AMSN Annual Discover the Possibilities Nurses as Second...The establishment of nursing theory can be...
Transcript of AMSN Annual Discover the Possibilities Nurses as Second...The establishment of nursing theory can be...

AMSN AnnualConvention: Discover the Possibilities
Nurses as SecondVictims: Peers Supporting Peers
OFFICIAL NEWSLETTER
A
Volume 26 – Number 3May/June 2017
Sheri Jacobson
WClinical nurses are often intimidated by nursing theory. Facilitating connections among theoryand practice eliminates barriers and fosters innovative advances in patient care and nursing.Empowering nurses through nursing theory applications provides solid foundations for practice.
When the phrase nursing theory is mentioned, it may elicit less than favorable responses fromclinical nurses who remember the term being elaborated upon somewhere along the continuum ofnursing school long ago, but to whom it has no relative impact on their view of practice today. It isimportant for nurses to understand the definition of nursing theory to apply it in practice and forit to make sense in their everyday nursing activities. According to CurrentNursing.com (2012):
“A nursing theory is a set of concepts, definitions, relationships, and assumptions or propo-sitions derived from nursing models or from other disciplines and projects a purposive, system-atic view of phenomena by designing specific inter-relationships among concepts for the pur-poses of describing, explaining, predicting, and/or prescribing” (para. 3).The establishment of nursing theory can be traced back to the times of Florence Nightingale,
but it came to life during the 1960-1970s (Masters, 2014) with the brainstorming and critical thinkingof early nurse theorists like Martha Rogers, Sister Callista Roy, and Dorothy Orem to name a fewof the pioneers. Examples of nursing theories that emerged during this period were Roger’s Scienceof Unitary Human Beings, Roy’s Adaptation Theory, and Orem’s Self-Care Deficit Theory.
How Can Clinical Nurses Relate Nursing Theory to Practice?Nurses, perhaps unknowingly, apply nursing theory in their daily practice. Below are a few short
scenarios demonstrating how nursing theory undergirds everyday nursing practice.Scenario 1:
A patient has recently undergone an appendectomy. On Post-Op Day 1, the nurse begins dis-charge planning and performs wound care and a dressing change. While there, the nurse educates the
continued on page 14
Economic Implications of Creating a Discharge Nurse Role on a Medical-Surgical Nursing Unit. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4Legal Nursing: Healthcare Advocates in Nursing – Benefits and Burdens. . . . . . . . . . . . . . . . . . . . 7Quality Matters: Nurses Impact Quality of Care – That’s a Good Thing, Right?. . . . . . . . . . . . . . . 8Joining Forces:A Smartphone App as Adjunctive Therapy to Help Veterans Cope with Suicidal Thoughts. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10Nutrition to Improve Outcomes: Malnutrition in the Hospitalized Patient – Helpful Resources. . . . . 16
CNE

2
Volume 26 – Number 3May/June 2017
Reader ServicesMedSurg Matters!Academy of Medical-Surgical NursesEast Holly Avenue, Box 56Pitman, NJ 08071-0056(856) 256-2300 • (866) 877-AMSN (2676)Fax (856) [email protected]
MedSurg Matters! is owned and publishedbimonthly by the Academy of Medical-SurgicalNurses (AMSN). The newsletter is distributed tomembers as a direct benefit of membership.
AdvertisingContact Rick Gabler, Advertising Representative, (856) 256-2314.
Back IssuesTo order, call 866-877-AMSN (2676).
Editorial ContentAMSN encourages the submission of news itemsand photos of interest to AMSN members. Byvirtue of your submission, you agree to the usageand editing of your submission for possible publica-tion in the AMSN newsletter, online, and in otherpromotional and educational materials.
To send comments, questions, or article sugges-tions, or if you would like to write for us, contactthe Editor at [email protected].
AMSN Publications and ProductsTo order, call 866-877-AMSN (2676), or visitwww.amsn.org.
ReprintsFor permission to reprint an article, call 866-877-AMSN (2676).
IndexingMedSurg Matters! is indexed in the CumulativeIndex to Nursing and Allied Health Literature(CINAHL).
© Copyright 2017 by AMSN. All rights reserved.Reproduction in whole or part, electronic ormechanical without written permission of the pub-lisher is prohibited. The opinions expressed inMedSurg Matters! are those of the contributors,authors and/or advertisers, and do not necessarilyreflect the views of AMSN,MedSurg Matters!, or itseditorial staff.
Publication Management is provided byAnthony J. Jannetti, Inc., which is accreditedby the Association Management Company
Institute.
Highlights• Connect with friends andinspirational nurses
• Learn from visionaryspeakers and leaders
• Relax and rejuvenate in a desert paradise

Here’s what to expect: The industry’s topspeakers who will draw waves of laughter from thecrowd, followed by deep insights that will have yourethink any practice boundaries you’ve set foryourself.
You’ll see the possibilities and recognize yourown potential. You’ll be surrounded by friends andcolleagues as you learn in a resort ringed by moun-tains.
Nothing wrong with that picture, right?
Let’s Dive In New this year is a free pre-convention work-
shop on Thursday, October 12. This interactive ses-sion, “Prepared Nurses Protect Patients: PreventionStrategies for Healthcare-Associated Infections andEmerging Infectious Diseases,” will include the lat-est information on infectious disease, disease trans-mission, and emerging threats, as well as evidence-based strategies.
The workshop is a collaboration betweenAMSN, the American Nurses Association (ANA),and the Centers for Disease Control andPrevention (CDC). Register early because seatingis limited.
The convention will officially begin later thatday with Opening Ceremonies and an OpeningAddress by Sharon Cox, MSN, RN. Ms. Cox willexplore ways to boost sagging morale and build anextraordinary practice environment in her session,“Staying Positive While Working with Pearl andGrumpy.”
Next, you’ll attend the Opening Reception,enjoy hors d’oeuvres, chat with exhibitors in theExhibit Hall, and view innovative posters by yournursing colleagues.
The next day, Peter Buerhaus, PhD, RN, FAAN,FAANP(h), one of America’s best known nursingworkforce experts, will explore “The RNWorkforce – Relationship to the Medical-SurgicalNurse and Healthy Practice Environment,” for theconvention Keynote Address.
On Saturday, be sure to attend the Town Hall,“Putting the Spotlight on You: Nurses as Leaders.”You can take the mic during the interactive discus-sion and share how you lead, mentor, and advancethe nursing profession. Summer Bryant, MSN, RN,CMSRN, will be hosting the Town Hall, which isalways one of the most popular events at the con-vention.
Concurrent sessions run throughout themeeting and include such topics as staffing, reduc-ing readmissions, obtaining quality outcomes, andmany more clinical, leadership, and managementissues.
You’ll be able to earn up to 15.25 contacthours for the full 3-day convention.
For complete details and to register, visit convention.amsn.org. If you want to save $65, markyour calendar so you don’t forget that the EarlyBird Discount ends August 14, 2017.
Questions? Call 866-877-2676 or email [email protected].
AMSN Annual Convention:Discover the Possibilities
AMSN has a convention in October designed to inspireyou personally and professionally. And better yet, it will
happen in the desert oasis of Palm Springs, CA.
