cystic fibrosis pancreatic - Proceedings of the National ... · Acystic fibrosis pancreatic...
Transcript of cystic fibrosis pancreatic - Proceedings of the National ... · Acystic fibrosis pancreatic...

Proc. Natl. Acad. Sci. USAVol. 87, pp. 4012-4016, May 1990Cell Biology
A cystic fibrosis pancreatic adenocarcinoma cell line(chloride channel/pancreas)
R. A. SCHOUMACHERa, J. RAMa, M. C. IANNUZZIc, N. A. BRADBURYad, R. W. WALLACEad, C. TOM HONc,D. R. KELLYawe, S. M. SCHMIDf, F. B. GELDERg, T. A. RADOah, AND R. A. FRIZZELLaiaGregory Fleming James Cystic Fibrosis Research Center, and Departments of 'Physiology and Biophysics, bPediatrics, dPharmacology, ePathology, andhMedicine, University of Alabama at Birmingham, University Station, Birmingham, AL 35294; cDepartment of Internal Medicine, University of Michigan,Ann Arbor, MI 48103; bDepartment of Chemotherapy and Toxicology, Southern Research Institute, Birmingham, AL 35255; and gDepartment of Surgery,Louisiana State University, Shreveport, LA 71130
Communicated by I. S. Edelman, March 12, 1990 (received for review January 26, 1990)
ABSTRACT We established a pancreatic adenocarcinomacell line (CFPAC-1) from a patient with cystic fibrosis (CF) andassessed some of its properties. The cells show epithelialmorphology and express cytokeratin and oncofetal antigenscharacteristic of pancreatic duct cells. Basal and stimulatedlevels of cAMP and cAMP-dependent protein kinase and thebiophysical properties of single Cl- channels in CFPAC-1 aresimilar to those of airway and sweat gland primary cultures andCl--secreting epithelial cell lines. Anion transport and singleCl- channel activity was stimulated by Ca2+ ionophores but notby forskolin, cAMP analogs, or phosphodiesterase inhibitors.The cells express the CF gene and manifest the most commonCF mutation, deletion of three nucleotides resulting in aphenylalanine-508 deletion. These properties have been stablethrough >80 passages (24 months), suggesting that CFPAC-1can serve as a continuous cell line that displays the CF defect.
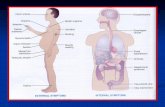
Cystic fibrosis (CF) is a chronic, inherited disease thatimpairs the electrolyte transport properties of epithelial cellsin the airways, sweat glands, pancreas, and other organs (1).The primary culture of human epithelial cells from some ofthese tissues has permitted studies of the functional basis ofthe CF defect. Single-channel patch-clamp analysis has re-vealed apical membrane Cl- channels in CF cells that aredefective in their activation by cAMP-mediated agonists (2,3) but are stimulated by agents that raise intracellular Ca2+(2). While patch-clamp studies are feasible using a limitedsupply of human epithelial cells, an understanding of themolecular and biochemical basis ofthe CF defect in epithelialcells is likely to require access to permanent cell lines.A patient at the University of Alabama at Birmingham
Cystic Fibrosis Care Center developed pancreatic adenocar-cinoma; the clinical presentation is described in detail else-where (4). The patient was a 26-year-old white male with CF,pancreatic insufficiency, moderate pulmonary involvement,and insulin-dependent diabetes mellitus. Exploratory lapa-rotomy revealed a large tumor in the head ofthe pancreas andmultiple smaller lesions in the liver. Histology showed awell-differentiated pancreatic ductal adenocarcinoma. As-cites fluid and tumor fragments were obtained at autopsy, 6weeks after larparatomy. This report details the developmentand characterization of a continuous cell line from thismaterial, including analysis of the regulated anion transportproperties and the CF genotype.
