IMCI Chart Booklet Trytry
-
Upload
lighto-ryusaki -
Category
Documents
-
view
240 -
download
1
Transcript of IMCI Chart Booklet Trytry
-
8/12/2019 IMCI Chart Booklet Trytry
1/80
-
8/12/2019 IMCI Chart Booklet Trytry
2/80
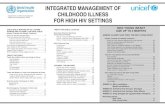
AGE ASSESS, CLASSIF
Assess, lassi!" aCheck for PossiThen ask: DoesThen Check forThen check feedThen Check forThen Check the
'ssess (ther Pr 'ssess the moth
Treat the %o&ng #n(ral 'ntibiotic))))Intramuscular 'To Treat for Diar Immunise +veryTreat Local InfeCorrect PositioniCommon breastCorrect #re#arat,o to feed a b,ome Care for
Gi'e Follo()&* aLocal Bacterial IThrush)))))))))))Feeding ProbleLo !eight))))))))
-E O-.#NG FO-
S# K %
Division of Child ,ealth
and Develo#ment .C,D/S# K H#/.
AGE 2 MONTHS UP TO 0 %EA-S
ASSESS AND CLASSIFY THE SICK CHILDTREAT THE CHILD, +ontin&edAssess, lassi!" and #denti!" Treat$ent
Check for 0eneral Danger "igns ))))))))))))))))))))))))))))))))))))) 1Gi'e E tra Fl&id !or .iarrhoeaThen 'sk 'bout 2ain "ym#toms:and ontin&e FeedingDoes the child have cough or difficult breathing? )))))))))))))))) 1
Plan ': Treat for Diarrhoea at ,ome)))))))))))))))))))))))))34Does the child have diarrhoea? )))))))))))))))))))))))))))))))))))))))) 5Plan B: Treat for "ome Dehydration ith ($")))))))))34Does the child have fever? )))))))))))))))))))))))))))))))))))))))))))))) 6Plan C: Treat for "evere Dehydration 7uickly))))))))))38Classify malaria ))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))6
Does the child have an ear #roblem?)))))))))))))))))))))))))))))))) 4 Gi'e Follo()&* areThen Check for 2alnutrition and 'naemia ))))))))))))))))))))))) 8
Pneumonia))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))39Then Check the Child&s Immuni ation "tatus))))))))))))))))))) 8!hee e .first e#isode/))))))))))))))))))))))))))))))))))))))))))))))39 'ssess (ther Problems)))))))))))))))))))))))))))))))))))))))))))))))))))) 8Diarrhoea still #resent after 4 days -------)39Check for sym#tomatic ,I; infection ))))))))))))))))))))))))))))))) 9Dysentery))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))))39Persistent Diarrhoea)))))))))))))))))))))))))))))))))))))))))))))))))3E
% % %
0ive salbutamol via s#acer for 4 days.#) >/ 0ive oral #rednisone for threedays .#) >/)#! there is an" se'ere +lassi!i+ation, gi'e !irstdose o! *rednisone and sal3&ta$ol 3e!ore
'll other children ithhee e WHEE>E
5F#-STEP#SO.E8
% 0ive salbutamol via s#acer for 4 days . #) >/% #! an" se'ere +lassi!i+ation gi'e sal3&ta$ol 3e!ore re!erral% Follo @u# in 4 days if still hee ing% 'dvise the mother to return if hee e recurs
-ESP#-ATO-% -ATE#! the +hild is Fast 3reathing is1 months u# to 31 months: 0? or more breaths #erminute 31 months u# to 4 years =? or more breaths #erminute
Danger signs Cough 2
'ssess and classifyG I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
5/80
.oes the +hild ha'e diarrhoea4
lassi!" all +hildren (ith
T o of the follo ing signs:
Lethargic or unconscious "unken eyes ot able to drink or
drinking #oorly "kin #inch goes back
very slo ly)
.#A--HOEA W#THSE:E-E
.EH%.-AT#ON
% Start treat$ent !or se'ere deh"dration 5Plan *61;86
% -EFE- U-GENT/% to hos*ital% Gi'e !re@&ent si*s o! O-S on the (a"% Ad'ise the $other to +ontin&e 3reast!eeding% Kee* the +hild (ar$ on the (a" to hos*ital
#F %ES,ASK
Forho
l
ong?
If diar r hoea f or 36 day
s
ormore*hasthechildlost eight?
Isther ebloodinthestool?
!hattreat
ment isthemothergiving?
/OOKO-FEE/:
JLook at the child&s gener al cond
i
tion)
Is the child:@ Lethar gic
or unconscio
u
s?@$estless and ir r itable?
JLo
okforsunkeneyes
J(ff erthechild
fluid)
Is thechild:@
ot able to dr ink or dr inking #oor ly?@Drinkin
-
8/12/2019 IMCI Chart Booklet Trytry
6/80
geagerly*thir sty?
J Pinchthe skinof theabdomen)
Doesitgoback:@sloly?
@ or verysloly?.morethan 1seconds/
diar rhoea !or .EH%.-AT#ON
lassi!".#A--HOEA
And i!diarrhoea 1=da"sor$ore+lassi! "
T oofthefolloingsigns: $
estless*irritable
"unkeneyes
Dr inkseagerly*thirsty
"kin#inchgoes
backsloly)
otenou
ghsignstoclassify assevere orsome dehydration
Dehydration#resent($
,istory ofeightloss
o dehyd
r ation and
ohistor y ofeight
loss
.#A--HOEA W#THSOME
.EH%.-AT#ON
NO :#S#9/E
.EH%.-AT#ON
SE:E-EPE-S#STENT.#A--HOEA
PE-S#STENT.#A--HOEA
%0ive f luid and f ood to tr eat f or some dehydr ation .Plan
B #)34/%
'dvisemothertocontinuebr eastfeeding%
'dvisethe
mother
hentoreturnimm
ediately.#)18/%Follo@u#in1daysifnotim#r oving
%0ivefluidandfoodtotreatfordiar rhoeaathome .Plan
'#)34/%
'
dvisemother
hentor etur nimm
ediately.#)18/%F
ollo
@u#in4daysif
notim#r oving
% Star ttr eat$ent! or deh"dr at
ion 5i!*r esent8
%Gi'e:ita$inA&nlessadosehas3eengi'eninthelast$onth5*6128%onsiders"$*to$ati+H#:5*6 8
%Gi'e
! r e@&entsi*s o!O-S on the (a"% -
e! er to hos*ital
% Counsel the m
otheraboutfeeding.#)14/
%0ivevitamin
'unlessados
th.#)31/%Considersym#tomatic,I;.#)9/%
'd
visemother
hentoreturnimmediately.#)18/%Follo@u#in4days
And i!3lood
in stool+lassi! "
E:E-E.
%SENTE-
%
% Start treat$ent!or deh"dration i!*resent% -e!erU-GENT/% tohos*ital% Gi'e !re@&ent
si*so!O-Sonthe
(a"
%T
reat for 4days ithnalidiAicacid .#)>/
% 'dvisethemotherhen toreturnimmediately .#)18/% Follo @u# in 1days
Di 's3
-
8/12/2019 IMCI Chart Booklet Trytry
7/80
guideline
-
8/12/2019 IMCI Chart Booklet Trytry
8/80
.oes the +hild ha'e !e'er4By history* or tem#erature 59)4K C or above
lassi!" all +hildren (ith
6
'ny general dangersign ($
"tiff neck($
Bulging fontanelle)
SUSPE TE. MEN#NG#T#S
% Gi'e !irst dose o! a$*i+illin #M or +e!tria one #M 5*6178% Test the 3lood s&gar, then treat or *re'ent lo( 3lood s&gar
5Page 1=8% Gi'e one dose o! *ara+eta$ol !or !e'er 7BC or a3o'e 5*61?8% -e!er U-GENT/%#F
%ES,ASK
Forho
long?
Ifmorethan 9days*hasfeverbeen#resenteveryda
y?
/OOKAN.FEE/
For sti
f f neck and bulging f ontanel
le)
Look f orothercauses off ever
!e'er!or MEN#NG#T#S
ogener aldangersignsand
o stif f neck or
bulging f ontane
lle
-
8/12/2019 IMCI Chart Booklet Trytry
9/80
FE:E- ) OTHE-AUSE
%Treatcauseoffeverif
found%0ive#ar
acetamolintheclini
cforhigh
fever5/ and test to determine hetherthe child is infected at age 31 months
- if the child is o'er one "ear arrange testingto determine if the child is infected% Counsel mother about her o n health and about #revention
of ,I; infection% If breastfeeding counsel about im#ortance of safe seA
during breastfeeding to #revent ,I; transmission tothebaby if the mother becomes infected hile breastfeeding
#! the +hild has 3een +lassi!ied as s"$*to$ati+ H#: in the *ast and had a *ositi'e H#: test, do not assess again ) gi'e !ollo()&*+are !or +on!ir$ed s"$*to$ati+ H#: 5*6 2?8
-
8/12/2019 IMCI Chart Booklet Trytry
15/80
"ym#tomatic ,I; 'ssess and classify G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
16/80
THEN HE K THE H#/.DS #MMUN#SAT#ON STATUS% Gi'e all $issed i$$&nisations toda"6 This in+l&des si+ +hildren 5&nless 3eing re!erred8 and those
(itho&t their +ards% #! there is no -TH gi'e a ne( one toda"% Ad'ise the $other (hen to +o$e !or the ne t i$$&nisation
fjjrkf p^qflk p` ebarib!