To see the full program and to register, visitconvention.amsn.org

Instructions for ContinuingNursing Education Contact HoursEconomic Implications ofCreating a Discharge NurseRole on a Medical-Surgical
Nursing UnitDeadline for Submission:
June 30, 2019
MSNN1703
To Obtain CNE Contact Hours1. For those wishing to obtain CNE contact hours,
you must read the article and complete theevaluation through the AMSN Online Library.Complete your evaluation online and print yourCNE certificate immediately, or later. Simply goto www.amsn.org/library
2. Evaluations must be completed online by June30, 2019. Upon completion of the evaluation, acertificate for 1.2 contact hour(s) may be printed.
FeesMember: FREERegular: $20
Learning OutcomeAfter completing this learning activity, the
learner will be able to implement practices for safepatient handling on the medical-surgical unit thatcan prevent injuries related to patient transport.
Learning Engagement ActivityDownload and review: Centers for Medicare &
Medicaid Services (CMS). (2016). Acute inpatientPPS: Case Mix Index. Available at https://www.cms.gov/ Medicare/Medicare-Fee-for-Service-Payment/ AcuteInpatientPPS/Acute-I n p a t i e n t - F i l e s - f o r - D own l o a d - I t em s /CMS022630.html
The author(s), editor, editorial committee, con-tent reviewers, and education director reported noactual or potential conflict of interest in relation tothis continuing nursing education article.This educational activity is jointly provided by
Anthony J. Jannetti, Inc. and the Academy ofMedical-Surgical Nurses (AMSN).Anthony J. Jannetti, Inc. is accredited as a
provider of continuing nursing education by theAmerican Nurses Credentialing Center’sCommission on Accreditation.Anthony J. Jannetti, Inc. is a provider approved
by the California Board of Registered Nursing,provider number CEP 5387. Licensees in the stateof California must retain this certificate for fouryears after the CNE activity is completed.This article was reviewed and formatted for
contact hour credit by Rosemarie Marmion, MSN,RN-BC, NE-BC, AMSN Education Director.
4
Economic Implications of Creating aDischarge Nurse Role on a Medical-Surgical Nursing Unit
CNECONTINUING
NURSINGEDUCATION
Kevin ShimpBrett Neville
This article describes the impact of creat-ing a specific discharge nurse role.Expedited discharge times, improvedHCAHPS scores, and cost effectiveness aresome of the positive outcomes resultingfrom having a designated discharge nurse.
The Patient Protection andAffordable Care Act (ACA) of 2010introduced several provisions into theever-changing environment of healthcare in the United States. These provi-sions call for reforms within the health-care delivery system that expand cover-age to more Americans, increaseaccountability from health insurancecompanies, reduce healthcare costs,and increase overall quality of healthcare in America (ACA, 2010).
Quality of care in hospitals is eval-uated and reimbursed by benchmarkeddata, length of stay, unplanned readmis-sions within 30 days, and the occur-rence of preventable, hospital-acquiredconditions such as catheter-associatedurinary tract infections, central line-associated bloodstream infections, andfalls with injury. The measurable qualityindicators, as well as the patients’reported perception of their quality ofcare, present challenges. Patient satis-faction scores generally focus on thehospital discharges process, responsive-ness of staff, pain management, cleanli-ness of the environment, and amount ofwait time for a bed in an appropriatecare environment. Therefore, there isan increased need for hospitals andhealthcare facilities to operate differ-ently. Hospitals are seeking safer, time-lier, effective, equitable, efficient, andpatient-centered methods in providingcare. Several issues are identified in thepatient discharge process.
Identifying the ProblemHospitals frequently release
patients with inadequate dischargeinstructions, limited coordination ofcare by the interprofessional teams, andminimal communication of communityresources (Jeangsawang, Malathum,Panpakdee, Brooten, & Nityasuddhi,2012). The role of Clinical Coordinatorwas created at a large urban hospital inan effort to facilitate patient flow andimprove discharge outcomes. This rolewas designed to improve identified dis-charge deficiencies and improve theprocesses. As the inpatient census con-tinued to grow over time, the hospitalbegan facing limited capacity for admis-sions. This translated to patients’ lim-ited access to necessary and appropri-ate care and lost revenue to diversionhours. When delays in throughputoccurred on surgical units, patientswere often detained in recovery areasand in operating rooms. This too lim-ited patients’ access to necessary careand caused losses in revenue as surgicalcases were delayed and/or canceled.
The role of the ClinicalCoordinator is a resource that canimprove quality and patient satisfactionduring specific times of the day that areespecially turbulent with admissions,discharges, and transfers. Decreasedoperating room hold times for patientsboarding in recovery areas leads todecreased diversion hours andincreased surgical volumes, which influ-ences financial success. Turbulent/highactivity times on a unit can be assessedwith an intensity rating accounting foradmissions, discharges, and transfers.The high activity of a unit is notreflected in the midnight census, fore-going consideration of the turnover ofpatients throughout the shift.These tur-bulent times are not captured in census

5
866-877-2676 Volume 26 – Number 3
reports and do not translate to budget sheets. However, thisis a heavy workload, and the burden of the work directlyaffects the primary care nurse.
Acute Care Surgery is a 28-bed, fast-paced surgical nurs-ing unit, which averaged 125 discharges per month and 4.8discharges per day over the last five years. Responding to thecall for improved outcomes in care delivery, the leadershipteam planned to pilot the implementation of transitioning theClinical Coordinator role to an admission and dischargenurse role. The three existing Clinical Coordinators wouldcontinue their administrative role seven days per week, andthe new admission and discharge role five days per week,thereby remaining budget neutral. The plan focused on tran-sitioning the role of the Clinical Coordinator on high volumedays to facilitate admissions and discharges. This new rolewas called the admission/discharge nurse.
Success of the project was measured by increasedpatient satisfaction scores and decreased hours of the dis-charge order entry time to the time of actual patient depar-ture. Decreasing the time by one hour for each patient would
allow Acute Care Surgery to generate 62.5 additional patientdays per year, resulting in a potential revenue increase of$187,500 in additional room and board charges.
InterventionThe pre-intervention data supported the need for a
pilot. This data was presented to the Acute Care Surgeryfrontline leadership team to discuss commitment, buy-in, andestablish guidelines for the pilot. The Clinical Coordinatorsagreed to the guidelines of sharing administrative resourcesand admission/discharge role. If the pilot proved to be suc-cessful, their hours would be split between serving as theadministrative/resource Clinical Coordinator and the admis-sion/discharge nurse.
The workflow of the admission/discharge nurse includedthe following:
Ensure a provider entered a discharge order into the•patient’s medical record.
Collaborate with the bedside nurse caring for the•patient to coordinate teaching and final preparations.
Provide instruction and teaching to the patient and family.•Assess for and remove invasive lines and catheters as•ordered for discontinuation.
Secure patient belongings and discharge medications.•Facilitate safe transportation to discharge location.•For admissions, the admission/discharge nurse collabo-
rated with the hospital, sending units such as Post AnesthesiaCare Unit or Emergency Department, to ensure a safe nurs-ing care handoff. After handoff was completed, the patientwas transported to the unit, where the admission/dischargenurse provided a focused admission screening and per-formed an in-depth skin assessment. These focused assess-ments were designed to help raise awareness of skin injuriesand invasive devices present on admission. One result of col-laboration between other units was the primary nurse andthe admission/discharge nurse increased effective interpro-fessional communication and quality of care as evidenced byunit benchmarking. The workload burden of the direct carenurse was decreased during the turbulent times, allowing fora decrease in patient assignment adjustments that oftenoccurred three times a day.
