Posterior reversible encephalopathy syndrome following a ...
Posterior reversible encephalopathy syndrome
-
Upload
neurologykota -
Category
Health & Medicine
-
view
45 -
download
3
Transcript of Posterior reversible encephalopathy syndrome

POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME
DR. SUMIT KAMBLESENIOR RESIDENTDM NEUROLOGY, GMC, KOTA
MODERATORDR. DILIP MAHESHWARIASSO. PROF. NEUROLOGY

HISTORICAL BACKGROUND• In 1897, Vaquez and Nobecourt pointed out the correlation of
toxemia of pregnancy and HTN
• In1928, Oppenheimer and Fishberg introduced the term hypertensive encephalopathy
• In 1996, Hinchey and colleagues first described the clinical condition- reversible posterior leukoencephalopathy( RPLE)
Semin Neurol 2011;31:202–215

INTRODUCTION• Disorder of reversible subcortical vasogenic brain oedema in
patients with acute neurological symptoms (eg, seizures, encephalopathy, headache, and visual disturbances) in the setting of renal failure, blood pressure fluctuations, cytotoxic drugs, autoimmune disorders, and pre-eclampsia or eclampsia.
• Reversible posterior cerebral edema syndrome• Posterior leukoencephalopathy syndrome• Hyperperfusion encephalopathy• Brain capillary leak syndrome
Lancet Neurol 2015; 14: 914–25

• Brain imaging usually reveals vasogenic oedema predominantly involving the bilateral parieto-occipital regions.
• PRES is caused by endothelial injury related to abrupt blood pressure changes or direct effects of cytokines on the endothelium, which leads to breakdown of the blood– brain barrier and subsequent brain oedema.
• PRES is generally reversible, both radiographically and clinically, and has a favourable prognosis.

PHYSIOLOGY OF CEREBROVASCULAR BLOOD FLOW
• Cerebral blood flow autoregulation - cerebral circulation normally maintains a constant cerebral blood flow, despite changes in cerebral perfusion pressure
• Largely driven by changes in cerebral arteriolar wall diameter, which can be produced by several mechanisms, including cerebrovascular pressure reactivity , chemical factors (eg, carbon dioxide tension), and autonomic nervous system.
Lancet Neurol 2015; 14: 914–25

• Blood pressure decreases - cerebral arteriolar vasodilation occurs, preserving adequate blood flow and perfusion for neuronal and glial needs.
• Blood pressure increases – arterioles constrict as a physiological response to maintain a steady—and not increasing—cerebral blood flow.

• Endothelium regulates vascular tone by secreting a combination of vasodilators (nitric oxide, prostacyclin, hydrogen sulfide, and endothelium-derived hyperpolarising factor) and vasoconstrictors (throm boxane A2, endothelin 1, and angiotensin II).
• With chronic HTN, the resistance arterioles undergo proliferation of the muscular media adapting to the chronically high perfusion pressures
• This results in a shift of the autoregulation curve to the right

NORMAL CEREBRAL AUTOREGULATION

DYNAMICS OF CBF IN PTS WITH CHRONIC HTN

PATHOPHYSIOLOGY OF PRES• 1. Cerebral Hyperperfusion- Rapidly developing hypertension
exceeds the upper limit of cerebral blood flow autoregulation and causes hyperperfusion.
• When the pressure rise is rapid and severe, the autoregulatory response might be insufficient, hyperperfusion can occur, and the blood–brain barrier breaks down, allowing the interstitial extravasation of plasma and macromolecules.
• Posterior brain regions can be particularly susceptible to hyperperfusion because little sympathetic innervation exists in posterior fossa.
J Stroke Cerebrovasc Dis 2012; 21: 873–82.