d b
Birth
8 eeks
3 eeks
36 eeks
> months
s ` ` fkb
BC0 (P;@
DPT ,IB@3 (P;@3 ,e# B3
DPT ,IB@1 (P;@1 ,e# B1
DPT ,IB@5 (P;@5 ,e# B5
2easles 3
Check vitamin ' and give
dose if
:#T AM#N A P-OPH%/A #S
0ive every child a dose of vitamin ' everysiA months from the age of 8 months .#)31/)$ecord the dose on the $T,C
-OU T#NE WO-M T-EATMENT0ive every child mebenda ole every 8months from the age of one year) $ecord
3< months
4 yearsDPT@6 (P;@6 2easles 1 none given in #ast 8 months.#)31/
DT (P;@4
the dose on the $T,C)
ASSESS OTHE- P-O9/EMS$emember to ask if the child has any other #roblems like skin sores not covered in the I2CI assessment
MAKE SU-E H#/. W#TH AN% GENE-A/ .ANGE- S#GN #S -EFE--E. after first dose of an a##ro#riate antibiotic and other urgent treatments)Check the blood sugar in all children ith a general danger sign and treat or #revent lo blood sugar)
G I2CI 0uideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
17/80
Immunisation 'ssess and classify
"
-
8/12/2019 IMCI Chart Booklet Trytry
18/80
T-EAT THE H#/.A--% OUT THE T-EATMENT STEPS #.ENT#F#E. ONTHE ASSESS AND CLASSIFY
HA-T
TEA H THE MOTHE- TO G#:E O-A/ .-UGS For WHEE>E gi'e Sal3&ta$ol and PrednisoneAT HOMEFollo( the general instr&+tions 3elo( !or e'er" oral dr&g to 3e gi'en atho$e6 Also !ollo( the instr&+tions listed (ith ea+h dr&gDs dosage ta3le6
% .eter$ine the a**ro*riate dr&gs and dosage !or the +hildDs age or(eight
% Tell the $other the reason !or gi'ing the dr&g to the +hild
% .e$onstrate ho( to $eas&re a dose
% Wat+h the $other *ra+tise $eas&ring a dose 3" hersel!
% As the $other to gi'e the !irst dose to her +hild
% E *lain +are!&ll" ho( to gi'e the dr&g
% Ad'ise the $other to store the dr&gs sa!el"
% E *lain that all the ta3lets or s "r&* $&st 3e &sed to !inish the+o&rse o! treat$ent, e'en i! the +hild gets 3etter
% he+ the $otherDs &nderstanding 3e!ore she lea'es the +lini+
For H#: #NFE T#ON gi'e o)tri$o azole to Pre'ent#n!e+tions
% ",( LD (T B+ 0I;+ T( B'BI+" D+$ 8 !++ " (F '0+% For 3a3ies o! $others (ho are H#: in!e+ted, give co@trimoAa ole once
SA/9UTAMO/5-a*id a+ting
3ron+hodilator8
WE#GHT
P-E.N#SONE
.4mg/(nce daily
6@8kg 1 tabs
O8@>kg 5 tabs
O>@31kg 6 tabs
O31@ 4 tabs
O36@ 8 tabs
O39@3>kg
9 tabs
O3>@1 kg
< tabs
"albutamol metered doseinhaler .3 ug #uff/ 4 #uffs
ith a s#acer for 4 days
USE OF A SPA E- ' s#acer is a ay of delivering the bronchodilator drugs effectively into thelungs) o child under 4 years should be given an inhaler ithout a s#acer) 's#acer orks as ell as a nebuliser if correctly used)
S*a+ers +an 3e $ade in the !ollo(ing (a"% se a 4 ml cool drink bottle)% Cut a hole in the end or the to# of the bottle in the same sha#e as the
mouth#iece of the inhaler) This can be done using a shar# knife% In a small baby a mask can be made by making a similar hole in a
#lastic .not #olystyrene/ cu#% 'lternatively commercial s#acers can be used if available
To &se an inhaler (ith a s*a+er% "hake the inhaler ell% Insert mouth#iece of the inhaler through the hole in the bottle or #lastic
cu#)% The child should #ut the o#ening of the bottle into his mouth and breath
in and out through the mouth% ' carer then #resses do n the inhaler and s#rays into the bottle hile the
child continues to breath normally% !ait for three to four breaths and re#eat for total of five s#rays% For younger children #lace the cu# over the child&s mouth and use as a
s#acer in the same ay
+ " $+ T,'T 'LL C'$+$" (F C,ILD$+ "I 0 I ,'L+$" '$+ 'BL+ T( "+ ' I ,'L+$ ' D "P'C+$ +FF+CTI;+L%
daily for five days a eek from the age of 8 eeks) If the baby has nosym#@toms at 31 months arrange ,I; testing to determine if child is infected
% For +hildren (ith s"$*to$ati+ H#:in!e+tion give once daily five days #er eek.can be given even if mother refuses ,I;testing/
For PNEUMON#A and A UTEEA-
-
8/12/2019 IMCI Chart Booklet Trytry
19/80
AGE WE#GHT
AMO % #//#NS%-UP
.314 mg #er 4ml/
0ive three1 to31 monhs
6@4 kg 1*4 ml
O4= 3 4 ml
31 monthsto
4 years
O3 = 36 9)4 ml
O36@1
k3 ml
AGEor WE#GHT
NA/#.## A #.
SUSPENS#ON
.14 mg 4 ml)/
0ive four31@16 months
#9@ N34kg/ 1)4 ml
1@4 years.34@ N1 kg/ 4 ml
#NFE T#ON gi'e A$o "+illin
For .%SENTE-% gi'eNalidi i+ A+id
-
8/12/2019 IMCI Chart Booklet Trytry
20/80
O)T-#MO A>O/E S%-UP 5 =?
-
8/12/2019 IMCI Chart Booklet Trytry
21/80
TEA H THE MOTHE- TO G#:E O-A/ .-UGS AT HOMEFollo( the instr&+tions 3elo( !or e'er" oral dr&g to 3e gi'en at ho$e
Also !ollo( the instr&+tions listed (ith ea+h dr&gDs dosage ta3le
% Gi'e Para+eta$ol !or +hroni+ *ainrelie! 5stage 18% Add reg&lar odeine !or +hroni+ se'ere
*ain 5stage 28% "afe doses of Paracetamol can be slightly higher for #ain) se the table and teach
mother to measure the right dose)% 0ive Paracetamol every 8 hours if #ain ."tage 3/ #ersists)
Stage 2 *ain is chronic severe #ain as might ha##en in illnesses such as 'ID")% "tart treating "tage 1 #ain ith regular .not #rn/ #aracetamol)% In older children* Q Paracetamol tablet can re#lace 3 ml syru#% If the #ain is not controlled* add regular .not #rn/ codeine)% "tart Codeine on the lo er dose* gradually increasing de#ending on the child&s re@
s#onse* to the maAimum dose)
For ANAEM#A gi'e #ron% Check the strength and dose of the iron syru# tablet very carefully% 0ive t o doses daily for 1 months) Follo @u# every 36 days for 1 months% 0ive Iron syru# ith food) Iron may make the stools black)% (verdose ith iron is dangerous* caution the mother to kee# it out of reach of children)
AGE or WE#GHT #-ON S%-UPFerrous gluconate
0ive t ice daily
1 months u#to 6 months .6 @ N8 kg/ 4 dro#s
6 months u#to 16 months .8@N34kg/ 3
1R4 years .34 @ 15 kg/ 1
For MA/A-#A Gi'e o)arte$ether % -EFE- A// H#/.-EN UN.E- ONE %EA- U-GENT/% TO HOSP#TA/% 0ive the first dose of co@artemether in the clinic and observe for one hour 6If child
vomits ithin an hour re#eat the dose% "econd dose should be taken at home < hours later % Then t ice daily for further t o days% Co@artemether should be taken ith food
WE#GHT 5age8 O)A-TEMET
TOTA/ NUM9E-OF
3 = 34kg .3@4 years/ 3 tablet 8
(ver 34kg 1 tablets 31
WE#GHT
AGE.(nly if you do
notkno the
ei ht
PainStage 1Para+eta
$ol ; hrl"
Pain Stage 2Add odeine Phos*hate
s"r&* 20 $g *er 0 $l ; hrl"#nitial dose Ma i$&$
1 @ N5k
nder 1months
1m
)1 ml 3) ml
5 @ N4k
1 u# to 8months
1)4 ml )5 ml 1) ml
4 @ NEPAM53 mg 1mls/
N 4kg N8 months )4 mls
4@ N 3 kg 8@ N 31 months 3) mls
3 @ N 34kg 3@ N 5 years 3)4mls
34= 3> kg 6@ N 4years 1) mls
% If convulsions have not sto##ed after 3 minutes re#eat dia e#am dose
-
8/12/2019 IMCI Chart Booklet Trytry
28/80
AMP# #//#N% Check strength of am#icillin) sually 14 mg vials but other strengths are avail@
able)% Dilute 14 mg vial ith 3ml of sterile ater .14 mg ml/% IF $+F+$$'L I" (T P(""IBL+ ($ D+L'%+D* re#eat the am#icillin in ection
every 8 hours% Where there is a strong s&s*i+ion o! $eningitis the dose o! a$*i+illin +an
3e in+reased = ti$es
AGE WE#GHT .OSE .OSE AMP# #//#Nkg 4 1)
Clinic treatmentsT reat the child
13G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
29/80
G#:E THESE T-EATMENTS #N /#N# ON/%% E *lain to the $other (h" the treat$ent is 3eing gi'en
Pre'ent /o( 9lood S&gar 5H"*ogl"+ae$ia8 d&ring Trans!er to Hos*ital% #! the +hild is a3le to s(allo(
If breastfed: ask the mother to breastfeed the child* or give eA#ressed breastmilk If not breastfed give a breastmilk substitute or sugar ater) 0ive 5 @4 ml of milk or sugar ater before de#arture To make sugar water: Dissolve 4 level teaspoons of sugar (20 grams) in a 200-ml cup of clean water
% #! the +hild is not a3le to s(allo( Insert nasogastric tube and check the #osition of the tube 0ive 4 mls of milk or sugar ater before transfer
Treat the +hild !or /o( 9lood S&gar /OW 9/OO. SUGA- #S /ESS THAN 7 $$ol
-
8/12/2019 IMCI Chart Booklet Trytry
30/80
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
31/80
G#:E E T-A F/U#. FO- .#A--HOEA AN. ONT#NUE FEE.#NG
Plan A Treat !or .iarrhoea at Ho$e