ResultsThe pilot was conducted in April and May 2014, and the
admission/discharge role officially started in June 2014. Figure1 illustrates the increase in discharges from 2013 to 2015 forboth medicine and surgical service patients on Acute CareSurgery, allowing for a rebound in a decreased year of dis-charges as seen in 2013. Figures 2 and 3 illustrate that suc-cess was achieved as evidenced by an increase in medicinepatient days when compared to surgical patients and anincrease in the Case Mix Index (CMI). CMI is a form of meas-urement used to demonstrate the acuity of patients(Centers for Medicare & Medicaid Services, 2016). The busi-ness days with the most discharges were validated consis-tently since the start of the process and continued to have
!%!&$
!%&&$
!"+&$
!"*&$
!"#&$
!")&$ !"% $
!"##$
!"% $
!%&%$!%&%$
%"$%"$
,-.0123 $ $,-./01234.$56!($
!"%&$
!""&$
!"(&$
!"'&$,-./ $ $4.$56!"$ /01234.$56!%$ Discharges FY13 Discharges FY14 Discharges FY15
Figure 1.Discharges by Fiscal Year for CCH7
(+""$
('""$
(*""$
("""$
#""$
+""$
%& $
!"#$!"#$
(')($
&'$
,-./0/1-$23$4567$,-./0/1-$23$4567$,-./0/1-$23$4567$
+""$
'""$
*""$
"$
Figure 2.Increase in Medicine Patient Days by Fiscal Year
(+'!"
()'!"
(!'!"
('!"
#&'!"
#+'!"
#% '!"
#$%&'!"
()*'()*'!"
(!'
!
,-.'/0()',-.'/0($'
#)'!"
#!'!"
!'
%&'("'/0()' ,-.'/0(*'
Figure 3.Case Mix Index (CMI) by Fiscal Year for CCH7

the highest amounts of discharges and correlating admis-sions.
An increase in patient satisfaction associated with thedischarge process was not anticipated, but embraced. Asnoted in Figure 4, the three specific measurements thataddress the discharge process within the Hospital ConsumerAssessment of Healthcare Providers (HCAHP) surveys post-op are: discharge information (represented in green), helpafter discharge (represented in blue), and symptoms to mon-itor (represented in yellow). The dotted red line representsthe linear progression since the start of the process throughMarch 2015. The quality of bedside nurses’ communicationduring patient interactions addressing discharge-learningneeds is a significant predictor of the patient’s perception ofreadiness to go home (Nosbusch, Weiss, & Bobay, 2010).
The most exciting result for the team was the creationof additional hospital beds. Capacity and throughput havebeen a focal part of the Clinical Coordinator role sinceinception, with previously minimal results. The use of the newClinical Coordinator role as an admission/discharge nurseinfluenced discharges, being completed earlier in the day,allowing Acute Care Surgery to demonstrate its impact onhospital-wide diversion as depicted in Figure 5. The staff ofAcute Care Surgery immediately talked about how theycould get the discharges executed prior to noon when theysaw these results.
ConclusionDischarges and admissions may be positively affected
when designated resources are allocated (Wong et al., 2011).Many facilities do not have additional resources to allocatefor new roles; therefore, a better way to utilize existing rolesis necessary. Understanding current full-time equivalents andassessing the ability to reallocate these resources or adjust-ing skill mix to meet the demands created by the high activityof a unit is an opportunity. Challenges of establishing anadmission/discharge role include, but are not limited to, thecreation of another handoff of care, which may increase risk.Evidence in the literature speaks to communication errors
associated with handoffs in healthcare (Coleman et al., 2013).A decrease in communication leads to errors and poorpatient outcomes. When patients are not clear regardingtheir discharge instructions, an increase in readmissions mayresult (Coleman et al., 2013). The exploration of the admis-sion/discharge nurse role is warranted on units with highactivity/turbulence created by the admissions, discharges, andtransfers of patients.
ReferencesCenters for Medicare & Medicaid Services (CMS). (2016). Acute
inpatient PPS: Case Mix Index. Retrieved April 10, 2017, fromhttps://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS022630.html
Coleman, E.A., Chugh, A., Williams, M.V., Grigsby, J., Glasheen, J.J.,McKenzie, M., & Min, S.J. (2013). Understanding and executionof discharge instructions. American Journal of Medical Quality,28(5), 383-391.
Jeangsawang, N., Malathum, P., Panpakdee, O., Brooten, D., &Nityasuddhi, D. (2012). Comparison of outcomes of dis-charge planning and post-discharge follow-up care, providedby advanced practice, expert-by-experience, and novicenurses, to hospitalized elders with chronic healthcare condi-tions. Pacific Rim International Journal of Nursing Research,16(4), 343-360.
Nosbusch, J.M., Weiss, M.E., & Bobay, K.L. (2010). An integratedreview of the literature on challenges confronting the acutecare staff nurse in discharge planning. Journal of ClinicalNursing, 20(5-6), 754-774.
Patient Protection and Affordable Care Act (ACA). (2010). 42U.S.C., §18001.
Wong, E., Yam, C., Cheung, A., Leung, M., Chan, F., Wong, F., & Yeoh,E. (2011). Barriers to effective discharge planning: A qualita-tive study investigating the perspectives of frontline health-care professionals. BMC Health Services Research, 11(242), 1-10. doi:10.1186/1472-6963-11-242
Kevin Shimp, MSN, RN, CCRN, is a Nurse Manager, VCUMedical Center, Acute Care Surgery, Richmond, VA.
Brett Neville, MS, RN, CCRN-CSC, is a ClinicalCoordinator, VCU Medical Center, Clinical Transplant Center,Richmond, VA.
Academy of Medical-Surgical Nurses www.amsn.org
6
Figure 4.Patient Satisfaction Scores Based on HCAHP Reporting
&
Discharge Scorecard – C
$"'
%.-,*+
')
$%&"'#
$%&""#
&
Acute Care Surgery CCH7
&
ery
&
Oct-14 Sep-14 Aug-14
'()
&!"
#$"%
01 &,/+!-.!,&*+()
$%&!'#
$%&!"#&
Dec-14 Nov-14 ct-14
1+!,&6.!,&5+342+!,&&
Jan-15 -14
789+!:&+!,&&
16.7% 18.1% 15.1% 17.7% 13.9% 22.1% D/C after 18:00
26.5% 23.5% 19.8% 25.0% 23.8% 19.3% D/C 12:00-14:00
Figure 5.Comparison of Discharge Times:
Noon Through 2:00 p.m. vs. After 6:00 p.m.

Healthcare Advocates inNursing: Benefits and
BurdensToday, nurses are aware of the healthcare crisis and the
need for change; however, few take the time to realize howthe history of nursing has molded and contributed to thequandary that we face in today’s healthcare system. In addi-tion, nurses need to demonstrate the will, time, energy, andpolitical savvy needed to “play the game” to take on sometype of advocacy role to influence a change in policies, laws,or regulations that govern our system and in their own facil-ities (Abood, 2007).
