Drugs not in common use in cardiac ER
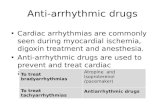
-
Upload
amir-mahmoud -
Category
Health & Medicine
-
view
47 -
download
2
Transcript of Drugs not in common use in cardiac ER

Mohamed helmy, MD
National heart institute

65 years old male patient presented in the ER by attack of hypertensive crisis with BLP :260/120 resistant to medications including IV nitrate and iv Frusamid…….Whats your Next option ???????

50 y male patient known to have uncontrolled hypertension presented in the ER by sever agonizing chest pain radiating to the back , unequal radial pulse , blp 179/100 in the rightarm, TTE revealed aortic regurge with suspected flap in the ascending aorta whatsyour first chiose drug ?????????

During PPCI for 45 female patient presented in the ER by extensive anterior MI , CA revealed big thrombus in the proximal LAD and after stenting there is noreflow , whatsyour prefered medication ?????????

Sodium nitroprusside (Abbreviated SNP, brand name: Nitropress) has potent vasodilating effects in arterioles and venules (venulesmore than arterioles, but this selectivity is much less marked than that of nitroglycerin)[6]. It is administered intravenously in cases of acute hypertensive emergency. SNP breaks down in circulation to release nitric oxide (NO). NO activates guanylatecyclase in vascular smooth muscle and increases intracellular production of cGMP. cGMP activates Protein Kinase G which activates phosphatases which inactivate Myosin light chains. Myosin light chains are involved in muscle contraction. The end result is vascular smooth muscle relaxation, which allow vessels to dilate.
In the human heart, nitric oxide reduces both total peripheral resistance as well as venous return, thus decreasing both preloadand afterload. For this reason, it can be used in severe cardiogenic heart failure where this combination of effects can act to increase cardiac output. In situations where cardiac output is normal, the effect is to reduce blood pressure.


Sodium nitroprusside slowly breaks down to release 5 cyanide ions, especially upon exposure to UV light. Despite the toxic potential of cyanide, nitroprussideremains an effective drug in certain clinical circumstances such as malignant hypertension or for rapid control of blood pressure during vascular surgery and neurosurgery. The cyanide can be detoxified by reaction with a sulfur-donor such as thiosulfate, catalysed by the enzyme rhodanese. In the absence of sufficient thiosulfate, cyanide ions can quickly reach toxic levels.[7] The half-life of nitroprusside is 1–2 minutes, but the metabolite thiocyanate has an excretion half-life of several days.

Sodium nitroprusside is appropriate for the acute treatment of congestive heart failure. The starting dose is 0.3 to 0.5 μg/kg/min titrated to goal attainment of desired hemodynamics but usually not beyond 5 μg/kg/min. Doses of 10 µg/kg/min or sustained administration will result in excessive cyanide production, which may occasionally lead to cyanide poisoning and may rarely lead to the development of methemoglobinemia. Both conditions require immediate intervention with cessation of the infusion and/or initiation of hemodialysis and possibly administration of thiosulfate or methylene blue

DRUG DOSAGE ONSET/DUR ADV.EFFE
Nitroprusside 0.25-
10mcg/kg/min
Instant/1-2min. Thiocyanate,cyani
de poisoning
Nitroglycerine 5-100mcg/min 1-5min/3-5min Flushing,headach
e,methemoglobin
Nicardipine 5-15mg/hr 5-10min/1-4hr Tachycardia,flushing
.avoid-heart failure
Hydralazine 10-20mg 5-15min/3-8hr Flushing,tachy,avoid
-A.diss,MI
Enalapril 10-40mg IM,1.25-
5MG1Vq6hr
20-30min/6hr Hypotension,renal
failure,hyperkalemia
Fenoldopam 0.1-
0.3mcg/kg/min
5min/10-15min Flushing,headache,t
achy

Labetalol - alpha-1 and non-selective beta blocker
- beta blockade predominates during IV administration (3-7 times alpha blockade)- beta blockade prevents reflex increase in heart rate, cardiac output and myocardial oxygen consumption- in pre-eclampsia rapidly reduces BP without decreasing uteroplacental blood flow- crosses placenta but neonatal bradycardia and hypoglycaemia rarely seen- disadvantages in pre-eclampsia include interpatient variability in dose requirement and variable duration of action
Dose For acute hypertension bolus of 1-2 mg/kg over 10 min OR mini-boluses of 20 mg followed by 20-80 mg every 10 min OR incremental infusion of 0.5-4 mg /min. This method is least likely to cause
hypotension and bradycardia For pre-eclampsia 10 mg IV initially double dose every 10 min as necessary to a maximum of 300 mg alternatively: 1-2 mg/min IVI reducing to 0.5 mg/min or less after arterial