MATERIALS AND METHODSCulture Techniques. Primary cultures of epithelial cells
from fragments of pancreatic (primary) and liver (metastatic)
tumors were established by using an explant technique (5).Ascites fluid was centrifuged and the pellet was resuspendedin culture medium. All cultures were initially seeded andgrown in RPMI 1640 medium (Sigma); after passage 2, wechanged to the richer Iscove's modified Dulbecco's medium(Sigma), which has been used successfully for a variety oftumor cell lines (6). Media were supplemented with 10%1o fetalbovine serum and maintained at 370C in a 5% C02/95% airatmosphere. Cells were usually passaged at 1:10 dilution byexposure to 0.05% trypsin in a 1.5 mM EDTA buffer at 370Cfor 3 min. Xenograft culture in congenitally athymic mice wasattempted with standard techniques (7).Morphology and Markers of Differentiation. Cells cultured
on coverslips were fixed in 10%o neutral-buffered formalin andembedded in paraffin. Cytokeratin expression was evaluatedby immunofluorescence (8), using pooled mouse monoclonalanti-keratin (Boehringer Mannheim). For transmission elec-tron microscopy, cells were fixed with 3% glutaraldehyde in0.1 M Sorenson's buffer for 1 hr and postfixed in 1% OS04 inSorenson's buffer for 1 hr. After dehydration through anethanol series, the cells were flat-embedded in Polybed 812resin (Polysciences). The expression of several oncofetalantigens (CEA, POA, ACAA, CA 19-9) was evaluated bystandard ELISA, performed on medium removed from near-confluent cell cultures after 3 days of incubation. Unusedmedium served as control.
Isotopic Anion Efflux. Cells were plated at a density of 105cells per cm2 on 35-mm culture dishes that were used when80-100% confluent. Effluxes were performed at 370C, usinga phosphate-buffered Ringer's (PBR) solution containing 140mM NaCl, 3.3. mM KH2PO4, 0.83 mM K2HPO4, 1 mMCaSO4, 1 mM MgSO4, 10 mM glucose, and 10 mM Hepes,buffered to pH 7.4. Cells were loaded with 1251 (1-2 ,uCi/ml;1 Ci = 37 GBq) for 30 min, washed briefly with PBR to depleteextracellular 1251, and efflux was monitored by a sample-replace procedure. After five samples, the solutions con-tained 10 ,M forskolin, 2 ,uM ionomycin, or 10 ,uM A23187.Remaining monolayer 1"I was extracted in 0.1 M nitric acid.Sample and extract counts were summed and the efflux wasexpressed as a time course of the loaded 1251I remaining in themonolayer. This assay monitors conductive anion exit asevidenced by inhibition of efflux by raised extracellular [K+]to depolarize membrane voltage or by the Cl- channelblockers 5-nitro-2-(3-phenylpropylamino)benzoic acid, di-phenylamine carboxylic acid (9), or indanyloxyacetic acid 94(10) (data not shown),cAMP Determination. Cells were cultured as described in
the efflux experiments. After a 30-min preincubation andwash with PBR, monolayers were exposed to control andexperimental solutions for various times at 37°C. IntracellularcAMP was assayed according to published methods (11),using a radioimmunoassay kit (NEN); 0.1 pmol of [3H]cAMP
Abbreviation: PKA, protein kinase A.
4012
The publication costs of this article were defrayed in part by page chargepayment. This article must therefore be hereby marked "advertisement"in accordance with 18 U.S.C. §1734 solely to indicate this fact.

Proc. NatL. Acad. Sci. USA 87 (1990) 4013
was added to each sample to assess recovery. Data arereported as pmol of cAMP per mg of protein (12).
Protein Kinase A (PKA) Activity. Cytosolic fractions(100,000 x g; 60 min supernatant) were prepared from cellsgrown to confluence in 100-mm dishes. cAMP-dependentPKA activity was determined by the ability of cAMP tostimulate incorporation of 32P04 from [y-32P]ATP (Amer-sham) into the synthetic substrate Kemptide (13). Proteinkinase activities are reported as pmol ofP04 incorporated permin per mg of cytosolic protein.
