Pharmacotherapy of Bronchial Asthma
-
Upload
druprathnakarmddihpgdhm -
Category
Documents
-
view
15 -
download
5
description
Transcript of Pharmacotherapy of Bronchial Asthma

Beethoven
John F. Kennedy Calvin Coolidge
Elizabeth Taylor
Bob Hope
Charles Dickens
ASTHMA COMPANY!!
8 Marriages7 Men!!2 Oscars

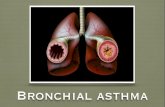
•B.Asthma• ASTHMA IS DEFINED• CHRONIC INFLAMMATORY DISEASE OF AIRWAYS• CHARACTERIZED BY INCREASED
RESPONSIVENESS OF THE TRACHEOBRONCHIAL TREE, MULTIPLICITY OF STIMULI.
• MANIFESTED PHYSIOLOGICALLY• BY WIDESPREAD NARROWING OF THE AIR
PASSAGES• RELIEVED SPONTANEOUSLY OR AS
A RESULT OF THERAPY.• MANIFESTED CLINICALLY• BY PAROXYSMS OF DYSPNEA,
COUGH, AND WHEEZING.

•B.Asthma…..course

B.Asthma…Pathogenesis

The outpouring of mucus from hypertrophied submucosal glands, the bronchoconstriction,
and dehydration ,contribute to the formation of mucus plugs that can block airways in asthmatic
patients.
INSPISSATED MUCUS PLUG
COUGHED UP BY A PATIENT
DURING AN ASTHMATIC ATTACK

B.Asthma…Pathogenesis
Bronchospasm
Bronchospasm
Inflammation
&
HyperactivityInflammation
&
Hyperactivity
Non-Allergens
•Infection
•Exercise
•Cold air
•En.Pollutants
Non-Allergens
•Infection
•Exercise
•Cold air
•En.Pollutants
Allergens
•House
dust
•Cockroach
•Cat dander
•Molds
•Pollens
Allergens
•House
dust
•Cockroach
•Cat dander
•Molds
•Pollens
Neura
lNeura
l

Allergen challenge1h 6h
•Early ReactionType I•Preformed mediator release
•Late ReactionType II•Inflammatory cell recruitment and activation•MAY LAST WEEKS
Early And Late Reaction

B.Asthma…Pathogenesis-Chemical mediators
•Eosinophil Cationic protein
•E.Major Basic Protein
Reversed byβagonists
Theophylline

Neural stimuli
Noxious stimuli[Irritants]

B.Asthma…Pathogenesis
•Pharmacologic stimuliAspirin-Can be fatal [AIA]ß-adrenergic antagonists-Can be
fatalSulfiting agents-Pot.metasulfite
[ pharmaceuticals as preserving agents]
Tartarazine

Allergic inflammation of airways

Pharmacotherapy of Bronchial Asthma
12
3
4

Pharmacotherapy of Bronchial Asthma
Long Term Control Medications
Quick Relief Medications
1.Short acting ß2 Agonists
2.Methylxanthines3. Anticholinergics[Not alone]
1.Glucocorticoids
2.Long-acting ß2 agonists
3.Combined medications
4.Mast cell stabilizers
5.Leukotrine modifiers
6.Methyl xanthines

Pharmacotherapy of Bronchial Asthma1. BronchodilatorsA. ß2 Agonists-Salbutamol, Bambuterol,Salmeterol,Formoterol, EphedrineB. Methylxanthines-Theophylline,Aminiohylline
,Choline theophyllinate C. Anticholinergics-Ipratropium bromide,
Triotropium bromide2. Leukotrine
modulators
Montelukast, Zafirlukast,
Zileuton
3. Mast cell stabilizers- Nedocromil
Sod. Cromoglycate [Cromonil ]
4. CorticosteroidsA. Systemic-
Hydrocortisone,-- i.v Prednisolone,--oralInhalational:
Beclamethasone5. Anti-IgE Antibody:
Omalizumab

