals on each task for each participant. The 23
best-fitting covariance structure for the residuals across trials was a diagonal structure, which 24
Pressure profiles tongue resistance training
10
estimated a unique variance for each trial, but had no additional correlation among these 1
residuals. Autoregressive and compound symmetry covariance structures were tested, but neither 2
resulted in improved fit of the model, so the simpler diagonal structure was retained (-2RLL = 3
7607.58). Sex was included as a fixed, between-subjects factor to both models, but there were no 4
significant main effects in either one (rise slope: F(1, 14.4) = 0.112, p = 0.743; release slope 5
F(1, 16.47) = 0.354, p = 0.56). Consequently, the sex factor was dropped from the model. Post-6
hoc tests compared each of the nine pressure tasks to each of the two bolus swallowing tasks 7
(DSW and DSANEC), using Sidak adjustments to control for Type I error. The nine pressure 8
tasks were not compared to each other, since these comparisons were not of interest. 9
Results 10
The water,and nectar-thick apple juice swallowing tasks typically elicited activation of 11
both the anterior and posterior pressure bulbs. The saliva swallow tasks presented with this same 12
activation pattern at least 94% of the time. By contrast, the anterior half-maximum tongue-press 13
tasks were significantly less likely to display activation of both bulbs (χ2, df 10, = 424.43, p = 14
0.000) and involved isolated activation of the anterior bulb at least 84% of the time. The 15
posterior maximum tongue-press task most commonly elicited co-activation of both bulbs (77% 16
of the time), with the remaining cases involving isolated posterior bulb activity. The posterior 17
half-maximum tongue-press tasks involved co-activation of both bulbs between 50% and 56% of 18
the time, and isolated posterior activation 35-47% of the time. 19
The activation pattern comparison suggested that anterior-emphasis half-maximum 20
tongue-press tasks were dissimilar from swallowing tasks in their tongue-pressure profiles. This 21
was further confirmed in the descriptive statistics (Table 2) and the Forest Plot comparisons of 22
rise and release-slope confidence interval overlaps. These suggested that the AHMAX and 23
Pressure profiles tongue resistance training
11
PMAXTP tasks had similar rise-slopes to the water and nectar-thick swallows (Figure 2), while 1
the ESS and PHMAXSLOW tasks overlapped with the water and nectar-thick juice swallows for 2
release-slope (Figure 3). 3
In the mixed model ANOVAs, a significant main effect of task was found in the rise 4
slope data, F(10, 129.18) = 12.74, p < 0.001). The AHMAXFAST task had a significantly 5
greater rise slope than both discrete water (p < .001) and nectar-thick apple juice (p < .001) 6
swallowing tasks. None of the other tasks showed significant differences in pairwise 7
comparisons to the water and nectar-thick juice swallows. 8
A significant main effect of task was also found in the release slope data, F(7, 82.52) = 9
16.78, p = 0.000). The smaller value for the error degrees of freedom in this analysis reflects 10
exclusion of the anterior-emphasis half-maximum tongue-press tasks from the model, based on 11
the fact that these involved no activation of the posterior pressure bulb. Posthoc pairwise 12
comparisons identified significant differences between discrete water swallows and the PHMAX 13
(p < 0.007), PHMAXFAST (p < 0.000) and PMAXTP (p < 0.000) tasks. Significant pairwise 14
differences from the nectar-thick juice swallows were also found for the PHMAXFAST (p < 15
0.000) and PMAXTP (p < 0.011) tasks. 16
In summary, all tasks other than the AHMAXFAST task were found to have statistical 17
similarity (or non-difference) from water and nectar-thick juice swallows with respect to rise 18
slope. Of these, inspection of confidence interval overlaps suggests that the AHMAX and 19
PMAXTP tasks have rise slope values that fall closest to those seen in liquid swallowing tasks. 20
With respect to release slope, clear differences were noted between liquid swallowing tasks and 21
the AHMAX (regular rate, slow and fast), PHMAX, PHMAXFAST and PMAXTP tasks. This 22
leaves the non-effortful and effortful saliva swallow tasks and the posterior half-maximum slow 23
Pressure profiles tongue resistance training
12
task, which demonstrated statistical non-difference from the liquid swallowing tasks. Of these, 1
confidence interval overlaps were strongest for the effortful saliva swallows and PHMAXSLOW 2
task. 3
4
5
Discussion 6
The primary goal of this study was to identify those tongue resistance training tasks that 7