Single-Channel Recording. Techniques for single-channelrecording using the cell-attached and excised, inside-outconfigurations of the patch-clamp method have been de-scribed in detail (2, 14). The recording pipette contained 150mM NaCI, 2 mM CaCl2, 5 mM MgCl2, and 5 mM Hepes (pH7.2) or a similar solution in which NaCl was replaced by 135mM N-methyl-D-glucamine chloride plus 15 mM NaCl. Bathsolutions contained 150mM NaCl, 5 mM MgCl2, 1 mM CaCl21 mM EGTA, and 5 mM Hepes (pH 7.2). Estimated free Ca2Wof the bath was 10 ,uM. Relative ion permeabilities werecalculated as described (14). To determine the relative per-meabilities to sodium and chloride, bath NaCl was changedto 300 or 50 mM. For the halide selectivity determinations,bath NaCl was replaced by NaBr or Nal.DNA and RNA Analyses. Cells were harvested and resus-
pended in PBS to a concentration of 5 x 106 cells per ml.DNA and RNA were prepared as described (15, 16). DNAwas amplified by using Thermus aquaticus DNA polymerase(Taq polymerase) (17). The amplification sequences for ge-nomic DNA were 5'-CAGTTlTCCTGGATTATGCCTG-GCAC-3' and 5'-GTTGGCATGClT-GATGACGCTTC-3'.RNA was amplified via cDNA (16). Reactions for reversetranscriptase were performed in a 50-,ul volume. Two reac-tion mixtures each contained 1 ,ug of total RNA, 21 units ofMoloney murine leukemia virus reverse transcriptase (Boeh-ringer Mannheim), and 3 ug of oligo(dT) as primer. Onereaction mixture without reverse transcriptase served as acontrol for DNA contamination of the RNA preparation. Allthree were incubated for 1 hr at 37°C. ForRNA amplification,the reaction mixtures were the same as for DNA except that10 ,ul of the RNA reaction mixture was used in place ofgenomic DNA and the primer sequences were from exon 7(5'-CCACCATCTCATTCTGCATTGTTCTGC-3') and exon13 (5'-TCCAGGAGACAGGAGCATCTCCTTCTAATG-3').After amplification, 50 ,ul of chloroform was added and eachtube was centrifuged to separate the aqueous phase from themineral oil.
..aII
To test for the presence of either the common CF mutationor the normal sequence, the samples were divided and run induplicate agarose gels, and the DNA was transferred toNytran (Schleicher & Schuell) by Southern blotting usinglOx SSC (lx SSC = 0.15 M NaCl/0.015 M sodium citrate).Hybridization with allele-specific oligonucleotides was per-formed as described (17).
RESULTSIn Vitro Cultre and Morphology. Growth was observed
from >70% of adherent tumor explants; the first outgrowthswere noted 2-3 weeks after plating. Three morphologies wereobserved in the initial cultures: (i) epithelial cells, which grewin a cobblestone pattern and had a high nucleus/cytoplasmratio; (ii) fibroblastoid cells; and (iii) round cells, both ofwhich had lower nucleus/cytoplasm ratios, grew in a disor-ganized pattern and occasionally contained multiple nuclei.Differential trypsinization (16) was used to purify cells withepithelial morphology from the mixed primary cultures ofmetastatic liver tumor; this cell line was designated CFPAC-1, and its properties are described in this report.CFPAC-1 has been in continuous culture for >24 months
and 80 passages, without evidence of altered morphology (bylight microscopy) or anion transport (by isotopic flux; seebelow). The cells lack both contact inhibition and dilutionlimitation of their proliferation. Their doubling times were 30and 32 hr at passages 17 and 74, respectively. They have beencloned by the Noble agar and limiting-dilution techniques.Both tumor and ascites fluid samples were tumorigenic inathymic mice, suggesting a potential for virtually unlimitedcell volume expansion at low in vitro passage number.Karyotype analyses of CFPAC-1 cells at passage 25 (n = 7)revealed hyperdiploidy with 65-75 chromosomes (median,73) per nucleus, including several translocations. Two orthree normal-appearing copies ofchromosome 7, the locus ofthe CF gene, were observed in every metaphase photo-graphed.