Sympathomimitecis[Bronchodilators]
MOA:
Pharmacological actions:a)Bronchodilatationb)Inhibit mediator release from mast cellsc)Inhibit micro vasc.leakaged)Increase ciliary activity
c) Tachycardiad) Skeletal muscle
tremor
ß2 Selective•Salbutamol[Albuterol],•Terbutaline,•Metaproterenol, •Pirbuterol•Salmeterol, •Formoterol•Non-selective:
•Adrenaline, Ephidrene, Isoproterenol:Not used because of CVS effects
Increase formation


ß2 Selective Sympathomimitics
Salbutamol[Albuterol], Terbutaline, Metaproterenol, Pirbuterol
Route of Admin: • MDI [Inhalation]: Peak15’ To 4-6h• Nebulizer[Inhalation]: For emergency-More
effective,[Less co-ordination required]Larger particles, hence dose is more
• Tablets [Salbutamol & Terbutaline] [Oral]: • Not usually used.• Children, • Severe asthma-Aerosol worsens cough• No advantage, Over inhalation, More
systemic actiono S.C: Terbutaline is availableLong acting, accumulation on repeated
administration

ß2 Selective Sympathomimitics……
• Salmeterol & Formoterol[Long acting]a)Long acting because highly lipid solubleb)Combined with corticosteroids in long term
therapyc) Not used alone
ß2 Selective Sympathomimitics Toxicity:
• Inhalational-Safe• Oral-Cardiac toxicity,
tremors

ß2 Selective Sympathomimitics…USES
Short acting-• Rescue therapy• Caution-Use of 2 or more cannisters /month
→Marker of risk of long term asthma mortality →Requires anti-inflammatory to prevent loss of
pulmonary functionLong acting• Not for acute• Long term-not controlled by low dose ICS• May carry a risk of arrhythmia

Pharmacotherapy of Bronchial Asthma
1. BronchodilatorsA.ß2 Agonists-
Salbutamol, Bambuterol, Salmeterol,Formoterol
EphedrineB. METHYLXANTHINES
THEOPHYLLINE, AMINIOHYLLINE, CHOLINE THEOPHYLLINATE
C. Anticholinergics-
2.Leukotrine modulators
3.Mast cell stabilizers-
4. Corticosteroids
5. Anti-IgE Antibody:

Methyl xanthines-Theophylline
Source Alkaloid contentTea leaves
CaffeineTheophylline
50mg1 mg
1cup
Coffee seeds
Caffeine 75 mg 1 Cup
Cocoa, Chocolate
TheobromoineCaffeine
24 mg4mg
1Cup
Cola Caffeine 30 mg 200ml

•Inhibition of PDEs •Accumulation of cyclic AMP and cyclic GMP, •Increasing signal transduction through these pathways
•Competitive antagonist at adenosine receptors
MOA:


Methyl xanthines-TheophyllinePharmacological actions
• CNS;• Low and moderate
doses, caffeine—• Cortical arousal • Increased alertness Deferral of fatigue.• Nervousness and
tremor• Very high doses, • Medullary
Stimulation – convulsions- death;
• CVS:• +ve chronotropic and
inotropic effects LOW Block Adenosine
receptors Mod PDE inhibition-Accu.of
cAMP High Release of Ca at
sarcoplasmic reticulum Increase blood flow-
Pentoxyfiilline

Methyl xanthines-TheophyllinePharmacological actions…..
• GIT: Stimulate secretion of gastric acid
and digestive enzymes. [Coffee . Not caffeine]
• KIDNEY Theophylline—weak diuretic. Not
useful• SMOOTH MUSCLE The bronchodilation Adverse effects, limit the dose Inhibit antigen-induced release of
histamine from lung tissue;

Methyl xanthines-Theophylline
• SKELETAL MUSCLE
• Improves-contractility, reverses fatigue of the diaphragm in patients –COPD
Not the first line therapy in Asthma[ADE]
Only when others fail
S.R. Tab in chronicTDM InexpensiveApnoea in
premature infants• PK?????
USESPharmacological actions

