Overview of contraception
-
Upload
obsgynhsnz -
Category
Education
-
view
1.926 -
download
2
Transcript of Overview of contraception

OVERVIEW OF OVERVIEW OF CONTRACEPTIONCONTRACEPTION
DR SHABBIR AHMAD DR SHABBIR AHMAD SHEIKHSHEIKH
PENSYARAH (UNISZA)PENSYARAH (UNISZA)
Dan PAKAR O&G (HSNZ)Dan PAKAR O&G (HSNZ)

INTRODUCTIONINTRODUCTION• According to figures from the population Reference Bureau, there are 8300 million humans on the
planet.• There are 42 births and 17 deaths
every 10 seconds, a net gain of 25 extra people somewhere on the globe every 10 seconds.

INTRODUCTIONINTRODUCTION
• According to UN figures, out of about 180 million conceptions each year, at least 75 million are unwanted.
• This results in about 50 million abortions.
• Around 600 000 women die each year (one woman/min)- killed by pregnancies.
• 200 000 would not die if adequate services/contraception make available to them

CHOOSING CONTRACEPTIVE METHOD
• Individual general health• Frequency of sexual relationship• Consideration for adolescent women• Number of partners• Considerations for women who have recently
given birth• Considerations for women near menopauseReligion and Moral belief

COUNSELLING
• Mode of action• Effectiveness• Side effects • Benefits• How to use the method

TYPES OF TYPES OF CONTRACEPTIONCONTRACEPTION

Types of contraceptionTypes of contraception1. 1. Oral contraceptionOral contraception
Combined oral contraceptiveCombined oral contraceptive Progestogen–only pills/ Mini- PillProgestogen–only pills/ Mini- Pill
2. Injectable contraception2. Injectable contraception Progestogen only injectablesProgestogen only injectables
• DMPA : Depo-provera (depot medroxyprogesterone acetate)DMPA : Depo-provera (depot medroxyprogesterone acetate)• NET-EN : norethisterone enantateNET-EN : norethisterone enantate
Combined injectable contraceptiveCombined injectable contraceptive• Cyclofem/ Lunelle Cyclofem/ Lunelle • MesignaMesigna
3. Implant3. Implant Implanon (etonogestrel implant)Implanon (etonogestrel implant) Norplant/ Jadelle (levonorgestrel implant)Norplant/ Jadelle (levonorgestrel implant)
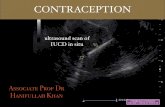
4. Intrauterine devices4. Intrauterine devices LNG IUD : MIRENALNG IUD : MIRENA Copper IUDCopper IUD

Types of contraceptionTypes of contraception5. Combined Hormonal Patch : EVRA5. Combined Hormonal Patch : EVRA
6. Combined Hormonal Ring : Nuva Ring6. Combined Hormonal Ring : Nuva Ring
7. Barrier methods7. Barrier methods - Male condom- Male condom
DiaphragmDiaphragm Cervical capCervical cap Sponges & spermicidesSponges & spermicides
8. Periodic abstinence8. Periodic abstinence CalenderCalender Ovulation methodOvulation method Sympto-thermalSympto-thermal Hormone monitoringHormone monitoring
9. Sterilisation9. Sterilisation Female : BTLFemale : BTL Male : VasectomyMale : Vasectomy

USED OF CONTRACEPTION IN UKUSED OF CONTRACEPTION IN UK
METHOD OF CONTRACEPTION USE (%)
Combined oral contraceptive pill 36
Condoms 28
Intrauterine contraception (copper device & Mirena®)
7
Injectable medroxyprogesterone acetate (DMPA or Depo-Provera®)
4
Withdrawal (coitus interruptus) 4
Natural family planning 3
Implanon® 2
Diaphragms <1
Sterilization 11
Vasectomy 13

COMBINED HARMONAL COMBINED HARMONAL CONTRACEPTIVESCONTRACEPTIVES

PreparationsPreparations
COCP (The Pill)COCP (The Pill) Injectables Injectables Patch - EVRAPatch - EVRA®® Vaginal ring – NUVA RINGVaginal ring – NUVA RING®®

1. COMBINED ORAL 1. COMBINED ORAL CONTRACEPTIVE PILL CONTRACEPTIVE PILL
(THE PILL)(THE PILL)

The PillThe Pill
• Oral contraceptives have gone through many changes through the years since they were introduced in the 1960s.
• When taken regularly and according to the directions, birth control pills are 98% to 99% effective in preventing pregnancy

Combined oral contraceptive pills
• “The pill” contains combination of two hormones- Synthetic oestrogen- Synthetic progesterone

FORMULATIONS FORMULATIONS Low dose, 2Low dose, 2ndnd generation Pills generation Pills
1.1.EE (20mcg) + NET (1mg) EE (20mcg) + NET (1mg) LoestrinLoestrin
2.2.EE (20mcg) + LNG (100mcg)EE (20mcg) + LNG (100mcg) LoetteLoette
Low dose, 3rLow dose, 3rdd generation Pills generation Pills
1.1.EE (20mcg) + Desogestrel 150mgEE (20mcg) + Desogestrel 150mg MercilonMercilon
2.2.EE (20mcg) + Gestodene 75mcgEE (20mcg) + Gestodene 75mcg MalianeMaliane
Low dose, 4Low dose, 4thth generation Pills generation Pills
1. EE (20mcg) + Drospirenone 3mg1. EE (20mcg) + Drospirenone 3mg YAZYAZ

FORMULATIONS FORMULATIONS
Standard dose, 2Standard dose, 2ndnd generation Pills generation Pills
1.1.EE (30mcg) + LNG (150mcg)EE (30mcg) + LNG (150mcg) NordetteNordette
Standard dose, 3rStandard dose, 3rdd generation Pills generation Pills
1.1.EE (30mcg) + Desogestrel 150mcgEE (30mcg) + Desogestrel 150mcg MarvelonMarvelon
2.2.EE (30mcg) + Gestodene 75mcgEE (30mcg) + Gestodene 75mcg MinuletMinulet
Standard dose, 4Standard dose, 4thth generation Pills generation Pills
1. EE (30mcg) + Drospirenone 3mg1. EE (30mcg) + Drospirenone 3mg YasminYasmin

FORMULATIONS FORMULATIONS
High dose, 2High dose, 2ndnd generation Pills generation Pills
1.1.EE (35mcg) + LNG EE (35mcg) + LNG TrinordiolTrinordiol
High dose EE + Anti-androgenHigh dose EE + Anti-androgen
1.1.EE (35mcg)+Ciproterone acetate 2mgEE (35mcg)+Ciproterone acetate 2mgDiane35Diane35
New COCPNew COCP
Estradiol + dienogest Estradiol + dienogest Qlair Qlair

Who Should Not Use Who Should Not Use the Pillthe Pill

WHO medical eligibity criteria WHO medical eligibity criteria for contraception use.for contraception use.

Who Should Not Use the PillWho Should Not Use the Pill
1. A history of pulmonary embolism or genetic disorders that could cause thrombosis (blood clots).
2. Uncontrolled hypertension 3. A history of stroke or heart attack 4. Severe liver disease 5. Migraine headaches with a
neurological component

Who Should Not Use the PillWho Should Not Use the Pill
6. Diabetes with retinopathy or kidney problems (diabetes alone does not prevent the use of the pill)
7. Estrogen-dependent cancer of the breast or endometrium

Mode of Action COCPMode of Action COCP
Suppression of ovulationSuppression of ovulation By prevention of ovarian follicular maturationBy prevention of ovarian follicular maturation By interrupting the oestrogen-mediated positive By interrupting the oestrogen-mediated positive
feedback on the hypothalamic-pituitary axis thus feedback on the hypothalamic-pituitary axis thus preventing LH surgepreventing LH surge
Thicken the cervical mucus Thicken the cervical mucus reduce sperm penetrabilityreduce sperm penetrability
Thinning of the endometrium Thinning of the endometrium reducing likelihood of implantationreducing likelihood of implantation

When to take the pill?When to take the pill?In principal: at any time if it is reasonably certain that the woman is not pregnantIn principal: at any time if it is reasonably certain that the woman is not pregnant

How to take the pill?How to take the pill?
1 pill is taken every day for 21 days and followed by 7 1 pill is taken every day for 21 days and followed by 7 days of pill free period, during which the women will have days of pill free period, during which the women will have a ‘withdrawal bleed’. a ‘withdrawal bleed’. For YAZ , 24days & 4 days pill free For YAZ , 24days & 4 days pill free period.period.
Timing is not as critical as it is with POPs, but it is a good Timing is not as critical as it is with POPs, but it is a good practice to get into habit of taking the pill at a similar time practice to get into habit of taking the pill at a similar time every day.every day.

Missed pillsMissed pills
PrincipalPrincipal
It takes 7 consecutive pills to ensure that It takes 7 consecutive pills to ensure that ovulation has been suppressedovulation has been suppressed
It is thus vital to avoid lengthening the pill free It is thus vital to avoid lengthening the pill free week to more than 7 daysweek to more than 7 days

Missed 1Missed 1stst week week
If pills are missed in the FIRST 7 DAYS of If pills are missed in the FIRST 7 DAYS of pill taking, the ovaries will not have 7 pill taking, the ovaries will not have 7 consecutive pills to ensure suppression of consecutive pills to ensure suppression of ovulation following pill-free week THUS ovulation following pill-free week THUS emergency contraception should be given emergency contraception should be given if necessary and EXTRA PRECAUTIONS if necessary and EXTRA PRECAUTIONS used until seven further pills have been used until seven further pills have been taken without a breaktaken without a break

Missed 2Missed 2ndnd week week
If pills are missed in the SECOND 7 DAYS If pills are missed in the SECOND 7 DAYS of the packet then the ovaries will have at of the packet then the ovaries will have at least 7 pills to ensure suppression of least 7 pills to ensure suppression of ovulation ovulation THUS theoretically THUS theoretically emergency emergency contraception and extra precaution contraception and extra precaution SHOULD NOT BE NEEDED.SHOULD NOT BE NEEDED.