• Important factors that influence breakdown in the blood–brain barrier
1. Patient’s mean baseline blood pressure, 2. Proportional rise in blood pressure, 3. Rapidity with which the change takes place

• 2. Cerebral Hypoperfusion - 15–20% of patients with PRES are normotensive or hypotensive and that, even among patients who are hypertensive, less than 50% have a documented mean arterial pressure above the usually quoted upper limit of cerebral blood flow autoregulation (≥140–150 mm Hg).
• Endothelial dysfunction - from systemic toxic effects - hypertension could be a reaction to insufficient brain perfusion


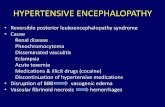
COMORBID CONDITIONS/TRIGGERS• Pregnancy-related conditions1. Eclampsia2. Hydatidiform mole
• Major medical illness1. Organ transplantation2. Thrombotic thrombocytopenic purpura3. Henoch-Schonlein purpura4. Autoimmune inflammatory disease: systemic lupus, scleroderma,
Wegener’s, periarteritis nodosa5. Sepsis/systemic inflammatory response syndrome/multiple organ failure6. Alcohol and drug withdrawal7. Hypomagnesemia, hypercalcemia, hypocholesterolemia8. Renal failure

• Neurologic illness1. Guillain-Barre’s syndrome2. Spinal cord injury with autonomic dysreflexia3. Head injury
• Drugs that cause endothelial dysfunction1. Immunosuppressant agents - Cyclosporine A2. Chemotherapeutic agents, especially high-dose multidrug -Tacrolimus
(FK506), Cisplatin, Gemcitabine, Bevacizumab3. Erythropoietin4. Blood transfusion5. Indinavir6. Cytarabine7. IVIg

CLINICAL FEATURES
Epidemiology • Age - 4 to 90 years, most cases occur in young to middle-aged
adults, mean age ranging across case series from 39 to 47 years
• Female predominance
• Acutely or subacutely, usually developing during several hours or days.

Encephalopathy• severity from confusion, somnolence, and lethargy to coma• reported in 13 % to 90 % of cases
Seizure• Up to 92 % of cases• Secondary generalized seizures are common (53–62 %) , rarely
focal (23 %-28 %) • Status epilepticus - 3 % to 13 %

Visual abnormalities• found in 26 % to 67 % of patients• blurred vision (7 -18 %)• visual neglect (4 -27 %)• homonymous hemianopsia (4 -20 %)• visual hallucinations (3 -5 %) • cortical blindness (8 -33 %)
Focal neurological signs• 3-17% cases• hemiparesis or aphasia,
Myelopathic symptoms and signs (Am J Neuroradiol 2012; 33: 896–903.)

PREVALENCE OF CLINICAL SYMPTOMS AND SIGNS
SYMPTOMS PREVALENCE
Encephalopathy 50–80%
Seizure 60–75%
Headache 50%
Visual disturbances 33%
Focal neurological deficit 10–15%
Status epilepticus 5–15%
J Stroke Cerebrovasc Dis 2012; 21: 873–82.

DISTRIBUTION OF CLINICAL FEATURES IN COHORT STUDIES OF PRES
Clinical Features Hinchey1996 (N=13)
Bartynski2007(N=136)
McKinney2007(N=76)
Lee2008(N=36)
Burnett2010(N=79)
Encephalopathy 10 (67 %) 39 (26 %) 10 (13 %) 34 (94 %) 76 (90 %)Seizure 11 (73 %) 97 (71 %) 58 (76 %) 33 (92 %) 56 (70 %)
Headaches 8 (53 %) 39 (26 %) 3 (4 %) 19 (53 %) 26 (31 %)
Visual abnormalities 10 (67 %) 39 (26 %) 3 (4 %) 13 (36 %) 24 (29 %)
Nausea/vomiting 8 (53 %) 39 (26 %) NR NR NR
Focal neurological signs
NR NR 2 (3 %) 1 (3 %) 14 (17 %)
Acute hypertension 12 (80 %) 91 (67 %) NR NR 62 (78 %)
Annual Update in Intensive Care and Emergency Medicine 2011

DIAGNOSIS
• Acute and subacute neurological symptoms in the appropriate clinical context (ie, in the presence of pronounced hypertension, blood pressure fluctuations, immuno suppression, autoimmune disorders, renal failure, pre-eclampsia, or eclampsia).
• Diagnosis of PRES is not mainly radiological; the clinical context is crucial in making correct diagnosis.