o&nsel the $other on the 7 -&les o! Ho$e Treat$ent1' Gi'e E tra Fl&id, 26 ontin&e Feeding, 76
When to -et&rn
1' GIVE E TRA FLUID .as much as the child ill take/% TE// THE MOTHE-2
Breastfeed freHuently and for longer at each feed If the child is eAclusively breastfed* give sugar@salt solution ."""/ in addition
to breastmilk If the child is not receiving breastmilk or is not eAclusively breastfed* give one or
more of the follo ing: food@based fluids such as soft #orridge* amasi .maas/*""" or ($")
#t is es*e+iall" i$*ortant to gi'e O-S at ho$e (hen
the child has been treated ith Plan B or Plan C during this visit the child cannot return to a clinic if the diarrhoea gets orse
%TEA H THE MOTHE- HOW TO M# AN. G#:E SSS or O-STo make """: 3 litre boiled .or clean/ ater
< teas#oons sugar half a teas#oon salt
% SHOW THE MOTHE- HOW MU H F/U#. TO G#:E #N A..#T#ON TO THEUSUA/ F/U#. #NTAKE
# to 1 years: 4 to 3 ml after each loose stool1 years or more: 3 to 1 ml after each loose stool
Tell the $other to
0ive freHuent small si#s from a cu#) If the child vomits* ait 3 minutes) Then continue* but more slo ly C ontinue giving eAtra fluid unti l the diarrhoea sto#s
SSS is the sol&tion to 3e &sed at ho$e to prevent deh"drationO-S sa+hets $i ed (ith +lean (ater are &sed to +o rre!t deh"dration 6
Plan 9 Treat !or So$e .eh"dration (ith O-S
Gi'e in +lini+ re+o$$ended a$o&nt o! O-S o'er =)ho&r *eriod% .ETE-M#NE AMOUNT OF O-S TO G#:E .U-#NG F#-ST = HOU-S6
0ive 1 mls of ($" for each kg of body eight every hour
AGE U* to =$onths
= $onths&* to 12$onths
12 $onths&* to 2"ears
2 "ears&* to 0"ears
WE#GHT N 8 kg 8 @ N 3 kg 3 @ N 31 kg 31 @ N1 kg
A$o&nt o! !l&id o'er = ho&rs in $ls
1 @ 64 64 @ < < @ >8 >8 @ 38
VUse the chil !s age onl" when "ou o not know the weight. The appro#imate amount of $%& re'uire (in ml) canalso e calculate " multipl"ing the chil !s weight in kg times 20 an give this amount of flui ever" hour(20mls kg). $ne teacup is appro#imatel" 200mls
% SHOW THE MOTHE- HOW TO G#:E O-S SO/UT#ON6 0ive freHuent small si#s from a cu# If the child vomits* ait 3 minutes) Then continue* but more slo ly Continue breastfeeding henever the child ants If the child ants more ($" than sho n* give more
% AFTE- = HOU-S2 $eassess the child and classify the child for dehydration "elect the a##ro#riate #lan to continue treatment Begin feeding the child in clinic
% #F THE MOTHE- MUST /EA:E 9EFO-E OMP/ET#NG T-EATMENT
"ho her ho to #re#are ($" solution at home "ho her ho much ($" to give to finish 6@hour treatment at home 0ive her instructions ho to #re#are """ for use at home +A#lain the 5 $ules of ,ome Treatment:
2' CONTINUE FEEDING
3' "HEN TO RETURN See COUNSEL THE MOTHER +hart5*621)2 8
1' GIVE E TRA FLUID
-
8/12/2019 IMCI Chart Booklet Trytry
32/80
2' CONTINUE FEEDING 3' "HEN TO RETURN See Plan A !orre+o$$ended !l&ids
and See COUNSEL THE MOTHER +hart 5*621)2 8
Diarrhoea@Plan ' and BT reat the child
15G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
33/80
G#:E E T-A F/U#. FO- .#A--HOEA AN. ONT#NUE FEE.#NG
Plan Treat !or Se'ere .eh"dration &i+ l"% cliil( qeb ^ool( p) fc
^kp( bo f p *vbp+ , dl
^`ol pp) fc *kl+, dl al( k) J Start #: !l&id i$$ediatel" ) If the child can drink* give ($" by mouth hile the dri# is set u#) 0ive 1 ml kg $inger&s Lactate "olution .or* if not available* normal saline/ every hour
#n the !irst hal! ho&r Plan !or the ne t 0 ho&rs0ive 1 ml I; for each kilogram eight* beforereferral
-e*eat this amount if brachial #ulse is eak ornot detectable 6
0ive 1 ml I; for each kilogram eight* everyhour hile the child is in the clinic a aitingtransfer)
2onitor and record ho much fluid the child receives
"T'$T ,+$+
Can you give intravenous .I;/ fluidimmediately?
vb#
kl
Is I; treatmentavailable nearby . ithin5minutes/?
vb
Arrange &rgent re!erral to hos*ital !or !&rther $anage$ent -eassess the +hild e'er" 1) 2 ho&rs (hile a(aiting trans!er6 If hydration status is not im#roving* give
the I; dri# more ra#idly) 'lso give ($" .about 4 ml kg hour/ as soon as the child can drink: usually after 5@6 hours .infants/ or 3@
1 hours .children/) $eassess an infant after 5 hours if he is still at the clinic) Classify dehydration) Then choose the
a##ro#riate #lan .'* B* or C/ to continue treatment) If you cannot refer observe for at least 8 hours after the child has been fully rehydrated
-e!er U-GENT/% to hos*ital !or #: treat$ent ) If the child can drink* #rovide the mother ith ($" solution and sho her ho to give freHuent si#s
during the tri# or give ($" by naso@gastic tube)
k
're you trained to use a naso@gastric . 0/ tube forrehydration?
kl vb
Can the child drink?
-
8/12/2019 IMCI Chart Booklet Trytry
34/80
kl
$efer $0+ TL% to hos#ital for I; or 0 treatment
Start reh"dration 3" t&3e 5or $o&th8 (ith O-S sol&tion : give 1 ml kg hour for 8 hours .total of 31ml kg/)
Arrange &rgent re!erral to hos*ital !or !&rther $anage$ent -eassess the +hild e'er" 1)2 ho&rs (hile (aiting trans!er
)If there is re#eated v omiting or abdominal distension* give the fluid more slo ly) 'fter 8 hours reassess the child if he is still at the clinic) Classify dehydration) Then choose the
a##ro#riate #lan .'* B* or C/ to continue treatment)
NOTE If the child is not referred to hos#ital* observe the child at least 8 hours after rehydration to be sure
the mother can maintain hydration giving the child ($" solution by mouth)
Diarrhoea@#lanC Treat the child
16
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
35/80
G#:E FO//OW)UP A-Eare !or the +hild (ho ret&rns !or !ollo()&* &sing A// the 3o es that $at+h +hildDs *re'io&s +lassi!i+ations6
#! the +hild has an" ne( *ro3le$, assess, +lassi!" and treat the ne( *ro3le$ as on the ASSESS AND CLASSIFY +hart6
% PNEUMON#AA!ter 2 da"s Check the child for general danger signs)
'ssess the child for cough or difficult breathing)I#WW X##b ## C YiX##fcv % .#A--HOEAA!ter 2 da"s 5diarrhoea (ith so$e deh"dration8 or 0 da"s 5no 'isi3le
deh"dration8, i! diarrhoea *ersists
As @ Is the child breathing slo er?- Is there less fever?- Is the child eating better?
Treat$ent
+Z (F 'ssess the child for general dangersignsand diarrhoea)
As ) 're there fe er stools?@ Is the child eating better?
Treat$ent
I#WW X##b ## C YiX##fcv
% If +hest indra(ing or a general danger sign * give first dose of ceftriaAone or am#icillin I2I)Then -EFE- U-GENT/% to hos*ital6
% #! 3reathing rate, !e'er and eating are the sa$e, or (orse -EFE- .unless the child hasnot been taking the antibiotics correctly/)
% #! 3reathing slo(er, less !e'er, or eating 3etter, com#lete the 4 days of antibiotic)
-e$ind the $other to gi'e one e tra $eal dail" !or a (ee 6
% WHEE>E 5F#-ST EP#SO.E8A!ter 2 or 0 da"s i! still (heezing
Check the mother is using the inhaler and s#acer correctly 'ssess and classify the child for cough or difficult breathing andtreat according tc classification) .see *&&+&& , *&&/1 #)1/
'sk: @ ,as the child&s breathing im#roved?
Treatment:
% If the child is still hee ing and the mother is using the inhaler correctly $+F+$)% If the child is still hee ing* and the mother is not using the inhaler correctly= sho her ho
to use it and let her #ractise until she feels confident) $evie in another five days) If stillhee ing after a further 4 days refer)
% If the hee ing has sto##ed advise the mother to kee# the inhaler and s#acer at home anduse it if the hee ing recurs) "he should bring the child back if the hee e recurs)
% #! +hild is deh"drated no(, treat !or deh"dration and -EFE-% If diarrhoea same as before and classified as ( ;I"IBL+ D+,%D$'TI( continue
ith #lan ' at home and revie again in 4 days) If diarrhoea still continuing after afurther 4 days* treat for #ersistent diarrhoea and $+F+$
% If diarrhoea im#roving continue ith home treatment
% .%SENTE-%A!ter 2 da"s
'ssess the child for diarrhoea) &ee *&&+&& , *&&/ 1 (p3)As
- 're there fe er stools?- Is there less blood in the stool?- Is there less fever?- Is there less abdominal #ain?- Is the child eating better?