Missed 3Missed 3rdrd week week
If pills are missed in the THIRD 7 DAYS of pill If pills are missed in the THIRD 7 DAYS of pill taking the next packet of pills should be started taking the next packet of pills should be started WITHOUT having PILL FREE WEEKWITHOUT having PILL FREE WEEK
This is again to ensure that seven consecutive This is again to ensure that seven consecutive days of pill taking is achieved before allowing 7 days of pill taking is achieved before allowing 7 days free from the pilldays free from the pill
IN PRACTICE women will find it easier to have 1 IN PRACTICE women will find it easier to have 1 set of rules to cover all eventualities set of rules to cover all eventualities

Missed pillsMissed pills

When to stop?When to stop? In a fit and healthy woman In a fit and healthy woman with no contraindications to with no contraindications to
taking the pill, there is no need to stop just because of taking the pill, there is no need to stop just because of age.age.
However, with regular bleeds and normal levels of However, with regular bleeds and normal levels of oestrogen, the oestrogen, the onset of the menopause will be maskedonset of the menopause will be masked..
It is wise to It is wise to choose the age of 50 to stop the COC choose the age of 50 to stop the COC pill pill and use another method of contraceptionand use another method of contraception
Taking COCP would mask common bld markers of the Taking COCP would mask common bld markers of the menopause such as oestradiol and FSH levels – this menopause such as oestradiol and FSH levels – this effect disappears after 6 weeks effect disappears after 6 weeks and levels of these and levels of these markers can be relied on.markers can be relied on.

AdvantagesAdvantages High efficacyHigh efficacy
Failure rate (pearl index) 0.1-1/100 woman yearsFailure rate (pearl index) 0.1-1/100 woman years ReversibleReversible
Prompt return to ovulation with 70% of women ovulating in Prompt return to ovulation with 70% of women ovulating in the 1the 1stst cycle and 98% by the 3 cycle and 98% by the 3rdrd cycle cycle
Not related to intercourseNot related to intercourse Reduction in menstrual blood flowReduction in menstrual blood flow
Reduced the menstrual blood flow by 50% Reduced the menstrual blood flow by 50% especially with YAZespecially with YAZ

AdvantagesAdvantages
Less dysmenorhoeaLess dysmenorhoea Reduce menstrual prostaglandin release thus reducing Reduce menstrual prostaglandin release thus reducing
uterine contractility and dysmenorrhoeauterine contractility and dysmenorrhoea
Predictability of mensesPredictability of menses Treats PMS/PMDD, Treats PMS/PMDD, especially with YAZ.especially with YAZ. Reduction in benign breast diseaseReduction in benign breast disease Reduction in functional ovarian cystReduction in functional ovarian cyst Reduction in PIDReduction in PID
Due to progesterone effect on cervical mucus- increase viscosity Due to progesterone effect on cervical mucus- increase viscosity impedes ascent of pathogens and may confer protective effect. impedes ascent of pathogens and may confer protective effect.
Lower menstrual flow also reduces bacterial growthLower menstrual flow also reduces bacterial growth

AdvantagesAdvantages
Reduction in ectopic pregnancy rateReduction in ectopic pregnancy rate All forms of contraception reduce the incidence of ectopic All forms of contraception reduce the incidence of ectopic
pregnancypregnancy Risk of ectopic pregnancy in COCP users is 0.005 per 1000 Risk of ectopic pregnancy in COCP users is 0.005 per 1000
woman years, comparable to that associated with vasectomy woman years, comparable to that associated with vasectomy and lower than the risk associated with barrier contraception, and lower than the risk associated with barrier contraception, IUCD or tubal ligationIUCD or tubal ligation
Reduction in ovarian and endometrial cancerReduction in ovarian and endometrial cancer COCP use for 4 and 8 years associated with 40% and 51% reduction in COCP use for 4 and 8 years associated with 40% and 51% reduction in
risk of ovarian cancer respectively risk of ovarian cancer respectively COCP use for 4 and 8 years associated with 54% and 66% reduction in COCP use for 4 and 8 years associated with 54% and 66% reduction in
risk of endometrial cancer respectivelyrisk of endometrial cancer respectively

DisadvantagesDisadvantages Cardiovascular effectCardiovascular effect
VTEVTE Myocardial infarctionMyocardial infarction Cerebrovascular accidentsCerebrovascular accidents Raised blood pressureRaised blood pressure
Breast cancerBreast cancer Cervical cancerCervical cancer
Compared with never users of oral contraceptives, the relative risks Compared with never users of oral contraceptives, the relative risks of cervical cancer increased with increasing duration of useof cervical cancer increased with increasing duration of use
Liver adenoma or carcinomaLiver adenoma or carcinoma CholestasisCholestasis GallstonesGallstones

2.INJECTABLE COMBINED 2.INJECTABLE COMBINED CONTRACEPTIVESCONTRACEPTIVES

Injectable combined contraceptiveInjectable combined contraceptive
1. Cyclofem/ Lunelle . 1. Cyclofem/ Lunelle . (25mg Medroxyprogesterone 25mg Medroxyprogesterone acetate & 5mg oestradiol cypionate)acetate & 5mg oestradiol cypionate)
2. Mesigyna . 2. Mesigyna . (Norethisterone enantate & estradiol Norethisterone enantate & estradiol valerate)valerate)
Given once monthly by intramuscular injection – Given once monthly by intramuscular injection – every 4 weeks +/- 7 daysevery 4 weeks +/- 7 daysAdvantages over IM depo:Advantages over IM depo:
Improved bleeding patterns and swift return of Improved bleeding patterns and swift return of fertility on discontinuationfertility on discontinuation

3. COMBINED 3. COMBINED CONTRACEPTIVE PATCHCONTRACEPTIVE PATCH

ORTHO EVRA ORTHO EVRA Contains Contains 6mg norelgestromin 6mg norelgestromin and 0.75mg ethinyl oestradioland 0.75mg ethinyl oestradiol
20 cm squared trans-dermal system –apply at upper 20 cm squared trans-dermal system –apply at upper outer outer arm, abdomen, buttock and backarm, abdomen, buttock and back
The patch is The patch is changed every 7 days changed every 7 days for 3 weeks with a drug-for 3 weeks with a drug-free 7 day intervalfree 7 day interval
Patient compliance is significantly higher with the contraceptive patch compared to oral contraceptive pills
But expensive.
Pearl index = 0.88. In comparative Pearl index = 0.88. In comparative trials, efficacy better than , efficacy better than COCPCOCP

Transdermal Contraceptive Transdermal Contraceptive System: DescriptionSystem: Description
• 3-patch system– Apply 1 patch each week for 3 weeks– Apply each patch the same day of the
week
• 1 week is patch-free
Week 1 Week 2 Week 3 Week 4
Patch #1 Patch #2 Patch #3
28-day cycle
Patch-free
Week 5
Start next cycle
28-day cycle
Abrams LS, et al. J Clin Pharmacol. 2001;41:1232-1237, 1301-1309; Abrams LS, et al. Contraception. 2001;64:287-294; Creasy GW, et al. Semin Reprod Med. 2001;19:373-380; Audet MC, et al. JAMA. 2001;285:2347-2354; Smallwood GH, et al. Obstet Gynecol. 2001;98:799-805.

Transdermal Contraceptive Patch: Transdermal Contraceptive Patch: ApplicationApplication
• Size: 20 cm2 • Composed of 3 layers:
– a release liner removed at the moment of application
– a medicated adhesive layer– An outer protective polyester
layer • Applied to the buttocks,
upper outer arm, lower abdomen, or the upper torso (excluding the breast)
Keder LM. J Pediatr Adolesc Gynecol. 2002;15:179-181.

Transdermal Contraceptive Patch: Transdermal Contraceptive Patch: AdvantagesAdvantages
• Weekly application encourages compliance
• Easy verification of presence reassures user of continued protection
• Does not require vaginal insertion
• Contraceptive effects are rapidly reversible
• Excellent cycle control after 3 months

Transdermal Contraceptive Patch: Transdermal Contraceptive Patch: DisadvantagesDisadvantages
• Application site reactions • Not as effective in women
weighing >198 pounds• Side effects are similar to
oral contraceptives except for:
- higher rates of breast pain during first 2 months
- higher rates of dysmenorrhea
• May be difficult to conceal• No protection against HIV or
other sexually transmitted infectionsZieman M, et al. Fertil Steril. 2002;77(Suppl 2):S13-S18.

