Managed Care: Overview of Behavioral Health Services ... · Introduction & Housekeeping Reminders...
Transcript of Managed Care: Overview of Behavioral Health Services ... · Introduction & Housekeeping Reminders...

Managed Care: Overview of Behavioral Health Services Transitioning to Medicaid Managed Care on July 1, 2019
June 7, 2019

Introduction & HousekeepingReminders
‣ Slides and recording will be posted at MCTAC.org
‣ Information and timelines are current as of the date of the presentation
‣ This presentation is not an official document. For full details please refer
to the provider and billing manuals

Children’s Medicaid Overview of Key Components

Key Components of Children’s Medicaid System Transformation‣ Six New State Plan Services for Children (Three services began in January 2019)
‣ Transition to Health Home Care Management (Occurred April 1, 2019)
◦ Current 1915(c) Waiver Providers Transition to Health Home
◦ Care Management provided under 1915(c) Transition to Health Home Care Management
‣ Transition of six 1915(c) waivers to 1915c Waiver authority under one consolidated
Children’s Waiver (Occurred April 1, 2019):
◦ Office of Mental Health (OMH) Serious Emotional Disturbance (SED) Waiver
◦ Department of Health (DOH) Care at Home (CAH) I/II waiver
◦ Office for People with Developmental Disabilities (OPWDD) Care at Home Waiver
◦ Office of Children and Families (OCFS) Bridges to Health (B2H) SED, Developmental
Disability (DD) and Medically Fragile Waivers

Key Components of Children’s Medicaid System Transformation
‣ Alignment of 1915(c) HCBS under one array of Home and Community
Based Services (HCBS) authorized under 1115 Demonstration Waiver
(Planned for October 1, 2019; Pending CMS Approval)
◦ Remove the Managed Care exemption for children now in six 1915(c) waivers
‣ Lifting the exemption of children in foster care with Voluntary Foster Care
Agency (VFCA) to Managed Care (Planned for October 1, 2019; Pending
CMS Approval)
‣ Transition of certain carved out Behavioral Health services into Managed
Care benefit package (July 1, 2019)

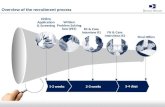
Timeline Update Children’s Transition Timeline Scheduled Date
• Implement three of the six new Children and Family Treatment and Support Services (CFTSS) (Other Licensed
Practitioner, Psychosocial Rehabilitation, Community Psychiatric Treatment and Supports) in Managed Care and Fee-
For-Service
January 1, 2019
COMPLETED
• Waiver agencies must obtain the necessary LPHA recommendation for CFTSS that crosswalk from historical waiver
services and revise service names in Plan of Care for transitioning waiver children. This is the last billable date of
waiver services that crosswalk to CPST and/or PSR.
January 31, 2019
COMPLETED
• Transition from Waiver Care Coordination to Health Home Care Management January 1- March 31, 2019
COMPLETED
• 1915(c) Children’s Consolidated Waiver is effective and former 1915c Waivers no longer active April 1, 2019
COMPLETED
• Implement Family Peer Support Services as State Plan Service in managed care and fee-for-service
• BH services already in managed care for adults 21 and older are available in managed care for eligible individuals under
21 (e.g. PROS, ACT, etc.)
• OMH licensed SED designated clinics serving children with SED diagnoses are carved-in to managed care
• SSI children begin receiving State Plan behavioral health services in managed care
• Three-year phase in of Level of Care (LOC) expansion begins
July 1, 2019
July 1, 2019
July 1, 2019
July 1, 2019
July 1, 2019
• 1915(c) Children’s Consolidated Waiver Services carved-in to managed care• Children enrolled in the Children’s 1915(c) Waiver are mandatorily enrolled in managed care• Voluntary Foster Care Agency Article 29-I per diem and services carved-in to managed care• Children residing in a Voluntary Foster Care Agency are mandatorily enrolled in managed care
• 29-I Licensure becomes effective for Voluntary Foster Care Agencies
October 1, 2019
October 1, 2019
October 1, 2019
October 1, 2019
October 1, 2019
• Implement Youth Peer Support and Training and Crisis Intervention as State Plan services in managed care and fee-for-
service
January 1, 2020
Managed care services and enrollment are pending CMS approval

Transition of Existing State Plan Behavioral Health Services to Managed Care for Children