Treat$ent% If the child is deh"drated * treat for dehydration .#)34 M 38/ and -EFE-
% If n&$3er o! stools, 3lood in the stools, !e'er, a3do$inal *ain, or eating is(orse or the sa$e -EFE-
% #! !e(er stools, less !e'er, less a3do$inal *ain, and eating 3etter continuegiving nalidiAic acid until finished
Ens&re that ) the $other &nderstands the oral reh"dration $ethod !&ll") the $other &nderstands the need !or an e tra $eal ea+h da" !or a
(ee
-
8/12/2019 IMCI Chart Booklet Trytry
36/80
Pneumonia* diarrhoea* hee e* dysentery0ive follo u# care
1G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
37/80
dfs b cliil( -r. ^ob% are !or the +hild (ho ret&rns !or !ollo()&* &sing all the 3o es that $at+h the
childDs *re'io&s +lassi!i+ations6% #! the +hild has an" ne( *ro3le$, assess, +lassi!" and treat the ne( *ro3le$ as
on the ASSESS AND CLASSIFY +hart6
% PE-S#STENT .#A--HOEA
A!ter 0 da"sAs @ ,as the diarrhoea sto##ed?
@ ,o many loose stools is the child having #er day?
Treat$ent% If the diarrhoea has not sto**ed .child is still having 5 or more loose stools #er day/)
Treat for dehydration if #resent) Then -EFE- to hos#ital)
% If the diarrhoea has sto**ed .child having less than 5 loose stools #er day ) counselon feeding .#)13@16/ and tell the mother to gi'e one e tra $eal e'er" da" !or one (ee
NOTE Attention to the diet is an essential *art o! the $anage$ent o! the +hild (ith*ersistent diarrhoea )
% MA/A-#A
#! !e'er *ersists a!ter 2 da"s, or ret&rns (ithin 1= da"s :Do a full reassessment of the child for fever) &ee *&&+&& , *&&/ 1 (p 4)
Treat$ent% If the child has an" general danger sign, 3&lging !ontanelle or sti!! ne+ * treat as
" "P+CT+D 2+ I 0ITI" .#)6/ and -EFE-6
% #! $alaria ra*id test (as *ositi'e at initial 'isit and fever #ersists or recurs -EFE-the child to hos#ital
% If the child has any +a&se o! !e'er other than $alaria * give treatment
o&nsel about #revention of malaria including the im#ortance of insecticide@treated bednets
% FE:E- ) OTHE- AUSE#! !e'er *ersists a!ter 2 da"sDo a full reassessment of the child for fever) &ee *&&+&& , *&&/ 1 (p. 4)
'ssess for other causes of fever)
Treat$ent% If the child has an" general danger sign or sti!! ne+ or 3&lging !ontanelle * treat as for
" "P+CT+D 2+ I 0ITI" .#) 6/ and -EFE- &rgentl"
% If the child has any identi!ied +a&se o! !e'er give treatment
% If no +a&se o! !e'er is !o&nd, -EFE-
% #! !e'er has 3een *resent e'er" da" !or da"s *-EFE-
% EA- #NFE T#ONA!ter 0 da"s i! *ain or dis+harge *ersists$eassess for ear #roblem) O &ee *&&+&& , *&&/ 1 chart. ( p. 5)Check for fever
Treat$ent
A UTE EA- #NFE T#ON% If there is tender s(elling 3ehind the ear or high !e'er .5
-
8/12/2019 IMCI Chart Booklet Trytry
38/80
iar r hoea* m
alar ia* Fever
= o
ther cause* ear
inf ection) 0ive
f ollo
u# c
ar e
1"
G I2CI guideline"e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
39/80
G#:E FO//OW)UP A-E% are !or the +hild (ho ret&rns !or !ollo()&* &sing all the 3o es that $at+h the +hildDs
*re'io&s +lassi!i+ations6
% #! the +hild has an" ne( *ro3le$, assess, +lassi!" and treat !or the ne( *ro3le$ as on
the ASSESS AND CLASSIFY +hart6
% FEE.#NG P-O9/EMA!ter 0 da"s
- 'ssess feeding .#)13/ and counsel .#)13@16/)- $evie the feeding #roblem identified at the last visit- If you counsel her to make further changes to her child&s feedingfollo u# again in another 4 days- Check on available resources and ensure that advice is a##ro#riate
% $evie every 5 days until the child is gaining eight
% ANAEM#AA!ter 1= da"s
@ Check haemoglobin*
Treat$ent
% #! hae$oglo3in lo(er than 3e!ore, -EFE-
% If the hae$oglo3in has not i$*ro'ed or the child has #almar #allor afterone month* -EFE- for assessment
% Ifhae$oglo3in is higher than 3e!ore, continue iron) $evie in 36 days) Continuegiving iron every day for 1 months
% NOT G-OW#NG WE//A!ter 1= da"s
@!eigh the child and determine if the child is still lo eight for age)- Determine eight gain- $eassess feeding .#)13/ and counsel .#)13@16/
Treat$ent% If the child gaining (eight (ell * #raise the mother) $evie monthly for gro th monitoring)
% If the child is still lo( (eight !or age, counsel the mother about feeding) 'sk the motherto return in 36 days) $evie monthly until the child is feeding ell and gaining eightregularly or is no longer lo eight for age)
% If the +hild has not gained (eight or has lost (eight * check for #ossible sym#tomatic,I; .#)9/) 'ssess feeding and if there is a feeding #roblem counsel and revie in further36 days) If #oor eight gain continues after another 36 days -EFE-
% E#!ept$%n: If you do not think that feeding ill im#rove* refer the child)
IF ' % 2($+ F(LL(!@ P ;I"IT" '$+ ++D+D* 'D;I"+ T,+ 2(T,+$ (F T,+ NE T FO//OW)UP :#S#T 'D;I"+ T,+ 2(T,+$ WHEN TO -ETU-N #MME.#ATE/% 5*62;8
Chronic +ar infection* feeding #roblem* 'naemia* ot gro ing ellFollo u# care
1$G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
40/80
dfs b cliil( -r. `^ob clo qeb `efia ( fqe pr p.b`qba pvj.qlj^qf` efs lo h kl( k efs
%FO//OW)UP FO- SUSPE TE. S%MPTOMAT#H#: 5!irst ret&rn 'isit onl"8
If child has had an ,I; test* check results
#! testing not done% 'dvise the mother about benefits of ,I; testing and
refer for further counselling if necessary)% 'rrange ,I; counselling and testing if mother
agrees)% Tell mother about available su##ort structures and if
acce#table* #ut her in contact ith these #eo#le)% If mother refuses testing #rovide ongoing care for the
child according to routine monthly follo @u# of all,I; infected children .this #age/) Discuss ith themother hether she ishes the child to have co@trimoAa ole)
#! H#: test *ositi'e% +nsure that the mother receives #ost@test counsel@
ling)% Discuss ith her any other orries or Huestions that
she has)% Tell her about organisations* su##ort grou#s or focal
#eo#le that could #rovide su##ort)% Treat according to routine monthly follo @u# of all
,I; infected children .this #age/% If child is belo 31 months the test ill need to be
re#eated after 31 months of age to confirm infection
#F H#: test negati'e% Counsel mother on #reventing ,I; infection and
about her o n health% If breastfeeding advise her about the im#ortance of
safe seA during breastfeeding
%FO//OW)UP MONTH/% FO- SUSPE TE. O- ONF#-ME. H#:#NFE T#ON
For all +hildren +on!ir$ed H#: *ositi'e or (here there isSUS) PE TE. S%MPTOMAT# H#: and the stat&s is still&n no(n
% "tart continue co@trimoAa ole #ro#hylaAis .#)>/
% 'ssess and classify the child at each visit and treat according to classifications
% 'ssess feeding* and check eight and eight gain)- +ncourage breastfeeding mothers to continue breastfeeding- Poor a##etite and lo eight are common in these children*
advise on any ne or continuing feeding #roblems .#)13@16/- Check for oral thrush and mouth sores and treat .#)33/
- If any history of diarrhoea* check for na##y rash and treat% 0ive ;itamin ' according to schedule .#)31/)
% Provide #ain relief if the child is in any #ain .#)3/)
% Tell the mother about community su##ort structures and if ac@ce#table* #ut her in contact ith them)
% 'dvise about home care- 'dvise mother to bring the child back if any ne illness
develo#s because it is im#ortant to treat infections- 'dvise the mother about the im#ortance of hygiene in the
home* in #articular hen #re#aring food for the child)
% Follo @u# monthly
% 2onitor the health of the mother)- 'dvise about safe seA and family #lanning- If the mother is #regnant refer her for counselling her
about #revention of transmission of ,I; and feedingchoices for her ne baby)
%PA//#AT#:E A-E FO- S%MPTOMAT# H#: #NFE T#ON
% This should hel# the family care for the child ith as littlesuffering as #ossible) This starts at the time of diagnosisand continues throughout the illness
% 2edical thera#y may be discontinued because it is leadingto unnecessary suffering and se#aration of the child fromhis family) T,I" D+CI"I( ",( LD B+ 2'D+ 'T T,+ $+F+$$'L C+ T$+ 'FT+$ T,+ C,ILD ,'" B++F LL% '""+""+D)
% 'fter this decision has been made #alliative care alone canbe offered at #rimary care level) ntil then #alliative careshould be offered together ith routine medical treatment
Palliati'e +are sho&ld 3e gi'en as !ollo(s :% If the child has #ain #rovide adeHuate *ain relie! )
' 5 stage #rocess may be used .#)3 /:% "tage 3: #aracetamol%"tage 1 .if #ain is not ell controlled/: codeine #hos
#hate% "tage 5 .if #ain relief still not ell controlled/: mor#hine
may be used as #rescribed by the doctor)
% o&nsel the mother so that:% the child remains nourished and ell hydrated% the child remains clean* dry and comfortable% any skin lesions .abscesses or ulcers/ are dressed and
ke#t clean
% S&**ort the mother and other family members:%$efer to community su##ort structures .if acce#table/
%Provide information and counselling to hel# the family ithHuestions and fears they may have%The family mother should make a decision about here it
is best for the child to die%Counsel the mother about her o n health
"ym#tomatic ,I; Infection0ive follo u# care
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
41/80
2%
-
8/12/2019 IMCI Chart Booklet Trytry
42/80
`lrkpbi qeb jlqebo
% Assess the Feeding o! Si+ hildren &nder 2 "ears5or i! ANAEM#A or NOT G-OW#NG WE// 8 'sk Huestions about the child&s usual feeding and feeding during this illness) Com#are the mother&s ans ers to theFeed$n& Re!%mmendat$%n' for the child&s age on # 3>
ASK ( Ho( are "o& !eeding "o&r +hild4
#! the 3a3" is re+ei'ing an) 3reast$il *ASK
- ,o many times during the day?- Do you also breastfeed during the night?