IMAGING• Useful to exclude alternative diagnoses• Confirms diagnosis of PRES.
• Computed tomography (CT):Hypodensities in a suggestive topographic distribution

MRI BRAIN
• T1: hypo intense in affected regions
• T1 C+ (Gd): patchy variable enhancement. It can be seen in ~35%
of patients, whether leptomeningeal or cortical pattern.
• T2: hyperintense in affected regions
• DWI: usually normal
• ADC: signal increased in affected regions due to increased diffusion
• GRE: may show hypointense signal in cases of haemorrhage
• SWI: may show microhemorrhages in up to 50%

RADIOLOGICAL CHARACTERISTICS OF PRES
1. Holohemispheric watershed pattern (23 %)• watershed zone between the anterior and posterior cerebral
arteries and the middle cerebral artery• confluent vasogenic edema extends through the frontal, parietal,
and occipital lobes

2. Dominant parietal-occipital pattern (22 %)• previously thought to be typical of PRES• posterior part of the parietal and occipital lobes is
predominantly involved
Am J Neuroradiol 2012; 33: 896–903.)

3. Superior frontal sulcus pattern (27 %)• Patchy edema predominates in the frontal lobes along the mid
to posterior aspect of the superior frontal sulcus.• parietal and occipital lobes are variably involved

4. Partial or Asymmetric Expression of the Primary Patterns (27.9%)• Asymmetric abnormalities in the affected parietal or occipital
lobes.

ATYPICAL MRI FINDINGS IN POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME• Edema can affect basal ganglia and brainstem in up to a third
of cases and the cerebellum in up to half
• Restricted diffusion can be seen on MRI in 15–30% of cases
• Presence of restricted diffusion is generally associated with irreversible structural injury and incomplete clinical recovery.
Am J Neuroradiol 2012; 33: 896–903

• Enhancement is seen in about 20% of patients with PRES
• Intracranial haemorrhage - 10–25% of cases. Intraparenchymal hemorrhage is the most common type and sulcal subarachnoid haemorrhage is the second most common type. About 18–30% of patients with haemorrhage have both types

DIFF ERENT TYPES OF INTRACRANIAL HAEMORRHAGE IN POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME

ATYPICAL MRI FINDINGS IN POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME
• Axial T2 fluid-attenuated inversion recovery sequences show predominant
• (A) brainstem • (B) basal ganglia• (C) thalamus • (D) pontine
involvement

23 yr-old-male cocaine-induced malignant hypertension, presenting with headaches, confusion and spinal cord syndrome

Radiological Features
Hinchey1996 (N=13)
Casey2000N = 16
Bartynski2007(N=136
McKinney2007(N=76)
Lee2008(N=36)
Burnett2010(N=79)
Bilateral 15 (100%) 11 (69%) 98 (72%) NR 36(100 %) NR
Asymmetric 10 (67 %) NR 21 (15 %) 2 (3 %) NR NR
Confluent NR 2 (13 %) 31 (23 %) 44 (58 %) 2 (13 %) 12(16 %)
Gray matter 4 (27 %) NR NR 22 (29 %) 16 (44 %) NR
Posterior > anterior
14 (93 %) 15 (94 %) 30 (22 %) NR NR NR
Occipital 14 (93 %) NR 134 (99 %) 75 (99 %) NR NR
Parietal 13 (87 %) 8 (50 %) 134 (99 %) 75 (99 %) NR 50 (67 %)
Frontal 7 (47 %) 14 (88 %) 93 (68 %) 60 (89 %) 22 (61 %) 61 (81 %)
Temporal 9 (60 %) 16 (100 %)
55 (40 %) 52 (68 %) NR 62 (83 %)
Brainstem 2 (13 %) NR 17 (13 %) 14 (18 %) 21 (58 %) NR
Cerebellum 1 (7 %) NR 41 (30 %) 26 (34 %) 21 (58 %) NR
Basal ganglia 1 (7 %) 3 (19 %) 19 (14 %) 9 (12 %) NR NR

REGIONAL INVOLVEMENT BY PRES IN SERIES OF 136 PATIENTS
AJNR 2007;28:1302-07

DIFF ERENTIAL DIAGNOSES OF POSTERIOR REVERSIBLEENCEPHALOPATHY SYNDROME (PRES)
Infectious encephalitis• Fever• Peripheral leucocytosis• CSF pleocytosis• Positive CSF Gram stain or culture• Positive CSF microbial serology or PCR• Can be unilateral in brain imaging
Autoimmune or paraneoplastic encephalitis• History of malignancy or tumour• Antigen-specific antibody in serum or CSF• Can be unilateral in brain imaging
Lancet Neurol 2015; 14: 914–25

