Poster 59: Ptosis Crutch: Success Treating Myogenic Ptosis Secondary to Myasthenia Gravis
-
Upload
joseph-pruitt -
Category
Documents
-
view
216 -
download
2
Transcript of Poster 59: Ptosis Crutch: Success Treating Myogenic Ptosis Secondary to Myasthenia Gravis

Poster 57
A Delayed Diagnosis of Pattern Macular DystrophyJanice McMahon, O.D., William Flynn, andLavender Streiff, O.D., Illinois College ofOptometry/Illinois Eye Institute, 3241 South MichiganAvenue, Chicago, Illinois 60616
Background: Pattern macular dystrophies are a group ofdisorders that typically present in midlife and are inheritedas an autosomal dominant trait. Patients are often asymp-tomatic but may complain of mild blur, central scotomas, ormetamorphopsia. Symptoms generally do not correlate wellwith the macular appearance as only mild visual complaintsare common even with striking macular changes. Patterndystrophies have been divided into 5 groups based on theirpigmentary characteristics; patients may exhibit multiplepatterns or may show progression from one pattern toanother over time. Management of the pattern dystrophiesincludes genetic counseling, Amsler grid testing, and pho-todocumentation. Visual prognosis is typically good.Case Summary: A 54-year-old black male presented to theIllinois Eye Institute in 2008, 5 years after his last visit to thissame clinic. He reported blurred vision but had not beenwearing his �3.00 spectacle prescription. His ocular historywas notable for macular mottling OU, which caused metamor-phopsia on Amsler grid testing. Given that macular degenera-tion is not prevalent in this demographic, Stargardt’s had beenconsidered but was ruled out with an electroretinogram. Best-corrected distance visual acuity in 2008 was 20/50 O.D., 20/25O.S., reduced from 20/30 O.D., 20/20 O.S. in 2003. Dilatedfundus exam now noted significant, well-demarcated, atrophicmacular changes in both eyes, certainly more dramatic than thepreviously described mottling. Fundus photos were taken andan OCT confirmed macular atrophy in both eyes with the righteye OCT having an appearance typical of a full-thicknessmacular hole. The diagnosis of pattern dystrophy was dis-cussed with the patient, who reported no other family history.He was given a home Amsler grid and is scheduled to befollowed on an annual basis.Conclusion: Though the pattern dystrophies are considereduncommon, it is likely that they go undiagnosed or evenmisdiagnosed because of their visual sparing properties andsubtle, variable fundus appearance. This case illustrates theprogressive nature of pattern dystrophy and the importance ofdifferentiating it from other lesions in order to better under-stand its prognosis and visual impact. One of the most strikingand unexpected features of this case is the OCT result; based on itsanalysis one would expect the patient to have a macular hole,which, given the fundus appearance and acuity, is not present.
Poster 58
Alternative Considerations for the High Myope—PhakicIntraocular LensesSandra Fortenberry, O.D., and Pat Segu, O.D., TheUniversity of Houston, College of Optometry, 505 J.Davis Armistead Building, Houston, Texas 77204-2020
Background: This poster provides information for alterna-tive approaches for patients seeking refractive surgery whohave high amounts of myopia. Although only 1 FDA devicewas used in this clinical case, there are 2 FDA-approveddevices that will be discussed in addition to combinedtherapies and contraindications.Case Report: A 36-year-old Hispanic male presented withinterest in refractive surgery options. With his current rigidgas-permeable contact lenses, his vision was 20/70 O.D. and20/40 O.S. A cycloplegic refraction yielded high myopia of�21.00-0.75x172 O.D. and �20.50-0.50x011 O.S. withacuities of 20/40 O.D. and O.S. His external ocular healthshowed bilateral nasal pterygium and open angles by go-nioscopy. His internal ocular health was unremarkable. Thepatient was then evaluated for phakic intraocular contactlenses. An iridotomy was performed in each eye by yaglaser prior to surgery. A Visian Intraocular Contact Lenswas implanted in both eyes and limbal relaxation incisions(LRI) were created on the right cornea. After these proce-dures, the patient had �3.25-0.50x010 O.D. and �3.25-0.50x010 O.S. of residual myopia. The patient later re-turned for conventional laser-assisted in situ keratomileusis(LASIK) performed with IntraLase, after which his acuitywas 20/30-2 O.D. and 20/30 O.S. without spectacles ortraditional contact lenses.Conclusion: Optometrists play a vital role in improving thequality of life for many patients. As ocular primary careproviders, it is our job to distinguish which patients arecandidates for refractive surgery options and to make properreferrals. Patients depend on optometry to guide, educate,and protect their vision. This poster will discuss a clinicalcase of intraocular contact lenses used to correct highrefractive error.
Poster 59
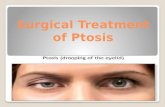
Ptosis Crutch: Success Treating Myogenic PtosisSecondary to Myasthenia GravisJoseph Pruitt, O.D., Pauline Ilsen, O.D.,Carolin Yeung, O.D., West Los Angeles Veterans AffairsHealthcare Center/Southern California College ofOptometry, Bldg. 304, Room 2-111, 11301 Wilshire Blvd,Los Angeles, California 90073
A 60-year-old white male presented to the neurology de-partment with a chief complaint of wanting management ofmyasthenia gravis (MG). The patient’s medical history wasonly remarkable for hypertension and a history of prostatecancer. The neurologic exam noted a limited field of gaze inall directions and a ptosis at rest in the right eye only. Thepatient was diagnosed with Presumed Seronegative MG andwas prescribed pyridostigmine and Azathioprine and was toreturn for a follow-up neurology exam. Two months later atthe follow-up neurology exam, it was found that there hadnot been a significant improvement, especially with regardsto ptosis O.D., from the initial examination. Therefore, thepatient was then prescribed high-dose intravenous human
325Poster Presentations

immunoglobulin (IVIg) 400 mgs/kg x 5 days and a referralsent to optometry/ophthalmology for a refraction and spec-tacles fitted with ptosis crutches. Three weeks later, thepatient presented to optometry for a refraction, and he wasfound to have a slight astigmatic refractive error withpresbyopia OU. The patient was prescribed glasses fittedwith a ptosis crutch. Later the same day at the optometricexamination, the patient presented in neurology to reviewhis most recent lab work and it was determined he wasindeed positive for seronegative MG.
