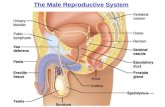
The Male Reproductive System Male Reproductive System Epididymis.
Lesson 1: Reproductive Systems. Male reproductive system.
-
Upload
sophia-hopkins -
Category
Documents
-
view
232 -
download
3
Transcript of Lesson 1: Reproductive Systems. Male reproductive system.

Lesson 1: Reproductive Systems

Male reproductive system


Further functions
Urethra: tube from ejaculatory duct through penis that carries semen and urine (but not at the same time)
Prostate: also neutralizes acidity of vagina Bulbourethral gland: also “cleans out”
urethra, releases fluid before ejaculation, contributes to unplanned pregnancies
Sperm make only a small part of semen; 90+% of volume from seminal vesicles


1.Mitosis makes enough cells from spermatogonium to keep the same number and produce sperm2.Primary spermatocytes grow3.Cells divide through the two divisions of meiosis (secondary spermatocytes)4.Cells (spermatids) differentiate as they developSertoli cells support developing sperm.
(germinal epithelium)

(spermatozoa)
(produce testosterone)
(nurse cell)

Structure of a Mature Sperm (50 um)
Acrosome: chemicals to enter egg
Nucleus: haploid Midpiece: “motor”, many
mitochondria Flagellum: protein, 9+2
microtubule pattern Flagellum ~40 um

Hormonal Control of Spermatogenesis
Luteinizing hormone (LH): increases testosterone levels
Follicle Stimulating hormone (FSH): controls meiosis / number of sperm
Testosterone: helps sperm production and development
* FSH and LH named for role in females (menstrual cycle)

Secondary sexual characteristics
Related to sexual development, but not necessary for reproduction
Development occurs during puberty

Roles of Testosterone in Males Gonads become either
testes or ovaries (ovary is default)
Gene on Y chromosome (when fetus is in week 7) shifts gonads to testes
Testes release testosterone Testosterone leads to
development of secondary sexual characteristics at puberty
Production of sperm Maintenance of sex drive

Timing and Number of Sperm Production
Begins at puberty, continues until death Continually produced, millions each day Complete process takes several months One diploid cell produces 4 haploid sperm
with equal amounts of cytoplasm May be released voluntarily

1
2
3
4
6
7
89
10
11
5
1. Ureter2. Urinary
bladder3. Seminal
vesicle4. Prostate5. Bulbourethr
al gland6. Vas
deferens (ductus deferens)
7. Epididymis8. Scrotum9. Testes10.Urethra11.Penis



(holds fetus in uterus)
(site of fertilization)
(for urination)


All follicles present at birth (one primary oocyte each)
Follicle stimulating hormone (FSH) causes some follicles to develop; usually one per month will mature
The follicle stays in the same place in the ovary
The mature, large, fluid- filled follicle seen before ovulation is called a Graafian follicle.
After ovulation, the follicle becomes the corpus luteum
Mature (Graafian)
follicle

unequal division of cytoplasm

A secondary oocyte is released to the fallopian tubes (oviduct) in ovulation
When triggered by the arrival of a sperm, meiosis will finally be completed, releasing the second polar body.
(also called yolk, contains lipid droplets)
(and centrioles)for
first
Haploid DNA in metaphase II

Estrogen and progesterone are major female hormones. They cause Pre-natal (embryonic/fetal) development of
female sex organs Development of secondary sexual
characteristic during puberty

Timing and Number of Ova Production
All eggs begin meiosis during fetal development
At puberty, ~1 egg / month continues meiosis, release time hormonally controlled (menstrual cycle)
Meiosis only completed if sperm enters egg
Unequal division of cytoplasm; one diploid cell produces one ovum and 2-3 polar bodies
Compare oogenesis and spermatogenesis.

Spermatogenesis v. Oogenesis In testes
Millions produced continually (after puberty); released as needed / voluntary control
Four motile sperm produced per meiosis (equal cytoplasm)
Meiosis begins (primarily) in puberty
Sperm made indefinitely Requires testosterone
and Sertoli (nurse) cells
In ovaries One oocyte released per
month long cycle, hormonal control
One egg per meiosis (+2-3 small polar bodies) with unequal division of cytoplasm
Meiosis begins during fetal stage, none in childhood, completed after puberty (when sperm present)
Viable egg supply gone by menopauseSimilarities include: mitosis in germ cells, cell growth before meiosis,
two divisions of meiosis, haploid nuclei, need for LH and FSH, etc.

1. Uterus2. Fallopian
tube (oviduct)
3. (Fimbriae)4. Ligament5. Cervix6. Vagina7. Endometriu
m8. Ovary9. Urinary
bladder10.Urethra11.Pelvic bone12.Clitoris13.Labia14.Urethral
orifice15.Intestine16.Anus