Transdermal Contraceptive Patch: Pooled Transdermal Contraceptive Patch: Pooled Analysis of EfficacyAnalysis of EfficacyThrough 13 CyclesThrough 13 Cycles
22,160 Cycles
Number of Pregnancie
s
Probability of Pregnancy*
Method Failure
12 0.8%
UserFailure
3 0.6%
*Kaplan-Meier estimates of the cumulative probabilities of pregnancy.
Zieman M, et al. Fertil Steril. 2002;77(Suppl 2):S13-S18; Smallwood GH, et al. Obstet Gynecol. 2001;98(Pt 1):799-805; Audet MC, et al. JAMA. 2001;285:2347-2354; Hedon B, et al. Int J Gynaecol Obstet. 2000:70(suppl 1):78.

Efficacy of the Contraceptive PatchEfficacy of the Contraceptive PatchVersus an Oral ContraceptiveVersus an Oral Contraceptive
Cycles
No. of Pregnancies
Probability of Pregnancy Pearl Index
Method
failureUser
failure
Method
failureOveral
lMethod
* Overall†
Patch(n=811)
5,240 4 1 1.1 1.3 0.99 1.24‡
OC(n=605)
4,167 4 3 1.3 1.8 1.25 2.18‡
Patch = Ortho Evra® transdermal patch; OC = Triphasil® oral contraceptive*Failure when taken as directed†User failure plus method failure ‡The difference in efficacy was not statistically significant
Audet MC, et al. JAMA. 2001;285:2347-2354.

Transdermal Contraceptive Patch: Transdermal Contraceptive Patch: Most Common Adverse Events Most Common Adverse Events
Audet MC, et al. JAMA. 2001;285:2347-2354.
Adverse Event
Number of Patients (%)
Ortho Evra® Patch
(n=812)
Oral Contraceptiv
e(n=605)
P Value
Headache 178 (21.9) 134 (22.1) 0.95
Nausea 166 (20.4) 111 (18.3) 0.34
Application site reaction 164 (20.2) – –
Breast discomfort* 152 (18.7) 35 (5.8) <0.001
Upper respiratory infection 108 (13.3) 108 (17.9) 0.02
Dysmenorrhea 108 (13.3) 58 (9.6) 0.04
Abdominal pain 66 (8.1) 51 (8.4) .85*Reported only during the first 2 study cycles.

Transdermal Contraceptive Patch:Transdermal Contraceptive Patch:Patient Counseling on Usage and DisposalPatient Counseling on Usage and Disposal• Application:
– Use a new location for each patch– Apply to clean, dry skin– Apply where it won’t be rubbed by clothing: on buttocks,
abdomen, upper outer arm, upper torso– Do not use on irritated or abraded skin– Do not use on the breasts– Avoid oils, creams, or cosmetics until after patch placement– Bathe and swim as usual
• Anticipate more breast discomfort during the first 2 months
• Store at room temperature • Do not cut, alter or damage the patch as if may alter
contraceptive efficacy• Do not flush a used patch into the water system; fold
the used patch in half and place in the trash

Transdermal Contraceptive Patch:Transdermal Contraceptive Patch:Patient Counseling on Basic InstructionsPatient Counseling on Basic Instructions• If switching from an oral contraceptive, apply the
patch as soon as withdrawal bleeding begins (Day 1 Start)
- Sunday Start: use backup protection for 7 days unless Sunday is the first day of the menstrual cycle
• Wear each patch for 7 days; subsequent patch changes are made on the same day of the week
• No more than 7 days should lapse between the application of the last patch of the prior 21-day cycle and the first patch of the next 21-day cycle
• For partial or full detachment, make sure the exposed undersurface of the patch is clean and adherent; press it into place for 10 seconds; if the patch does not adhere completely, remove it and replace it with another patch

28-Day Cycle (Days 1-28)
Patch #1
Days 1-7
Patch #2
Days 8-15
Patch #3
Days 16-21No Patch
Next 28-Day Cycle (Days 29-56)
This patch was not applied:• Apply a new patch immediately; this is the new “patch change day”• Use backup protection for 7 days• Consider emergency contraception
Patch application is 1 to 2 days late:• Apply new patch immediately; Make this the new “patch change day” • No backup protection is required
Patch application is >2 days late:• Immediately start new 21-day application cycle•Use backup protection for 7 days•Consider emergency contraception
Patch #1
This patch was not removed:• Remove immediately• Start cycle on day 29
Transdermal Contraceptive Patch:Transdermal Contraceptive Patch:Managing Missed or Late ApplicationsManaging Missed or Late Applications

Contraception During Perimenopause: Contraception During Perimenopause: Transdermal PatchTransdermal Patch
Available methods (Failure rates)*
• Ethinyl estradiol/norelgestromin patch (8%)
Prevents unintended pregnancy
Yes
Minimizes hormonal fluctuations
Yes
Provides additional health benefits
• Bone protection • Cycle control
Grimes DA, Wallach M, eds. Modern Contraception: Updates from The Contraception Report. 2007; Hatcher RA, Nelson AL. In: Contraceptive Technology. 2004:391-460.

Transdermal Contraceptive Patch:Transdermal Contraceptive Patch:Risk for Venous ThromboembolicRisk for Venous Thromboembolic
Events*Events*
Jick SS, et al. Contraception. 2006;73:223-228;Cole JA, et al. Obstet Gynecol. 2007;109:339-346.
Relevant Studies
Odds Ratio (95% Confidence
Interval)
Jick SS, et al., 2006
0.9 (0.5–1.6)
Cole JA, et al., 2007
2.4 (1.1–5.5)
*Women should be counseled that all combined contraceptive products increase the risk of venous thromboembolic events; use of these products should be discontinued if a patient becomes immobilized.

4. COMBINED 4. COMBINED CONTRACEPTIVE CONTRACEPTIVE
VAGINAL RINGVAGINAL RING

NUVANUVA ring ring• It is made of latex-free plastics.• Diameter : 54 mm• CONTAINS ethinyl estradiol 15
ug and etonorgestrel 120 ug.• The ring is worn for 21 days
and removed for 7 days to allow withdrawal bleedings.
• Same risks and benefits as COC but is more expensive.
• Cycle control is better & breakthrough bleeding is less common.
• Efficacy is 99.4%.• If remain inserted >4wks
backup contraception untill new ring has been in place for 7 days.

Progestogen-only Progestogen-only Hormonal contraceptionHormonal contraception

1.Progestogen only Pill 1.Progestogen only Pill (mini-pill)(mini-pill)

FormulationsFormulations
Ethynodiol diacetate 500mcgEthynodiol diacetate 500mcgFFemulenemulen
Norethisterone 350mcgNorethisterone 350mcgNoriday / MicronorNoriday / Micronor Levonorgestrel 30mcgLevonorgestrel 30mcg Microval Microval Norgestrel 75mcg Norgestrel 75mcg NeogestNeogest Desogestrel Desogestrel CerazetteCerazette

Progestogen-only PillsProgestogen-only Pills
Suitable for women with VTE, migraine, older Suitable for women with VTE, migraine, older women who smoke, women with hypertension, women who smoke, women with hypertension, valvular heart disease and diabetes mellitus – valvular heart disease and diabetes mellitus – avoids oestrogenic S/E of COCPavoids oestrogenic S/E of COCP
ContraindicationsContraindications PregnancyPregnancy Undiagnosed vaginal bleedingUndiagnosed vaginal bleeding Severe arterial diseaseSevere arterial disease Liver adenomaLiver adenoma

AdvantagesAdvantages Failure rate 0.3-3/100 women yearsFailure rate 0.3-3/100 women years Effective when used correctlyEffective when used correctly well toleratedwell tolerated No artificial oestrogen component thus all of the s/e No artificial oestrogen component thus all of the s/e
related to oestrogen e.g. risk of circulatory disease are related to oestrogen e.g. risk of circulatory disease are potentially absentpotentially absent
Readily reversible method of contraceptionReadily reversible method of contraception Efficacy increases with age and may be reduced if Efficacy increases with age and may be reduced if
weight > 70kgweight > 70kg Do not affect the raised FSH and oestradiol levels Do not affect the raised FSH and oestradiol levels
associated with menopause thus reduce the problems of associated with menopause thus reduce the problems of diagnosing the menopause on hormonal contraceptiondiagnosing the menopause on hormonal contraception

DisadvantagesDisadvantages
Strict adherence to the rules of pill taking Strict adherence to the rules of pill taking is essentialis essential
Pattern of bleeding is unpredictablePattern of bleeding is unpredictable Associated with increased incidence of Associated with increased incidence of
ovarian follicular cysts and increased risk ovarian follicular cysts and increased risk of ectopic pregnancy (compared to COCP)of ectopic pregnancy (compared to COCP)

Mode of actionMode of action Main effect : Thicken cervical mucus thus Main effect : Thicken cervical mucus thus
decreased sperm penetrability of cervixdecreased sperm penetrability of cervix Reduce receptivity of endometrium to Reduce receptivity of endometrium to
implantationimplantation Reduction in ovulationReduction in ovulation
Suppress ovulation in Suppress ovulation in ~~40%, this is unpredictable and varies 40%, this is unpredictable and varies between cycles resulting in irregular menstruationbetween cycles resulting in irregular menstruation
10-15% of women have complete inhibition of ovarian activity 10-15% of women have complete inhibition of ovarian activity and are amenorrhoeicand are amenorrhoeic
50%have regular ovulatory cycles with normal luteal phase 50%have regular ovulatory cycles with normal luteal phase and a normal menstrual cycleand a normal menstrual cycle
Reduce fallopion tube motilityReduce fallopion tube motility