In 1976, Jo Ann Ashley wrote Hospitals, Paternalism, andthe Role of the Nurse, in which she described the existence ofhierarchical disparities among professionals in the hospitaland the lack of respect toward nurses.Ashley wanted to givea voice to nurses. Ashley’s ideas are consistent with currentanalyses, as well as conventional wisdom, that exist in theUnited States and other Western countries, inherent system-atic problems in healthcare practice and provision (Group &Roberts, 2001). Kendig (2006) stated every day, nurses arepositioned to see not only the impact of health policy onindividual patients but also the need for more comprehensivechanges in the policies that address many health-relatedissues. In 2017, more than ever, nurses have an opportunityto assist patients in making a change to the healthcare sys-tem. Many Americans are not happy with how health care isbeing provided. Many nurses are still unhappy with con-straints applied to professional practice. Both groups are beg-ging to be heard. In the past, nurses considered whistleblow-ers put themselves at personal and professional risk.
As a whistleblower, the nurse assumes the role of ahealthcare policy advocate. This type of advocacy necessi-tates stepping beyond our own practice setting and into theless familiar world of policy and politics, a world in whichmany nurses do not feel prepared to operate effectively(Abood, 2007).Ashley (1975) stated that nurses did not wantto antagonize either doctors or hospital administrators.Ashley also felt that the lack of women in politics and pre-sentence of sexism in the hospital family influenced the socialconceptions regarding the perception of nursing (Ashley,1976).
In 2017, there is more diverse representation than anytime in history; however, more nurse representation is stillneeded. Given our history, most nurses are not surprised bydiscouraging news, such as highly variable quality of caredelivered by a system that is poorly coordinated, thus driving
7
Volume 26 – Number 3
up costs, and putting patients at risk (Schoen, Davis, How, &Schoenbaum, 2006). As challenging and time-consuming as itmay be, accepting this responsibility offers nurses the uniqueopportunity to make a difference and to have the satisfactionof being part of bringing a better healthcare system into real-ity for themselves and their patients (Abood, 2007). Not onlydoes advocacy add another dimension to our discipline, itprovides us with the power bases to make changes in today’shealthcare system and have more control over patient careand outcomes (Abood, 2007).
To effect communication, negotiation, conflict manage-ment, critical thinking, and quality care, a personal and collec-tive decision must be made to change our way of thinking.We need to focus on power and its relationship to freedom,choice, and action (Kagan, 2006). Jo Ann Ashley did not sug-gest that nurses were victims (Kagan, 2006). Ashley wantednurses to embrace the fight against the issues that dominatedsectors of health care (Kagan, 2006). Nurses who are willingto take the risk of being labeled a whistleblower by acceptingthe responsibility of a healthcare advocate will gain the satis-faction of bringing a better healthcare system into reality forthemselves and their patients (Abood, 2007). Please join mein making your voice heard. Contact your local representa-tives, become involved in your nursing organization, and gainthe satisfaction of knowing you made a difference in thehealthcare system of today.
ReferencesAbood, S. (2007). Influencing health care in the legislative arena. The
Online Journal of Issues in Nursing, 10(1), Manuscript 2.Ashley, J.A. (1975). Power, freedom, and professional practices in nurs-
ing. Superior Nurse, 6(1), 12-29.Ashley, J.A. (1976). Hospitals, paternalism, and the role of the nurse. New
York: Teacher’s College Press.Group, T.M., & Roberts, J.I. (2001). Nursing, physician control, and the med-
ical monopoly: Historical perspectives on gendered inequality in roles,rights, and practice. Bloomington, IN: Indiana University Press.
Kagan, P. (2006). Jo Ann Ashley 30 years later: Legacy for practice.Nursing Science Quarterly, 19(4), 317-327.
Kendig, S.M. (2006). Advocacy, action, and the allure of butter: A focus on pol-icy. Highlights of the Nurse Practitioners in Women's Health 8thAnnual Conference. Retrieved from http://www.medscape.org/viewarticle/523631
Schoen, S.C., Davis, K., How, K.H., & Schoenbaum, S.C. (2006). U.S.health system performance: A national scorecard. Health Affairs,25(6). Retrieved from http://content.healthaffairs.org/content/25/6/w457
Helen P. Neil, MSN, RN, CLCN, FNC, is President andOwner, Neil Nurse Consulting, LLC, and Faculty, LSU Health –School of Nursing, New Orleans, LA. She is the “Legal Nursing”Column Editor.
Legal Nursing
If you have any questions or comments regarding the “Legal Nursing” column, or if you are interested in writing, please contact ColumnEditor Helen P. Neil at [email protected].

8
Nurses Impact Quality of Care:That’s a Good Thing, Right?Just when I figured that everybody involved in the deliv-
ery of and/or recipients of health care realized the positiveimpact that nurses have on safety and quality, the newscomes out that nurses’ salaries dropped 3.1% in 2016 (Zolot,2016). Few things will make the average person (nurse ornot) crankier than a smaller paycheck. Despite an ongoingshortage of nurses, there seems to be a failure to grasp thatthe profession continues to believe itself over-worked andunder-paid. The downtrend in salaries could be associatedwith any number of current factors: discontinuation of orga-nizational bonus structures, retirement of seasoned nurses,newer nurses replacing seasoned nurses. Surely this is notthe best strategy for encouraging a new generation to jointhe profession.
To figure out how we got here, we need historical per-spective.The evolution to the modern nurse has been a slowand rather painful process. We are all versed in the angelictales of ancient nurses: Florence Nightingale, the historic“Lady with the Lamp,” who transformed the quality andsafety of nursing and hospital care by using the then fledglingscience of statistics (Woodham-Smith, 1951); Clara Barton,the Civil War Angel of the Battlefield; and Margaret Sanger,the founder of Planned Parenthood; among many other prac-titioners who have paved our course.
Nurses have, for decades, battled the paternalistic influ-ence existing in health care. Envision the days of old whennurses got up from their chair so that the esteemed physiciancould rest his weary whatever. Think of the days when wewere considered only in terms of stereotypes: Dickens’boozy Sairy Gamp, the long-suffering handmaiden, the crone,the sexy nymphet waiting to marry the doctor, nurse ratchet,white stockings, and white polished shoes.We were paid lit-tle and asked to dedicate our caring souls to serving others.Angels of Mercy required few earthly possessions I suppose.Of course, in those days, there were few options for womento pursue when seeking a career opportunity – nurse, nun,teacher, prostitute, housewife; that was pretty much thescope of available career opportunities for women.
Today, our patrons of quality and safety include theoristsaplenty, and the likes of Patricia Benner, Linda Aiken, andLoretta Ford. Benner is revered for her devotion to the edu-cation of nurses. Aiken has produced much evidence regard-ing the correlation between staffing, nursing education levels,
and patient outcomes (Morin, 2012). The co-founder of theNurse Practitioner movement, Loretta Ford, actually soughtto expand the role of Public Health Nurses and well-babycare (Advance Healthcare Network for NPs and PAs, 2015).
With the profession’s progression, better education,technology, a livable wage, and more respect, why are we stillso under-valued? Maybe, because no matter what we want tothink, nurses continue to sit at the back of the health carebus. A 2014 National Quality Forum (NQF) publicationdescribing Person- and Family-Centered Care CoreConcepts does not acknowledge the contribution nursesmake daily, engaging patients and their families. Seriously, ifthe nation’s standard bearer in health care quality and safetycannot utter the words “Registered Nurse” as we worktoward achieving the goal of engaging patients in their owncare, then we must recognize the gap between public percep-tion, colleague conceptualization, and the reality of the con-tributions made by the medical-surgical nurse in practice.