Pharmacodynamics - direct arteriodilator with little venodilator action
- reduces diastolic pressure more than systolic- may induce reflex tachycardia and increased cardiac output which may blunt its hypotensiveeffect. Combination with a central alpha-2 agonist or a beta blocker decreases this reflex sympathetic activity- improves renal and uteroplacental blood flow in pre-eclampsia- onset time 10-20 min. Duration of action 6-8 h
Adverse effects - reflex tachycardia
- headaches,- nausea & vomiting- flushing- skin rash- lupus syndrome: more likely to develop after prolonged therapy, in slow acetylators and in patients with renal failure- infusions may be difficult to titrate in pre-eclampsia and may be associated with a higher incidence of fetal distress- in presence of hypovolaemia may result in hypotension and fetal distress- neonatal thrombocytopenia (rare)
Dose - in hypertensive emergencies: IV boluses of 10-20 mg, repeated as necessary at 15 min
intervals, to a maximum of 50 mg. Can also be given as an infusion: 0.5-1 mg/min- in pre-ecplamsia for control of BP: 5 m

46 y male patient known to have CHF (EF:28%), presented in the ER by attack of acute sever dyspnea, pulmonary congesion with increase in CVP , poor response to max doses of dpopamin and dobuamine
Whats your next option

Mode of action vasodilatory, natriuretic and diuretic effects primarily mediated via natriuretic peptide receptor A on vascular smooth muscle,
endothelium, kidneys and adrenals no direct inotropic effect ± reduces aldosterone and inhibits plasma renin activity Pharmacokinetics administration: IV infusion distribution
◦ distribution t1/2 ~2 mins◦ mean volume of distribution at steady state 0.19 l/kg
elimination by multiple routes:◦ after binding to cell surface natriuretic peptide receptor C nesiritide is internalized and
degraded◦ hydrolysis by endopeptidase◦ renal filtration
elimination t1/2 ~18 mins clearance proportional to body weight (~0.55 l/h/kg) dosage adjustment not required in patients with renal dysfuncti

Dosage and Administration AdultsIV Recommended dose is 2 mcg/kg IV bolus over 60 sec followed by
continuous infusion at a dose of 0.01 mcg/kg/min. If hypotension occurs during administration, reduce or discontinue the dose and start other measures to support BP.
General Advice For IV administration only. Not for intradermal, IM, subcutaneous, or intra-arterial
administration. Follow manufacturer's instructions for reconstitution of powder and final dilution
for infusion solution. Do not shake or agitate vials during reconstitution or dilution. Do not use filter
needles during preparation of infusion. Do not administer if solution is cloudy, discolored, or contains particulate matter. Prime IV tubing with infusion solution prior to connecting to patient's vascular
access port and prior to administering bolus dose and starting infusion. Infusion rate may be increased by 0.005 mcg/kg/min, no more often than every 3
h up to a max of 0.03 mcg/kg/min. Increases in infusion rate should be preceded by a bolus dose of 1 mcg/kg.
Do not administer through a central heparin-coated catheter. Flush catheter between administration of nesiritide and any incompatible
injectable medication.

Clinical indications
acute decompensated heart failure with dyspnoea on minimal exertion or at rest◦ reduces preload. Rapid reduction in pulmonary capillary wedge pressure (faster than glyceryl trinitrate) and
right atrial pressure◦ reduces afterload resulting in increase in cardiac output◦ diuresis & natriuresis◦ 6 month mortality similar to patients treated with nitrate but lower than those treated with dobutamine
contraindicated in cardiogenic shock or in patients with systolic BP <90 mmHg
Adverse effects
Cardiovascular
Similar incidence to patients treated with nitrate.
hypotension◦ usually resolves spontaneously or responds to fluid challenge of 250 ml or less◦ duration of episode longer than hypotensive episodes associated with glyceryl trinitrate
not proarrhythmic
Non-cardiovascular
Less common than with glyceryl trinitrate
general pain
abdominal pain
catheter-related pain
headache
nausea

Adverse effects
Cardiovascular
Similar incidence to patients treated with nitrate.
hypotension◦ usually resolves spontaneously or responds to fluid challenge of 250 ml or less
◦ duration of episode longer than hypotensive episodes associated with glyceryl trinitrate
not proarrhythmic
Non-cardiovascular
Less common than with glyceryl trinitrate
general pain
abdominal pain
catheter-related pain
headache
nausea
Drug interactions
does not interact with enalapril
interactions with IV vasodilators (including IV ACE inhibitors) and other cardiovascular drugs have not been formally studied
Dosage & administration
bolus of 2 mcg/kg followed by infusion of 0.01 mcg/kg/min
reduce dose/discontinue if hypotension occurs
should only be used in pregancy if potential benefit to mother outweighs potential risk to fetus
administer with caution to breastfeeding mot