#! 3a3" is re+ei'ing re*la+e$ent $il , ASK
- !hat re#lacement milk are you giving?- ,o many times during the day and night?- ,o much is given at each feed?- ,o is the milk #re#ared?- ,o is the milk being given? Cu# or bottle?- ,o are you cleaning the utensils?- If still breastfeeding as ell as givingre#lacement milk could the mother give eAtrabreastmilk instead of re#lacement milk .es#ecially
if the baby is belo 8months/
Does the child take any other food or fluids?- !hat food or fluids?
- ,o many times #er day?- !hat do you use to feed the child?
#! lo( (eight !or age, ASK- ,o large are servings?
- Does the child receive his o n serving?- !ho feeds the child and ho ?
-
8/12/2019 IMCI Chart Booklet Trytry
43/80
During this illness* has the child&s feeding changed? If yes* ho
Feeding adviceCounsel the mother
21G I2CI guideline 'ugust 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
44/80
`lrkpbi qeb jlqebo
FEE.#NG -E OMMEN.AT#ONS #N S# KNESS AN. #N HEA/THNOTE: These feeding recommendations should be followed for infants of all mothers who DO NOT KNOW their HIV status
U* to ;Months o! Age
Breastfeed as often as the child ants*day and night*
Feed at least < times in 16 hours)
Do not give other foods or fluids
; Months &*to 12 Months
Continue to breastfeed asoften as the child ants
0ive 7 ser'ings of nutritious com#lementary foods) Al(a"s miAmargarine* fat* oil* #eanut butter or ground nutsith #orridge)
'lso add: chicken* egg* beans* fish or full cream
milk* or mashed fruit and vegetables* at least
once each day)
If baby is not breastfed* give 5 cu#s .5 A 1 ml/of full cream milk as ell)
If baby gets no milk* give 8 com#lementaryfeeds #er day
12 Months &*to 2 %ears
Continue to breastfeedas often as the childants) Breastmilk is still an im#ortant foodat this age and hel#s #revent infections
0ive at least 4 adeHuate nutritious feeds)Increase the variety and Huantity ithfamily foods:
2iA margarine* fat* oil* #eanut butteror ground nuts ith #orridge 0ive egg* meat* fish or beans daily 0ive fruit or vegetables t ice every
day 0ive milk every day* es#ecially if no
longer breast feeding)
Feed actively ith her o n serving
2 %ears andOlder
0ive the child her o n servingof family foods 5 times a day)
In addition* give 1 nutritioussnacks such as bread ith #eanutbutter* full cream milk or fresh fruitbe@ t een meals
Continue active feeding
-
8/12/2019 IMCI Chart Booklet Trytry
45/80
objbj/bo ql bk`lro^db cbbafkd arofkd fiikb pp ^ka ql ^asf pb ql dfsb ^k b0 qo^ jb^i ^ a^v clo lkb ( bbh ^cqbo ^k fiikbpp F
Feeding recommendationsCounsel the mother
22 G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
46/80
FEE.#NG -E OMMEN.AT#ONS #F MOTHE- #S H#: POS#T#:E
U* to ;Months o! Age
Sa!e transition!ro$
e +l&si'e3reast!eeding
; Months &*to 12Months
12 Months &*
to 2 %ears
9reast!eed e +l&si'el" as often asthe child ants* day and night) Feed at least < times in 16 hours) Do not give other foods or fluids .2iAed
feeding could lead to ,I; transmission/
"afe transition to re#lacement milk andcom#lementary feeds at 6 to 8 months
O- 5i! !easi3le and sa!e8
For$&la !eed e +l&si'el" .no breast milk at allV/) 0ive formula or modified co &s milk (ther foods or fluids are not necessary Pre#are correct strength and amount ust
before use .#)58/) se milk ithin an hour and discard any left
.a fridge can store formula for 16 hours/
Cu# feeding is safer than bottle
Clean the cu# and utensils ith soa# If using a bottle* also boil 4 minutes or
sterilise after each use 0ive formula 8 to < times a day .#)58/
E +e*tion onl" heat treated or 3oiled3reast $il +an still 3e gi'en
Sa!e transition meansra#idly changing from allbreast milk* to none V)
'void miAing breast milk ith other food orfluids .this increases risk of ,I; transmission/)
"uggest transition some time bet een 6 and 8months* or earlier if mother can safely do so) Do not breast feed after 8 months)
Hel* $other *re*are !or transition 2other should discuss eaning ith her family if #ossible +A#ress milk to #ractice cu# feeding Find a regular su##ly of formula or other
milk Learn ho to safely #re#are and store milkat home
Hel* $other $a e the transition Teach mother to cu# feed her baby
.#)58/
"tart giving only formula or co s milk)"to# breastfeeding com#letely) +A#ress and discard some breastmilk* to
kee# comfortable till lactation sto#s) 0ive com#lementary feeds from 8
months
E +e*tion onl" heat treated or3oiled 3reast $il +an still 3e gi'en
Do not breast feed after siA monthsunless the child is already kno n tobe infected)
0ive 5 servings of nutritious
com#lementary foods) 'l ays miAmargarine* fat* oil* #eanut butter orground nuts ith #orridge)
'lso add: chicken* egg* beans* fish or full cream
milk* or mashed fruit and vegetables* each
day)
0ive at least 5 cu#s .5 A 1 ml/ of fullcream milk .or infant formula/ #er day)0ive milk ith a cu#* not a bottle)
If no milk available* give 8
com#lementary feeds #er day
0ive at least 4 adeHuate nutritiousfeeds)
Increase the variety and Huantity ithfamily foods:
2iA margarine* fat* oil* #eanut butter or ground nuts ith #orridge 0ive egg* meat* fish or beans daily 0ive fruit or vegetables t ice every
day 0ive milk every day
Feed actively ith her o n serving
-
8/12/2019 IMCI Chart Booklet Trytry
47/80
Feeding recommendations for ,I;Counsel the mother
23G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
48/80
% o&nsel the Mother A3o&t Feeding Pro3le$s#! the +hild is not 3eing !ed as in re+o$$endations, +o&nsel the $other a++ordingl"6 #n addition
#! $other re*orts di!!i+<" (ith 3reast!eeding, assess 3reast !eeding6 5See YOUNG INFANT +hart *67? 8o Identify the reason for the mothers concern and manage any breast #roblem
o If needed* sho correct #ositioning and attachmento Build the mother&s confidence) 'dvise her that freHuent feeds im#rove lactation)
#! the +hild is less than ; $onths old and is ta ing other $il or !oodso Build mother&s confidence that she can #roduce all the breastmilk that the child needs) !ater and other milk are not necessary
o If she has sto##ed breastfeeding* refer her to a breastfeeding counsellor to hel# ith re@lactationo "uggest giving more freHuent* longer breastfeeds* day or night* and gradually reducing other milk or foods)#! other $il needs to 3e +ontin&ed, +o&nsel the $other too Breastfeed as much as #ossible* including at night .unless mother is ,I; ve and has chosen eAclusive formula feeding/
o 2ake sure the other milk is infant formula or breastmilk substitute)o Pre#are other milk correctly and hygienically* and give adeHuate amounts)o Finish #re#ared milk ithin an hour)#! she has started +o$*le$entar" !eedso +ncourage her to give milk feeds firsto If the infant is 6 @ 8 months* advise her to continue to give 3 @ 1 nutritious com#lementary feeds #er day)
#! the $other is &sing a 3ottle to !eed the +hildo $ecommend a cu# instead of a bottleo "ho mother ho to feed the child ith a cu# .#)58/
#! the +hild is not 3eing !ed a+ti'el"o "it ith the child and encourage eatingo 0ive the child an adeHuate serving in a se#arate #late or bo l
#! the +hild has a *oor a**etite, or is not !eeding (ell d&ring this illnesso Breastfeed more freHuently and for longer if #ossibleo se soft* varied* favourite foods to encourage the child to eat as much as#ossible) o 0ive foods of a suitable consistency* not too thick or dryo (ffer small* freHuent feeds) Try hen the child is alert and ha##y* and give more food if he sho s interesto Clear a blocked nose if it interferes ith feedingo If the child has a sore mouth* suggest soft foods that don&t burn the mouth e)g) eggs* mashed #otatoes* #um#kin or avocado)o 0ive #hysical hel# @ a s#oon the right si e* food ithin reach* child sitting on caregiver&s la# hile eatingo +A#ect the a##etite to im#rove as the child gets better
#! there is no !ood a'aila3le in the ho&seo ,el# mother to get a Child "u##ort 0rant for all her children under 9 yearso Put her in touch ith a "ocial !orker and local organisations that mayassist o 0ive her vegetables from the clinic gardeno "u##ly milk and "u#er Porridge from the P+2 schemeo 0ive mother reci#es for locally a##ro#riate "u#er Porridge
Feeding #roblems
-
8/12/2019 IMCI Chart Booklet Trytry
49/80
Counsel the mother G I2CI guideline
"e#tember 1 12&
-
8/12/2019 IMCI Chart Booklet Trytry
50/80
S*e+ial Feeding -e+o$$endations
% Feeding Ad'i+e !or the Mother o! a hild (ith S%MPTOMAT# H#: #NFE T#ON
% The child ith sym#tomatic ,I; infection should be encouraged to breastfeed) There is no danger of infection through breastmilk hen the child hassym#@ toms
% The child should be fed according to the feeding recommendations for his age .#)11/
% These children often suffer from #oor a##etite and mouth sores* give a##ro#riate advice .this #age/
% If the child is being fed ith a bottle encourage the mother to use a cu# as this is more hygienic and ill reduce e#isodes of diarrhoea
% Inform the mother about the im#ortance of hygiene hen #re#aring food because her child can easily get sick) "he should ash her hands after going tothe toilet and before #re#aring food If the child is not gaining eight ell* the child can be given an eAtra meal each day and the mother can encourage himto eat more by offering him snacks that he likes if these are available
% 'dvise her about her o n nutrition and the im#ortance of a ell balanced diet to kee# herself healthy) +ncourage her to #lant vegetables to feed her family)
% #! the +hild has a *oor a**etite
Plan small freHuent meals) 0ive milk rather than other fluids eAce#t here there is diarrhoea ith some
dehy@ dration 0ive foods ith a high energy content) 0ive snacks bet een meals) Check for oral thrush or mouth ulcers) Consider ,I; if the a##etite remains #ersistently #oor)
% #! the +hild has $o&th sores
$ecommend soft foods that don&t burn the mouth e)g) eggs* mashed#otatoes* #um#kin or avocado) 'void s#icy* salty and rough foods)
Cho# foods finely and give cold drinks or crushed ice* if available)
% Feeding -e+o$$endationsFor PE-S#STENT .#A--HOEA
If still breastfeeding* give more freHuent* longer breastfeeds* dayand night)
If taking other milk:- 3st choice: re#lace ith increased breastfeeding ($- 1nd choice: re#lace ith fermented milk #roducts* such as amasi
.maas/ or yoghurt ($- 5rd choice: re#lace half the milk ith nutrient@rich semisolid food
.like mashed fruit or vegetables)/
For other foods* follo feeding recommendations for the child&s age 'void very s eet foods or drink
0ive small* freHuent meals at least 8 times a day
Feeding advice for ,I; Infection Counsel the mother 25
-
8/12/2019 IMCI Chart Booklet Trytry
51/80
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
52/80
% Ad'ise the Mother to #n+rease Fl&id .&ring #llnessFO- AN% S# K H#/.