Services Carved-In to Medicaid Managed Care on July 1, 2019‣ Behavioral health services already in managed care for adults 21 and
older will be carved in for eligible individuals under 21
• Assertive Community Treatment (ACT)
• Comprehensive Psychiatric Emergency Program (CPEP) (including Extended Observation Bed)
• Personalized Recovery Oriented Services (PROS)
• Continuing Day Treatment (CDT)
• OASAS Outpatient and Opioid Treatment Program (OTP) services (hospital based)
• OASAS Outpatient Rehabilitation Services (hospital based)
• Partial Hospitalization

Services Carved-In to Medicaid Managed Care on July 1, 2019
‣Behavioral health State Plan services for children who have federal Social Security Insurance disability status or have been determined Social Security Insurance-Related by New York State (SSI children)
‣OMH specialty clinics designated for MMC enrolled children who have met criteria for a serious emotional disturbance (SED)
Please note: Medicaid/Medicare children (dually eligible) are not being carved in during this transition.

What Does This Mean?‣ Effective July 1, 2019, these services for eligible children under age 21
will be part of the MMCP benefit package and claiming will follow billing
procedures defined in New York State Health and Recovery Plan (HARP) /
Mainstream Behavioral Health Billing and Coding Manual:
https://www.omh.ny.gov/omhweb/bho/harp-mainstream-billing-manual.pdf
‣ Providers must ensure necessary authorization is in place for services
provided after July 1, 2019.
• Providers should begin checking managed care enrollment for all individuals
served who are under 21, and should contact those individuals’ MMCPs to
ensure authorizations are place.

Continuity of Care‣ Children and youth under 21 can continue to see their same providers for up to
24 months for a continuous episode of care, regardless of whether the provider
is in the child’s Plan’s network
‣ For the services covered in this presentation, Plans should ensure
authorizations are provided for existing providers/service level for up to 60 days
from the carve in date to ensure there are no gaps in coverage or access to
services, until the provider and the Plan have established an arrangement for
continued services
• This means that providers must work with Plans prior to 7/1/19 but no later than 60
days after 7/1/19 to ensure authorizations are in place for continued services
• This requirement does NOT prohibit Plans from conducting utilization management
on these services

Assertive Community Treatment (ACT)

Referrals to ACT‣ Level Of Service Determination (LOSD)
• NYC & ROS (see ACT Utilization Management Guidance)
• Referring provider contacts MCO
• MCO UM staff review to ensure individual meets ACT level of care admission
criteria
• MCO notifies of LOSD within 24 hours

ACT Authorization and Concurrent Review‣ Authorization - the accepting ACT team will contact the MCO within seven
(7) days prior to the date of admission to obtain the prior authorization
and determine a timeframe for concurrent review
‣ Concurrent Reviews - recommend aligning with OMH required concurrent
review with assessment and service plan dates (6-months)
• Most individuals who are appropriate for ACT level of care will require services
for a period of at least 2-3 years and many will require an even longer duration
• It is expected that the intervals for UM should reflect the longer-term nature of
the service.

Billing for ACT ‣ACT claims are submitted using the last day of the month, in
which the services were rendered, as the date of service (e.g.
Services provided in July will submit a claim with 7/31/19 as
the service date)
‣ACT Service Authorization/Reimbursement is in “Units” only◦ Unit = 1 month of service
‣ Three Rate Codes◦ 4508 Full Payment
◦ 4509 Partial Payment
◦ 4511 Hospital

Overview of the ACT Model: Billing
Billing:
‣ Full Rate – must provide a minimum of 6 visits per month,
three 3 of which may be collateral (family, employment,
landlord, etc.)
‣Partial Rate – must provide a minimum of two 2 visits per
month, but fewer than 6

Overview of the ACT Model: Billing
‣ Inpatient Rate - clients who are admitted for treatment to an inpatient facility and
are anticipated to be discharged within 180 days of admission; a minimum of 2
inpatient face-to-face contacts are provided in a month
• In the month of admission and/or month of discharge full payment rate
reimbursement is permitted for any month in which four or more community-based
contacts combined with inpatient face-to-face contacts equals six or more total
contacts in the month.
• In the month of admission and/or month of discharge stepdown/partial payment rate
reimbursement is permitted when a minimum of two community-based contacts are
provided in a month, or when a minimum of one community contact, combined with a
minimum of one inpatient contact, is provided.