Clinical Results Natrecor has been evaluated in 10 trials that included 941 subjects with
congestive heart failure. The randomized, double-blind VMAC (Vasodilation in the Management of Acute
Congestive Heart Failure) trial included 489 subjects who required hospitalization for management of shortness of breath at rest due to acutely decompensated CHF. The trial compared the effects of Natrecor, placebo and intravenous nitroglycerin when added to background therapy. Among other measures, the trial was designed to evaluate the change from baseline in pulmonary capillary wedge pressure (PCWP) and the change from baseline in subjects' dyspnea (abnormal breathing), evaluated after three hours.
Results demonstrated that subjects receiving Natrecor reported greater improvement in their dyspnea at three hours than subjects receiving placebo. Additionally, there was a greater reduction in mean PCWP for the Natrecor-treated group compared to placebo- and nitroglycerin-treated subjects.
In a second double-blind trial, 127 subjects requiring hospitalization for symptomatic CHF were randomized to receive placebo or one of two doses of Natrecor. Results demonstrated that subjects receiving both doses of Natrecorreported greater improvement in dyspnea at six hours compared to subjects receiving placebo.






28 Y female patient presented to you in the ER by attack of repeated palpitation, presyncope , no PH of RHD, IHD, and she was hemodynamicaly stable , normal echodopplerstudy
ECG revealed the following strip :


Supports SVT
◦ Slowing or termination by vagal tone
◦ Onset with premature P wave
◦ RP interval <100mS
◦ P & QRS rate & rhythm linked to suggest ventricular activation depends on atrial discharge
◦ Long-short cycle sequence
Supports VT
◦ Fusion beats
◦ Capture beats
◦ AV dissociation
◦ P & QRS rate & rhythm linked to suggest that atrial activation depends on ventricular discharge
◦ “compensatory” pause
◦ L axis deviation
◦ QRS duration >140mS

The administration of adenosine during SVT may be a useful diagnostic as well as therapeutic intervention.
Adenosine may unmask atrial flutter when the diagnosis is not readily apparent from the ECG.
It is particularly effective for treatment of arrhythmias that depend on the AV node, such as AV node re-entry or orthodromic AV re-entry. The response of atrial tachycardias is variable. Sometimes adenosine terminates these arrhythmias and other times it reveals the P-wave morphology by creating AV block.
It is also used to differentiate VT from SVT with aberrant conduction. VT is rarely affected by adenosine, but SVT will either terminate or be exposed by transient AV block. Adenosine may not have any effect if it is administered slowly through a peripheral vein or if the
patient has consumed caffeine.

Receptors
3 types of receptors. A1 and A2 receptors are subtypes of P1 class of receptors
A1 or A2 agonist-receptor complex is responsible for inhibition or stimulation of adenylatecyclase and a decrease or increase in intracellular cAMP respectively.
adenosine also has actions which are not mediated via cAMP
both cAMP mediated effects and other actions appear to be mediated by G proteins
A1 and A2 receptors blocked by methylxanthines such as theophylline
A3 receptor has recently been characterized. It is resistant to blockade by methylxanthines but may be stimulated by both A1 and A2 agonists
Cardiac electrophysiological effects
mostly mediated by A1 receptor
depression of sinus node automaticity and AVN conduction. Associated with an increase in PR and AV intervals but not in HV interval, suggesting a site of action proximal to bundle of His. Mediated by:
activation of a specific outward K current which is independent of adenylate cyclase. Results in shortening of the atrial action potential, hyperpolarisation of the SAN cells and depression of the amplitude, duration and rate of rise of action potential in AVN cells.
attenuation of effects of catecholamines by inhibiting adenylate cyclase stimulation of the inward calcium current in atrial and ventricular myocytes. Greater inhibition of this current occurs after previous stimulation by beta agonists
stimulation of presynaptic adrenergic receptors on adrenergic nerves which decreases the amount of norepinephrine released for any given level of sympathetic stimulation

Drug interactions
dipyridamole potentiates action by inhibiting uptake
methylxanthines are competitive antagonists and may necessitate larger doses
can be safely administered to patients taking digoxin, quinidine, beta blockers, calcium blockers, ACE inhibitors
Adverse effects
occur in approx 20% but are brief (<1 min)
include:◦ facial flushing◦ SOB◦ chest tightness◦ asystole
Contraindications
not recommended in patients with sick sinus syndrome due to possibility of prolonged heart block
bronchospasm
© Charles Gomersall December 1999
©Charles Gomersall, September, 2012 unless otherwise stated. The author, editor and The Chinese University of Hong Kong take no responsibility for any adverse event resulting from the use of this webpage.Copyright policy Contributors


30 male patient presented in the ER by attack of unstble angina and he developed rapid palpitation , ECG revealed Atrial flutter , he was hemodynamicaly stable
Whats your drug of choice???


