Glycemic Control Coaching Call - NYS Partnership for … partnership of the Healthcare Association...
Transcript of Glycemic Control Coaching Call - NYS Partnership for … partnership of the Healthcare Association...
A partnership of the Healthcare Association of New York State and the Greater New York Hospital Association
Glycemic Control Coaching Call
June 21, 2016
NYS PARTNERSHIP FOR PATIENTS
Agenda
2
Topic Speaker
Welcome and Introduction Cathleen Wright NYSPFP
Outpatient DM Medication
Thérèse Franco, MD, FHM Virginia Mason Medical Center
Seattle, WA
Naina Sinha, MD Assistant Professor of Medicine
Division of Endocrinology, Diabetes & Metabolism Weill Cornell Medical College
New York, NY
Next Steps and Q&A Alissa Beers NYSPFP
NYS PARTNERSHIP FOR PATIENTS
Glycemic Management Resources
3
o Webinar 4- September 13, 2015 from 12 – 1 pm
o Society for Hospital Medicine Glycemic ControlCommunity
o NYSPFP Project Manager
o NYSPFP Website
NYS PARTNERSHIP FOR PATIENTS
Glycemic Control Conference Agenda
July 22, 2016 4
Topic Presenter
Improving Glycemic Control in Non-Critical Care Units
Society for Hospital Medicine Faculty
Improving Glycemic Control in Critical Care Units
Hardwiring Glycemic Control Practices
Special Situations
Hypoglycemia Society for Hospital Medicine Faculty
Role of Glycemic Control Program in the Hospital
Transition out of the Hospital
Patient and Professional Education
NYS PARTNERSHIP FOR PATIENTS
Questions for Audience
5
o What have you implemented since attending thein-person Glycemic Control conference?
o What, if any, challenges are you experiencing inimplementing changes to your GlycemicManagement Program/protocols?
o What, if any, questions do you have relative tothe Glycemic Control conference topics?
7
Presenters
Thérèse Franco, MD, FHM Virginia Mason Medical Center Seattle, WA
Naina Sinha, MD Assistant Professor of Medicine Division of Endocrinology, Diabetes & Metabolism Weill Cornell Medical College New York, NY
8
Type 1 vs Type 2 Diabetes
Type 1 • Autoimmune disease• β-cell destruction
• Little or no insulinproduction
• Ketosis prone
Treatment: • Lifestyle Changes• Insulin Dependence
Type 2 • Insulin resistance &• Insulin deficiency &• Gut hormone GLP-1
deficiency & GIP resistance
• weight, BP & LDLcommon
Treatment: • Lifestyle Changes• Oral agents, GLP-1 RAs• May Require insulin
9
Glu
cose
(m
g/dL
)
Diabetes diagnosis
50
100
150
200
250
300
350
Fasting glucose
Kendall DM, Cuddihy, RM, Bergenstal RM © 2009 International Diabetes Center. All rights reserved
Years
Rel
ativ
e am
ount
-10 -5 0 5 10 15 20 25 30
Insulin resistance
Insulin level
Onset Diabetes
Pre Diabetes (IFG, IGT)
0
50
100
150
200
250
-15
Natural History of T2DM
Postmeal Glucose
10
peripheral glucose uptake
hepatic glucose production
pancreatic insulin secretion
pancreatic glucagon secretion
Multiple Defects of T2DM
HYPERGLYCEMIA
− +
−
gut carbohydrate delivery & absorption
incretin effect
?
Renal Threshold
12
Targeted Sites of T2DM Meds ↑Insulin
SUs Meglitinides GLP-1, DPP-4 I
GLP-1, Amylin TZDs, Metformin
↓Glucagon
GLP-1, DPP-4 I Amylin
TZDs
SGLT-2 inhibitors
Metformin GLP1, TZDs
GLP-1, Amylin, AGIs
Defronzo RA. Diabetes;2009;58:773-795
↓HGP
↑Glu uptake
↓Glu reabsorption
Gl effects CNS effects
↓Lipotoxicity
Tahrani. AA. Lancet. 2011; 378:182-97
13
Glycemic Targets- ADA/EASD 2016 • HbA1c < 7.0% (mean PG ∼150-160 mg/dl)
Pre-prandial PG 80-130 mg/dl
Peak post-prandial PG <180 mg/dl
• Individualization is key:
Tighter targets (6.0 - 6.5%) - younger, healthier
Looser targets (7.5 - 8.0%+) - older, co-morbidities, hypoglycemia prone, etc.