How to take?How to take? One tablet daily taken on day 1 of cycle and taken One tablet daily taken on day 1 of cycle and taken
continuously without a breakcontinuously without a break Should be taken at the same time every day and Should be taken at the same time every day and
within 3 hrs at the mostwithin 3 hrs at the most If pill missed for more than 3 hrs, additional If pill missed for more than 3 hrs, additional
precautions needed for following 2 days – precautions needed for following 2 days – An estimated An estimated 48hrs of POP use was deemed necessary to achieve the contraceptive effects on 48hrs of POP use was deemed necessary to achieve the contraceptive effects on cervical mucuscervical mucus
Maximal effect on cervical mucus is at 4 hrs after pill Maximal effect on cervical mucus is at 4 hrs after pill takingtaking
The only antibiotics that would reduce the efficacy of The only antibiotics that would reduce the efficacy of the POP are the enzyme inducer such as rifampicin or the POP are the enzyme inducer such as rifampicin or griseofulvingriseofulvin

When to take the pill?When to take the pill?
POP can be started at any time if POP can be started at any time if pregnancy can be excludedpregnancy can be excluded
First day or two of menses, if started later First day or two of menses, if started later than this – extra precautions needed for than this – extra precautions needed for following 7 daysfollowing 7 days
Can be started immediately following a Can be started immediately following a miscarriage or termination of pregnancymiscarriage or termination of pregnancy
When changing from COCs, an immediate When changing from COCs, an immediate switch is recommendedswitch is recommended

CerrazetteCerrazette®®
Released in 2003Released in 2003 Contain 3Contain 3rdrd generation of progestogen – generation of progestogen –
desogestrel 75mcgdesogestrel 75mcg Evidence show that it inhibits ovulation in 97% of Evidence show that it inhibits ovulation in 97% of
cyclescycles Window period of 12 hours Window period of 12 hours instead of 3 hoursinstead of 3 hours Taken every day with no breakTaken every day with no break Useful for younger women who cannot or do not Useful for younger women who cannot or do not
wish to take oestrogen containing products or wish to take oestrogen containing products or women who cannot tolerate other POPs.women who cannot tolerate other POPs.

2. INJECTABLE 2. INJECTABLE PROGESTOGENSPROGESTOGENS

INJECTABLESINJECTABLES
PreparationsPreparations• DMPA : Depo-provera (depot DMPA : Depo-provera (depot
medroxyprogesterone acetate)medroxyprogesterone acetate)• NET-EN : norethisterone enantateNET-EN : norethisterone enantate
Main effect : inhibition of ovulationMain effect : inhibition of ovulation Also has effect on endometrial and cervical mucusAlso has effect on endometrial and cervical mucus

Depo-proveraDepo-provera®® Depo-Depo-
medroxyprogesterone medroxyprogesterone acetate 150mgacetate 150mg
Deep im injectionDeep im injection Every 3 months +/- 2 Every 3 months +/- 2
weeksweeks Failure rate 0.25-0.5/100 Failure rate 0.25-0.5/100
woman yearswoman years Use of broad spectrum Use of broad spectrum
antibiotics do not antibiotics do not compromised efficacy compromised efficacy since the route does not since the route does not depend on absorption depend on absorption from the gutfrom the gut

BenefitsBenefits Suitable for women Suitable for women
who forget to take pills, particularly travellers, due to frequent changes who forget to take pills, particularly travellers, due to frequent changes in time zones, missed pills are likely or where suboptimal compliance is in time zones, missed pills are likely or where suboptimal compliance is expectedexpected
Who wish for a secret or ‘private’ methodWho wish for a secret or ‘private’ method In whom oestrogen is contraindicated:In whom oestrogen is contraindicated: mild to moderate hypertension,diabetes mild to moderate hypertension,diabetes
mellitus in the absence of vascular disease, age >35yo & smoking)mellitus in the absence of vascular disease, age >35yo & smoking)
Associated with reduction in sickling crises in sufferers of Associated with reduction in sickling crises in sufferers of sickle cell disease and reduced frequency of seizures in sickle cell disease and reduced frequency of seizures in epileptic women having cyclical attacksepileptic women having cyclical attacks
Does not have any effect on the risk of ovarian and Does not have any effect on the risk of ovarian and endometrial cancerendometrial cancer
Little or no association with stroke, MI or VTE .Little or no association with stroke, MI or VTE .

Side effects & RisksSide effects & Risks Menstrual disturbances are likely with irregular frequent vaginal Menstrual disturbances are likely with irregular frequent vaginal
bleedingbleeding Amenorrhoea becomes more likely with repeated dosesAmenorrhoea becomes more likely with repeated doses
• 30% after 130% after 1stst dose dose• 55% after 455% after 4thth dose dose
Weight gainWeight gain 3-19% of users may develop headaches, dizziness, breast 3-19% of users may develop headaches, dizziness, breast
tenderness and mood changestenderness and mood changes Associated with delay in return to normal fertility Associated with delay in return to normal fertility
On average following a final injection of DMPA, ovulation returns On average following a final injection of DMPA, ovulation returns after 4-5 months, may be as long as 24 monthsafter 4-5 months, may be as long as 24 months
78% had conceived by 12 months and over 92% had conceived 78% had conceived by 12 months and over 92% had conceived by 24 months following discontinuationby 24 months following discontinuation
Thought to be due to slow metabolism of the drug from the Thought to be due to slow metabolism of the drug from the microcrystalline deposits in muscle tissuemicrocrystalline deposits in muscle tissue

Depo-provera and osteoporosisDepo-provera and osteoporosis There is evidence that depo-provera causes a significant There is evidence that depo-provera causes a significant
reduction in bone mineral density. This effect may be reduction in bone mineral density. This effect may be more important in adolescents. This reduction appears to more important in adolescents. This reduction appears to be partly reversible after discontinuation and resumption be partly reversible after discontinuation and resumption of ovarian activityof ovarian activity
In adolescentsIn adolescents, it should only be used after other , it should only be used after other methods have been considered and found to be methods have been considered and found to be unsuitable or unacceptableunsuitable or unacceptable
In all women, careful re-evaluation of risks and benefits In all women, careful re-evaluation of risks and benefits of treatment should be undertaken in those who wish to of treatment should be undertaken in those who wish to continue use for continue use for longer than 2 yearslonger than 2 years

Depo-subQ provera 104Depo-subQ provera 104
A new micronised, A new micronised, subcutaneous formulation subcutaneous formulation of Depo-proveraof Depo-provera® 104mg® 104mg
Every 12 weeksEvery 12 weeks Fewer side effects such Fewer side effects such
as weight gainas weight gain The efficacy and delay in The efficacy and delay in
return of fertility is similar return of fertility is similar with im depo-provera®with im depo-provera®
Can be self administeredCan be self administered

NoristeratNoristerat®®
200mg norethindrone enanthate200mg norethindrone enanthate Administered every 8 weeks +/- 2 weeksAdministered every 8 weeks +/- 2 weeks Less effect on bleeding patternLess effect on bleeding pattern Pearl index 0.4-2.0/100 woman yearsPearl index 0.4-2.0/100 woman years

3. PROGESTOGEN 3. PROGESTOGEN IMPLANTSIMPLANTS

ImplantImplant
PreparationsPreparations1.Implanon (etonogestrel 1.Implanon (etonogestrel implant)implant)
2.Norplant/ Jadelle 2.Norplant/ Jadelle (levonorgestrel implant)(levonorgestrel implant)

ImplanonImplanon 68mg 68mg etonorgestreletonorgestrel – active metabolite of desogestrel – active metabolite of desogestrel A single 40 mm rod, just 2 mm in diameter.A single 40 mm rod, just 2 mm in diameter. Initial release rate of 60-70mcg/day and falls gradually to Initial release rate of 60-70mcg/day and falls gradually to
around 25-30mcg at the end of 3 yearsaround 25-30mcg at the end of 3 years Inserted subdermally in the groove between biceps and Inserted subdermally in the groove between biceps and
triceps in the non-dominant hand about 8-10cm from the triceps in the non-dominant hand about 8-10cm from the medial epicondylemedial epicondyle
Can be administered up to day 5 of menses without the Can be administered up to day 5 of menses without the need for additional contraceptionneed for additional contraception
License for 3 years – efficacy may be lower during the 3License for 3 years – efficacy may be lower during the 3rdrd year in overweight womenyear in overweight women
Inhibit ovulation by prevention of LH surge, also affect Inhibit ovulation by prevention of LH surge, also affect cervical mucus thickening and endometriumcervical mucus thickening and endometrium

Implanon- timing of insertionImplanon- timing of insertion
Day 1 to day 5 of menses. If later than day Day 1 to day 5 of menses. If later than day 2, recommend additional contraception till 2, recommend additional contraception till day 7. If after day 7, must make sure day 7. If after day 7, must make sure abstinence.abstinence.
Immediate after 1Immediate after 1stst trimester abortion trimester abortion Day 21 after 2Day 21 after 2ndnd trimester abortion or trimester abortion or
deliverydelivery During breast feedingDuring breast feeding

Implanon- advantages & Implanon- advantages & benefitsbenefits
Feature of ‘forgetability’ / better complianceFeature of ‘forgetability’ / better compliance Long action plus high continuation ratesLong action plus high continuation rates Efficacy not being affected by broad-spectrum Efficacy not being affected by broad-spectrum
antibiotics antibiotics Oestrogen free- usable in past VTE, excellent Oestrogen free- usable in past VTE, excellent
choice for many diabeticschoice for many diabetics Unchanged blood pressureUnchanged blood pressure Can use in past ectopicsCan use in past ectopics Rapidly reversible- after removal 44/47 women Rapidly reversible- after removal 44/47 women
will ovulate within 3 weekswill ovulate within 3 weeks Failure rate fewer than 0.1/100 woman yearsFailure rate fewer than 0.1/100 woman years