Indication Peak Effect
(min) T1/2 Duration Receptor HR BP
Esmolol Yes Yes 2 9 min 10-20
min
1
Atenolol No Yes 2 6-7 h 12 h 1
Labetalol No Yes 5 5.5 h 3-5 h 1,1&2
Metoprolol No Yes 20 3-7 h 5-8 h 1
Propranolol Yes No <10 4 h Variable 1&2
Diltiazem Yes No 2-5 3.4 h 1-3 h Ca2+
Verapamil Yes No 3-5 2-5 h 1-2 h Ca2+

Brevibloc (Esmolol Hcl)
Bristol-Myers Squibb Company
Ultrashort-acting, Cardioselective (ß1) Beta blocker(IV)
Indication:
--- Supraventricular Tachycardia--- Atrial Fibrillation
--- Atrial Flutter ---Peri-OP, Post-OP Tachycardia / Hypertension
--- Acute Myocardial Ischemia

ß1-selective Adrenergic Receptor Blocker,
ß1:ß2 = 40:1 (highly cardioselective)
Very Soluble in Water
No Intrinsic Sympathomimetic Activity
No Membrane Stabilizing Activity
No Significant Drug Interaction
Rapid Onset: 2 mins
Ultra-short Action: 10-20 mins

Decrease in--- heart rate (peak effect in 60 sec)
--- blood pressure (peak effect in 2 min)
--- cardiac index
--- rate pressure product (RPP)
--- left and right ventricular ejection fraction
Prolongation of--- sinus cycle length
--- decrease AV node conduction velocity
--- decrease the rate of SA node activity
--- antegrade Wenckebach cycle length
--- the sinus node recovery time
--- increase AV nodal refractoriness interval

A Selective Approach:◦ Targeted to the Heart
◦ Little effect on Bronchial Smooth Muscle
◦ Maybe used with caution in p'ts with asthma, COPD
A Flexible Approach:◦ Administer as long as indicated…..
◦ Maintenance infusions up to 48 hrs or short as you want; rapid reversal of effect within minutes

A Confident Approach:◦ Easy to titrate upward or downward to desired heart
rate
◦ Allows maximum beta blockade while still maintaining
ventricular function
An Effective Approach:◦ Rapid control of atrial fibrillation,atrial flutter and sinus
tachycardia

The Advantage of Brevibloc III

Indication
- Supraventricular tachycardia (SVT)
- Peri-OP, post-OP Tachycardia / Hypertension
- Acute Myocardial Ischemia
Dosage
Loading: 0.5 mg/kg, over 1 min
Maintenance: 0.05-0.2 mg/kg/min; *0.2 mg/kg/min --- average effective dosage: 0.1 mg/kg/min

Dosage Guideline

A “less toxic” amiodarone
Half-life: 13-19 hours
Only FDA-approved for atrial fibrillation/flutter◦ Not as effective as amiodarone

GI irritation
Prolongs QT interval
Negative inotrope◦ Contraindicated in:
NYHA IV
Acute CHF exacerbations

Metabolized by CYP 3A4
Inhibits CYPs 3A4 & 2D6 and P-gp
Increases digoxin levels
Dosing: 400 mg BID

Pharmacology◦ Type III antiarrhythmic
◦ Indicated for acute conversion of atrial flutter a/o fibrillation
◦ Proarrhythmic
More so in patients w/ CHF
If ibutilide fails to convert, it may at least enhance the response to electrocardioversion

Monitor for proarrhythmias, including torsade de pointes, for 4-6 hours after dosing and until QT is not prolonged
Hepatically cleared◦ Half-life: ~6 hours

Approved Dosing◦ 1 mg (0.01 mg/kg < 60 kg) over 10 min; repeat,
if needed, after 10 min
◦ Preload with magnesium (?)
Alternative Method of Dosing◦ 2 mg (placed in 50 cc D5W) over 30 minutes
◦ Stop infusion when patient converts
◦ Preload with magnesium (?)