• Avoidance of hypoglycemiaDiabetes Care 39: S43-44
14
Factors to Consider when Choosing Pharmacological Agents for Diabetes ►Current A1C
►Duration of diabetes
►Body weight (BMI, abdominal obesity)
►Age of patient
►Co-morbidities
►Risk of hypoglycemia
►Cost of medication
►Convenience/ complexity
15
Biguanides
• Metformin (Glucophage®)• Metformin XR (Glucophage XR®, Fortamet®,
Glumetza®)• Metformin liquid (Riomet®)
16
Biguanides Metformin Mechanism ↓ hepatic glucose production
↑ insulin sensitivity Efficacy ↓ A1c 1.5%
Advantages ↓ CV risk (UKPDS), ↓ IGT -> T2DM (DPP) no hypos ↓ appetite- possible wt loss ↓ cancer risk $ generic
Disadvantages GI s/e Lactic acidosis (very rare) B12 def
Contraindications Impaired renal fx (eGFR <30) excessive ETOH, CHF Hold 48 hrs pre/post contrast studies Caution in elderly (>80 yo)
18
TZDs Pioglitazone, Rosiglitazone
Mechanism ↑ Insulin sensitivity- ↓ resistance
Efficacy ↓ A1c 0.8-1.0% Advantages No hypos; durable
No renal excretion Beneficial lipid effects; + vasc effects (pio) ↓ insulin requirement
Disadvantages Slow onset Wt gain –sc, peripheral Fluid retention/edema- esp w/insulin Bladder CA risk- pio (?) Macular edema; fracture risk
Contraindications Black box-> may cause/exacerbate CHF; contraindicated NYHA Class III or IV CHF
19
Sulfonylureas
• Glimepiride (Amaryl®)• Glipizide (Glucotrol®, Glucotrol XL®)• Glyburide (Micronase®, Glynase®, DiaBeta®)
20
Sulfonylureas Glimepiride, Glipizide, Glyburide
Mechanism ↑ insulin secretion- long acting (12-24 hrs) - need functioning beta cells
Efficacy ↓ A1c 1-2% Advantages No lag time
Easy dosing $
Disadvantages Hypos (esp glyburide) Wt gain Low durability
Contraindications Caution if renal/hepatic disease Adjust dose in elderly Sulfa allergy
22
Glinides Repaglinide, Nateglinide
Mechanism ↑ insulin secretion- fast acting , short duration (onset 15-30 min; lasts 2-4 hrs) - need functioning beta cells ↓ PPG
Efficacy ↓ A1c 1- 1.5% Advantages Work quickly; short half life
Can titrate based on BG, carb content Safe at higher levels of Cr than SUs
Disadvantages Hypos, wt gain (less than SUs) Frequent dosing
Contraindications Caution if renal/hepatic disease Adjust dose in elderly
24
AGIs Acarbose, Miglitol
Mechanism Delays CHO absorption in small intestine ↓ PPG
Efficacy ↓ A1c 0.5- 0.8%
Advantages no wt gain no hypos Non-systemic- good CV safety
Disadvantages Flatulence, bloating, diarrhea Frequent dosing- with meals If used with insulin/secretogogue-> must treat hypos with glucose Limited efficacy
Contraindications Intestinal disorder Cirrhosis
25
Incretins- key points:
• GLP-1 and GIP- major incretin (gut) hormones• Involved in many aspects of glu metabolism• Effect diminished in T2DM• Released in response to food ingestion• Degraded by DPP-4• Possible β-cell preservation
26
GLP-1 Effects in Humans
Stomach: Helps regulate
gastric emptying
Promotes satiety and reduces appetite
Liver: ↓ Glucagon reduces
hepatic glucose output Beta cells: Enhances glucose-dependent