most closely resemble bolus swallows in their pressure slope rise and release characteristics, so 8
that these tasks might become a focus in future swallowing treatment studies. We have 9
demonstrated that in healthy young adults, the rise slope characteristics of anterior emphasis 10
half-maximum tongue-press tasks (AHMAX) and posterior-emphasis maximum effort tongue-11
press tasks (PMAXTP) are most similar to those seen in water and nectar-thick juice swallows. 12
Similarly, the slope characteristics of pressure release in saliva swallowing tasks (non-effortful 13
and effortful) and slow posterior-emphasis half-maximum tongue-press tasks (PHMAXSLOW) 14
are similar to those seen in liquid swallowing tasks. As an outcome of this study, we propose that 15
future research should explore the potential of treatment protocols emphasizing these tasks, (i.e., 16
with slope profiles that are not significantly different from those seen in healthy swallowing), to 17
yield improvements that generalize to functional swallowing. It must, of course, be recognized 18
that the absence of significant differences in an ANOVA test cannot be interpreted to imply 19
equivalence across the tasks that were compared in this study. The current findings, therefore, 20
represent preliminary evidence that requires further substantiation. 21
It is of interest to note that the pressure ranges registered during discrete water and 22
discrete nectar-thick swallowing tasks in this experiment fell well short of maximum isometric 23
Pressure profiles tongue resistance training
13
pressure values (normalized to a value of 600 mm Hg) consistent with previous studies9. This 1
phenomenon appears to have occurred to a greater degree in our research participants than 2
previously described in the literature. The healthy young adults in this study registered 3
swallowing pressure amplitudes in the range of only 10% -15% of maximum isometric values, 4
i.e. pressures of 50-100 mm Hg or 6-12 KPa), normalized using a standardized maximum 5
isometric pressure value of 600 mm Hg. Previous studies have observed a higher range of 6
swallowing pressures approaching 50% of maximum values9. One possible explanation for this 7
apparent discrepancy is the fact that the current study did not involve radiation exposure, thereby 8
allowing greater (and perhaps more representative) sampling of behavior across repeated task 9
performances. However, this finding also suggests that the ideal magnitude of partial-pressure 10
targets requires further study. Our study explored pressure profiles for half-maximum tongue-11
press tasks. It remains unknown whether tongue-press tasks targeting values in the 10-25% 12
maximum range, or those targeting values in the >50% maximum range may have slope profiles 13
that differ from swallow pressure slope profiles to an even smaller extent. At this point it is 14
clearly premature to speculate on the ideal magnitude of partial pressure task targets. 15
A second observation of importance in this study, as shown in Table 2, is that half-16
maximum tongue-press tasks with anterior emphasis typically result in pressure patterns with 17
little or no activity registered at the medial and posterior palate bulb locations. Posterior-18
emphasis half-maximum tasks failed to involve anterior bulb activation in a substantial number 19
of our participants. This suggests that these tasks elicit pressure patterns that are questionably 20
similar to those seen in normal swallowing tasks and further supports our concern that they may 21
not have sufficient similarity in slope characteristics to bolus swallows for inclusion in tongue-22
resistance training protocols for swallow-rehabilitation. 23
Pressure profiles tongue resistance training
14
Non-effortful saliva swallows yielded quite different pressure patterns than bolus 1
swallows in this study. Specifically, both the rise and release phases of pressure were prolonged 2
in the NESS task; consequently, the slopes of pressure rise and release at the anterior and 3
posterior pressure bulbs, respectively, were found to be significantly less steep than those 4
observed in bolus swallows. This finding suggests that there may be a particular salience to the 5
parameter of pressure slope for swallowing function in the presence of a bolus, and that it may 6
not be adequate to focus exclusively on pressure range as a therapeutic target. 7
Inspection of the descriptive statistics in Table 2 shows that pressure slopes were steeper 8
in the rise phase for discrete water swallows than for discrete nectar-thick juice swallows, while 9
the reverse phenomenon (steeper release) was observed with the nectar-thick stimuli. This 10