30 μg
25 μg
20 μg
15
10
5 μg5 μg
10 μg
15 μg
20 μg
Theophylline toxicity and plasma concn•Death, •Convulsions, Shock, Arrhythmias•Delirium-Worsening CVS-
•VPBs- ↑ Muscle tone-Flashes of light•Tachypnioea-Agitation
•Tremors-•Restlessness-•Palpitation•Vomiting-Headache-Insomnia
BRONCHODLATION
TherapeuticRange
Toxic
μ g/ml

Theophylline- Drug Interactions• Metabolism Inducers: Smoking, Phenytoin,
Rifampicin, Phenobarbitone• DOSE of Theophylline ?????
• Metabolism inhibitors-Erythro, Cipro, Cimetidine, OCP
• DOSE of Theophylline??????
PreperationsTablets, SR Tabs. Aminophylline-Inj. ,

Why NSAIDs worsen Asthma?
Linoleic acid
Arachidonic acid
Prostaglandins (PG) Leukotrienes (LT)
LipoxygenaseCyclooxygenase
Anti-inflammatory steroidsGlucocorticoids
NSAIDsaspirin
Worsening of Asthma
Zileuton
Cox 1 Specific

Pharmacotherapy of Bronchial Asthma
3. Mast cell stabilizers-
4. Corticosteroids
5. Anti-IgE Antibody:
1. BronchodilatorsA. ß2 Agonists-Salbutamol, Bambuterol,
Salmeterol,Formoterol, EphedrineB. Methylxanthines-
Theophylline, Aminiohylline, Choline theophyllinate
C. ANTICHOLINERGICS-• IPRATROPIUM
BROMIDE,• TRIOTROPIUM
BROMIDE2.
Leukotrine modulators

Antimuscarinic Agents
Effect of Vagal Tone[Ach
Effect of Vagal Tone[Ach]
Effect of Antimuscarinics?????Receptors
•Ipratropium Bromide•Tiotropium Bromide[longer acting]•Inhalation•As Rotacaps• + Salbutamol•More effective in COPD•Not always effective-Other pathways?
Datura a source of ATROPINEWas in India from ages


Pharmacotherapy of Bronchial Asthma1. BronchodilatorsA. ß2 Agonists-Salbutamol, Bambuterol,
Salmeterol,Formoterol, EphedrineB. Methylxanthines-
Theophylline, Aminiohylline, Choline theophyllinate
C. Anticholinergics-Ipratropium bromide, Triotropium bromide
2. LEUKOTRINE MODULATORSMONTELUKAST, ZAFIRLUKAST,ZILEUTON
3. Mast cell stabilizers-
4. Corticosteroids5. Anti-IgE
Antibody:

:Leukotriene Modifiers: 1. Leukotriene Receptor Antagonists
2. 5-Lipoxygenase Inhibitor
• Arachidonic acid
• 5-Lipoxygenase
• Leukotrines[LTB4, C4, D4]
• LT Receptors
•Food interferes with absorption•Prophylactic•Oral•Safe
•Efficacy and use same as below•Short acting•Hepatotoxic
5-Lipoxygenase Inhibitor
Zileuton
Leukotriene Receptor Antagonists MontelukastZafirlukast
Airway edema,*Smooth muscle*constriction, *Inflammatory process
PRPHYLACTIC


Pharmacotherapy of Bronchial Asthma1. BronchodilatorsA. ß2 Agonists-Salbutamol, Bambuterol,
Salmeterol,Formoterol, EphedrineB. Methylxanthines-
Theophylline, Aminiohylline, Choline theophyllinate
C. Anticholinergics-Ipratropium bromide, Triotropium bromide
2. Leukotrine modulatorsMontelukast, Zafirlukast,Zileuton
3. MAST CELL STABILIZERS- NEDOCROMIL
SOD. CROMOGLYCATE [CROMONIL ]
4. Corticosteroids5. Anti-IgE
Antibody:

Mast cell stabilizers
•Nedocromil]•Sod. Cromoglycate [Cromonil]•Inhibit degranulation of mast cells•Route-MDI•Uses-Asthma, Allergic rhinitisAllergic conjuctivitis
PRPHYLACTIC

Pharmacotherapy of Bronchial Asthma1. BronchodilatorsA. ß2 Agonists-Salbutamol, Bambuterol,
Salmeterol,Formoterol, EphedrineB. Methylxanthines-
Theophylline, Aminiohylline, Choline theophyllinate
C. Anticholinergics-Ipratropium bromide, Triotropium bromide
2. Leukotrine modulators
Montelukast, Zafirlukast,
Zileuton
3. Mast cell stabilizers- Nedocromil
Sod. Cromoglycate [Cromonil ]
4. CORTICOSTEROIDSA. SYSTEMIC-
HYDROCORTISONE, PREDNISOLONEINHALATIONAL:
BECLAMETHASONE5. Anti-IgE Antibody:

Glucocorticoids• Asthma
• Airway inflammation,
• Airway hyperreactivity,
• Acute bronchoconstriction
• Glucocorticoids do not directly relax airway smooth
muscle
• No effect on acute bronchoconstriction
• Most effective drugs
• Profound and generalized antiinflammatory action
• Very few mechanisms of inflammation escape the inhibitory effects
1. Modulation of cytokine and chemokine production;
2. ↓ of PG synthesis; 3. ↓ Accumulation of
basophils, eosinophils,4. ↓Vascular permeability 5. Potentiate the effect of ß-
agonists

Inhaled Glucocorticoids[Aerosol therapy]
1. Glucocorticoids are very effective in controlling asthma,
2. Systemic glucocorticoids -serious adverse effects
3. Inhaled glucocorticoids - target drug directly to the site of inflammation-LUNG
4. Enhance the therapeutic index
5. ↓number and degree of side effects
6. Without sacrificing clinical utility
PREPERATIONS• Beclomethasone
dipropionate • Triamcinolone
acetonide • Flunisolide• Fluticasone
propionate• Budesonide• Mometasone• Ciclesonide[Trial]

GlucocorticoidsUses
• Acute asthma • Persistent asthma• ‘Status’-Acute severe• Oral prednisone• COPD-Exacerbations

Glucocorticoids-ADE• ADE[Inhalation]
• Cough, oral candidiasis• Dysphonia• Abolished by rinsing the
mouth after use and• Use of a spacer device.• Systemic effects can
occur [Inhalation] :• Increases with dose• Growth retardation
(children)• Increased bone catabolism
(osteoporosis risk)• Adrenal suppression• Bruising
• ADE:Oral glucocorticoids
• Hypertension• Diabetes• Proximal
myopathy• Osteopenia/
osteonecrosis• Central
adiposity/purple striae/buffalo hump

Glucocorticoids; Some facts
•Steroid phobia•Inhaled is not=systemic Or = Anabolic steroids
•Regular therapy is important•If inadequately controlled, Long-acting Beta agonist can be combined-Combination inhalers•Fluticasone+Salmaterol•Budesonide+Formeterol

Other Drugs OMALIZUMAB•Anti-IgE Monoclonal AB•Prophylactic•Expensive
Future:1.MAB against cytokines2.Antagonists of cell adhesion molecules3. Protease inhibitors4. Immunomodulators5.Macrolides[??Anti Chlamydial]6.PDE4 Specific inhibitorsRoflumilast, Cilomilast, Tofimilast

Pharmacotherapy
Causes of airway narrowing and Tt.• Broncho constriction• Mucosal edema• Cellular infiltration• Hyperplasia of secretory cells• Hyperplasia of vessel wall• Hypertrophy of smooth muscles
Easily reversed
Sustained
Tt with
Anti-infl.
required

Management
[Rescue medication]
?

