C. Douglas Phillips MD FACR Director of Head and Neck ... · Director of Head and Neck Imaging...
Transcript of C. Douglas Phillips MD FACR Director of Head and Neck ... · Director of Head and Neck Imaging...
C. Douglas Phillips MD FACR
Director of Head and Neck Imaging
Weill Cornell Medical College/NewYork-Presbyterian Hospital
Disclosures
Neither I nor any family members have
any pertinent financial relations of note
regarding material in this presentation
Special thanks to Dr. Deborah
Shatzkes for case material and ideas
The Orbit
Brief Anatomy
Orbital Trauma
Orbital Infectious/Inflammatory Disease
IOIS (orbital pseudotumor)
Orbital cellulitis
Vascular Lesions of the Orbit
CCF
Venous or lymphatic malformations
Differential diagnoses of orbital disease
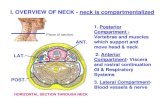
Major Anatomic Compartments
Globe
Optic nerve and sheath
Extraocular Muscles
Lacrimal Gland
Intraconal vs. Extraconal Compartment
Preseptal vs. Postseptal Compartment
Globe and Optic Nerve
Globe
Divided into anterior and posterior segments by lens
Optic nerve and sheath
Orbital (tortuous)
Intracanalicular
Intracranial or intracisternal
Intraconal Compartment
4 rectus muscles and
fibrous septa make up
muscle cone
Extraocular muscles
originate from
common tendinous
ring (annulus of Zinn)
in orbital apex
Contains optic nerve,
vessels, CN III, IV and
VI and retrobulbar fat
Extraconal Compartment
Outside muscle
cone
Between bony orbit
and rectus muscles
Contains lacrimal
gland and fat
Anterior clinoid process
Optic nerves
Superior orbital fissure
Sphenoid sinus (air filled)
Orbital Apex
Lacrimal Sac
Nasolacrimal apparatus has close relationship with ethmoid air-cells
Nasolacrimal duct
Drains into inferior meatus
Protected by bony canal
Normally may be opacified with fluid or contain air
Orbital Trauma
Fractures involving orbit are common
and can be urgent
Thin section CT with MPR is necessary
to depict and detail these fractures
Soft tissue injuries are often overlooked
but can be more serious
S/P assault w/ blunt and sharp instruments, multiple stab
wounds: ruptured globe, retinal detachment
Orbital Infectious/Inflammatory
Diseases
Infections of orbit
60% of primary orbital disease
Often complication of sinusitis
Superficial tissues most commonly
Extraconal and preseptal
Can extend and involve intraconal soft tissues and/or CNS
Immunocompromised hosts – remember fungal disease
Orbital Inflammatory Disease
Wide range of immunologic conditions
may affect orbit
Remember orbital involvement with
systemic immunologic diseases
Cross-reactivity of many immune
complexes with orbital structures
Stages of Orbital Cellulitis
Inflammatory edema/pre-septal cellulitis
Post-septal disease
Subperiosteal phlegmon/abscess
Orbital cellulitis
Orbital abscess
Ophthalmic vein and cavernous sinus
thrombosis
Pre-septal Orbital Cellulitis
Erythema, pain, conjunctivitis, blurred vision
80% <10 years of age
Staph/Strep are common organisms
Imaging: CT with contrast
indicated in patients with unreliable physical exam due to age or signs of post-septal involvement
MR if accessible
Orbital Cellulitis
Extension from periorbital structures or pre-septal infection
Mortality/morbidity very low Pre-ATBX: 17% mortality, 20% blind in affected
eye
Now estimated <1%
Complications arise from progressive disease Subperiosteal/orbital abscess (7-9%)
Ophthalmic vein/cavernous sinus thrombosis (50% mortality)
Intracranial abscess
Orbital Inflammatory Conditions
Primary considerations
Idiopathic orbital inflammatory disease
(IOID), or orbital pseudotumor
Thyroid orbitopathy
Mixed, collagen-vascular diseases, and
other orbital inflammatory conditions
○ Sjogren’s, sarcoid, etc.