insulin secretion
Alpha cells: ↓ Postprandial
glucagon secretion
Secreted upon the ingestion of food
27
Nauck et al. Diabetologia. 1986
Incretin effect on insulin secretion
Oral glucose load Intravenous glucose infusion
Time (min) In
sulin
(mU
/l)
80
60
40
20
0 180 60 120 0
Time (min)
Insu
lin (m
U/l
)
80
60
40
20
0 180 60 120 0
Incretin effect
Control subjects (n=8) People with Type 2 diabetes (n=14)
28
GLP-1 enhancement GLP-1 secretion is impaired in T2DM
Natural GLP-1 has extremely short half-life
Add GLP-1 agonists with longer half-life: • exenatide• exenatide LAR• liraglutide• albiglutide• dulaglutide
Injectables
Block DPP-4, the enzyme that degrades GLP-1: • sitagliptin• saxagliptin• linagliptin• alogliptin
Oral agents
29
GLP-1 Receptor Agonists Exenatide (Byetta®)
Exenatide LAR (Budureon®)
Liraglutide (Victoza®)
Albiglutide (Tanzeum ®)
Dulaglutide (Trulicity®)
30
GLP-1 RA • Advantages
– Appetite suppression, wt loss– Glucose dependent insulin secretion– Low risk of hypos– Dosing- some weekly– CV benefit (Liraglutide- LEADER trial, 2016)
• Disadvantages/caution– s/e: nausea– Pancreatitis– Renal disease; contradindicated eGFR<30 (exenatide)– Gastroparesis– Black box: risk of MTC (medullary thyroid CA)– $$$
31
Exenatide (Byetta®) Exenatide LAR (Bydureon®)
• Exenatide- FDA -> 2005Exenatide LAR- FDA -> 2012
• Synthetic GLP-1 (53% homology)
32
Exenatide /Exenatide LAR
Exenatide- • monotherapy and w/metformin, TZD, SU, basal
insulin• Dose: 5 or 10 mcg SC bid within 60min of meal
Exenatide LAR • w/metformin, TZD, SU• Dose: 2 mg SC weekly independent of meals
33
Liraglutide (Victoza®)
• FDA -> 2010• Analog of human GLP-1 (97% homology)• monotherapy and w/ metformin, TZD, SU, basal
insulin• Once daily, independent of meals• Dose: start 0.6mg SC qd x1wk, then 1.2 mg; can
titrate to 1.8 mg• Saxenda® - FDA-> 12/14; wt loss; 3 mg/day• IDegLira – insulin degludec + liraglutide
34
Other GLP-1 RA
Albiglutide (Tanzeum®) • FDA-> 4/14• Dose: 30 mg or 50 mg weekly• Mixing, wait required• OK w/ basal insulin
Dulaglutide (Trulicity®) • FDA-> 9/14• Dose: 0.75 mg or 1.5 mg weekly• Autoinjector
35
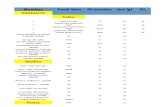
GLP-1 RA Drug Dose Dosing
schedule Mixing Needles
Byetta® (exenatide)
5 mcg 10 mcg
Twice daily within 60 min of meal
No Not included (32 g 4mm)
Bydureon® (exenatide LAR)
2 mg Weekly Yes 23 g, 7 mm
Tanzeum® (albiglutide)
30 mg 50 mg
Weekly Yes 29 g, 5 mm
Trulicity® (dulaglutide)
0.75 mg 1.5 mg
Weekly No 29 g, 5 mm Built in
Victoza® (liraglutide)
0.6, 1.2, 1.8 mg
Daily No Not included (32 g 4 mm)
36
Kieffer TJ, Habener JF. Endocr Rev. 1999;20:876-913 Deacon CF et al. Diabetes. 1995;44:1126-1131
DPP-4 Inhibitors
GLP-1 actions
Mixed meal
GLP-1 active
Plasma
Intestinal GLP-1 release
GLP-1 inactive
DPP-IV
Rapid inactivation (>80% of pool)
Renal clearance
X
37
DPP- 4 inhibitors
• Sitagliptin (Januvia®) – FDA->10/06• Saxagliptin (Onglyza®) - FDA -> 7/09• Linagliptin (Tradjenta®) - FDA -> 5/11• Alogliptin (Nesina®) – FDA-> 1/13
38