Prasugrel
• Developed by Lilly and Sankyo
• Drug belongs to the same class as clopidogrel—thienopyridine P2Y12 receptor antagonists
• Acts directly on the receptor
Heartbeat – November 2005

• Data reported from a pooled analysis of three early-phase studies
• In total, 112 healthy volunteers were randomized to receive either a 60-mg loading dose of prasugrel or a 300-mg loading dose of clopidogrel in a two-way crossover design
• ADP-induced platelet aggregation was measured in blood samples at four to five hours and 24 hours after the medications were administered
Heartbeat – November 2005

All subjects responded effectively to prasugrel, but when the same subjects were given clopidogrel, between 22% and 43% were classed as nonresponders, depending on the definition of nonresponder used
Heartbeat – November 2005

Agent metabolized differently, and more rapidly, than clopidogrel
• Issue of no-response or low response shifted upward with prasugrel
"Is more platelet inhibition better for improving outcomes, as we've seen with clopidogrel vs just aspirin alone?"
- Cannon
Heartbeat – November 2005

The Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel–Thrombolysis in Myocardial Infarction 38 (TRITON-TIMI 38) randomized 13 608 ACS patients undergoing PCI to prasugrel or standard dose clopidogrel,20 and showed that prasugreltherapy was associated with significantly reduced rates of ischaemic events, including stent thrombosis, but with an increased risk of major bleeding

The presently described TRITON-TIMI 38 substudy was not powered to show a significant difference in clinical outcomes between patients on prasugrel and those on clopidogrel. However, this substudy was designed and sufficiently powered to show differences in platelet function between patients on prasugrel and those on clopidogrel. Previous studies have shown that such differences in platelet function affect clinical outcome.7–

45 female patient addmitted in the ER with ACS, on iv nitrare , heparin , ASA, clopidogrelat fifth day she start to complain from sever dyspnea , tachpnea , Po2 65, , with hematemsis and then developed DVT, CT angio revealed PE, after 2days she developed acute ischemia in right leg ,lab revealed plat count 53000, mild anaemia
Whats your possible diagnosis and management???

Venous thromboembolism
Arterial thrombosis
Skin lesions at heparin injection site
Acute platelet activation syndromes
10/98medslides.com 54

a rapid drop in platelets may also be indicative of HIT, particularly if the patients received heparin within the previous 3 months
a fall in platelet count of >50% that begins after 5 days of heparin therapy, but with the platelet count > 150 x 109/L, should also raise the suspicion of HIT
10/98medslides.com 55

Lower limb involvement
Stroke
Myocardial infarction
Other
10/98medslides.com 56
AM J Med 1996;101:502-507
Venous thrombotic events predominate over arterialevents by 4:1 ratio. Usually involving large vessels.

HIT-associated mortality is high (about 18%)
5% of affected patients require limb amputation
Overt bleeding or bruising is rare even with severe thrombocytopenia
Appropriate management can limit morbidity and mortality
10/98medslides.com 57

Test Advantages Disadvantages
PAA Rapid and simple Low sensitivity - not suitable for
testing multiple samples
SRA Sensitivity >90% Washed platelet (technically
demanding), needs radiolabeled
material 14C
HIPA Rapid, sensitivity >90% Washed platelets
ELISA High sensitivity, High cost, lower specificity for
detects IgA and IgM clinically significant HIT
10/98medslides.com 58
Thromb Haemost 1998;79:1-7

Ancrod◦ a defibrinogenating snake venom
◦ slow onset of action (must be given over 12 to 24 hours)
◦ does not thrombin generation which is important in the pathogenesis of HIT
◦ HIT and DIC patients may already be hypofibrinogenemic
10/98medslides.com 59
Blood 1996;88(Suppl 1):626a

The only direct thrombin inhibitor approved for use and for treatment of HIT in the U.S.
German trial of 200 patients with HIT◦ 75% to 81% effectively anticoagulated◦ significant reduction in composite endpoints
(death, limb amputation, new thrombotic complications) compared with historical control
7 day 10% vs 23% 35 day 25% vs 52%
10/98medslides.com 60
Blood 1996;88(suppl):281a

a small synthetic non-polypeptide molecule
a direct thrombin inhibitor
FDA approved June30, 2000
has the same theoretical advantages of lepirudin ◦ short half-life (< 1hr)
◦ lack of cross-reactivity for HIT antibodies
◦ potent antithrombin activity
metabolized predominantly by the liver, may require dose adjustment
excreted normally even in severe renal failure
Update 10/00medslides.com 61