Short acting β2 agonist SOS for symptom relief
ICSLow Dose
ICSLow Dose
ICS High Dose
ICS High Dose
LABA
LABA LABA
OCS
1 MildIntermittent
MildPersistent
SeverePersistent
VerySevere
Persistent
ModeratePersistent
Stepwise approach to asthma therapy
•ICS: Inhaled corticosteroid
•LABA: Long acting β2 agonist
•OCS: Oral corticosteroid
Harrison II Vol. Page 1605
3
4
5
2

Acute Severe asthma1. High flow OXYGEN via mask2. Nebulised high dose beta2-
agonists 3. Intermittent repeated doses
(every 15-30 minutes) to continuous nebulisation
4. +Nebulised ipratropium -5. Steroid therapy - continue
oral prednisolone therapy for 3 days (children) or 5 days
6. Intravenous hydrocortisone -Patients unable to take oral medication.
7. IV fluids where dehydrated 8. Correction of hypokalaemia
9. Bolus IV magnesium sulphate - in those over 5 years with poorly responsive
10. IV[Infusion?] aminophylline - only used in patients with near-fatal or life threatening asthma with poor response
11. Antibiotics are not indicated routinely.
12. May require intubation.

Aerosol Delivery of Drugs
• Accomplishes topical application• Most of Anti asthma drugs, Otherwise systemically
toxic• Particles >10 mm – deposited in mouth and
oropharynx,• Particles smaller than 0.5 mm are inhaled to the
alveolae and subsequently exhaled without being deposited in the lungs.
• Particles with a diameter of 1 to 5 mm deposited in small airways hence the most effective.
• Unfortunately, no system in use produces particles limited to the appropriate size range.

Metered dose Inhaler

Step1:Shake the inhaler well.
Step 2: Breathe out gently, place the mouthpiece in the mouth with lips curled around it.
Step 3: Begin breathing in slowly but at the same time, press down on the inhaler canister.
Step 4: Continue breathing in slowly and steadily until the lungs are full.
Step 5: Hold your breath for 10 seconds or for as long as comfortable. Breathe out slowly.
MDI

Rotahaler
Step 1: Insert a rotacap, transparent end first, into the raised square hole of the rotahaler
Step 2: Rotate the base of the Rotahaler in order to separate the two halves of the rotacap.
Step 3: Breathe in as deeply as you can*. Hold your breath for 10 seconds. Breathe out slowly.
*Note: If you are breathing correctly, you will hear the soft rattling sound of the rotacap.

How to use the Spacer[Less cordination required]
Step 1: Assemble your Spacer by fitting the two parts together
Step 2: Shake the Inhaler. Fill the inhaler into the slot opposite the mouthpiece.
Step 3: Close your lips firmly around the mouthpiece.
Step 4: Release a dose of medicine into the Spacer and breathe in steadily and deeply through your mouth.
Step 5: Remove the Spacer and hold your breath for as long as comfortable. Breathe out slowly
Zerostat Spacer

Nebulizer
MDI•Drug micronizedAnd under pressure•Sprayed into the mouth•Then pt.inhales
Rotahaler•Powder in a capsule•Pt effort is•Required to draw the drug and inhale
Nebulizer•Drug driven by compressed air/oxygen•Motorized•Less pt effort•Emergencies•Expensive

Bronchial asthma
• Inflammatory disease• NSAIDs not effective! But may worsen.• Inflammation , secretions and
bronchospasm.• Each is targeted by appropriate group
of drugs• Severe asthma may be fatal• Regular medication very important.• Steroid phobia is ill placed.• Children are also not spared

New drugs targeting Th2 lymphocytes in asthma
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2259400 • J Occup Med Toxicol. 2008; 3(Suppl 1): S6.• Gaetano Caramori,1 David Groneberg,2 Kazuhiro
Ito,3 Paolo Casolari,1 Ian M Adcock,3 and Alberto Papi1