A physician or neurologist should ultimately make thediagnosis of MG. Nevertheless, due to the susceptibility ofthe ocular muscles to the disease process, eye care providersare on the front line, especially since it is suggested �85%to 90% of all individuals diagnosed with MG have ocularinvolvement. Furthermore, �20% to 50% of all cases ofMG are purely ocular, in which case, a distinction is madeand is specifically said to be ocular MG. Therefore, becauseoptometrists are most likely to be the first to encounter anundiagnosed patient, they must be able to maximally pro-vide the care within their scope of practice. As for ptosis,outside of surgical intervention, the ptosis crutch is a viableoption. A ptosis crutch is a good and inexpensive, lessinvasive option for those with complications secondary toptosis that are not yet at the point of surgical intervention.
Poster 60
A Case of Bilateral Idiopathic Central SerousChorioretinopathyElizabeth D. Jones, B.S., and Kimberly D. Kohne, O.D.,Indiana University School of Optometry, 800 EastAtwater, Bloomington, Indiana 47401
Background: Idiopathic central serous chorioretinopathy(ICSC) is a condition in which there is leakage of fluid fromthe choroid into the subretinal space, under the RPE, orboth. Symptoms present can be blurred or dim vision,metamorphopsia, and central scotoma. Typically it is uni-lateral, with bilateral presentation in only about 14% to 30%of cases. It is of unknown etiology, affecting predominatelymales between the ages of 20 and 50 years. It can beassociated with type-A personality, stress, hypochondriasis,and steroid use. Among the differentials are AMD, choroi-dal inflammatory disorders, optic nerve pits, macular de-tachment as a result of an RRD or macular hole, choroidaltumor, or pigment epithelial detachment.Case History: This case looks at the diagnosis and manage-ment of a patient with bilateral ICSC. A 20-year-old malepatient reported to the primary care clinic because he hadnoticed a spot of light in the vision of his left eye adjacentto his central vision. His BVA was 20/25 O.D. and 20/40-2O.S., with NIPH OU. External and pupil evaluation re-vealed a grade 1 afferent pupillary defect OS. Slit lampexamination was unremarkable. Dilated fundus examinationrevealed dim foveal light reflex O.D., - FLR O.S., and anasymmetrical macular appearance between the 2 eyes.
Amsler grid was normal O.D. with metamorphopsia O.S.The patient denied steroid or ephedra usage, but was stillsuspect as possibly having ICSC. Optical coherence tomog-raphy (OCT) of both eyes revealed serous detachments ofthe neurosensory retina in both eyes, confirming bilateralICSC.Conclusion: The patient was educated about his condition,that it typically resolves on its own, and may worsen beforefinal resolution. Follow-up evaluation 2 weeks later re-vealed improved VAs and � FLR OU, as well as almostcomplete resolution of macular swelling O.D. and muchimproved swelling O.S. upon OTC evaluation.
Poster 61
Temporal Field Loss Associated With Tilted Optic NerveRichard Steven Savoy, O.D., Southern College ofOptometry, 1245 Madison Avenue, Memphis, Tennessee38104
Background: Its etiology being a common board question,bitemporal field loss can be an alarming finding during anoptometric examination. The most common and certainlymost well-known etiology defining this ocular sign is achiasmal lesion, specifically a pituitary adenoma or otherpotentially morbid lesion. Indeed, every first-year optome-try student recognizes that the optic nerve decussates behindthe eye and that the 2 nasal nerve fiber bundles combine toform the optic chiasm. This pinpoints the chiasm as a uniquelandmark where the nasal optic nerve fibers of both eyes canbe compromised by a solitary lesion. Thankfully, in somecases, bilateral temporal field loss can actually manifestfrom a simple anatomic anomaly commonly seen as malin-serted or “tilted” optic discs instead of a cranial mass.Case History: Following is a summary of the significantfindings related to this case report. This patient was a51-year-old man who presented for examination complain-ing only of reading blur. His ocular history was remarkablefor previous LASIK surgery. Predilation examination wasessentially normal except for a noticeably constricted lefttemporal visual field by finger counting and “extent of field”confrontation testing. Dilated fundus examination revealedtilted optic nerves with white, reflective peripapillarychanges noted nasally to the nerve in each eye. Refractilebodies, tentatively identified as optic nerve drusen, werealso noted bilaterally. Automated field testing (particularlythe seldom used “screening field,” which extends to 60degrees temporally) showed significant temporal field losson both sides. B-scan confirmed mild bilateral drusen. MRIwas normal. The oblique optic nerve insertion, possiblycomplicated by optic nerve drusen, was diagnosed as thecause of the field loss.Conclusion: A case such as this can present a diagnosticdilemma for the clinician. Prudence may dictate MRI in allsimilar cases as the implications for the patient are obvi-ously serious should the clinician overlook chiasmal pathol-ogy. Nevertheless, awareness of this “normal” anatomical
326 Optometry, Vol 79, No 6, June 2008