difference, which was in the order of 20-120 mm Hg/sec, requires further investigation because it 11
may reflect an important modulatory factor in swallowing related to the precision of slope 12
application and release across stimuli of differing viscosity. Furthermore, this suggests that 13
pressure withdrawal by the posterior tongue may be a particularly important component in 14
swallowing function. Pressure withdrawal has not, to our knowledge, been targeted in tongue 15
resistance training protocols to date. 16
Clearly, a major issue with respect to the interpretation of this study is the fact that these 17
pressure phenomena were measured in healthy adults. It remains unknown whether people with 18
swallowing impairment involving tongue weakness will demonstrate similarities in pressure 19
profiles across tasks in the same manner. A broader sampling of healthy adults across the age 20
span will also be needed in order to establish normative ranges for adults of different ages with 21
respect to pressure slope parameters. These considerations precluded the direct application of 22
these findings to patient populations. Nonetheless, we speculate that if patients with dysphagia 23
Pressure profiles tongue resistance training
15
are found to have deviant pressure slopes, a meaningful goal of swallowing intervention would 1
be to attempt to establish more normative pressure slope patterns. The findings of the present 2
study serve to inform such future efforts, and suggest that an emphasis on tasks with slope 3
characteristics similar to those seen in healthy swallowing may be an appropriate place to start. 4
5
Conclusion 6
In conclusion, this study has identified a subset of tongue-pressure resistance training 7
tasks, which display pressure slope characteristics similar to those typically seen in water and 8
nectar-thick liquid swallows. Saliva swallows were also found to yield pressure release slope 9
profiles that closely resemble those typically seen in water and nectar-thick liquid swallows. We 10
conclude that protocols for tongue-resistance training in individuals with dysphagia should 11
incorporate these tasks to a substantial extent, if a goal of treatment is to include tasks that are 12
similar to swallowing. 13
14
Pressure profiles tongue resistance training
16
Acknowledgments: 1
The authors gratefully acknowledge assistance provided by Melanie Moore, Rebecca Cliffe and 2
Nicole Buesselberg during data collection and processing. 3
4
Pressure profiles tongue resistance training
17
References 1
1. Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual 2
exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53(9):1483-9. 3
2. Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR et al. The effects of 4
lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150-8. 5
3. Sharkawi AE, Ramig L, Logemann JA, Pauloski BR, Rademaker AW, Smith CH et al. 6
Swallowing and voice effects of Lee Silverman Voice Treatment (LSVT): a pilot study. Journal 7
of Neurology, Neurosurgery & Psychiatry. 2002;72(1):31-6. 8
4. Burkhead LM, Sapienza CM, Rosenbek JC. Strength-training exercise in dysphagia 9
rehabilitation: principles, procedures, and directions for future research. Dysphagia. 10
2007;22(3):251-65. 11
5. Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue 12
strengthening exercises in young normals. Folia Phoniatr Logop. 2003;55(4):199-205. 13
6. Wheeler KM, Chiara T, Sapienza CM. Surface electromyographic activity of the 14
submental muscles during swallow and expiratory pressure threshold training tasks. Dysphagia. 15
2007;22(2):108-16. 16
7. Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, et al. Rehabilitation of 17
swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal 18
UES opening. Gastroenterology. 2002;122(5):1314-1321. 19
8. Clark HM. Neuromuscular treatments for speech and swallowing: a tutorial. Am J Speech 20
Lang Pathol. 2003;12(4):400-15. 21
Pressure profiles tongue resistance training
18
9. Nicosia MA, Hind JA, Roecker EB, Carnes M, Doyle J, Dengel GA et al. Age effects on 1
the temporal evolution of isometric and swallowing pressure. Journals of Gerontology Series A-2
Biological Sciences & Medical Sciences. 2000;55(11):M634-40. 3
10. Winstein CJ, Rose DK, Tan SM, Lewthwaite R, Chui HC, Azen SP. A randomized 4
controlled comparison of upper-extremity rehabilitation strategies in acute stroke: A pilot study 5
of immediate and long-term outcomes. Archives of Physical Medicine and Rehabilitation. 6
2004;85:620-8. 7
11. Monfils M-H, Plautz EJ, Kleim JA. In search of the motor engram: Motor map plasticity 8
as a mechanism for encoding motor experience. Neuroscientist. 2005;11(5):471-83. 9