There was an old rhyme that my daddy used about hiswork, and I carried it with me when I first started nursing(back in the old ‘let me get the doctor’ era):
It’s not my job to drive the trainThe whistle I cannot blowIt’s not my job to say how farThe train’s allowed to goIt’s not my job to blow off steamOr even ring the bellBut let the damn thing jump the trackAnd see who catches hell
– Author unknownIf we remember that our system was designed to hold
us responsible for outcomes but also to thwart our effortsto practice autonomously, then we understand not just thissimple poem but also why nurses are often unnamed or sim-ply part of the team and ambiguous hospital staff. “Nursingcare is an integral part of patient care processes in the acutehospital environment. Research in the past decade has beenundertaken to develop an evidence base for the relationshipbetween patient outcomes potentially sensitive to nursing(OPSN) and nurse staffing in the acute inpatient setting”(Joint Commission, 2009, NSC-1-1). Nurse-sensitive care(NSC) performance measures include (but are not limitedto): falls with injury, hospital-acquired pressure ulcers,restraints, central line-associated bloodstream infections(CLABSIs), and catheter-associated urinary tract infections(CAUTIs) (Joint Commission, 2009). We are charged withreducing patient readmissions, obligated to provide educa-tion and wellness counseling, and we own patient and familyengagement as well as patient satisfaction. If we bear respon-sibility for outcomes, then we need to strive harder toachieve bedside leadership, organizational acknowledgement(that includes monetary recognition), and collegial accept-ance for the role we play.
Practice ownership is essential to advancing personal, pro-fessional, and organizational goals. So what is the nurse to do?
Quality Matters
If you have questions or comments regarding the "Quality Matters" column, or if you are interested in writing, please contactColumn Editor Marguerite Windle at [email protected].

9
866-877-2676 Volume 26 – Number 3
Join a nursing organization or two.•Historically, nursing specialties with strong membership•exert power. Have you ever wondered why ICU nursescare for two patients? The American Association ofCritical-Care Nurses, founded in 1969 and now withover 100,000 members, has provided enough support-ive evidence to maintain unit-based staffing levels.Every nurse is at the core a medical-surgical nurse.The•Academy of Medical-Surgical Nurses (AMSN) is cele-brating its 25th year as a nursing organization.The AMSNsupports safe, high quality patient care and professionaland personal development.
Earn your specialty certification.•Certification is a demonstration of the individual nurse’s•commitment to lifelong learning and achieving acknowl-edgement by the certifying body as to clinical compe-tence. Certification requires ongoing education formaintenance of certification, which encourages the sus-tentation of clinical excellence.Earning certification reaffirms your commitment to•nursing as a profession. Plus, it makes you feel great!
Volunteer to serve your nursing organization.•Whether your volunteerism is at a chapter or organi-•zational level, volunteers are essential to actualization ofthe organization’s stated mission.Volunteer work is an opportunity to meet other like-•minded nurses and expand the professional experience.
Volunteer for organizations to serve others.•The American Red Cross provides services to mitigate•suffering post-disaster, as well as general nursing.Some organizations, whether faith-based or globally•developed, provide nurses the opportunity to renderaid to the less fortunate.
Continue education with vigor.•Get inspired by attending an education conference. An•education conference is an opportunity to meet nurseswith similar practice experiences across the country. Advance your degree. Nurses returning to university•need not commute to a brick and mortar campus.Online courses are available to earn a BSN, MSN, andNP, for instance.
Become political. Ferret out issues locally and nationally•that impact nurses and take a stand. Imagine what wouldhappen if every RN in the United States, all 3 million plus,contacted their members in the House of Representativeand the Senate and demanded that action be taken onexisting bills regarding staffing levels (Bureau of LaborStatistics, 2015).
The Registered Nurse Safe Staffing Act of 2015 [H.R.•2083 / S.1132] introduced to Congress in 2015(Congress.gov, 2015)H.R. 2083 – Currently in the House Ways and Means•Committee – Subcommittee Health (Congress.gov,2015)
S.1132 – Currently in Senate Finance Committee•(Congress.gov, 2015)Only fourteen states have passed any type of legislation•regarding nurse:patient ratios or nurse-driven staffinglevel (American Nurses Association, 2017)
Transformational leadership/clinical leadership are not just•for nurses in organizational management.
Lead by example.Always do the right thing for the right•reason. Don’t cut corners when nobody is looking.Clinical leaders have an awareness of external forces•driving health care, especially as they relate to directpatient care. Our health care environment is continuallyin a state of flux, which precipitates organizationalchanges. Cognition of the external factors that fomentthe internal care environment can help reduce stress byproviding an understanding of the need for change.
Nurses impact quality and safety. Nurses by nature arecreative, imaginative, and motivated to provide excellentcare. As we increase participation in the global essence ofnursing, we feel more in control of our practice. Doors openbeyond, which is opportunity. That’s a good thing!
ReferencesAdvance Healthcare Network for NPs and PAs. (2015). Q&A with
Loretta Ford. Retrieved from http://nurse-practitioners-and-physician -assistants.advanceweb.com/Features/Articles/QA-with-Loretta-Ford.aspx
American Nurses Association (ANA). (2017). Nurse staffing. RetrievedMarch 13, 2017, from http://www.nursingworld.org/ MainMenuCategories/ThePracticeofProfessionalNursing/Nurse- Staffing
Bureau of Labor Statistics. (2015). Occupational employment statistics:Registered nurses. Retrieved March 13, 2017, from https://www.bls.gov/oes/current/oes291141.htm
Congress.gov. (2015). H.R. 2083 and S. 1132 – Registered Nurse SafeStaffing Act of 2015. Retrieved from https://www.congress.gov/bill/114th-congress/house-bill/2083
Joint Commission, The. (2009). Implementation guide for the NQFendorsed nursing-sensitive care measure set. Oakbrook Terrace, IL:Author.
Morin, K.H. (2012). Linda Aiken: Improving health care outcomesthrough research (Part One). Reflections on Nursing Leadership,38(1).
National Quality Forum (NQF). (2014). Patient and family engagementaction pathway: Fostering authentic partnerships between patients,families, and care teams. Washington, DC: Author.
Woodham-Smith, C. (1951). Florence Nightingale. New York: McGraw-Hill Book Company, Inc.
Zolot, J. (2016). Salaries for nurses decrease, while NP salaries rise.American Journal of Nursing, 116(11), 16.
Marguerite Windle, MSN, RN, CMSRN, is an independentcontractor providing Clinical Nursing Education and LegalNurse Consultant services in eastern PA. She is the AMSNCoordinator for the National Quality Forum (NQF) and theNursing Alliance for Quality Care (NAQC), and the “QualityMatters” Column Editor.

Joining ForcesVisit amsn.org/joiningforces for more information oncaring for the unique needs of members of the military.
If you have questions or comments regarding the “Joining Forces” column, or if you are interested in writing, please contactColumn Editor Patricia J. Bartzak at [email protected].