Epithelial Markers and Ultrastructure. Transmission elec-tron microscopy of CFPAC-1 grown on plastic coverslipsreveals epithelial polarization with apical microvilli, tightjunctions, and gap junctions (Fig. la). CFPAC-1 cells stainstrongly positive for keratin by immunofluorescence (Fig.lb), confirming their epithelial origin. They express oncofetalantigens that are associated with pancreatic ductal adeno-carcinoma (18, 19). ELISA of culture medium supernatantsrevealed 9 ng of carcinoembryonic antigen per ml, 28 ng of
-I.
FIG. 1. (a) Transmission electron micrograph from confluent in vitro culture of CFPAC-1, passage 10, showing apical microvilli andglycocalyx, subapical cytoplasmic vacuoles containing mucin granules, and tightjunctions between adjacent cells. (x 10,100.) (b) Keratin stainingby immunofluorescence of CFPAC-1 cells, passage 10. (x550.)
Cell Biology: Schoumacher et al.

4014 Cell Biology: Schoumacher et al.
pancreatic oncofetal antigen per ml, 5 Ag ofadenocarcinoma-associated antigen per ml, and 12,000 units ofCA 19-9 per ml(n = 2). Virgin medium contained no detectable amounts ofthese antigens. These findings suggest that CFPAC-1 isderived from a tumor of the pancreatic duct (20).
Radioiodide Efflux. The macroscopic anion transport prop-erties of CFPAC-1 cells were assessed by using an isotopicanion (1251) efflux assay (Fig. 2). The Cl--secreting humancolonic adenocarcinoma cell line, T84, served as a positivecontrol for the effects ofcAMP- and Ca2+-mediated secretoryagonists. 1251 efflux from T84 monolayers increased 7-fold inresponse to the adenylate cyclase activator, forskolin, or theCa2+ ionophores, A23187 or ionomycin (Fig. 2a). In contrast,CFPAC-1 responded to the Ca2+ ionophores with 7- and27-fold increases in anion efflux but did not respond toforskolin (Fig. 2b). In other experiments, 125j efflux fromCFPAC-1 also was not affected by the cAMP analogues8-Br-cAMP and chlorophenylthio-cAMP, or the phosphodi-esterase inhibitor isobutylmethylxanthine (100 AM each).cAMP and PKA Levels. Levels of the intracellular media-
tors of forskolin's effects, cAMP and the cAMP-dependentPKA, were determined in CFPAC-1 and T84 cells. BasalcAMP levels in T84 and CFPAC-1 were 11 ± 2 (SEM) (n =16) and 10 ± 1 pmol per mg of protein (n = 15), respectively.After 15 min of exposure to 10 ,uM forskolin, cAMP in T84and CFPAC-1 increased to 1570 ± 225 (n = 14) and 415 ± 78pmol per mg of protein (n = 13), respectively. Fig. 3a showsthat the time courses of cellular cAMP accumulation in T84and CFPAC-1 during the initial 2 min offorskolin stimulation,a time that correlates with the initiation of the anion transportresponse (Fig. 2), do not differ in T84 and CFPAC-1.
a
5001r.
0G)0
P0.1012bA
;w
100+
10-
b
o*
co> -a
.0) .0
>
*-) ,.< _.O) S.
Proc. Natl. Acad. Sci. USA 87 (1990)
o T84* CFPAC- 1
V,
iTime (min)
= ControlCM PKA Inhibitor
cAMPwu PKA Inhibitor+cAMP
T84
a100 4
0,.)
-4
._
co 0
o4 o
-4
10-10*O 1 ~ ~~~~~~~~~23
b
100
. ° \~~~~~~~I
1O - o 0Forskoln (10 I&)(n- 16) \0 A23187 (10 MM)(n-6)
. - onomycin (2 pM)(n-6)
3- I
0 1 2 3Time (min)
FIG. 2. Time course of 1251 efflux from T84 (a) and CFPAC-1 (b)cells. Stimulation of efflux by agonist is expressed as the ratio of themaximal slope observed after agonist addition/slope at 1.00-1.25min. The rapid initial efflux component (0-0.5 min) is due to washoutof extracellular 1251 (C. J. Venglarik and R.A.F., unpublished data).