DPP-4 Inhibitors Sitagliptin, Saxagliptin, Linagliptin, Alogliptin
Mechanism Slows breakdown of incretin hormones -> ↑ glucose dep insulin secretion -> ↓ glucagon secretion
Efficacy ↓ A1c 0.5- 0.9%
Advantages Oral, easy dosing, well tolerated Wt neutral No hypos No renal contraindication
Disadvantages S/E: URI sxs, nasopharyngitis, H/A Pancreatitis Saxagliptin- CHF ?potential to interfere with immune fx $$$
Contraindications Hypersensitivity to individual meds
39
DPP- 4 Inhibitors Name Max dose Renal dosing
Januvia® (sitagliptin)
100 mg daily 25-50 mg daily
Onglyza® (saxagliptin)
5 mg daily 2.5 mg daily
Tradjenta® (linagliptin)
5 mg daily Same dose
Alogliptin® (nesina)
25 mg daily 6.25-12.5 mg daily
40
1. DeFronzo RA, et al. Curr Med Res Opin 2008; 24:2943-29522. Drucker DJ and Nauck MA. Lancet. 2006;368:1696-1705
Properties/EffectGLP-1 Receptor
Agonists1,2DPP-4
Inhibitors1,2
Glu dep insulin production +++ ++
Glu dep decrease in glucagon +++ +
Gastric emptying Delayed No effect
Food intake No effect
Body Weight Neutral
Hypoglycemia No No
Side effects N/V Minimal
Administration SC 1 or 2x/day or weekly
Oral Daily
Incretin Therapies: Major Differences
42
SGLT-2 inhibitors
• Canagliflozin (Invokana)- FDA -> 3/13• Dapagliflozin (Farxiga)- FDA -> 1/14• Empagliflozin (Jardiance)- FDA -> 8/14
43
SGLT-2 inhibitors Canagliflozin, Dapagliflozin, Empagliflozin
Mechanism ↑ Urinary excretion of glucose
Efficacy ↓ A1c 0.7-1 %
Advantages Oral, easy dosing Wt loss Possible BP lowering CV benefit (empagliflozin)
Disadvantages UTI; genital infections Hypotension; hyperkalemia Increased calcium excretion DKA
Contraindications eGFR <45 , <60 (Dapagliflozin)
44
SGLT2 Inhibitors and DKA
• 5/15/15 FDA issued warning• 20 cases reported from May 2013 to June
2014 • Euglycemic• ~50% had RF for DKA: eg acute illness,
infection, ↓ insulin dose• Median time to onset after initiation-> 2 wks• Pt education important!
Rosenstock. Euglycemic DKA A Predictable, Detectable, and Preventable Safety Concern With SGLT2 Inhibitors. Diabetes Care. 2015 Sep; 38(9): 1638-1642.
45
Human & Analog Insulins in US
Adapted from American Diabetes Association. Diabetes in the Latino Population. Available at: http://www.diabetes.org/uedocuments/LatinoSlidesAugust05.ppt.
0 2 4 6 8 10 12 14 16 18 20 22 24
Plas
ma
Insu
lin L
evel
s
Regular: up to 8 hours
NPH: up to 12 hours
Hours
-U100 glargine: 20–26 hrs -U 300 glargine: up to 36 hrs
-U 100 & U200 degludec: up to 42 hours
aspart, lispro, glulisine: up to 4 hours
-U100 detemir: up to 24 hours
46
Basal/ Bolus Insulin Therapy
Bolus Bolus Bolus
Basal: detemir/ degludec/ glargine
Bolus: aspart/ lispro/ glulisine
B L D Bedtime
Insu
lin E
ffect
B = breakfast L = lunch D = dinner
47
B D L Bedtime
Insu
lin E
ffect
Pre-Mix Insulin: Ex. of Twice Daily Dosing
B = breakfast L = lunch D = dinner
48
Some Newer Insulin Pens TRESIBA U100 & U200 U500 PEN:
COMING SOON
Humulin N (NPH) KwikPen
U300 Toujeo
U200 Humalog
49
Current Concentrations of Insulin in the U.S.