Implanon- problems & Implanon- problems & disadvantagesdisadvantages
Menstrual disturbancesMenstrual disturbances Improve over 3-5 monthsImprove over 3-5 months NSAIDs and low dose COCs are generally effective NSAIDs and low dose COCs are generally effective
treatment strategies for implanon related bleedingtreatment strategies for implanon related bleeding Minor general side effects – acne, headache, Minor general side effects – acne, headache,
abdominal pain, breast pain, dizziness, mood abdominal pain, breast pain, dizziness, mood changes, reduced libido and hair losschanges, reduced libido and hair loss
Body weight – slight increaseBody weight – slight increase Possible hypo-oestrogenismPossible hypo-oestrogenism Local adverse effects – discomfort, expulsion, Local adverse effects – discomfort, expulsion,
migration and scarringmigration and scarring

Implanon - contraindicationsImplanon - contraindications
Absolute include progestogen dependant Absolute include progestogen dependant tumour, current severe hepatic disease, tumour, current severe hepatic disease, pregnancy, undiagnosed vaginal bleeding, pregnancy, undiagnosed vaginal bleeding, severe hypersensitivity and acute severe hypersensitivity and acute porphyriaporphyria
Relative include previous ectopic Relative include previous ectopic pregnancies and liver cirrhosispregnancies and liver cirrhosis

Levonorgestrel implantLevonorgestrel implant
Jadelle : 2 rods effective for 5 yearsJadelle : 2 rods effective for 5 years Norplant : Norplant :
6 capsules labelled for 5 years usage6 capsules labelled for 5 years usage Released a low dose levonorgestrel at rate of Released a low dose levonorgestrel at rate of
30-35mcg/24h after 18 months30-35mcg/24h after 18 months Failure rate 0.2-1/100 women yearsFailure rate 0.2-1/100 women years Large studies have found that it is effective for Large studies have found that it is effective for
7 years (in women <70kg)7 years (in women <70kg) No more available in UK marketNo more available in UK market

4.INTRAUTERINE 4.INTRAUTERINE DEVICESDEVICES


LNG IUD : MIRENA LNG IUD : MIRENA
Long-acting, rapidly Long-acting, rapidly reversiblereversible
52mg levonorgestrel 52mg levonorgestrel released at the rate of released at the rate of 20mcg/ day20mcg/ day
Frame is rendered radio-Frame is rendered radio-opaque by impregnation opaque by impregnation with barium sulphatewith barium sulphate
Width is 4.8mmWidth is 4.8mm Licensed for Licensed for
contraception for 5 yearscontraception for 5 years

LNG IUD : MIRENA LNG IUD : MIRENA
The contraceptive effect is achieved by The contraceptive effect is achieved by profound endometrial glandular and stromal atrophy, profound endometrial glandular and stromal atrophy,
a decidualisation effect and a foreign body effect in a decidualisation effect and a foreign body effect in the uterus rendering the endometrium unresponsive the uterus rendering the endometrium unresponsive to oestrogento oestrogen
Changes in the cervical mucus which prevent ascent Changes in the cervical mucus which prevent ascent of spermatozoaof spermatozoa
After removal, endometrial morphology returns After removal, endometrial morphology returns to normal with menstruation within 30 daysto normal with menstruation within 30 days
Failure rate of 0.09/100 women yearsFailure rate of 0.09/100 women years

When to use?When to use?
May be fitted up to 7 day of menstrual cycle May be fitted up to 7 day of menstrual cycle without need of additional contraceptionwithout need of additional contraception
Or at any time in the menstrual cycle with barrier Or at any time in the menstrual cycle with barrier contraceptives for the next 7 days, if it is contraceptives for the next 7 days, if it is reasonably certain that the woman is not reasonably certain that the woman is not pregnantpregnant
It may be fitted at the time of 1It may be fitted at the time of 1stst trimester trimester surgical abortionsurgical abortion
It is preferable to wait 6 weeks later following It is preferable to wait 6 weeks later following late 2late 2ndnd trimester abortion trimester abortion

Benefits including non-Benefits including non-contraception contraception
Return to fertility is rapidReturn to fertility is rapid Management of menorrhagiaManagement of menorrhagia
Reduction in menstrual blood loss of up to 97% after Reduction in menstrual blood loss of up to 97% after 12 months of use with an increase in serum ferritin 12 months of use with an increase in serum ferritin and Hb concentration.and Hb concentration.
DysmenorrhoeaDysmenorrhoea Low rate of ectopic pregnancyLow rate of ectopic pregnancy Management of endometrial hyperplasiaManagement of endometrial hyperplasia Protection against STD- thickening of cervical mucus, Protection against STD- thickening of cervical mucus,
inactivation of the endometrium and reduced bleedinginactivation of the endometrium and reduced bleeding Cost effectiveness – compare to cost of hysterectomy/ Cost effectiveness – compare to cost of hysterectomy/
medical treatment for menorrhagiamedical treatment for menorrhagia Progesteron arm of HRT in perimenopausal women.Progesteron arm of HRT in perimenopausal women.

Side effects/ complicationsSide effects/ complications Difficulties might be encounter with insertion especially in Difficulties might be encounter with insertion especially in
nulliparous womannulliparous woman Irregular bleeding – takes 3 months for endometrial Irregular bleeding – takes 3 months for endometrial
atrophyatrophy Increased incidence of functional ovarian cysts Increased incidence of functional ovarian cysts
compared to copper IUD userscompared to copper IUD users Amenorrhoea Amenorrhoea
unless appropriately counselled, some women may regard this unless appropriately counselled, some women may regard this as abnormalas abnormal
Occurs in 20% of womenOccurs in 20% of women Prosgestogenic side effects – oedema/ headache/ breast Prosgestogenic side effects – oedema/ headache/ breast
tenderness/ acne – subside after a few monthstenderness/ acne – subside after a few months Expulsion – commonly occurs during first month Expulsion – commonly occurs during first month
following insertionfollowing insertion

COPPER IUCDCOPPER IUCD 11stst generation generation
Copper sevenCopper seven Copper T 200Copper T 200
22ndnd generation generation Multiload 250Multiload 250 Nova TNova T
33rdrd generation generation Copper T380Copper T380 Multiload 375Multiload 375

Cu T 380 Cu T 380
Licensed for 8 years in the UKLicensed for 8 years in the UK First choice of IUCDFirst choice of IUCD Low failure rateLow failure rate
1.4-2.2/100 women over 5 years1.4-2.2/100 women over 5 years Low expulsion rateLow expulsion rate
~8/100 women over 5 years~8/100 women over 5 years

GyneFIX IUCDGyneFIX IUCD
Licensed for 5 yearsLicensed for 5 years Frameless device Frameless device with 6 copper beads with 6 copper beads
wound around a monofilament wound around a monofilament polypropylene threadpolypropylene thread
Should only be inserted by those who Should only be inserted by those who have received appropriate traininghave received appropriate training
Has similar efficacy to Cu T 380 but with Has similar efficacy to Cu T 380 but with significantly lower expulsion ratesignificantly lower expulsion rate 3.0/100 women at 3 years 3.0/100 women at 3 years vsvs 7.38/100 women 7.38/100 women


Copper IUDCopper IUD
Efficacy is dependent on the surface area Efficacy is dependent on the surface area of copperof copper
IUDs fitted after the 40IUDs fitted after the 40thth birthday need not birthday need not to be changed, since fertility declines to be changed, since fertility declines rapidly at this age and should be removed rapidly at this age and should be removed 1 year after the menopause1 year after the menopause

Complications of Copper IUD useComplications of Copper IUD use ExpulsionExpulsion
Most occur in the first year, especially in the first 3 monthsMost occur in the first year, especially in the first 3 months Increased risk of expulsion in woman withIncreased risk of expulsion in woman with
• heavy periodsheavy periods• Insertion within 6 weeks post-partumInsertion within 6 weeks post-partum• Previous expulsionPrevious expulsion• Inexperienced operatorInexperienced operator
Perforation Perforation Risk 1.2/1000 insertionsRisk 1.2/1000 insertions
Pelvic infectionPelvic infection 6 fold increase in risk of developing PID in the first 20 days following insertion compared 6 fold increase in risk of developing PID in the first 20 days following insertion compared
with any other timewith any other time Thereafter the risk of infection remains constant at 1.4/1000 womenThereafter the risk of infection remains constant at 1.4/1000 women
Increased menstrual lossIncreased menstrual loss Abdominal pain/ dysmenorrhoeaAbdominal pain/ dysmenorrhoea PregnancyPregnancy
Remove device gently if possible as soon as pregnancy is diagnosed : reduces the risk of Remove device gently if possible as soon as pregnancy is diagnosed : reduces the risk of spontaneous miscarriages by 50%spontaneous miscarriages by 50%
Exclude ectopic pregnancy ( risk 1:25 with IUCD)Exclude ectopic pregnancy ( risk 1:25 with IUCD)