12. Yeates EM, Molfenter SM, Steele CM. Improvements in tongue strength and pressure-10
generation precision following a tongue-pressure training protocol in older individuals with 11
dysphagia: three case reports. Clin Interv Aging. 2008;3(4):735-47. 12
13. Steele CM, Bailey GL, Molfenter, SM. Tongue pressure modulation during swallowing: 13
Water vs. nectar-thick liquids. Journal of Speech, Language & Hearing Research. 2010; 14
53(2):273-283 15
14. Steele CM, Huckabee ML. The influence of orolingual pressure on the timing of 16
pharyngeal pressure events. Dysphagia. 2007;22(1):30-6. 17
15. Huckabee ML, Steele CM. An analysis of lingual contribution to submental sEMG 18
measures and pharyngeal biomechanics during Effortful Swallow. Archives of Physical 19
Medicine and Rehabilitation. 2006;87(August):1067-72. 20
16. Hiiemae KM, Palmer JB. Tongue movements in feeding and speech. Crit Rev Oral Biol 21
Med. 2003;14(6):413-29. 22
Pressure profiles tongue resistance training
19
17. White R, Cotton SM, Hind J, Robbins J, Perry A. A comparison of the reliability and 1
stability of oro-lingual swallowing pressures in patients with head and neck cancer and healthy 2
adults. Dysphagia. 2009; 24(2): 137-144. 3
18. Bennett JW, Van Lieshout PH, Pelletier CA, Steele CM. Sip-Sizing Behaviors in Natural 4
Drinking Conditions Compared to Instructed Experimental Conditions. Dysphagia. 2009;24(2): 5
152-158. 6
7
8 9 10 11
12
13
Pressure profiles tongue resistance training
20
1
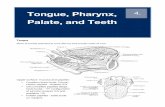
Figure 1. 2
Screen capture of anterior and posterior pressure bulb waveforms during an anterior tongue press 3
task. Onsets, offsets and peak pressures are denoted in each waveform by dashed vertical lines. 4
The portion of the anterior bulb waveform from pressure onset until peak pressure is the rise 5
phase. The portion of the posterior bulb waveform following the peak, until return to signal 6
baseline, is the release phase. Pressure slope for these phases was calculated as the change in 7
signal amplitude (in mm Hg) divided by the phase duration (seconds). 8
9
Pressure profiles tongue resistance training
21
1
Figure 2. 2
Forest plot showing the overlap in means and 95% confidence intervals for tongue pressure rise 3
slope, measured at the anterior palate, during 11 different tasks: DSW (discrete water swallows); 4
DSANEC (discrete nectar-thick apple juice swallows); NESS (non-effortful saliva swallows); 5
ESS (effortful saliva swallows); AHMAXSLOW (anterior emphasis half-maximum tongue 6
palate presses performed at a slow rate); AHMAX (anterior emphasis half-maximum tongue 7
palate presses); AHMAXFAST (anterior emphasis half-maximum tongue palate presses 8
performed at a fast rate); PHMAXSLOW (posterior emphasis half-maximum tongue palate 9
presses performed at a slow rate); PHMAX (posterior emphasis half-maximum tongue palate 10
presses); PHMAXFAST (posterior emphasis half-maximum tongue palate presses performed at a 11
fast rate); and PMAXTP (posterior emphasis maximum isometric tongue palate presses). The 12
dashed lines outline the interval capturing rise slope values for discrete water and nectar-thick 13
juice swallows. Tasks with means and confidence interval boundaries falling outside these lines 14
differ from these bolus swallowing tasks in rise slope. 15
16
Pressure profiles tongue resistance training
22
1
Figure 3. 2
Forest plot showing the overlap in means and 95% confidence intervals for tongue pressure 3
release slope, measured at the posterior palate, during 8 different tasks: DSW (discrete water 4
swallows); DSANEC (discrete nectar-thick apple juice swallows); NESS (non-effortful saliva 5
swallows); ESS (effortful saliva swallows); PHMAXSLOW (posterior emphasis half-maximum 6
tongue palate presses performed at a slow rate); PHMAX (posterior emphasis half-maximum 7
tongue palate presses); PHMAXFAST (posterior emphasis half-maximum tongue palate presses 8
performed at a fast rate); and PMAXTP (posterior emphasis maximum isometric tongue palate 9
presses). The dashed lines outline the interval capturing release slope values for discrete water 10
and nectar-thick juice swallows. Tasks with means and confidence interval boundaries falling 11
outside these lines differ from these bolus swallowing tasks in release slope. 12
13
Pressure profiles tongue resistance training
23
Table 1. Experimental instructions 1
Task Instruction
Maximum isometric pressure, anterior emphasis (AMAXTP)
Press the front of your tongue up to the front of your palate (touching the bony ridge just behind your upper teeth) as hard as you can. We will be calling this the “front position”.