90
80
70
60
50
40
30
20
10
c10
yo:lo:10
10 . __0.o 0
00.~~~~~~~~~.
0.001 0.010 0.1 1.0 10
cAMP (AM)
FIG. 3. (a) Time course of cAMP accumulation in response to 10,uM forskolin in T84 and CFPAC-1 cells. (b) cAMP-dependent PKAactivity in T84 and CFPAC-1. (c) Concentration-response relation ofPKA activity to cAMP for T84 (o) and CFPAC-1 (o) cell extracts.
Cytosolic extracts of T84 and CFPAC-1 contained similarlevels of PKA activity. A 5-fold increase in enzyme activitywas elicited by 5 ,uM cAMP in both cell lines (Fig. 3b). PKAinhibitor (21) caused a slight reduction in basal enzymeactivity and abolished the stimulation by cAMP. The con-centration-response relation between protein kinase activityand cAMP (Fig. 3c) did not differ in CFPAC-1 and T84; nosignificant differences in Vmax or Kd (the apparent dissocia-tion constant for cAMP) were observed (Kd = 0.20 jM forT84 vs. 0.23 uM for CFPAC-1). These Kd values are similaralso to those found in control (0.13 ,uM) and CF (0.14 ,uM)airway cells in primary culture (22). The findings indicate thatthe absence of an anion transport response to forskolin inCFPAC-1 cannot be related to deficient cAMP production orto an alteration in the total activity of PKA or its sensitivityto cAMP.
2
CFPAC- 1
0

Proc. Natl. Acad. Sci. USA 87 (1990) 4015
Electrophysiology. Patch-clamp techniques were used tidentify Cl- channels in CFPAC-1 cells. Channels weiactivated after patch excision by a sustained depolarizinvoltage, usually +80 mV, cytoplasmic side positive. In 26 c51 excised, inside-out membrane patches, depolarizatioinduced the activity of an outwardly rectifying anion channt(Fig. 4a). Two to four levels of single-channel current werpresent in 11 of the 26 channel-containing patches. Voltageinduced activation of outwardly rectifying Cl- channels iobserved in normal and CF airway cell membranes antserves as a positive control for the presence of channels ilkinase-activation studies (23, 24). The slope conductance othis channel was 39 ± 2 pS at 0 mV in symmetric 150 mNNaCl bath and pipette solutions, and chord conductancewere 68 ± 3 pS at +80 mV and 24 ± 1 pS at -80 mV (Fig4a). With asymmetric NaCI solutions, PNa/PC1 was 0.05 (n =2); substitution of pipette Na+ with N-methyl-D-glucamin4did not alter the current-voltage relationship. The halideanion selectivity, assessed from biionic substitution experiments (Fig. 4a) was 1 (1.7) > Br (1.4) > Cl (1.0) (n = 3). Theseproperties are identical to those reported for the outwardl)rectifying Cl- channel in the apical membranes of colonic
a
b Forsko1in
8pA
2.5 PA20 mm-c
-50 mV. C/A
+80 mV. I/O
C A23 187
WI-*+B0 mV. T/0
-80 TV. I/0
FIG. 4. (a) Current-voltage relations of the outwardly rectifyingCl- channel in CFPAC-1 recorded in the inside-out (I/O) excisedpatch configuration with NaCl (o), NaBr (A), or Nal (v) in the bath.(b) Failure of forskolin to activate Cl- channels during cell-attached(C/A) recording from CFPAC-1 (top trace), and records from aninside-out (I/O) patch after voltage activation. (c) Activation ofcurrents during C/A recording by 10FM A23187 at ±60 mV (top twotraces), and currents recorded subsequently I/O at +80 mV (bottomtwo traces). Holding voltages are given on the left. Horizontal linesdenote the closed state.
toreIgofnel
re
IdinAf
Table 1. Cl- channel activation in CFPAC-1Condition Forskolin A23187
C/A, activated by agonist 0 8I/O, activated by depolarization 4 11/O, not activated by either
agonist or depolarization 1 10Total 5 19
Results are expressed as number of membrane patches examinedunder cell-attached (C/A) or inside-out (I/O) recording conditions.Six minutes was allowed for activation. See legend to Fig. 4 for otherdetails.