Overview of the ACT Model: Billing
‣ 3 clinic pre-admission visits are allowed while enrolled in ACT; reimbursement for clinic or continuing day treatment services provided to a client, other than for pre-admission visits, are deducted from the amount paid to the provider of ACT services
‣ An individual may be both an active ACT client and enrolled in a personalized recovery oriented services (PROS) program for no more than three months within any 12-month period
‣ Reimbursement for services provided to clients who are receiving both ACT and PROS services will be limited to the partial payment rate for ACT

Transition to Managed Care for ACT Recipients 18-20
‣ Individuals 18-20 admitted to ACT as of July 1st 2019
• Authorization will need to be obtained prior to the July transition to
managed care.
• Providers should begin communicating with Plans now.
• Admission includes any individual who the team has a referral for
and has met at least once; has a completed immediate needs
assessment; OR has a completed Initial Comprehensive
Assessment/Comprehensive Service Plan

Personalized Recovery Oriented Services(PROS)

Referrals and Admission to PROS
‣A referral to PROS may be made by a practitioner, MCO, or self-
referral
‣ There are three phases of PROS services:
• Pre-Admission
• Admission
• Active Rehabilitation

Prior Authorization and phases of PROS
‣Pre-admission begins with an initial visit and ends when an
Initial Service Recommendation(ISR) is sent to the MCO for
prior authorization
‣Admission begins when the ISR is approved, the PROS then
has 60 days to develop an Individualized Recovery Plan.
‣Active Rehabilitation begins when Individualized Recovery
Plan is approved by the MCO

Utilization Management: PROS
‣Concurrent review and authorizations should occur at 3-month
intervals for Intensive Rehabilitation(IR) and Ongoing
Rehabilitation Services(ORS)
‣Community Rehabilitation Services(CRS) and Clinic Treatment
require 6-month review and authorization

Continuing Stay Criteria: PROS
‣ The member has an active recovery goal and shows progress
toward achieving it; or
‣ The member has met and is sustaining a recovery goal, but
would like to pursue a new goal; or
‣ The member requires a PROS level of care in order to maintain
psychiatric stability and there is not a less restrictive level of
care that is appropriate; or
‣Without PROS services the individual would require a higher
level of care

Billing: PROS
‣PROS claims are submitted using the last day of the month, in
which the services were rendered.
‣Base Rate Tier: The monthly payment for each PROS
participant, determined by the total number of PROS units that
person accumulated during the month.
‣Add-on Component: An additional payment for qualifying
Intensive Rehabilitation(IR), Ongoing Rehabilitation
Services(ORS), and Clinic Treatment (CT) services provided
during the month.

Continuing Day
Treatment (CDT)

Billing: CDT
‣ CDT Services are billed daily
3 Rate Tiers
‣ 1-40 hours
‣ 41-64
‣ 65+ hours
Visit Types
‣ Full Day- 4 hours minimum
‣ Half Day- 2 hours minimum
‣ Tiers determined by totaling the number of full day and half day regular visits, based on
their hour equivalent. As hours accumulate throughout the month, provider will move
from one tier to another to bill.

Billing: CDT
‣Claims for collateral, group collateral, preadmission and crisis
visits are billed separately from the CDT regular visits
‣ The reimbursement is the equivalent to the half day tier 1
amount regardless of the cumulative total of hours for CDT
regular visits in that month
‣Collateral group, preadmission, and crisis visits are excluded
from the calculation of the cumulative total hours in the
program for a recipient

Partial
Hospitalization

Billing for Partial Hospitalization‣Claims are submitted daily
‣ The applicable rate code/procedure code/modifier codes(s)
combination dependent on the number of hours of service a
day
‣Regular Rate/Crisis Rate reimbursement provided for service
duration of at least four hours and not more than seven hours
per recipient, per day

Billing for Partial Hospitalization‣Collateral- Clinical support services of at least 30 minutes in
duration but no more than 2 hours face to face interaction
between one or more collaterals and one therapist with or
without recipient
‣Group Collateral-Clinical support services of at least 60 min in
duration by not more than two hours provided to more than
one recipient and/or his/her collaterals. Cannot include more
than 12 collaterals in a face to face interaction with therapist
‣Pre-Admission-visits of 1-3 hours

Billing for Partial HospitalizationPre-admission
‣ 1-3 hours billed using crisis visit rate codes
‣ 4+ billed using regular rate codes
‣UA modifier required on all partial hospitalization pre-
admission claims.