WHO Medical Eligibility Criteria for IUD Use in WHO Medical Eligibility Criteria for IUD Use in Women with Certain Medical ConditionsWomen with Certain Medical Conditions
Medical Conditions
TCu-380AWHO Risk Category*
LNG-IUSWHO Risk Category*
Hypertension (controlled) 1 1
Multiple cardiovascular risk factors 1 2
History of DVT or pulmonary embolism 1 2
Stroke 1 2
Severe valvular heart disease (complicated)
2 2
HIV infection 2 2
AIDS (clinically well on antiretroviral therapy)
2 2
WHO. Medical Eligibility Criteria for Contraceptive Use. 3rd ed. 2004. Available at: http://www.who.int/reproductive-health/publications/mec/iuds.html.
AIDS = acquired immunodeficiency syndrome; DVT = deep vein thrombosis; HIV = human immunodeficiency virus; IUD = intrauterine device; LNG-IUS = levonorgestrel-releasing IUD; TCu-380A = copper-releasing IUD; WHO = World Health Organization
*Category 1= there are no restrictions for use of the contraceptive method; Category 2 = the benefits of using the contraceptive method generally outweigh the theoretical or proven risk

EMERGENCY EMERGENCY CONTRACEPTIONCONTRACEPTION

1. Yuzpe regime1. Yuzpe regime
EE 100mcg and LNG 500mcgEE 100mcg and LNG 500mcg
Given two tablets BD 12 hours apartGiven two tablets BD 12 hours apart
Given Given within 72 hours within 72 hours of unprotected intercourseof unprotected intercourse
Is likely to prevent Is likely to prevent 6 out of 8 pregnancies6 out of 8 pregnancies

2. Progesterone only2. Progesterone only
TWO regimesTWO regimes1. Single dose 1.5mg 1. Single dose 1.5mg levonorgestrellevonorgestrelEscapelleEscapelle
2. Two doses of 0.75mg 2. Two doses of 0.75mg levonorgestrel 12 hours apart levonorgestrel 12 hours apart LevonelleLevonelle
Is likely to prevent Is likely to prevent 7 out of 7 out of 8 pregnancies8 pregnancies

3. Progesterone receptor 3. Progesterone receptor ModulatorModulator
Ulipristal 30mg Ulipristal 30mg Marketed as Marketed as EllaOneEllaOne
It is used up to 120 hours following unprotected intercourse.
S/E – Vomiting
Not recommended to use >one time per cycle
If breast feeding avoid BF for next 36hrs.

4. Copper IUCD4. Copper IUCD spermicidal and blastocidal action of copper and the spermicidal and blastocidal action of copper and the
prevention of implantationprevention of implantation
Up to 5 days after the first act of unprotected coitusUp to 5 days after the first act of unprotected coitus
Can be removed when menses occurCan be removed when menses occur
Failure rate <1%Failure rate <1%
Main primary complicationsMain primary complications Uterine cramps/ bleedingUterine cramps/ bleeding Risk of infectionRisk of infection

5. Mifepristone ( RU486)5. Mifepristone ( RU486) Not licensed Not licensed for use as emergency contraceptionfor use as emergency contraception
progesterone antagonistprogesterone antagonist
Single dose of 600mg within 72 h of unprotected Single dose of 600mg within 72 h of unprotected sexual intercourse is highly effective and no sexual intercourse is highly effective and no pregnancies have been reported in randomised pregnancies have been reported in randomised trialstrials
Delay in subsequent menses is the main unwanted Delay in subsequent menses is the main unwanted side effect and seems to be dose related.side effect and seems to be dose related.

STERILISATIONSTERILISATION
Ratio of female to male Ratio of female to male sterilisation is 10:1sterilisation is 10:1

STERILISATIONSTERILISATION-intended to be permanent-intended to be permanent
MaleMale vasectomyvasectomy
FemaleFemale Mini LaparotomyMini Laparotomy
• The Pomeroy methodThe Pomeroy method• The Parkland techniqueThe Parkland technique• The Ushida methodThe Ushida method• The Irving methodThe Irving method• fimbriectomyfimbriectomy
LaparoscopicLaparoscopic• Filshie clipFilshie clip• Hulka clipHulka clip• Falope ringFalope ring
HysteroscopicHysteroscopic• Chemical method: quinacrineChemical method: quinacrine• Mechanical methodMechanical method
OvablocOvabloc®® Essure® deviceEssure® device

VasectomyVasectomy Local anaesthesia Local anaesthesia
whenever possiblewhenever possible
Involves division of the Involves division of the vas deferens.vas deferens.

VasectomyVasectomy Men should be advised to use contraception until Men should be advised to use contraception until
azoospermia is confirmedazoospermia is confirmed1.1. Testing should be done after 8 weeks of vasectomyTesting should be done after 8 weeks of vasectomy2.2. 2 samples not less than 4 weeks apart should be clear of 2 samples not less than 4 weeks apart should be clear of
spermsperm3.3. International Parenthood Federation suggested at least 20 International Parenthood Federation suggested at least 20
ejaculations are required to clear sperm before other ejaculations are required to clear sperm before other contraceptives methods should be discontinuedcontraceptives methods should be discontinued
Failure rates of 1:2000 in comparison to 1:200 in BTLFailure rates of 1:2000 in comparison to 1:200 in BTL Not associated with testicular cancer or heart diseaseNot associated with testicular cancer or heart disease Nearly 75% of men who undergo vasectomy will develop Nearly 75% of men who undergo vasectomy will develop
antisperm antibodiesantisperm antibodies

ComplicationsComplications ImmediateImmediate
Haematoma (1-2%)Haematoma (1-2%) Wound infection Wound infection
(up to 5%)(up to 5%) Failure Failure
• Due to failure of other Due to failure of other contraceptive methods in contraceptive methods in the initial post-op period the initial post-op period before azoospermia has before azoospermia has been confirmedbeen confirmed
LateLate Anti sperm antibody (75%)Anti sperm antibody (75%)
• Thought to be in response Thought to be in response to leakage of spermto leakage of sperm
• Harmless unless Harmless unless restoration of fertility is restoration of fertility is desireddesired
Sperm granulomaSperm granuloma• Presumably also in Presumably also in
response to leaked spermresponse to leaked sperm• Painful and persistentPainful and persistent• Can be effectively excisedCan be effectively excised
Chronic testicular painChronic testicular pain• Unknown causeUnknown cause

FEMALE STERILIZATIONFEMALE STERILIZATION

LAPAROSCOPIC LAPAROSCOPIC STERILISATIONSTERILISATION
Filshie clipFilshie clip Made of Titanium lined by silicone rubberMade of Titanium lined by silicone rubber Destroyed 4 mm of tubeDestroyed 4 mm of tube Failure rate 2-3/1000 proceduresFailure rate 2-3/1000 procedures
Hulka – Clemen clipHulka – Clemen clip A stainless steel spring with 2 plastic jaws made of LexanA stainless steel spring with 2 plastic jaws made of Lexan Destroyed about 3 mm of tubeDestroyed about 3 mm of tube 1 year pregnancy rate of 2/1000 women1 year pregnancy rate of 2/1000 women
Falope ringFalope ring Made of silicon rubber and using special design applicatorMade of silicon rubber and using special design applicator Placed over the loop of tubePlaced over the loop of tube It destroyed 2-3cm tube and difficult to applied if tube is thick / It destroyed 2-3cm tube and difficult to applied if tube is thick /
fibroticfibrotic Ischemia of loop give significant post op painIschemia of loop give significant post op pain

MINI LAPAROTOMYMINI LAPAROTOMY

1.The Pomeroy method1.The Pomeroy method A loop of the isthmic portion of the tube is elevated using A loop of the isthmic portion of the tube is elevated using
babcock and ligated and cut at its base.babcock and ligated and cut at its base.
The cut ends of the tube are cauterizedThe cut ends of the tube are cauterized

1.The Pomeroy method1.The Pomeroy method

2. The Parkland technique2. The Parkland technique
A 2-3 cm fenestration is made beneath the isthmic A 2-3 cm fenestration is made beneath the isthmic portion of the tube portion of the tube
Tube is ligated at both sites , 3cm apart.Tube is ligated at both sites , 3cm apart.
3cm portion of the tube is removed3cm portion of the tube is removed
Care must be taken not to pull on the suture during Care must be taken not to pull on the suture during ligation or during transection of the tube because this ligation or during transection of the tube because this can lead to shearing of the tube from underling mesentry can lead to shearing of the tube from underling mesentry resulting in bleedingresulting in bleeding

2. The Parkland technique2. The Parkland technique

3.The Uchida method3.The Uchida method Injection of vaso-constricting solution beneath the serosa Injection of vaso-constricting solution beneath the serosa
of the tube about 6 cm from the utero-tubal junction.of the tube about 6 cm from the utero-tubal junction.
The tube is ligated proximally and distally about 3cm The tube is ligated proximally and distally about 3cm apart and cut.apart and cut.
Ligated proximal stump is allowed to retract into the Ligated proximal stump is allowed to retract into the mesosalphinx and tmesosalphinx and the mesosalphinx is closed with he mesosalphinx is closed with purse-string suture. purse-string suture.
Ligated distal stump remained exteriorized.Ligated distal stump remained exteriorized.