A tumor (T84) cells (14) and human airway (2, 3) and sweats gland (25) cells in primary culture.
Cell-attached patches (Fig. 4b) were electrically quiet inthe absence of agonists, and five cell-attached patches re-
e mained quiet in the presence of 10 AtM forskolin (Table 1).e After patch excision to form the inside-out recording config-i- uration, Cl- channels were subsequently activated by depo-e larizing voltage (+80 mV) in four of these patches (Fig. 4b);Y one remained quiet. In contrast, 10 AM A23187 elicited Cl-c channel currents in 8 of 19 cell-attached patches (Table 1). Of
the 11 nonresponding patches, 1 was activated by depolar-ization after excision (inside-out). The cell-attached currentselicited by A23187 were typically less well defined than thoserecorded in the same patch after excision (Fig. 4c). However,these currents were never observed in the absence of iono-phore, and both inward and outward currents were observedin cell-attached recordings with N-methyl-D-glucamine chlo-ride in the pipette, a condition in which the inward currentsmust be due to Cl- flow from cell to pipette. This conclusionis supported by the 125J efflux studies (Fig. 2) and by thereversible, Ca2+-dependent stimulation of Cl- currents byA23187 and ionomycin during whole-cell recording fromCFPAC-1 (26). These results indicate that CFPAC-1 ex-presses the outwardly rectifying Cl--selective channel foundin other Cl--secreting epithelial cells and that it can beactivated by Ca2+ ionophores and depolarizing voltages butnot by cAMP-dependent agonists.DNA and RNA Analyses of the CF Genotype. The CF
genotype was assessed by amplification ofgenomic DNA andRNA via cDNA. The amplified products were transferred toNytran membranes for Southern blotting and were hybrid-ized to allele-specific oligonucleotides; the results are shownin Fig. 5. DNA samples homozygous for the normal sequenceand homozygous for the common CF mutation, a 3-base-pairdeletion, served as controls. CFPAC-1 cells are homozygousfor the common CF mutation, a deletion of three nucleotidesthat results in the absence of phenylalanine at position 508(AF5N) ofthe deduced amino acid sequence. In addition, theyexpress this mutant CF gene mRNA. The possibility ofDNAcontamination of the RNA was ruled out since no signal was
1 2 3 4 5
B
FIG. 5. Allele-specific oligonucleotide hybridization. Autoradio-graphs show the hybridization results with two specific oligonucle-otide probes. (A) The mutant (AF508) sequence is detected. (B) Thenormal DNA sequence is detected. Samples were amplified by PCR.Lanes: 1, genomic DNA control, homozygous AFSO8 mutant; 2,genomic DNA control, homozygous normal sequence; 3, CFPAC-1RNA, one round of amplification; 4, CFPAC-1 RNA, two rounds ofamplification; 5, CFPAC-1 DNA.
Cell Biology: Schoumacher et A

4016 Cell Biology: Schoumacher et al.
detected after two rounds of amplification of the RNAreaction without reverse transcriptase (data not shown).These results show that CFPAC-1 cells express the CF geneproduct and are homozygous for the common CF mutation.