Approximately 22 United States (U.S.) veterans commitsuicide each day, totaling about 8,000 deaths per year(Veterans Administration [VA], 2016). Veterans account for18% of all suicides in the country, yet they make up only 8.5%of the population (VA, 2016). Suicide is a complex event, and,in the veteran population, is often precipitated by wartimeexperiences, head injuries, and complicated survivor guilt. Assome veterans struggle with depression and post-traumaticstress disorder, thoughts can turn to hopelessness and self-harm. There has been some success with talk therapy, specif-ically cognitive behavior (CBT), and dialectical behavior ther-apies (DBT). CBT taps into the veteran’s cognitive abilities toacquire new behavioral techniques to enhance coping whensuicidal thoughts are present (Bush et al., 2015). DBT is moreproblem-focused and seeks to help the veteran develop adistress-tolerant approach to self-harming thoughts (Bush etal., 2015).
Talk therapy occurs within the therapeutic relationshipin the clinical setting. The risk for veteran suicide duringactive talk therapy is less than when the veteran leaves theappointment and is on his/her own, whether with family orworking, or just living life. It is during these times away fromthe therapeutic clinic setting that the veteran may experiencenegative thoughts, stress, and even suicidal thoughts and/orplans (Bush et al., 2015).
Prior to the digital age, some mental health therapistswould help their depressed and/or suicidal patients developa conventional hope box (CHB) (Bush et al., 2015). A CHB isa shoebox filled with items reminding the client why it wasimportant to live rather than die. Such items might include aflower from a wedding, a meaningful photograph, a lock ofhair from a child’s head, or a poem written years ago. Bushand colleagues (2015) remind us that depressed and suicidalpeople can name several reasons to die but find it difficult torecall even one reason to live.
In 2013, Bush and colleagues opened a randomized, con-trolled, 12-week study at the VA in Portland, OR, to test thehypothesis of a Virtual Hope Box (VHB). A VHB is similar tothe CHB, but is available on hand-held electronic devices(ClinicalTrials.gov, 2013). The phone app was developed inconjunction with the Department of Defense NationalCenter for Telehealth and Technology (Anderson, 2016). Thestudy selected U.S. veterans who were in active talk therapyand who had been identified as being at risk for suicide.Veterans with dementia, terminal illness, inpatient status, orunder guardianship were excluded from the trial
(ClinicalTrials.gov, 2013). The purpose of the study was toprovide participants with a customizable phone app consist-ing of icon selections similar to those categories found in theconventional hope box. The veteran could click the phone-based icons when self-harming or when suicidal thoughtsoccurred (Anderson, 2016).At the top of the app is a headingwith support phone numbers for veterans to click when incrisis to connect with a trained mental health therapist(Anderson, 2016). The five main icons are: Remind Me,Distract Me, Relax Me, Inspire Me, and Coping Cards (Bushet al., 2015).
The Coping Cards function allows the veteran torewrite positive mantras in response to negative thoughts.For example, if the veteran feels that a job is overwhelmingand difficult, he or she can type something like, “vacation in 2weeks,” “seeing my best friend on Friday night,” etc. Similarly,the Inspire Me icon can be preloaded with inspirationalquotes, such as a cherished phrase from a loved one like,“Don’t give up, when a door closes, a window opens.” TheRelax Me icon can be customized with deep breathing toolsand muscle relaxation that allow the user to select the timingand duration for inhalation, holding, and exhalation.Importantly, goal-directed thinking demonstrates future plan-ning, an important aspect of averting suicide, as belief in thefuture is an internal representation of hope (Sun & Shek,2012). The Distract Me function has a place for an activityplanner, which consists of a calendar for important futureevents such as “daughter’s ballet show.” The phone app doesnot require an internet connection to work and is encryptedat the military level to ensure confidentiality. Additionally, theapp is meant to work as adjunctive therapy with talk therapyand not to be used as a standalone product (Bush et al.,2015).
The idea of the VHB is to provide veterans strugglingwith negative self-talk a way to quickly recall previous suc-cesses, positive life experiences, past successful coping meth-ods, depictions of treasured relationships, meaningful musicselections, and distraction activities. Cell phones are ubiqui-tous throughout American society, including with most vet-erans, making downloading the app simple for most. The clin-ical trial reported that the phone app helped veterans over-come disturbing thoughts and that the phone app provided ameans of distraction, relaxation, and inspiration (Anderson,2016). Various statistically reliable and valid tools were usedto measure study outcomes including the Coping Self-Efficacy Scale, Beck Scale for Suicidal Ideation, and the Brief
10
A Smartphone App as Adjunctive Therapy to Help Veterans Cope with Suicidal Thoughts

11
866-877-2676 Volume 26 – Number 3
Reasons for Living Inventory (Anderson, 2016). Overall, thestudy showed that the phone app, when used as adjunctivetherapy with talk therapy, was effective in helping veteransbetter cope with negative thoughts and stress (Bush et al.,2015). Veterans in the study commented that a limitation ofthe phone app was that it didn’t convey the same smells andtextures as experienced with a CHB (Anderson, 2016).
The VHB is based on a pre-digital age modality of a shoe-box filled with personal items that help the depressed or sui-cidal person re-connect to the positive people and things intheir life. The concept of a life’s collage, so to speak, even inits creation by the individual, requires thought and positiveemotion. Such uplifting reminders help our veterans remem-ber at least one reason to live – a pet, a grandmother’sfavorite saying, sounds of the ocean, a photo of one’s child, oreven a dog tag representing survival. When such ideas canquickly and easily be brought to the forefront of the veteran’smind, as with the click of a phone app, then there is theopportunity to reshape thoughts, and ultimately, behavior,especially in the absence of a clinical therapy session. Hope isan elusive concept: powerful but difficult to operationalize. AVirtual Health Box is a new tool on the horizon to help aug-ment mental health therapy to reshape thoughts to promotegood coping skills in our nation’s veterans.
Though the VHB app is not currently available for wide-spread use, bedside nurses can view the prototype by view-ing Dr. Bush’s slide deck (Bush, 2016). As bedside nursesdeliver care, the principles of hope explored in this articlecan be shared within the context of the therapeutic relation-ship.
ReferencesAnderson, P. (2016, November 24). ‘Virtual hope box’ delivers real results.
Retrieved from http://www.medscape.com/viewarticle/872382Bush, N.E. (2016). An improved virtual hope box [PowerPoint slides].
Retrieved from https://msrc.fsu.edu/funded-research/improved-virtual-hope-box
Bush, N.E., Dobscha, S.K., Crumpton, R., Denneson, L.M., Hoffman, J.F.,Crain, A., … Kinn, J.T. (2015).A virtual hope box smartphone appas an accessory to therapy: Proof-of-concept in a clinical sampleof veterans. Suicide and Life-Threatening Behavior, 45(1), 1-9.
ClinicalTrials.gov. (2013). Virtual hope box – Effectiveness of a smartphoneapp for coping with suicidal ideation (VHB-RCT). Retrieved April 6,2017, from https://clinicaltrials.gov/ct2/show/NCT01982773
Sun, R.C., & Shek, D.T. (2012). Beliefs in the future as a positive youthdevelopment construct: A conceptual review. The Scientific WorldJournal, 1-8.
Veterans Administration (VA). (2016, July 6). VA suicide prevention pro-gram: Facts about veteran suicide. Retrieved fromhttps://www.va.gov/opa/publications/factsheets/Suicide_Prevention_FactSheet_New_VA_Stats_070616_1400.pdf
Patricia J. Bartzak, DNP, RN, CMSRN, is a Clinical Nurse,Burn/Trauma Unit, Brigham & Women’s Hospital, Boston, MA.She is the “Joining Forces” Column Editor.