3.The Uchida method3.The Uchida method

4. The Irving method4. The Irving method A fenestration is made beneath the tube about 4cm from A fenestration is made beneath the tube about 4cm from
the utero-tubal junction.the utero-tubal junction.
The tube is ligated proximally and distally about 3cm The tube is ligated proximally and distally about 3cm apart and resected.apart and resected.
A deep pocket is created in the myometrium on the A deep pocket is created in the myometrium on the posterior surface of uterus.posterior surface of uterus.
Ligated proximal end of the tube are sutured deep into Ligated proximal end of the tube are sutured deep into the myometrial tunnel.the myometrial tunnel.
Ligated distal stump remained exteriorized.Ligated distal stump remained exteriorized.

4. The Irving method4. The Irving method

Reversal of sterilisationReversal of sterilisation Reversal of female sterilizationReversal of female sterilization
Involves laparotomyInvolves laparotomy Does not always workDoes not always work Microsurgical techniques are associated with around Microsurgical techniques are associated with around
70% success70% success Carries a significant risk of ectopic pregnancy (up to Carries a significant risk of ectopic pregnancy (up to
5%)5%) Reversal of vasectomyReversal of vasectomy
Technically feasible in many cases with patency rates Technically feasible in many cases with patency rates of almost 90%of almost 90%
Pregnancy rates are much less (up to 60%) perhaps Pregnancy rates are much less (up to 60%) perhaps as a result of the presence of antisperm antibodiesas a result of the presence of antisperm antibodies

HYSTEROSCOPIC HYSTEROSCOPIC STERILISATIONSTERILISATION
QuinacrineQuinacrine
OvablocOvabloc®®
EssureEssure®®

1.Quinacrine1.Quinacrine Blind introduction of pellets of quinacrine into the Blind introduction of pellets of quinacrine into the
uterine cavity via an intrauterine device inserter.uterine cavity via an intrauterine device inserter.
The pellets dissolve near the both cornua, with The pellets dissolve near the both cornua, with some solution entering the tubes and causing a some solution entering the tubes and causing a fibrotic reactionfibrotic reaction
It involves the insertion of 252mg of quinacrine It involves the insertion of 252mg of quinacrine on two occasions one month aparton two occasions one month apart
Quoted efficacy of 98% at 2 yearsQuoted efficacy of 98% at 2 years

2.Ovabloc 2.Ovabloc intra-tubal deviceintra-tubal device
Mainly confined to a few centres in the Mainly confined to a few centres in the NetherlandsNetherlands
The procedures involves high pressure injection The procedures involves high pressure injection of viscous silicone into the ostium via a catheter.of viscous silicone into the ostium via a catheter.
The silicone conforms to the shape of the The silicone conforms to the shape of the ampulla of the tube and cures in approximately 5 ampulla of the tube and cures in approximately 5 minutes.minutes.

2.Ovabloc 2.Ovabloc intra-tubal deviceintra-tubal device
The silicone contains radio-opaque silver The silicone contains radio-opaque silver powder which enables a radiological check for powder which enables a radiological check for correct placementcorrect placement
Bilateral placement takes around 30 minutesBilateral placement takes around 30 minutes The woman is asked to use contraception for 3 The woman is asked to use contraception for 3
months, at which point a further plain X-ray is months, at which point a further plain X-ray is performed to exclude migration and expulsionperformed to exclude migration and expulsion
Published data reported insertion failure rate at Published data reported insertion failure rate at 17%17%
In women with a successful insertion the plug In women with a successful insertion the plug was expelled in 5% of caseswas expelled in 5% of cases

EssureEssure®® The procedure involves the hysteroscopic The procedure involves the hysteroscopic
application of a micro-insert into the application of a micro-insert into the intramural portion of the fallopion tubeintramural portion of the fallopion tube
Each device consists of a 4 cm long Each device consists of a 4 cm long nickle-titanium alloy outer coil within nickle-titanium alloy outer coil within which lie polyethylene terephthalate(PET) which lie polyethylene terephthalate(PET) fibresfibres
The procedure time from insertion to The procedure time from insertion to removal of the hysteroscope is around 9 removal of the hysteroscope is around 9 minutesminutes
Widely used in Australia, USA and the Widely used in Australia, USA and the EuropeEurope

The PET fibres induce a fibrous reaction in The PET fibres induce a fibrous reaction in the tube whick peaks at around 3 weeks.the tube whick peaks at around 3 weeks.
Patients are instructed to use alternatives Patients are instructed to use alternatives contraception for 3 months after the contraception for 3 months after the procedure.procedure.
A plain X-ray or HSG is done at this point to A plain X-ray or HSG is done at this point to check continued correct placement.check continued correct placement.
99.74% effectiveness with usage over 5 99.74% effectiveness with usage over 5 yearsyears

BARRIER METHODSBARRIER METHODS• Act by blocking the progress of sperm from Act by blocking the progress of sperm from
male partner to female thereby preventing male partner to female thereby preventing fertilizationfertilization
• Effective in preventing pregnancy and offer Effective in preventing pregnancy and offer protection against STIs and HIVprotection against STIs and HIV

Barrier contraception and Barrier contraception and spermicidesspermicides
MaleMale Male condomMale condom
LatexLatex polyurethanepolyurethane
Female Female Female condomFemale condom DiaphragmDiaphragm Cervical capCervical cap spongesponge

1.Male condom1.Male condom
• Estimated 44 million couples use this method
• Japan accounts for more than a quarter
• Despite the massive problem of HIV/AIDS, condom use remains low in Africa, Latin America and Middle East.

Male condomMale condom
• To control HIV/AIDS epidemic, it was calculated, 24 billion condoms need to be used/year, this figure not yet reached 10 billion


Male condomMale condom Failure rate reduce significantly when used correctly by Failure rate reduce significantly when used correctly by
well motivated individualwell motivated individual
Failure rate 2-15/100 women yearsFailure rate 2-15/100 women years
Men complain that they dislike condoms due to lack of Men complain that they dislike condoms due to lack of sensitivity around glans of penissensitivity around glans of penis
Advantages of Polyurethane condoms Advantages of Polyurethane condoms are baggier and less restrictive around the glans of the penis, are baggier and less restrictive around the glans of the penis,
giving more sensationgiving more sensation
Not affected by fat soluble products like baby oils which would Not affected by fat soluble products like baby oils which would cause breakage of latex condomcause breakage of latex condom


2. Female condom2. Female condom FemidomFemidom Made of polyurethaneMade of polyurethane Come in 1 sizeCome in 1 size Lines the vaginaLines the vagina An internal ring in the closed An internal ring in the closed
end of the pouch covers the end of the pouch covers the cervix and an external ring cervix and an external ring remains outside the vagina, remains outside the vagina, partially covering the perineumpartially covering the perineum
Prelubricated with silicone and Prelubricated with silicone and spermicide need not to be spermicide need not to be usedused
Design for single use and is Design for single use and is expensiveexpensive
Failure rate is 5 – 20 per100 Failure rate is 5 – 20 per100 women yearwomen year

3. Diaphragm3. Diaphragm Consist of thin, latex rubber hemisphere, rim Consist of thin, latex rubber hemisphere, rim
reinforced by flexible flat or coiled metal reinforced by flexible flat or coiled metal springspring
Should lie diagonally across cervix reaching Should lie diagonally across cervix reaching post vaginal fornix to behind symphysis pubis post vaginal fornix to behind symphysis pubis covering the cervix.covering the cervix.
Causes of failure areCauses of failure are Poor motivation Poor motivation Incorrect insertionIncorrect insertion Displacement during SIDisplacement during SI
To increase effectiveness use with spermicidal To increase effectiveness use with spermicidal is advised (Smith et al 1995)is advised (Smith et al 1995)
Failure rate Failure rate With spermicidal is 4-8 per 100 women With spermicidal is 4-8 per 100 women
yearsyears Without spermicidal is 10-18 per 100 Without spermicidal is 10-18 per 100
women yearswomen years

4. Cervical cap4. Cervical cap
FEMCAPFEMCAP Need not to be used with Need not to be used with
spermicidespermicide Made of nonallergic silicone Made of nonallergic silicone
rubber.rubber. Shaped like an American sailor’s Shaped like an American sailor’s
hathat Design to conform to the natural Design to conform to the natural
shape of the cervix; the brim shape of the cervix; the brim around the cap helps to create a around the cap helps to create a seal around the vaginal wall, seal around the vaginal wall, stopping the sperm from entering stopping the sperm from entering the cervixthe cervix
3 sizes3 sizes 22mm suitable for nulliparous22mm suitable for nulliparous 26mm suitable for woman who 26mm suitable for woman who
have been pregnant beforehave been pregnant before 30mm suitable for women have 30mm suitable for women have
had a vaginal deliveryhad a vaginal delivery Failure rate is 8 – 20 per 100 Failure rate is 8 – 20 per 100
women yearswomen years

DiaphragmDiaphragm CapCap FemaleFemale
condomcondom
Insertion before Insertion before coitus no longer coitus no longer thanthan
6 hrs6 hrs 6 hrs6 hrs 8 hrs8 hrs
After coitus After coitus should be left in should be left in place forplace for
6 hrs6 hrs 8 hrs8 hrs --
Maximal wear Maximal wear timetime
24 hrs24 hrs 48hrs48hrs 8hrs8hrs

5.Vaginal sponge5.Vaginal sponge Marketed as Marketed as ProtectaidProtectaid Can be inserted into the vagina up to 6 hours before Can be inserted into the vagina up to 6 hours before
sexual intercourse and can be left for a maximum of 12 hsexual intercourse and can be left for a maximum of 12 h Impregnated with a spermicide called F-5gelImpregnated with a spermicide called F-5gel efficacy of 90% with careful and consistent useefficacy of 90% with careful and consistent use Should be inserted 15 min prior to sexual intercourse Should be inserted 15 min prior to sexual intercourse Sexual intercourse may take place more than once Sexual intercourse may take place more than once
without the need to replenish the spermicidewithout the need to replenish the spermicide Should be left in situ for 6 h after the last episode of Should be left in situ for 6 h after the last episode of
sexual intercoursesexual intercourse

6.SPERMICIDES 6.SPERMICIDES A type of contraceptive A type of contraceptive
agent that work by killing agent that work by killing sperm.sperm.
It need to be in place in a It need to be in place in a woman's vagina before woman's vagina before intercourse if they are to intercourse if they are to prevent viable sperm from prevent viable sperm from reaching her uterus. reaching her uterus.
It come in a wide variety It come in a wide variety of forms, including of forms, including pessaries, creams, foams.pessaries, creams, foams.
The active ingredient in all The active ingredient in all spermicides is spermicides is Nonoxynol-Nonoxynol-9.9.