Authorization & Concurrent Review: Partial & CDT
‣Partial Hospitalization and CDT require prior authorization and
concurrent review

OMH Clinics

Billing: OMH Clinics Serving Individuals Under 21
‣ OMH clinics serving individuals under 21 who are enrolled in Medicaid
Managed Care will bill the Medicaid Managed Care Plan for these children.
This includes:
• Children with SSI, and
• Children with SED diagnoses
‣Billing will utilize the APG rate methodology and will include
• Rate code
• Procedure code
• Modifier code

Billing: OMH SED Clinics
‣As of July 1, 2019, Plans will cover OMH clinic services for all
enrollees, including children with SED diagnoses and SSI
children
‣ This means that SED clinics will no longer be able to bill FFS
for children with SED diagnoses.
‣Billing will utilize the APG rate methodology and will include
• Rate code
• Procedure code
• Modifier code

Authorization and Concurrent Review: OMH Clinics‣Plans must pay for at least 30 mental health clinic visits per
calendar year without requiring authorization. The 30-visit count should not include: prior fee-for-service visits or visits paid by another plan; off-site clinic services; psychiatric assessments; medication management visits; or crisis visits to the clinics
‣Multiple services received on the same day count as a single visit (and must be delivered consistent with OMH clinic regulations – Part 599.) NYS allows, but does not mandate, plans to require concurrent review requests for clinic services following the 30th visit paid by the Plan in a calendar year

Utilization Threshold: OMH Clinics
‣OMH will calculate “countable service days” claimed to
Medicaid by a clinic organization for an individual. When an
individual receives services in excess of the utilization
threshold, payment reductions will occur

Utilization Threshold: OMH Clinics
‣ For individuals whose age on April 1 of each state fiscal year was LESS than 21 years old, Medicaid payments for their “countable” services will be reduced by 50% beginning with their 51st service day during the fiscal year. This count will reset to zero at the beginning of each SFY thereafter (April 1st)
‣ For individuals whose age on April 1of each state fiscal year was equal to or greater than 21 years old, Medicaid payments for their countable clinic services will be reduced by 25% for their 31st through 50th service days during the state fiscal year. Payments for clinic services will be reduced by 50% beginning on their 51st service day during the fiscal year. This count will reset to zero at the beginning of each SFY thereafter.

OASAS Services

Prior Authorization and Concurrent Review
For the services discussed in this webinar the same standards for use of
the LOCADTR, prior authorization and Concurrent Review that you use for
the over 21 population that you serve are true for the under 21 population
beginning July 1, 2019.

OASAS Services in Medicaid Managed Care
‣Part 818 Chemical Dependence Inpatient Rehabilitation
Services
• Covered for non-SSI, all ages prior to 10/1/15
• ADDED SSI Adults over 21 as part of Adult BH Transition on
10/1/15

OASAS Services in Medicaid Managed Care
‣Part 820 Residential Services
• Stabilization
• Rehabilitation
‣ Free-Standing Part 820
• 1115 Demonstration Service added for ALL AGES, SSI/Non-SSI, as part of
Adult BH carve in
• First providers certified August 2016

OASAS Services in Medicaid Managed Care‣Part 822 Chemical Dependence Outpatient Services• Outpatient Clinic (CD-OP)
• Outpatient Rehabilitation
• Opioid Treatment Program (OTP)
‣Hospital Based Part 822• State Plan service added for Adults over 21, SSI/Non-SSI, as part of Adult BH carve
in
‣ Free-Standing Part 822• 1115 Demonstration Service Added for ALL AGES, SSI/Non-SSI, as part of Adult BH
carve in

OASAS Services Transitioning to Managed Care 7/1/19‣ Part 818 Chemical Dependence Inpatient Rehabilitative Services
• Chemical Dependence Inpatient Rehabilitative Services◦ Article 28/32- Under 21 SSI children to be carved in 7/1/19
‣ Part 822 Chemical Dependence Outpatient (CD-OP) Clinic; Rehabilitation and Opioid Treatment Programs (OTP)
• Outpatient Clinic ◦ Article 28/32-Under 21 (SSI & Non SSI)
• Outpatient Rehabilitation◦ Article 28/32-Under 21 (SSI & Non SSI)
• Opioid Treatment Program (OTP)◦ Article 28/32-Under 21 (SSI & Non SSI)

OASAS Services NOT Transitioning‣Part 817 Residential Rehabilitation Services for youth
• Article 32 Only is not currently included in MMC benefit and will remain Fee
For Service
‣Part 820 Residential Services
• Reintegration (NOT IN PLAN)

Children with Social Security Insurance

Children with Social Security Insurance
‣Enrolled children under the age of 21 who have federal Social
Security Insurance Disability status or have been determined
Social Security Insurance Related by NYS will now begin
receiving behavioral health services through Medicaid
Managed Care

Claims

Claims Submission
‣MMCPs and providers must adhere to the rules in the billing
and coding manual
‣MMCP must support both paper and electronic submission of
claims
‣MMCP must offer its providers an electronic payment option
including a web-based claim submission system