Become Certified inCare Coordination and Transition
Management (CCCTM™)
The CCCTM credential is the FIRST validation of RN carecoordination and transition management (CCTM).
CCCTM is the result of a collaboration of the Medical-Surgical Nursing Certification Board (msncb.org) and the American Academy of Ambulatory Care Nursing (aaacn.org).
Learn more at msncb.org or call MSNCB at 866-877-2676.
The challenge: Health care today is fragmented.Patients are falling through the cracks. Costs areclimbing.
The solution: Effective care coordination by acertified nurse.
The pivotal role: You, the RN, leading aninterprofessional team.
The outcome: Patients receive the right care, atthe right time, by the right health careprofessional.
You’re the missing piece in coordinated patient care

www.amsn.org
12
Nurses as Second Victims:Peers Supporting Peers
According to a 2013 report from the Lucian LeapeInstitute at the National Patient Safety Foundation, in orderto provide the safest and most effective care of patients, thehealthcare provider must 1) feel safe from physical and psy-chological harm and 2) be able to find joy and meaning intheir practice. While creating this culture is challenging atbest, nothing is more detrimental to a healthcare providerthan an adverse event, especially one that leads to litigationor a board complaint. In 2000, Wu contended that while apatient may be harmed with a medical error, the doctor isalso wounded by the same error; they are the second victim.It is at this time in a person’s career that it becomes difficultto even function, let alone find any joy or meaning in one’scareer. Most often, second victims experience feelings ofshame, fear, anger, guilt, self-doubt, and isolation. These feel-ings can lead to emotional incapacity, depression, burnout,impaired clinical care, drug or alcohol use, and even suicide.Physical symptoms and social avoidance are also possible. Incases of serious adverse events, the long-term consequencescan even mirror post-traumatic stress disorder (Edrees,Paine, Feroli, & Wu, 2011).
In a survey of 3,100 physicians, 81% of those who hadbeen involved in a clinical incident experienced some degreeof emotional distress (Pratt & Jachna, 2015). This research ledPratt and Jachna to further define second victim as “any cli-nician who experiences significant emotional distress due tothe course of clinical events” (p. 56).While much of the earlyresearch on second victim focused on physician colleagues, itwas also found that nurses have a high risk for second victim-related harm because of the amount of time spent caring forpatients and the number of medications administered(Quillivan, Burlison, Browne, Scott, & Hoffman, 2016).Medication errors are one instance of second victim-relatedharm experienced by nurses. Most authors agree that health-care systems have a responsibility to care for second victimsand that there are few structured emotional support serv-ices for care providers.
Early pioneers addressing second victim, such as KaiserPermanente, found that the stigma attached to accessingEmployee Assistance Programs and mental health servicesprevented care providers from utilizing those services (VanPelt, 2008). Fears regarding poor performance appraisal, pos-sible litigation, or a report to the licensing board may alsoprevent victims from seeking emotional support. Victimsoften did not know who it was safe to talk to and what they
could discuss. Recognizing the needs and the barriers, healthcare organizations began creating innovative support systemsfor caregivers such as the Brigham and Women’s Hospital,where they formalized a Peer Support Team to pair secondvictims with a trained peer support person with a commonclinical background (Van Pelt, 2008).
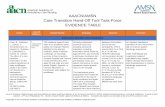
Stages of Recovery After an AdversePatient Event
University of Missouri Health Care added two items totheir internal patient safety culture survey to discover theneeds of their organization in relation to second victim. Itwas found that 175 out of 1,160 respondents had experi-enced a patient safety event that caused personal distress.This was described as “anxiety, depression, or concernsabout one’s ability to perform one’s job” (Scott, Hirschinger,Cox, McCoig, Brandt, & Hall, 2009, p. 325). In addition, 68%reported they did not receive institutional support with thisstress. In follow-up qualitative interviews with nurses, doc-tors, and other caregivers, six stages of recovery were delin-eated after an adverse patient event (see Table 1).
InterveningEarly training for the Peer Support Teams was based on
critical incident response and psychological first aid (Van Pelt,2008). The team was taught to listen, assess, and when nec-essary, refer to the next level of care. Psychological first aidpotentially decreases the risk of error through nervous sys-tem re-regulation after an unforeseen event. In addition, theongoing peer support after a bad outcome, claim, litigation,or board complaint provides a confidential means to verballyprocess the event and its effects. Both support the provider’sinherent resilience (Trent et al., 2016).
More resources continue to become available. In 2011,the World Health Organization published Psychological FirstAid: Guide for Field Workers. In 2014, the American Associationof Nurse Anesthetists published recommendations andresources for a critical incident stress management programthat allows for support during and more importantly, for aslong as necessary, after a critical adverse event. For thoseorganizations wanting to create their own primary and sec-ondary victim support program, Medically Induced TraumaSupport Services has a toolkit that can be accessed atwww.MITSS.org.
Evaluating the Effectiveness of PeerSupport Teams
In 2016, Trent and colleagues published a qualitativestudy highlighting the benefits support participants receivedfrom the peer support program, “SWADDLE,” in the BaylorScott and White healthcare system. In that study, the termhealth care adversity was coined and is defined as “difficult dis-closures, depositions, claims, lawsuits, and licensingboard/agency complaints” (Trent et al., 2016, p. 28).
HealthyPRACTICE ENVIRONMENTS
If you have any questions or comments regarding the “Healthy Practice Environments” column, or if you are interested inwriting, please contact Column Editor Debra Kahnen at [email protected].

Participants found it most useful to talk to respected peerswith similar training who could really understand and giveperspective to the experience of the event. The participantsalso reported it was useful to have preemptive educationregarding risk management and the legal processes. Bad out-comes, with or without medical error, are open to litigation.Due to how the SWADDLE volunteers are selected andtrained, the participants appreciated the fact that the com-munication is truly confidential peer support withoutrecords. The study also identified a need for further researchin the area of board complaints and the effects on providers,particularly in those states that have seen a sharp increase inboard complaint numbers since tort reform.
Supporting Each OtherWhile a formal peer support team is ideal, not all health-
care providers have access to a formal program. Mostauthors agree that the first response would be to genuinelyexpress care and concern by asking the person, “How are
you?” Peers should be taught how unhelpful and insensitivecomments can inflict further harm. Nurses frequently giveeach other psychological first aid. They talk to each other inthe medication room, the break room, and in the parking lot,offering encouragement and support to each other. Simple,more effective communication tools can be taught throughin-services and onboarding. Proper tools can improve theeffectiveness of how nurses support each other through thestressful and emotional mine field that is today’s medical-surgical nursing unit. It is equally important to educate on“second victim” and provide numbers and resources avail-able should emotional distress be encountered. Root causeanalysis can also be used as an opportunity to identify poten-tial second victims who might need attention.
Building on What We LearnedTragic and unexpected outcomes are part of health care.