Malignancy or tumour (lymphoma, gliomatosis cerebri, metastatic disease)• Subacute-to-chronic clinical presentation• History of malignant tumour• History of unintentional weight loss• Abnormal CSF cytology• Absence of clinical and radiological resolution• Can be unilateral in brain imaging
CNS vasculitis• Often subacute clinical presentation• CSF pleocytosis• Cytotoxic oedema in non-PRES-like pattern

Progressive multifocal leukoencephalopathy• Subacute-to-chronic clinical presentation• Can be unilateral in brain imaging
Osmotic demyelination syndrome• History of rapid normalisation of sodium or glucose concentrations• Does not preferentially affect the parieto-occipital lobes• Characteristic central pontine signal abnormality in a bat-wing shape

Acute demyelinating encephalomyelitis• Usually a disorder affecting children• Preceded by viral or bacterial infection• Fever in 50–75% of patients• Radiographically supratentorial lesions usually asymmetrical
Toxic leukoencephalopathy• History of illicit drug use• Positive drug or toxin screen• Symptoms progress for weeks• Magnetic resonance spectroscopy can show abnormally raised lactate and decreased N-acetyl aspartate concentrations

Reversible cerebral vasoconstriction syndrome
• Thunderclap headache• PRES quickly progresses over a few hours, complications may occur for
several days with the RCVS• Imaging PRES- Bilateral parieto-occipital lesions on MRI, typical for PRES• Imaging RCVS- classic pattern of ‘string of beads’ on Angiography, at least
two narrowings per artery on two different cerebral arteries at brain magnetic resonance angiography (MRA) or at conventional angiography
• 10% of cases there seems to be overlap between this syndrome and PRES

TREATMENT• General measures- aimed at maintaining ABC of the patient
• Symptomatic therapyAntihypertensives - reduce blood pressure by 25% within first
few hours.Anticonvulsants
• Correction/Removal of the underlying causeWithdrawl of offending drugTermination of pregnancy



PROGNOSIS• Brain lesions are reversible
• Most studies- excellent short term and long term outcome
• Symptoms usually seem to resolve in about 3–8 days (75–90%) while recovery of the MRI abnormalities takes longer—several days to weeks
• Mortality (3–6%) - intracranial haemorrhage, posterior fossa oedema with brainstem compression or acute hydrocephalus, or marked diffuse cerebral oedema and increased global intracranial pressure.

• Persistent neurological sequelae -10–20%
• Hyperglycaemia and time to control of the causative factor have been also reported to be independently associated with poor outcomes
• Poor outcome may also be related to associated comorbidity (sepsis) or intracerebral haemorrhage

• Recurrent PRES ~ 4% of cases
• More common in patients with uncontrolled hypertension compared with patients who have other causes compared with patients who have other causes (ie, immunosuppressant therapy).
• 10–15% develop recurrent seizures in the first few years after PRES

PAEDIATRIC POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME• Incidence - 0.4%
• Common causes- haematological disorders, kidney disease, or those taking cytotoxic drugs after organ transplantation, Glomerulonephritis, acute leukaemia, Henoch- Schonlein purpura, and haemolytic uraemic syndrome
• Clinical and radiological presentation appears to be similar to that in adults
• Mean blood pressure at presentation -140/85 mm Hg

AREAS OF UNCERTAINTY AND CONTROVERSY
• Opposing pathophysiological hypothesis – hypoperfusion / hyperprfusion
• Co-occurrence of neuromyelitis optica spectrum disorders and PRES - role of aquaporin-4 channelopathy in its pathogenesis ?
• Myelopathy or brainstem dysfunction
• PRES can be also be diagnosed in the presence of normal brain imaging ?

THANK YOU

REFERENCES• Posterior reversible encephalopathy syndrome: clinical and
radiological manifestations, pathophysiology, and outstanding questions Lancet Neurol 2015; 14: 914–25
• Semin Neurol 2011;31:202–215
• Understanding Posterior Reversible Encephalopathy Syndrome S. Legriel, F. Pico, and E. Azoulay. Annual Update in Intensive Care and Emergency Medicine 2011
• Posterior Reversible Encephalopathy Syndrome, Fundamental Imaging and Clinical Features Am J Neuroradiol 2012; 33: 896–903