• U-100 = 100 units/ml• U-200 = 200 units/ml• U-300 = 300 units/ml• U-500 = 500 units/ml
51
Transitions Between Hospital and Home
Diet? Activity level? Oral Agents? Non-insulin injectables?
Insulin?
Carb controlled meal plan,
taken off oral agents & placed on basal/bolus insulin
therapy
Diet? Activity level? Oral Agents? Non-insulin injectables?
Insulin? Follow Up Plan?
Prior to Discharge: Consider A1C, New co-morbidities,
and New contraindications
52
Consider the following at transition:
• If you are admitting someone with pancreatitis, checkthe medication list for incretin therapy, either a DPP-4inhibitor or GLP-1 RA.
• Consider masked, or “euglycemic” DKA in patientson an SGLT-2 inhibitor, particularly in type 1 patients
• At hospital discharge, comorbid conditions are a bigdriver of tailored therapy:
– Renal Insufficiency, with eGFR <30, limits your options significantly:• Safe, high potency options are insulin and thiazolidinediones• Safe, intermediate potency option is a DPP4 Inhibitor
– For heart failure patients, some meds should be avoided: Metformin(biguanide), Thiazodinediones, Saxagliptin (GLP-1 RA)
– For hepatic insufficiency, some meds should be avoided: Sulfonylureas,Glinides, Alpha-glucosidase inhibitors
53
Effective Hospital Discharge:
• Individualized inpatient diabetes self-management education• Mutually agreed upon discharge plan• Clear diabetes-specific instructions that are given to patient
and available to the next provider (PCP)
Rubin, D. Hospital Readmissions of Patients with Diabetes. Current Diabetes Reports, 2015. 15(4): p. 1-9.
55
Pre-Mix Insulins: Beware of “look-alike sound-alikes”
• Humalog mix – 75/25® (75% lispro protamine/25%lispro) & 50/50 (50% lispro protamine/50% lispro)
• Novolog mix – 70/30® (70% aspart protamine/30%aspart)
Human mix: Novolin 70/30® & Humulin 70/30®
Coming Soon? Ryzodeg 70/30 (degludec + aspart)
55
Diabetes Care 2015;38:140 Diabetologia 2015;58:429-442
Basal Only
Basal Plus Pre-Mix
Basal/Bolus
How Many Shots a Day?
56
57
Initiating & Intensifying Insulin: Discharge Regimens to Consider
• Basal Alone: 1 shot/day
• Basal Plus: 2 shots/day
• Pre-Mix: 1-2 shots/day
• Basal-Bolus: 4 shots/day
58
NYP/Cornell Transition Guide To Home
A1c < 7% A1c 7-9% A1c > 9%
Return to same home regimen unless contraindicated
Restart home regimen if not contraindicated, keep basal at 50-100 % of inpatient dose
Best option: Basal insulin at 75-100% of current dose & bolus insulin with meals at fixed or calculated dose Other options: • Basal Plus (basal insulin + bolus
insulin at largest meal)• Pre-mixed insulin before breakfast &
dinner• Basal insulin once daily + repaglinide
with meals• Basal insulin once daily & GLP-1
injectable daily or weeklyBolus insulins: aspart, lispro, glulisine. Pre-Mixed insulins: 70/30, 75/25 & 50/50. Basal insulins: degludec U100 & U200, detemir, glargine U100 & U300.