Discrete water swallow (DSW)
Take and swallow one sip of water, then remove the cup from your lips.
Discrete nectar-thick apple juice swallow (DSANEC)
Take and swallow one sip of this thick apple-juice, then remove the cup from your lips.
Non-effortful saliva swallow (NESS)
Swallow your saliva as you usually do.
Effortful saliva swallow (ESS)
Do a “hard” saliva swallow. Imagine that you are swallowing a whole grape.
Half-maximum anterior emphasis tongue-press (AHMAX)
In the front position you were able to hit a _____ kPa on your maximum effort tongue-press. Now I want you to aim for half of that value. So, try to hit a _____ kPa in the front position.
AHMAXSLOW Your half maximum target value in the front position is _____kPa. We now want you to complete this task slowly. We want you to gradually reach ____kPa. Try to make the numbers move up one at a time.
AHMAXFAST Your half maximum target value in the front position is _____kPa. We now want you to complete this task fast. We want you to hit that same target of ____kPa again but this time in a quick, fluid movement.
Maximum isometric pressure, posterior emphasis (PMAXTP)
Now you are going to perform a maximum effort press in the back position. Move the bulb about an inch further back from the front position. Then push straight up with the body of your tongue and squeeze the air out of the bulb against the roof of your mouth. Squeeze as hard as you can.
Half-maximum posterior emphasis tongue-press (PHMAX)
In the back position you were able to hit a _____ kPa on your maximum effort tongue-press. Now I want you to aim for half of that value. So, try to hit a _____ kPa in the back position.
PHMAXSLOW Your half maximum target value in the back position is _____kPa. We now want you to complete this task slowly. We want you to gradually reach ____kPa. Try to make the numbers move up one at a time.
PHMAXFAST Your half maximum target value in the back position is _____kPa. We now want you to complete this task fast. We want you to hit that same target of ____kPa again but this time in a quick, fluid movement.
Pressure profiles tongue resistance training
24
Table 2. 1
Task Phase Range (mm Hg*) Duration (ms) Slope (mm Hg/s)
Mean Std.
Deviation Mean
Std. Deviation
Mean Std.
Deviation
Discrete Water Swallows (DSW) Rise 61.80 83.82 220.18 177.30 369.59 319.08
Release 65.39 64.68 274.53 235.53 280.29 211.70
Nectar-thick Apple Juice Swallows (DSANEC) Rise 74.00 86.82 276.94 218.96 313.51 220.91
Release 77.77 58.40 257.51 177.77 371.48 240.60
Non-effortful Saliva Swallows (NESS) Rise 108.82 119.87 569.86 485.93 240.03 248.19
Release 75.74 103.05 422.24 433.10 206.88 230.45
Effortful Saliva Swallows (ESS) Rise 264.12 313.65 622.16 447.08 506.39 522.40
Release 145.27 143.26 483.99 513.06 354.60 283.40
Anterior Half Maximum Tongue Press (AHMAX) Rise 302.98 125.84 987.66 597.36 373.86 201.09
Release N/A N/A N/A N/A N/A N/A
Anterior Half Maximum Fast Tongue Press (AHMAXFAST)
Rise 345.80 144.42 443.84 261.41 933.51 461.39
Release N/A N/A N/A N/A N/A N/A
Anterior Half Maximum Slow Tongue Press (AHMAXSLOW)
Rise 235.07 117.53 1778.55 1045.40 198.25 217.81
Release N/A N/A N/A N/A N/A N/A
Posterior Half Maximum Tongue Press (PHMAX) Rise 71.63 95.09 641.68 380.08 262.11 246.32
Release 266.30 143.93 590.25 271.35 535.51 363.84
Posterior Half Maximum Fast Tongue Press (PHMAXFAST)
Rise 107.25 144.02 382.13 208.21 450.81 327.18
Release 283.65 201.39 367.23 158.83 908.07 612.49
Pressure profiles tongue resistance training
25
Posterior Half Maximum Slow Tongue Press (PHMAXSLOW)
Rise 66.18 79.26 1088.08 785.15 119.81 103.79
Release 178.55 118.34 794.85 522.26 316.24 238.06
Posterior Maximum Isometric Pressure (PMAXTP) Rise 220.78 237.29 881.47 584.84 367.37 344.29
Release 419.46 240.82 794.32 512.01 617.12 328.47
*normalized vs. maximum anterior palate isometric pressure of 600 mm Hg
1
2