Traditional MethodsTraditional Methods
1.1. Periodic abstinence Periodic abstinence
2.2. Coitus interruptusCoitus interruptus
3.3. Harmonal monitoring Harmonal monitoring
4.4. Cervical mucus method (billing Cervical mucus method (billing method)method)
5.5. Sympto-thermal method (basal body Sympto-thermal method (basal body temp)temp)

1. PERIODIC A1. PERIODIC ABSTINENCEBSTINENCE Also known as Also known as ovulation method, Rhythm method or ovulation method, Rhythm method or
Calender method or Fertility awareness methodCalender method or Fertility awareness method
Based on the assumption that menstrual cycle relatively Based on the assumption that menstrual cycle relatively constant and the viability of sperm in the female constant and the viability of sperm in the female reproductive tract (2-7 days) and the life span of ovum(1-reproductive tract (2-7 days) and the life span of ovum(1-3 days)3 days)
Pregnancy rate of 40 per 100 women yearsPregnancy rate of 40 per 100 women years General rule General rule
To estimate the beginning of fertile period by substracting 18 To estimate the beginning of fertile period by substracting 18 days from the length of the shortest cycledays from the length of the shortest cycle
To estimate the end of fertile period by substracting 11 days from To estimate the end of fertile period by substracting 11 days from the longest cyclethe longest cycle
Example is if cycles of 28-32 days, periodic abstinence should Example is if cycles of 28-32 days, periodic abstinence should be from day 10 to day 21be from day 10 to day 21

2. Coitus interruptus2. Coitus interruptus
Means withdrawal of the penis from Means withdrawal of the penis from vagina just before ejaculation to vagina just before ejaculation to prevent pregnancy.prevent pregnancy.
But it is not reliable as pre-ejaculatory But it is not reliable as pre-ejaculatory secretions may contain millions of secretions may contain millions of sperm.sperm.

3. Hormone monitoring 3. Hormone monitoring PERSONAPERSONA
A hand held monitor with disposable urine dip stickA hand held monitor with disposable urine dip stick Measures levels of LH and oestrogen in early morning Measures levels of LH and oestrogen in early morning
urineurine The ratio between the 2 hormones is used to defined the The ratio between the 2 hormones is used to defined the
start and the end of fertile phasestart and the end of fertile phase A red light is displayed on days when intercourse should A red light is displayed on days when intercourse should
be avoidedbe avoided Need to be programmed for 3 months ( test urine for 16 Need to be programmed for 3 months ( test urine for 16
days in the first month and 8 days in subsequent days in the first month and 8 days in subsequent months) before device can be relied uponmonths) before device can be relied upon
Failure rate Failure rate ~6/100 woman years with perfect use. ~6/100 woman years with perfect use.

3. Hormone monitoring 3. Hormone monitoring PERSONAPERSONA
Not suitables for:Not suitables for: Cycle length <23 days or > 35 daysCycle length <23 days or > 35 days PCOSPCOS BreastfeedingBreastfeeding Menopausal symptomsMenopausal symptoms Women taking hormonal medicationWomen taking hormonal medication

4. Cervical mucus method4. Cervical mucus method Also known as Also known as Billing methodBilling method Requires sensing and observing the cervical mucus Requires sensing and observing the cervical mucus
changes over timechanges over time Oestrogen induced changes at mid cycle: Increase in Oestrogen induced changes at mid cycle: Increase in
amount of clear, thin and stringy mucusamount of clear, thin and stringy mucus With ovulation and in the presence of progesterone, With ovulation and in the presence of progesterone,
mucus becomes opaque, sticky and much less stretchy mucus becomes opaque, sticky and much less stretchy or disappear all togetheror disappear all together
The of ovulation correspond closely to the day of peak The of ovulation correspond closely to the day of peak mucusmucus
Intercourse is permitted on the Intercourse is permitted on the 44thth day after the last day day after the last day of sticky, wet mucusof sticky, wet mucus

5.Sympto-thermal method5.Sympto-thermal method Basal body temperatureBasal body temperature
It is recorded before getting out of bed (early in the morning)It is recorded before getting out of bed (early in the morning) Progesterone secretion is associated with a rise in basal body Progesterone secretion is associated with a rise in basal body
temperature of about 0.5temperature of about 0.5°C°C Prior to ovulation the temp is usually below normal body Prior to ovulation the temp is usually below normal body
temperaturetemperature If practice alone, it requires abstinence until the night of 3If practice alone, it requires abstinence until the night of 3 rdrd day day
of a shift in temperatureof a shift in temperature
Combining the basal body temperature with the mucus Combining the basal body temperature with the mucus method method
abstinence begins when the mucus becomes sticky and moist.abstinence begins when the mucus becomes sticky and moist. Intercourse resumes the night of either the 3Intercourse resumes the night of either the 3rdrd day of a temp shift day of a temp shift
or the 4or the 4thth day after the last day of sticky, wet mucus which ever is day after the last day of sticky, wet mucus which ever is later later

CONTRACEPTIVE CONTRACEPTIVE VACCINESVACCINES
Research on vaccines has focused on three Research on vaccines has focused on three targets: targets:
1.1. human chorionic gonadotropin (hCG), human chorionic gonadotropin (hCG),
2.2. the sperm-binding glycoprotein in the zona the sperm-binding glycoprotein in the zona pellucida of the egg, and pellucida of the egg, and
3.3. sperm. sperm. Research on vaccines has been ongoing for Research on vaccines has been ongoing for
decades; many problems must be overcome, decades; many problems must be overcome, including inducing autoantibodies. including inducing autoantibodies.

Current status of FRV (fertility Current status of FRV (fertility regulating vaccinesregulating vaccines ) )
developmentdevelopment
Anti-sperm vaccinesAnti-sperm vaccines Sperm enzymes.Sperm enzymes. Sperm membrane antigens.Sperm membrane antigens. Anti-ovum vaccinesAnti-ovum vaccines Anti-conceptus vaccinesAnti-conceptus vaccines Structural placental antigens.Structural placental antigens. Hormonal placental antigens.Hormonal placental antigens.

Mechanism of action, Mechanism of action, reversibility and choicereversibility and choice
FRVs could act by preventing sperm FRVs could act by preventing sperm production, by interfering with ovulation, by production, by interfering with ovulation, by inhibiting fertilization, or by preventing inhibiting fertilization, or by preventing implantation of the blastocyst. It is implantation of the blastocyst. It is important that studies are carried out to important that studies are carried out to clearly determine how each FRV works. clearly determine how each FRV works. By understanding their mechanisms of By understanding their mechanisms of action, more efficient and predictable action, more efficient and predictable FRVs can be prepared and rational FRVs can be prepared and rational intervention strategies can be developed intervention strategies can be developed to reverse the effects of the FRVs on to reverse the effects of the FRVs on demand. demand.

Mechanism of action, Mechanism of action, reversibility and choicereversibility and choice
In addition, the user would be able to be In addition, the user would be able to be fully informed of the known or suspected fully informed of the known or suspected mechanisms of action of FRVs so that he mechanisms of action of FRVs so that he or she can choose a FRV that is or she can choose a FRV that is compatible with their personal beliefs and compatible with their personal beliefs and needs.needs.

Future prospects and needsFuture prospects and needs
Vaccine optimizationVaccine optimization Long-term safetyLong-term safety

Contraceptive Methods and Cancer RiskContraceptive Methods and Cancer Risk
MethodBreast Cancer
Cervical Cancer
Endometrial Cancer
Ovarian Cancer
Oral contraceptive ?
Vaginal ring NA NA NA NA
Contraceptive patch NA NA NA NA
Condom — — —
Diaphragm — — —
Injectable contraceptive
— — —
Intrauterine device — —
Abstinence — — —
Fertility awareness — — — —
Sterilization —
NA= research has not been conducted on the cancer–related risk of this method

Failures of contraceptionFailures of contraceptionMETHOD OF CONTRACEPTION FAILURE RATE PER 100
WOMAN YEARS
Combined oral contraceptive pills 0.1-1
Progestogen-only pills 1-3
Depo-Provera® 0.1-2
Implanon® 0.1
Copper IUD 1-2
Mirena® 0.5
Male condom 2-5
Diaphragm 1-15
Natural family planning 2-3
Vasectomy 0.02
Female sterilization 0.13

Conclusion Conclusion • Any method of family planning is
better than no method, though some methods are better than others.

Thank you for your Thank you for your attentionattention