% If child breastfed* breastfeed more freHuently and for longer at each feed) If child is taking breastmilk substitutes* increase the amountof milk given
% Increase other fluids) For eAam#le* give soft #orridge* amasi* """ or clean ater)
FO- H#/. W#TH .#A--HOEA
% 0iving eAtra fluid can be lifesaving) 0ive fluid according to Plan ' or Plan B .#)34/
% Ad'ise the Mother When to -et&rn to Health Wor er FO//OW)UP :#S#T
'dvise the mother to come for follo @u# at the earliest timelisted for the child&s #roblems)
#! the +hild has -et&rn !or!ollo() & in
P + 2(I'D%"+ T+$%
1day
P+$"I"T+ T
DI'$$,(+' C,$( IC+'$ I F+CTI(F++DI 0 P$(BL+2!,++G+ .FI$"T +PI"(D+/* if stillhee in ' % (T,+$ ILL +""* if not
4day
s
' '+2I' 36 days
(T 0$(!I 0 !+LL @ but no feeding #roblem 36 days
" "P+CT+D "%2PT(2'TIC ,I;"%2PT(2'TIC ,I; .confirmed/
36days
-
8/12/2019 IMCI Chart Booklet Trytry
53/80
WHEN TO -ETU-N #MME.#ATE/%
Ad'ise $other to ret&rn i$$ediatel" i! the +hild has an" o! these signs
'ny sick child Becomes sicker ot able to drink or breastfeed ;omiting everything Develo s a fever
If child has C( 0, ($ C(LD*return if:
Fast breathing Difficult breathing !hee ing
If child has Diarrhoea* return if: Blood in stool
NE T WE//) H#/. :#S#T 'dvise mother hen to return for neAt immunisationaccording to immunisation schedule) +ncouragemonthly visits for gro th monitoring
!hen to return
Counsel the mother G I2CI guideline
"e#tember 1 126
-
8/12/2019 IMCI Chart Booklet Trytry
54/80
% o&nsel the $other A3o&t Her O(n Health
% If the mother is sick* #rovide care for her* or refer her for hel#)
% If she has a breast #roblem .such as engorgement* sore ni##les* breast infection/* #rovide care for her or refer her for hel# .#)54/)
% 'dvise her to eat ell to kee# u# her o n strength and health)
% Check the mother&s immunisation status and give her tetanus toAoid if needed)
% 2ake sure she has access to:
- Family #lanning
- Counselling on "TD and 'ID" #revention% +ncourage mother to s#eak about social #roblems
% If the mother is ,I; #ositive give her advice about her o n health and consider starting her on co@trimoAa ole
-EMEM9E- THAT THE HEA/TH OF A H#/. .EPEN.S ON THE HEA/TH OF THE MOTHE-6
A/WA%S TH#NK OF THE MOTHE-S HEA/TH WHEN %OU A-E A-#NG FO- A S# K H#/.
2others health Counsel the mother
2
-
8/12/2019 IMCI Chart Booklet Trytry
55/80
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
56/80
ASSESS, /ASS#F% AN. T-EAT THE S# K %OUNG #NFANTAGE 1 WEEK UP TO 2 MONTHS
.O A -AP#. AP-A#SA/ OF A// WA#T#NG H#/.-ENASK THE MOTHE- WHAT THE %OUNG #NFANTDS P-O9/EMS A-E Determine if this is an initial or follo @u# visit for this #roblem)
- if follo @u# visit* use the follo @u# instructions on #age 5/
% Check mothers health% Counsel about general hygiene and care% If mother is ,I; #ositive give a##ro#riate
feeding advice and start the baby on co@trimoAa ole from the age of 8 eeks .#)>/
(
Possible Bacterial Infection 2" 'ssess and classify: The %oung Infant
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
58/80
T o of the follo ingsigns:
Lethargic orunconscious
"unken eyes "kin #inch goes
back very slo ly)
.#A--HOEA W#THSE:E-E.EH%.-AT#ON
%
%
%
%
-e!er U-GENT/% to hos*ital(ith intra'eno&s in!&sion 5see*lan *61; 86Gi'e the !irst dose o!+e!tria one #M# 5*6778Gi'e !re@&ent si*s o! O-S onthe ( a", i ! *os si3le6
9reast!eeding +an +ontin&eKee the +hildT o of the follo ingsigns:
$estless* irritable "unken eyes "kin #inch goes
back slo ly)
0ive fluid for some dehydration
.#A--HOEAW#TH SOME.EH%.-AT#ON
%
%
B #)34 / 'dvise the mother to continue breastfeedingFollo u# in 1 days
ot enoughsigns to classifyas some orseveredehydration)
NO :#S#9/E.EH%.-AT#ON
%
% %
0ive fluids to treat fordiarrhoea at home .Plan '#)34/Follo u# in 1 days)If eAclusively breastfed donot other fluids eAce#t """
give
.oes the "o&ng in!ant ha'e diarrhoea4
#F %ES, ASK :
For ho long?
Is there bloodin the stool?
/OOK AN. FEE/
Look at the young infant&s generalcondition) Is the infant:
@Lethargic or unconscious?@$estless and irritable?
Look for sunken eyes)
Pinch the skin of theabdomen) Does it go back:
@;ery slo ly .longer than 1seconds/?@or "lo ly?
!or.EH%.-AT#ON
lassi!".#A--HOEA
-
8/12/2019 IMCI Chart Booklet Trytry
59/80
and i! diarrhoea1= da"s or
$ore
J Diarrhoea lasting36 days or more)
SE:E-E PE-S#STENT.#A--HOEA
% -EFE- and treat for dehydration if#resent)
% ee# the baby arm on the ay tohos#ital)
Blood in the stool)Y
POSS#9/ESE-#OUS A9.OM#NA/P-O9/EM
% -e!er U-GENT/% to hos*ital% Kee* (ar$ on the (a" to hos*ital
and i! 3lood instool
Diarrhoea 'ssess and classify: The %oung Infant
G I2CI guideline "e#tember 1 1
2$
-
8/12/2019 IMCI Chart Booklet Trytry
60/80
THEN HE K FO- FEE.#NG P-O9/EM O-/OW WE#GHT #N 9-EASTFE. 9A9#ES
ot able to feed or NOT A9/E TOFEE.
% Gi'e !irst dose o! +e!tria one #M# 5*6778
% he+ 3lood s&gar then treat or ASK : ,
o
ar
eyoufeedingthebab
y? ,
o
isfeedinggoing?
,o
manytimes
do you
br eastf eed in 16 hour s?