○ Granulomatosis with polyangiitis (Wegener’s)
Orbital Pseudotumor
Most common intraorbital mass lesion in adults
Inflammation of ANY orbital structure of unknown cause Fat - 76%
Muscles - 57%
Optic nerve - 38%
Uvea/sclera - 33%
Lacrimal gland - 5%
Two types: Tumefactive (diffuse) and myositic
Tends towards transcompartment involvement
IOID or Orbital Pseudotumor
“Tumefactive” pseudotumor
Over 2/3rds of cases
Infiltrating more common than focal disease
75% retrobulbar, with or without muscle
cone involvement
Myositic pseudotumor
Second most common pattern
Unilateral involvement
Involves tendinous insertions
IOID or Orbital Pseudotumor
Imaging Distinguish tumefactive type from neoplasia
Distinguish pseudotumor from thyroid orbitopathy
CT
○ Intense enhancement of conal/intraconal lesions
○ Involvement of muscle tendons
MRI
○ Lesions are hypo- to isointense to fat on T2 (other neoplasia often hyperintense to fat on T2)
○ Intense enhancement
NB: Can look like ANYTHING!
Optic Neuritis
Optic nerve inflammation due to:
Demyelination (MS)
Infections: Lyme disease, TB, syphilis
Viral: HIV, HBV, herpes, CMV
50% of patients diagnosed with MS
Long term severe vision loss in 20%
Triad of symptoms: loss of vision, eye
pain, dyschromatopsia; 70% unilateral
Orbital Vascular Lesions
Cavernous hemangioma (orbital venous
malformation) is most common orbital
mass in adults
Emergent presentation may be seen
with a limited number of orbital vascular
lesions
Orbital Venous Malformation
(Cavernous Hemangioma) Most common orbital vascular lesion in adult
Classic imaging appearance in most cases 80% intraconal - usually retrobulbar
CT Homogeneous, slightly hyperdense
(microcalcifications)
Usually marked homogeneous enhancement
MR Isointense to muscle on T1
Hyperintense on T2
Patchy enhancement that may progressively opacify
Carotid Cavernous Fistula
Communication between ICA and cavernous sinus
Indirect CCF AV shunting via multiple dural arteries
○ Usually spontaneous
○ Most often in middle-aged women
Rare secondary to vascular tumor
Direct CCF Post-traumatic (arterial laceration)
Rupture of cavernous carotid aneurysm
Carotid Cavernous Fistula
Pulsatile exophthalmos, chemosis, bruit
Imaging findings
Dilatation of SOV
Exophthalmos with enlargement of EOM
Abnormal contour (bulging) of CS
CT and MR typically diagnostic
CTA/MRA superior in depiction
Catheter angiography for morphology and treatment
Observations
“Bulging” wall of
cavernous sinus
Too many flow voids
in cavernous sinus
Dilated ipsilateral
SOV
Lymphatic Malformations
Lymphocytes may proliferate during viral
infections and cause worsening
proptosis
Hemorrhage, either spontaneous or
secondary to minor trauma, is common
Results in “chocolate cysts”
Sudden proptosis, rare optic nerve
compression
Orbital Disease: Patterns
Lesion of bony orbit that involves orbit
Enlargement of the extraocular muscles
Retrobulbar mass
Retrobulbar infiltrate
Child Adult
Mets
(neuroblastoma,
sarcomas)
Leukemia/lymphoma
Rhabdomyosarcoma
Histiocytosis
Fibro-osseous lesion
Expansile PNS
process
Mets (lung, breast,
melanoma, renal)
Multiple myeloma
Meningioma
Leukemia/lymphoma
Fibro-osseous lesion
Expansile PNS
process
EOM Enlargement
Thyroid orbitopathy
Idiopathic Orbital Inflammatory
Syndrome (pseudotumor)
Metastatic disease
Infection
Lymphoproliferative disease
Vascular lesions
Retrobulbar Masses
Hemangioma
Lymphangioma
Met
Lymphoproliferative
disease
Hematoma
Schwannoma/neurof
ibroma
Rhabdomyosarcoma
Chloroma
Hemangiopericytoma
Meningioma
Optic n. lesions
Epidermoid/dermoid/
Teratoma
Orbital Infiltrative Processes
Infection
Hemorrhage
Lymphoproliferative disease
Pseudotumor
Sarcoid
Wegeners
Metastatic Disease
CCF/SOV thrombosis
Thyroid orbitopathy