Claims Submission‣ All Electronic claims will be submitted using the 837i (institutional) claim form
UB-04 should be utilized when submitting paper claims
‣ Every electronic claim submitted will require at least the following:
• Use of the 837i claim form;
• Medicaid fee-for-service rate code;
• Valid procedure code(s);
• Procedure code modifiers (as needed); and
• Units of service.
https://billing.ctacny.org/
‣ Insurance Law § 3224-a requires insurers and health maintenance organizations to pay undisputed claims within 45 days after the insurer receives the claim, or within 30 days if the claim is transmitted electronically

Claims Submission
‣Providers are expected to claims test with MMCPs prior to the
service implementation date. MMCPs were instructed to keep
their claims testing systems open throughout the transition.

Resources

State Guidance‣ Announcing the Implementation of Benefit Changes and Technical
Assistance Memo
• Memo for OMH Mental Health Providers
‣ OMH Specialty Designated Clinic services for children with SED carving
into Medicaid Managed Care on July 1, 2019

https://www.health.ny.gov/health_care/medicaid/redesign/behavioral_health/children/docs/2017-10_utilize_mgmt_guide.pdf
Utilization Management Guidelines for State Plan Services

Allowable Billing Combinations of Children’s Behavioral Health, Children and Family Treatment
Support Services and HCBS
HCBS/State
Plan Services
OMH
Clinic
OASAS
Clinic
OASAS
Opioid
Treatment
Program
OMH
ACT*
OMH
PROS*
OMH
CDT*
OMH
Partial
OASAS
Outpatient
Rehab
OLP/
CPST
PSR FPSS YPST
Day Habilitation Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes Yes
Community
Habilitation
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Caregiver &
Family Support
Services
Yes Yes Yes No No Yes Yes Yes Yes Yes Yes Yes
Respite Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Prevocational
services
Yes Yes Yes No No Yes Yes Yes Yes Yes Yes Yes
Supported
Employment
Yes Yes Yes No No Yes Yes Yes Yes Yes Yes Yes
Community Self
Advocacy
Training &
Supports
Yes Yes Yes No No Yes Yes Yes Yes Yes Yes Yes
*These services available to youth age 18 and older
**OMH guidance is forthcoming to avoid duplication in services.

Allowable Billing Combinations of Children’s Behavioral Health, Children and Family Treatment
Support Services and HCBS
HCBS/State
Plan Services
OMH
Clinic
OASAS
Clinic
OASAS
Opioid
Treatment
Program
OMH
ACT*
OMH
PROS*
OMH
CDT*
OMH
Partial
OASAS
Outpatient
Rehab
OLP/
CPST
PSR FPSS YPST
Other Licensed
Practitioner
(OLP)
Yes** No No Yes No No Yes No Yes Yes Yes Yes
Community
Psychiatric
Supports &
Treatment
(CPST)
Yes Yes Yes No No No Yes Yes _ Yes Yes Yes
Psychosocial
Rehabilitation
(PSR)
Yes Yes Yes No No No Yes Yes Yes _ Yes Yes
Youth Peer
Support &
Training
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes _
Family Peer
Support
Yes Yes Yes No Yes Yes Yes Yes Yes Yes _ Yes
Crisis
Intervention
Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes Yes
*These services available to youth age 18 and older
**OMH guidance is forthcoming to avoid duplication in services.

Allowable Billing Combinations of Children’s Behavioral Health, Children and Family Treatment
Support Services and HCBS
HCBS/State
Plan Services
OMH
Clinic
OASAS
Clinic
OASAS
Opioid
Treatment
Program
OMH
ACT*
OMH
PROS*
OMH
CDT*
OMH
Partial
OASAS
Outpatient
Rehab
OLP/
CPST
PSR FPSS YPST
Palliative Care
Pain &
Symptom
Management
Yes Yes Yes No No Yes Yes Yes Yes Yes Yes Yes
Palliative Care
Bereavement
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Palliative Care
Massage
Therapy
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Palliative Care
Expressive
Therapy
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Accessibility
Modifications
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
Adaptive and
Assistive
Equipment
Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes
*These services available to youth age 18 and older
**OMH guidance is forthcoming to avoid duplication in services.

Questions
Please send questions to: [email protected]
Logistical questions usually receive a response in 1 business day or less.
Longer & more complicated questions
can take longer.
We appreciate your interest and patience! Visit www.ctacny.org to view past
trainings, sign-up for updates and event announcements, and access resources