!hat f oods and f l
uidsinadditio
ntobr eastmilkar eyougivingtobaby?@if yeshooften?@ ho is itgiven?@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@ @@@@ @
LO O K , LI S T E N ,F E E L:
Plotthe
eighton the $
T,C to deter m
ine th
e
eight f or age)
Look f or
h
ite #atches i
-
8/12/2019 IMCI Chart Booklet Trytry
61/80
n themouth.thrush/
) ) ) ) ) ) ) ) ) ) ) )) ) ) ) ) ) ) ) ) ) ) )) ) ) ) ) )
lassi!"FEE.#NG
o attachment at all or
ot
suckling at all)
ot
ell
attachedtobr eastor
otsucklinge
ff ectivelyor
*re'entlo(3loods&gar65*61= 8
%Ad'isethe$otherho(to
ee*the"o&ngin!ant(ar $onthe
(a"tothe hos*ital6
% -e!erU-GEN
T/
% to hos*ital6
% 'dvise th
e m
other to br eastf eed as of ten
an
\
ched or not suckling ef f ectivel
y*teach cor r ect#ositioning and
#FAN #NFANT
Hasan"di! !i+<"! eeding,O
+6T$$7$%:
-touchingreast -open-turneoutwar -visi le a ovethan elowthe mouth
.'llsignsshould be#resent iftheattachmentis good)/
Is
the inf ant a
ble to attach?
no attachmentat all not wellattache gooattachment
Is
the
infa
nt
suc
klin
g
effe
ctiv
ely
.tha
t is*
slo
dee
#
sucks*
so
met
ime
s
#au
it
h
sali
ne
dro
#s
if it
int
erf
ere
s
it
h
bre
ast
fee
din
g)
2othereA#eri
encing#r oblemsf e
edingor
Lessthan
-
8/12/2019 IMCI Chart Booklet Trytry
62/80
attachment)\ If breastfeeding less than
< times in 16 hours*advise to increasefreHuency of feeding)
@ If moth er h as abreastfeeding #roblemsee advice for commonbreastfeeding #roblems.#)54/
% If receiving other foodsor drinks* counselmother aboutbreastfeeding more*reducing other foods ordrinks* and using acu#)
% If thrush* teach themother to treat for thrush at home) .#) 56/
% 'dvise mother to give homecare for the young infant)
.#)59/
%Follo
@u# any f e
eding #r oblem orthr ush i
n 1 days)
% Follo @u#lo eight forage in 9 days)
% 'dvisemother togivehomecare forthe younginfant) .#)59/
% Praisethemotherforfeedingthe infantell)
Use this *age to assess !eeding i! the in!ant isre+ei'ing an) 3reast$il
Feeding#roblem=breastfedinfants
3% 'ssess andclassify: The%oung Infant
-
8/12/2019 IMCI Chart Booklet Trytry
63/80
THEN HE K FO- FEE.#NG P-O9/EM O-/OW WE#GHT #N 9A9#ES -E E#:#NG NO9-EASTM#/K
ot able to feed or
ot sucking at all)
NOT A9/E TOFEE. )
% Treat as *ossi3le se'ere 3a+terial in!e+tion 5*62B8
% Gi'e !irst dose o! +e!tria one #M# 5*6778
% -e!er U-GENT/% to hos*ital
A LOOK,
LISTEN,FEEL:
,o
ar e you f eeding the baby?
,o
isfeedin
g going?
!h
at made you decide not to b
reastfeedV?
!hatmilk
ar eyougiving?
,o
manytimesduringthedayandnigh
t?
,o
muchi
sgivenateachf e
ed?
,o
ar eyou
#r e#ar ing the milk?
@
rateoreA#lainho
afeedis#r e#ar ed*and
ho
itisgiventotheb
-
8/12/2019 IMCI Chart Booklet Trytry
64/80
aby
!hat foodsand fluids inaddition tore#lacementmilk isgiven?
,o is themilk beinggiven? Cu#or bottle
,o are youcleaning theutensils?
Plot theeight onthe $T,Cto determinetheeight forage)
Look forulcers orhite#atches inthe mouth.thrush/)
lassi!"FEE.#NG
2ilkincorrectly or unhygienically#re#ared or
0ivingina##ro#riate re#lacementmilk orother foods fluids or
0ivinginsufficient
re#lacementfeedsor
sing afeedingbottle or
Thrush.ulcer
s orhite #atches inthemouth/ or
Loeightfor ageor
!eight gai
n is unsatisf act
or y
otlo
eightforageand noothersignsof inad
eHuate feeding)
FEE.#NG P-O9/EM O- NOT G-OW#NG WE//
NO F
EE.#NG P-O9/EM
% Counsela
boutf eeding
%+A#lain guidelines f orsaf e r e#lac
ementfeeding.#)58/
%Ide
ntif ymothersandfamily&sconcer nsaboutfeeding)"uggestthatmother gr aduallydecreasestheamountoffoodor fluidsoth
erthanmilkbeinggiven
%
'dvisethemothertouse acu#ratherthanbottletofeedthebabyandshoher ho
todothis.#)58/
% Ifthr ush*teach
the mother to tr eat f or thr ush at home .#)56/
%Follo
@u#any
f eeding #r oblem
in1days
%Fol
lo
u#in%
'dvisemothertocontinuefe
eding*andensur egoodhygiene%Pr ais
e the mother
NOTE
A +hild
$a" not 3e
3r east! ed 3e+a&se the
$other is H#
: in! e+ted6
-
8/12/2019 IMCI Chart Booklet Trytry
65/80
#!thisisnotthereason,+onsiderrest
ar ting3r east!eeding
orre!err altoa3r east
! eeding +o&nsellor i!
a'aila3le
F
e 's
-
8/12/2019 IMCI Chart Booklet Trytry
66/80
THEN CHECK I THE !O"N# IN $NT H$% $N! %&ECI$' (I%K $CTO(%
I% the infant as #remature or lo birtheight
% there as birth as#hyAia% the infant is not breastfed% the mother is a young adolescent% the mother is kno n to be ,I; #ositive% there is severe socioeconomic de#rivation 2 This infant is at high risk and s#ecial care should be taken to ensurethat there are no feeding #roblems and the child is gaining eight ell) 'rrange a##ro#riate regular follo @u# ith the mother
$efer to an a##ro#riate su##ort grou# if #ossible)
THEN HE K THE %OUNG #NFANTDS #MMUN#SAT#ON STATUS
#MMUN#SAT#ON S HE.U/E
A GE
Birth8 eeks3eeks
: A #NE
BC0 DPT ,IB@3DPT ,IB@1
(P;@(P;@3(P
,e# B3,e# B1
:#T AM#N A
1 I to the mother at delivery4 I for infants at 8 eeks if not 3reast!ed
% Gi'e all $issed doses on this 'isit6% Include sick babies and those ithout a
$T,C% If the child has no $T,C* issue a ne one
to@day)% 'dvise the caretaker hen to return for the
neAt dose)
ASSESS OTHE- P-O9/EMS
-
8/12/2019 IMCI Chart Booklet Trytry
67/80
ASSESS THE MOTHE-DS HEA/TH NEE.Seg6 N&tritional stat&s and anae$ia, +ontra+e*tion et+6 he+ h"giene *ra+tises
"#ecial risk factors Immunisationstatus
'ssess and classify %oung Infant
G I2CI guideline "e#tember 1 1
32
-
8/12/2019 IMCI Chart Booklet Trytry
68/80
T-EAT THE %OUNG #NFANT% Treat /O A/ 9A TE-#A/ #NFE T#ON (ith Er"thro$"+in s"r&*
E(!TH(O)!CIN %!("&% ive (hree (i.es dail4 for seve da4s
AGE or WE#GHT +rythromycin"yru#
Birth u# to 3 month .N 5 kg/ 3)14 ml
3 month u# to 1 months .5@6kg/ 1)4 ml
% Treat POSS#9/E SE-#OUS 9A TE-#A/ #NFE T#ON (ith #ntra$&s+&lar e!tria one% 0ive first dose of CeftriaAone I2I before the infant is referred urgently) 0ive a single dose of cetfriaAone to an infant ith #us draining from the
eye
EFT-#A ONE #NIE T#ON
WE#GHT e!tria one14 mg in 3ml
1 @5 kg )4 ml
O5 @ 8 kg 3 ml
% The dose of CefriaAone is 4 mg #er kilogram
% Dilute 14 mg vial ith 3ml of sterile ater
-
8/12/2019 IMCI Chart Booklet Trytry
69/80
'ntibioticsTreat the young infant33
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
70/80
T-EAT THE %OUNG #NFANT
%To Treat !or .iarrhoea, See T-EAT THE H#/., *610)1;If there is DI'$$,(+' !IT, "+;+$+ D+,%D$'TI( or DI'$$,(+' !IT, "(2+ D+,%D$'TI( .#)34@38/)If there is ]severe dehydration^ commence intravenous rehydration* give the f irst dose of ceftriaAone I2I .#)55/ and $+F+$ urgently)
%#$$&nise E'er" Si+ %o&ng #n!ant, as Needed6
%Tea+h the Mother to treat /o+al #n!e+tionsAt ho$e
% +A#lain ho the treatment is given)
% !atch her as she does the first treatment in the clinic)
% Treat !or E"e #n!e+tion (ith hlora$*heni+ol E"e Oint$ent
\ The mother should ash hands before and after treatment
% "he should return to the clinic if the infectionorsens)
The eyes must be cleaned ith a clean cloth then Chloram#henicol or tetracycline eye ointment is instilled inside the
lo er eyelid
Four times#er day
% To Treat !or S in P&st&les or U$3ili+al #n!e+tion
The mother should do the treatment t ice daily:% !ash hands% 0ently ash off #us and crusts ith soa# and ater % Dry the area% Paint ith #olyvidone iodine lotion or gentian violet% !ash hands
% Treat !or Thr&sh (ith N"statin or Gentian :ioletThe mother should:
% !ash hands% !ash mouth ith clean soft cloth ra##ed around the finger and et ith salt
ater % 0ive nystatin 3 ml 6 times a day or #aint ith diluted )4 gentian violet% !ash hands% 'dvise the mother on breast care% Check bottle or other utensil in use for hygiene)
Diarrhoea Local infections at home Treat the
young infant G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
71/80
young infant G I2CI guideline e#tember 1 1
3&
OUNSE/ THE MOTHE
-
8/12/2019 IMCI Chart Booklet Trytry
72/80
OUNSE/ THE MOTHE-
% Tea+h orre+t Positioning and Atta+h$ent !or 9reast!eeding% the mother must be seated comfortably
% "ho the mother ho to hold her infant- ith the infant&s head and body straight
- facing her breast* ith infant&s nose o##osite her ni##le- ith infant&s body close to her body
- su##orting infant&s hole body* not ust neck and shoulders)% "ho her ho to hel# the infant to attach) "he should:
- touch her infant&s li#s ith her ni##le- ait until her infant&s mouth is o#ening ide