Adapted with permission from algorithm by Umpierrez, G, Diabetes Care 2014
59
Common Diabetes PrescriptionsCommon Diabetes Prescriptions
Remember to Order Pen Needles with Pens & Syringes with Vials
Instructions BOLUS: NovoLog Flexpen® or Humalog KwikPen® Take (range, up to) units before meals BASAL: Lantus U100 or Toujeo U300 Solostar Pen® or Levemir or Tresiba U100 or U200 FlexTouch Pen® PREMIX: NovoLog Mix 70/30 Flexpen® or Humalog Mix 75/25 KwikPen® NPH: Humulin N Kwik Pen®
Take units at AM/PM OR Take units at AM and Take _____ units at PM
BD Nano or DUO (safety) pen needles DAW* Dispense #100 (or #200) use as directed, DAW* BD Ultrafine 6 mm 3/10 ml insulin syringe (Holds up to 30 units) DAW*
Dispense #100 (or #200) use as directed, DAW*
BD Ultrafine 6 mm 1/2 ml insulin syringe (Holds up to 50 units) DAW*
Dispense #100 (or #200) use as directed, DAW*
BD Ultrafine 6 mm 1 ml insulin syringe (Holds up to 100 units) DAW*
Dispense #100 (or #200) use as directed, DAW*
Accu-Chek Nano, Bayer Contour Next EZ , FreeStyle Freedom LITE OR OneTouch Ultra2 blood glucose meter Dispense: 1 meter
Accu-Chek Nano, Bayer Contour Next EZ , FreeStyle Freedom LITE OR OneTouch Ultra2 test strips Test BG x/day
Accu-Chek Nano, Bayer Contour Next EZ , FreeStyle Freedom LITE OR OneTouch Ultra2 lancets Test BG x/day
60
Inzucci et al. Diabetes Care 2015;38:140-149.
Approach to managementof hyperglycemia:
Patient attitude and expected treatment effortsexpected treat
Disease duration
Life expectancy
Important comorbidities
Established vascular complications
Resources, support system
Risks potentially associated wi th hypoglycemia, otheradverse events
more S t r i n g e n t
lessstringent
highly motivated, adherent,excellent self-care capacities
less motivated, non-adherent,poor self-care capacities
low high
newly diagnosed long-standing
long short
absent few / mild severe
absent few / mild severe
really available limited
62
ABCDs of choosing med
A -> Age, A1c (degree of hyperglycemia)
B -> Body wt/ BMI
C -> Cost/Coverage; Co-morbidities Convenience/Complexity; CV benefit
D -> Defect; Duration of DM
S -> Side effects ; Safety profile
63
• Individualize glycemic targets based on a variety of patientand disease characteristics.
• Diet, exercise, & education are foundations of T2DM therapy.
• Metformin is first choice at diagnosis unless contraindicated.
• After metformin, data are limited. Combination therapy with1-2 other oral / injectable agents is recommended.
• Over time, many patients will require insulin alone or incombination with other agents to maintain glycemic control.
• All treatment decisions should be made in partnership withthe patient, focusing on patient preferences, needs & values.
ADA/EASD Management of Hyperglycemia in T2DM, 2015 Position Statement Summary
64
T2DM Med Charts
• Diabetes Health Type 2 MedicationReference Guide:https://www.diabeteshealth.com/wp-content/uploads/2016/03/Type2.pdf
• MPR Diabetes Treatments Chart:http://www.empr.com/diabetes-treatments/article/123836/
65
References • American Diabetes Association. Standards of Care in Diabetes-2016.
Diabetes Care January 2016 39:S1-119.
• Eng C, Kramer CK, Zinman B, Retnakaran R. Glucagon-like peptide-1receptor agonist and basal insulin combination treatment for themanagement of type 2 diabetes: a systematic review and meta-analysis. Lancet. 11 September 2014.
• Hinnen DA. Therapeutic Options for the Management of PostprandialGlucose in Patients With Type 2 Diabetes on Basal Insulin. Clinical Diabetes2015;3:175-180.
• Inzucchi SE et al. Management of Hyperglycemia in Type 2 Diabetes, 2015:A Patient Centered Approach: Update to a Position Statement of theAmerican Diabetes Association and the European Association for the Studyof Diabetes. Diabetes Care 2015;38:140–149.
• Davidson MB, Raskin P, Tanenberg RJ, Vlajnic A, Hollander P. A stepwiseapproach to insulin therapy in patients with type 2 diabetes mellitus andbasal insulin treatment failure. Endocrine Practice 2011;17:395–403.