DISCUSSIONPancreatic function is markedly compromised in =80% ofCFpatients (1). When compared to non-CF subjects with similartrypsin secretion rates, CF patients have reduced HCO- andCl- secretion, suggesting a primary defect in anion secretionby pancreatic duct cells (27). Recent studies ofmicroperfusedrat pancreatic ducts suggest that anion secretion across theapical membrane involves an apical Cl- conductance inparallel with Cl-/HCO- exchange (28). This combination oftransport processes exploits the inwardly directed chemicalgradient for Cl- to drive HCO- secretion via electroneutralanion exchange and regulates HCO- secretion rate by recy-cling Cl- to the lumen via a cAMP-regulated Cl- channel. Adefect in cAMP-mediated activation of apical Cl- channelswould impair pancreatic HCO- and Cl- secretion and func-tionally link the defect in CF pancreatic duct cells to the Cl-channel regulatory defect identified in airway and sweatgland cells, where transepithelial Cl- secretion is impaired.j
Studies of CF have proceeded along two parallel tracksaimed at defining the CF mutation: a molecular approach toidentify the CF gene, and a functional approach to identifythe defective gene product. Now that the gene has beenidentified (30), the CFPAC-1 cell line should be useful inproviding virtually limitless quantities of cells for furtherbiochemical and physiologic investigations of the CF defect.In addition, these cells should be useful in genetic comple-mentation experiments (31) designed to correct the CF defectin Cl- channel regulation by stable expression of the normalcounterpart ofthe CFgene. This would provide well-matchedCF and normal cell lines for detailed functional evaluation ofthe gene product and for manipulation of the Ca2+-mediatedCl- channel regulatory pathways that are not impaired byCF.The results of patch-clamp studies (24, 25) indicate that CF
Cl- channels have normal ion conduction properties andCa2+-dependent activation. This has given rise to the ideathat the CF defect may not lie in the channel itself but in amembrane-associated regulatory protein that mediates chan-nel activation by PKA (24). The likely candidate for this roleis the CF gene product, the CF transmembrane regulator(CFTR). If this is true, then the structural features necessaryfor genetic complementation of defective cAMP-dependentchannel regulation may be in place in CFPAC-1 cells sincethey express the outwardly rectifying Cl- channel and Ca2'but not cAMP-dependent regulation of channel activity.
JRecently, single-channel studies identified an outwardly rectifiedCl- channel in primary cultures of human fetal pancreatic duct (29).It was activated in excised patches by depolarizing voltages. A 5 pSCl- channel was observed frequently and its basal activity (opentime) was enhanced -3-fold by the cAMP-mediated agonist secretin.The single-channel response to Ca2l-dependent agonists was notevaluated. Inasmuch as there is no anion transport response tocAMP in CFPAC-1, we cannot compare our findings to thoseobtained from primary cultures of pancreatic duct.
We thank A. Tousson and B. R. Brinkley (Department of CellBiology and Anatomy, University ofAlabama at Birmingham) for thecytokeratin localization studies, Dr. A. Carroll (Laboratory of Med-ical Genetics, University of Alabama at Birmingham) for the kary-otype analyses, Dr. R. Greger (Albert-Ludwigs University,Freiburg, F.R.G.) for 5-nitro-2-(3-phenylpropylamino)benzoic acid,
and Dr. D. W. Landry (Columbia University) for indanyloxyaceticacid 94. This work was supported by the National Institutes ofHealth(DK38518 and DK41330), the Cystic Fibrosis Foundation, and aParker B. Francis Foundation fellowship to R.A.S.
1. Taussig, L. M. (1984) Cystic Fibrosis (Thieme-Stratton, NewYork).
2. Frizzell, R. A., Rechkemmer, G. R. & Shoemaker, R. L.(1986) Science 233, 558-560.
3. Welsh, M. J. & Liedtke, C. M. (1986) Nature (London) 322,467-470.
4. McIntosh, J. C., Schoumacher, R. A. & Tiller, R. E. (1988)Am. J. Med. 85, 592.
5. Wallace, D. H. & Hegre, 0. D. (1979) In Vitro 15, 270-277.6. de St. Groth, S. F. (1983) J. Immunol. Methods 57, 121-136.7. Fogh, J. M. & Orfoe, T. (1977) J. Natl. Cancer Inst. 59,
221-225.8. Brinkley, B. R., Fistel, S. H., Marcum, J. M. & Pardue, R. L.
(1980) Int. Rev. Cytol. 63, 59-95.9. Wangemann, P., Wittner, M., Di Stefano, A., Englert, H. C.,
Lang, H. J., Schlatter, E. & Greger, R. (1986) Pflugers Arch.407, S128-S141.
10. Landry, D. W., Akabas, M. H., Redhead, C., Edelman, A.,Cragoe, E. J., Jr., & Al-Awqati, Q. (1989) Science 244, 1469-1472.