- move her infant Huickly onto her breast* aiming the infant&s lo er li# ell belo the ni##le)% Look for signs of good attachment and effective suckling) If the attachment or suckling is not good* try again)
% 2ost of the common breastfeeding #roblems eA#ressed by mothers are related to #oor #ositioning and attachment .see belo /
OMMON 9-EAST FEE.#NG P-O9/EMS
JNOT ENOUGH M#/KThe commonest reason hy mothers add other feeds early orsto# breastfeeding) sually the mother has enough milk butlacks confidence that it is enough)
Wh" does the $other thin the 3a3" is not getting eno&gh$il 4 The baby may cry a lot* or ant to feed often and for along time* or her breasts do not feel very full) "he may havetried giving a formula feed and noticed that the baby sle#t forlonger after ards)
.oes she gi'e the 3a3" an" other !ood or !l&ids4 This illreduce breast milk #roduction but if she breastfeeds more thereill be more milk) 'dvise her to gradually sto# giving otherfoods or fluids and increase the number of breastfeeds) "heshould breastfeed as often as the child ants* at least eighttimes in 16 hours both day and night)
he+ *osition and atta+h$ent @ if the baby is not ell at@tached* he may not be getting enough milk and ant to feedoften and for a long time)
If the baby is gro ing ell you can reassure the mother thatshe has enough milk and the baby is getting enough food)
SO-E O- -A KE.N#PP/ESSore ni**les are +a&sed 3" *oor atta+h$ent d&ring s&+ )ling and can lead to breastfeeding failure if it is so #ainful thatthe mother is reluctant to feed) The baby is not getting muchmilk and ants to feed more often) Breastfeeding should notbe #ainful) ' #oorly attached infant is suckling on the sensi@tive ni##le rather than taking the hole breast in the mouth)!hen you re#osition the infant so that it is ell attached thereis immediate relief and the baby begins to suckle effectively)
If the #oorly attached baby continues to suck* cracks may de@velo# in the ni##le) 's you im#rove attachment* the #ain isless and the mother may continue to breastfeed as the cracksheal) If the #ain is too severe* eA#ress breastmilk until the ni#@#le has healed and feed the baby from the other breast or itheA#ressed milk in a cu#) Putting a dro# of hindmilk on the ni#@#le after feeding ill also hel# healing)
"oreness may also be caused by thrush infection* #articularlyif #ain develo#s after a #eriod of #ain free feeding) Treat boththe mother and baby ith nystatin dro#s or cream)
THE 9A9% FEE.S OFTEN or-#ES A /OT
This may be because the infant is #oorly attachedand not suckling effectively so that he is Huicklyhungry again)
'ssess breastfeeding* check the #ositioningand attachment and advise the mother
If the baby is feeding often or the mother thinksthe child is more settled after a formula feed* thismay be because the feeding #attern is different ina formula fed baby* not because the child is hun@gry) Breastfed infants may feed more often andalso suckle for comfort)
Formula milk is more difficult for the baby to digesthich makes the interval bet een feeds longerbut this does not mean it is better for the baby)
35G I2CI guideline
"e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
73/80
e#tember 1 1
OUNSE/ THE MOTHE
-
8/12/2019 IMCI Chart Booklet Trytry
74/80
OUNSE/ THE MOTHE-
%%afe &re*aration of ormula )il+
Al a4s 0se a .arked c0p or7lass a d spoo (o .eas0re a(er a d (he scoop (o
.eas- 0re (he for.0la po der'
!ash 4o0r ha ds before pre- pari 7 a feed
8ri 7 (he a(er (o (he boil a d(he le( i( cool' eep i( cov- ered hile i( cools'
9eas0re (he for.0la po deri (o a .arked c0p or 7lass'9ake (he scoops level':0( i o e scoops for ever425 .ls of a(er'
Add a s.all a.o0 ( of (he cooled boiled a(er a d s(ir' Fill (he c0p or 7lass (o (he .ark i(h (he a(er' ;(ir ell'
Feed (he bab4 0si 7 a c0p'
!ash (he 0(e sils'
%Ho( to !eed a 3a3" (ith a +&*
% ,old the baby sitting u#right or semi@u#right on your la#
% ,old a small cu# of milk to the baby&s li#s- ti# the cu# so the milk ust touches the baby&s li#s- the cu# rests gently on the baby&s lo er li# and the edges of the cu# and
touch the outer #art of the baby&s u##er li#- the baby becomes alert and o#ens his mouth and eyes
% Do not #our the milk into the baby&s mouth) [ust hold the cu# to his li#s andlet him take it himself
% !hen the baby has had enough he closes his mouth and ill not take anymore
%A**ro i$ate a$o&nt o! !or$&la needed *er da"
'geinmon
!eight inkilos
'##roA) amountof formula in 16hours
Previously boiledater #er
umberof
scoo#s
'##roA)num@ berof feeds
-
8/12/2019 IMCI Chart Booklet Trytry
75/80
Breastfeeding!hen to return
36Counsel the mother
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
76/80
%Ad'ise Mother to Gi'e Ho$e are !or the %o&ng #n!ant1' F/U#.S Breastfeed freHuently* as often and for as long as the infantants* day or night* during sickness and health)
2' WHEN TO -ETU-N#! the in!ant has -et&rn !or !ollo()&* in
L(C'L B'CT+$I'LI @ F+CTI(
' % F++DI 0P$(BL+2
T,$ ",
( _`ab
L(! !+I0,T F($ '0+ T _`ab
Follo()&* :isit
When to -et&rn #$$ediatel" :
Ad'ise the +areta er to ret&rn i$$ediatel"i! the "o&ng in!ant has an" o! these signs
76 MAKE SU-E THAT THE %OUNG #NFANT #S KEPT WA-M AT A// T#MES6In cool eather cover the infant&s head and feet and dress the infant ith eAtraclothing)
% Breastfeeding #oorly or drinking #oorly% Becomes sicker% Develo#s afever % Fastbreathing% Difficult breathing% Blood in stool% ;omits everything% Irri tab le orlethargic %
Convulsions
-
8/12/2019 IMCI Chart Booklet Trytry
77/80
G I2CI guideline "e#tember 1 1
3
-
8/12/2019 IMCI Chart Booklet Trytry
78/80
G#:E FO//OW)UP A-E FO- THE S# K %OUNG #NFANTIf there is a ne #roblem@ assess* classify and treat the ne #roblem as on the '""+"" ' D CL'""IF% chart
%LOCAL *ACTERIAL INFECTION
'fter 1 days:Look at the umbilicus) Is it red or draining #us? Does redness eAtend to theskin? Look at the skin #ustules) 're there many or severe #ustules?Look at the #us draining from the eye) ,as the eye im#roved? Is there less #us draining?
Treatment:% If+ondition re$ains the sa$e or is (orse * refer to hos#ital)
% If+ondition is i$*ro'ed * tell the mother to continue giving the 4 days of antibiotic and continue treating for the local infection at home)
% THRUSH
'fter 1 days:Look for hite #atches in the mouth .thrush/)$eassess feeding) O "ee ]Then Check for Feeding Problem or Lo !eight^ above .#) 5 /)
% If thr&sh is (orse check that treatment is being given correctly* consider ,I; .#)9/
% If the infant has *ro3le$s (ith atta+h$ent or s&+ ling * refer to hos#ital)
% If thrush is the same or better* and the baby is feeding ell * continue ith nystatin .or gentian violet/ for a total of 4 days)
Local bacterialinfection ThrushF ollo u# care
G I2CI guideline "e#tember 1 1
3"
-
8/12/2019 IMCI Chart Booklet Trytry
79/80
G#:E FO//OW)UP A-E FO- THE S# K %OUNG #NFANT% FEE.#NG P-O9/EM
'fter 1 days: $eassess feeding #)5
'sk about any feeding #roblems found on the initial visit)% Counsel the mother about any ne or continuing feeding #roblems) If you counsel the mother to make significant changes
in feeding* ask her to bring the young infant back again after 4 days)
% If the young infant is lo eight for age* ask the mother to return after a further 4 days after the initial visit to measure theyoung infant&s eight gain) Continue follo @u# until the infant is gaining eight ell)
% if the young infant has lost (eight * $+F+$ the child)
E#!ept$%n:If you do not think that feeding ill im#rove* refer the child)
% NOT G-OW#NG WE// 'fter 9 days:!eigh the young infant and determine if the infant is still lo eight for age) $eassess feeding) "ee ]Then Check for Feeding Problem or Lo !eight^ above)
% If the infant is no longer lo( (eight !or age * #raise the mother and encourage her to continue)
% If the infant is still lo( (eight !or age, 3&t is gaining (eight * #raise the mother) 'sk her to have her infant eighed again ithin36 days or hen she returns for immunisation)* hichever is the earlier)
% If the infant is still lo( (eight !or age and has not gained (eight $+F+$)
E#!ept$%n:
If you do not think that feeding ill im#rove* or if the young infant has lost (eight * refer to hos#ital)
Feeding#roblem Loeight Follo u#care
G I2CI guideline "e#tember 1 1
-
8/12/2019 IMCI Chart Booklet Trytry
80/80
3$