11. Smith, P. L., Welsh, M. J., Stoff, J. S. & Frizzell, R. A. (1982)J. Membr. Biol. 70, 217-226.
12. Bradford, M. M. (1976) Anal. Biochem. 72, 248-254.13. Clegg, C. H., Correll, L. A., Cadd, G. G. & McKnight, S.
(1987) J. Biol. Chem. 262, 13111-13119.14. Halm, D. R., Rechkemmer, G. R., Schoumacher, R. A. &
Frizzell, R. A. (1988) Am. J. Physiol. 254, C505-C511.15. lannuzzi, M. C., Dean, M., Drumm, M. L., Hidaka, N., Cole,
J. L., Perry, A., Stewart, C., Gerrard, B. & Collins, F. S.(1989) Am. J. Hum. Genet. 44, 695-703.
16. Rappolee, D. A., Mark, D., Banda, J. & Werb, Z. (1988)Science 241, 708-712.
17. Lemna, W. K., Feldman, G. L., Kerem, B.-S., Fernbach,S. D., Zevkovich, E. P., O'Brien, W. E., Riordan, J. R., Col-lins, F. S., Tsui, L.-C. & Beaudet, A. L. (1990) N. Engl. J.Med. 322, 291-2%.
18. Hayakawa, T., Kondo, T., Shibata, T., Hamano, H., Kita-gawa, M., Sakai, Y. & Ono, H. (1988) Cancer 61, 1827-1831.
19. Pinto, V. B., Gelder, F. B. & Morris, D. M. (1986) Cancer Res.46, 6520-6524.
20. Cubilla, A. L. & Fitzgerald, P. J. (1984) Tumors ofthe ExocrinePancreas (Armed Forces Inst. Pathol., Washington, DC).
21. Cheng, H. C., Kemp, B. E., Pearson, R. B., Smith, A. J.,Misconi, L., Van Patten, S. M. & Walsh, D. A. (1986) J. Biol.Chem. 261, 989-992.
22. Barthelson, R. A. & Widdicombe, J. H. (1987) J. Clin. Invest.80, 1799-1802.
23. Schoumacher, R. A., Shoemaker, R. L., Halm, D. R., Tallant,E. A., Wallace, R. W. & Frizzell, R. A. (1987) Nature (Lon-don) 330, 752-754.
24. Li, M., McCann, J. D., Liedtke, C. M., Nairn, A. C., Green-gard, P. & Welsh, M. J. (1988) Nature (London) 331, 358-360.
25. Krouse, M. E., Hagiwara, G., Chen, J., Lewiston, N. J. &Wine, J. J. (1989) Am. J. Physiol. 257, C129-C140.
26. Cliff, W. H. & Frizzell, R. A. (1989) Pediatr. Pulmonol. Suppl.4, 123 (abstr.).
27. Forstner, G. G., Kopelman, H. R., Durie, P. R. & Corey,M. L. (1987) in Genetics and Epithelial Cell Dysfunction inCystic Fibrosis, eds. Riordan, J. & Buchwald, M. (Liss, NewYork), pp. 101-104.
28. Novak, I. & Greger, R. (1988) Pflugers Arch. 411, 546-553.29. Gray, M. A., Harris, A., Coleman, L., Greenwell, J. R. &
Argent, B. E. (1989) Am. J. Physiol. 257, C240-C251.30. Rommens, J. M., Tannuzzi, M. C., Kerem, B., Drumm, M. L.,
Melmer, G., Dean, M., Rozmahel, R., Cole, J. L., Kennedy,D., Hidaka, N., Zsiga, M., Buchwald, M., Riordan, J. R., Tsui,L.-C. & Collins, F. S. (1989) Science 245, 1059-1065.
31. lannuzzi, M. C., Weber, J. L., Yankaskas, J. R., Boucher,R. C. & Collins, F. S. (1988) Am. Rev. Respir. Dis. 138,%5-968.
Proc. Natl. Acad Sci. USA 87 (1990)