Scott (2015) encourages organizations to create formal sup-port programs to prevent the long-term personal sufferingthat may cause some nurses to leave the profession. Mostwork being done on second victim focuses on traumatic, life-changing events; however, work is also being done on the per-sonal distress that builds up over time and leads to burnout.One study (Lewis, Baemholdt, Guofen, & Guterbock, 2015)found a relationship between RN involvement in adverseevents and burnout, including burnout domains of emotionalexhaustion and depersonalization. In addition, the same studyfound that giving support to RNs could be beneficial in pre-venting the emotional exhaustion and depersonalization. Inanother study of 358 nurses, Quillivan and colleagues (2016)found that a non-punitive response to error was significantlyassociated with reductions in several dimensions of secondvictim distress. The authors suggest that reducing punitiveresponse to error and encouraging supportive interactionscould lessen the severity of the second victim experience.Aculture that looks at errors as learning experiences and pro-vides supportive peer and management relationships couldmore adequately prepare and preserve the integrity of thenursing work force. While most state boards and organiza-tions require documentation of errors, the conversationcould be supportive and one that focuses on learning andprofessional growth, reducing the adverse effects of shameand guilt.Additionally, resilience training can improve the abil-ity to bounce back after stressful or adverse events areencountered in health care. Building resilience will be dis-cussed in the next “Healthy Practice Environments” column.
ReferencesAmerican Association of Nurse Anesthetists. (2014). Guidelines for crit-
ical incident stress management. Retrieved December 22, 2016,from http://www.aana.com/resources2/professionalpractice/Pages/Guidelines-for-Critical-Incident-Stress-Management.aspx
Edrees, H.H., Paine, L.A., Feroli E.R., & Wu, A.W. (2011). Health careworkers as second victims of medical errors. Polskie ArchiwumMedycyny Wewnetrznej, 121(4), 101-108.
Lewis, E.J., Baemholdt, M.B., Guofen, Y., & Guterbock, T.G. (2015).Relationship of adverse events and support to RN burnout.Journal of Nursing Care Quality, 30(2), 144-152. doi:10.1097/NCQ.0000 000000000084
13
866-877-2676 Volume 26 – Number 3
Source: Adapted from Scott, Hirschinger, Cox, McCoig, Brandt, & Hall,2009.
Stage 1: Chaos and accidentresponse
In this stage, the victim may feelunable to think coherently andneed peer support.
Stage 2: Intrusive reflections In this stage, the victim’s mindplagues them with re-enact-ments, “what if” questions, andfeelings of inadequacy.
Stage 3: Restoring personalintegrity
In this stage, support is soughtout.
Stage 4: Enduring the inquisition In this stage, there is fear aboutjob security, license repercus-sions, and fear of future litigation.The person is still struggling withtrust and what others thinkabout them. This stage can becomplicated with negative gossip.
Stage 5: Obtaining emotionalfirst aid
Anxieties at this stage are aboutwho is a safe person to confidein. Many felt that “where to goand what could be said” werenever clear.
Stage 6: Moving on Three pathways to moving onwere identified: dropping out,surviving, and thriving. Droppingout is defined as changing eitherprofessional role or location orleaving the profession alltogether. Surviving is defined asdoing alright, but still beingplagued by the event. Thriving iswhen victims have had insightsand feel they have become betterpeople as a result of the incident.
Table 1.Stages of Recovery Following Adverse Patient Events

Academy of Medical-Surgical Nurses www.amsn.org
14
Lucian Leape Institute. (2013). Through the eyes of the workforce: Creatingjoy, meaning, and safer health care. Boston: National Patient SafetyFoundation. Retrieved from http://www.npsf.org/ ?page=throughtheeyes
Pratt, S.D., & Jachna, B.R. (2015). Care of the clinician after an adverseevent. International Journal of Obstetric Anesthesia, 24(1), 54-63.doi:10.1016/j.ijoa.2014.10.001
Quillivan, R.R., Burlison, J.D., Browne, E.K., Scott, S.D., & Hoffman, J.M.(2016). Patient safety culture and the second victim phenomenon:Connecting culture to staff distress in nurses. Joint CommissionJournal on Quality & Patient Safety, 42(8), 377-386.
Scott, S.D., Hirschinger, L.E., Cox, K.R., McCoig, M., Brandt, J., & Hall,L.W. (2009). The natural history of recovery for the healthcareprovider ‘second victim’ after adverse patient events. Quality &Safety in Health Care, 18(5), 325-330. doi:10.1136/ qshc.2009.032870
Scott, S.D. (2015). The second victim experience: Mitigating the harm.American Nurse Today, 10(9), 8-11.
Trent, M., Waldo, K., Wehbe-Janek, H., Williams, D., Hegefeld, W., &Havens, L. (2016). Impact of health care adversity on providers:Lessons learned from a staff support program. Journal ofHealthcare Risk Management, 36(2), 27-34. doi:10.1002/jhrm.21239
Van Pelt, F. (2008). Peer support: Healthcare professionals supportingeach other after adverse medical events. Quality & Safety in HealthCare, 17(4), 249-252.
World Health Organization. (2011). Psychological first aid: Guide for fieldworkers. Retrieved from http://www.who.int/mental_health/publications/guide_field_workers/en/
Wu, A. (2000). Medical error: The second victim. The doctor who makesthe mistake needs help too. British Medical Journal (InternationalEdition), 320(7237), 726-727.
Debra Kahnen, BSN, RN, CMSRN, is a Nursing Supervisor,Baylor University Medical Center, Dallas, TX. She is the “HealthyPractice Environments” Column Editor.
Maxine Trent, MS, is Program Director, SWADDLE, a peersupport program for health care adversity, Baylor Scott andWhite Health.
patient about keeping the wound clean and dry. The nurseinstructs the patient to breathe deeply, cough, and turn to pre-vent complications of pneumonia. The nurse assists the patientto the chair while making the patient’s bed.The nurse developsa plan with the patient that the patient will participate in thedressing change and move ‘from bed to chair’ on Post-Op Day2. Which nursing theory can you think of that would supportthe nurse’s activities and patient interactions? This is a demon-stration of Dorothy Orem’s Self-Care Deficit Theory. Thenurse is moving the patient from a stance of dependence toone of more independence along the health continuum.Scenario 2:
A couple is vacationing at the beach with their 10-year-old daughter when she is attacked by a shark. Unfortunately,the girl loses her left arm in the encounter, but she survivesa nearly fatal event. Surgical repair is required for the remain-ing bud of the limb. After several days of recovery, despite atraumatic event, the youth has a positive attitude and desiresto begin ambulation by walking up and down the halls of thepediatric unit.The nurse recognizes that the patient’s balancemay be altered and offers to accompany her. The patientambulates very well without any instability of gait and ven-tures into the teen room to obtain some books to read.Which nursing theory would capture the overall patient sce-nario? Sister Callista Roy’s Adaptation Theory can be appliedto this patient scenario. Roy's theory stated that in order fora person to respond positively to environmental changes orchallenges, adaptation must occur (Roy, 1984). The girldemonstrated positive adaptation to a life-changing event –the loss of a limb.Scenario 3:
An older adult is diagnosed with stage 4 liver carcinoma.The family is in the room, and the atmosphere is solemn.Thenurse comes into the patient’s room to see if anything isneeded. The nurse feels that she would like to do somethingto change the energy in the room and thinks to herself,“What could that be?” She shares with the family that shecan bring several recent comedy DVDs into the room for thepatient and family if they would like to watch movies. Thepatient perks up and states that he would like to see somemovies. Suddenly, the room feels like a cloud has been lifted;the energy has changed. When talking about energy, MarthaRoger’s Science of Unitary Human Beings may come to mind.Everything has a pattern, and interactions are patterns in andof themselves. Through the nurse’s interaction, the environ-mental pattern changed to a more positive one (Newman,1999).
As exemplified in these scenarios, nursing theory doesindeed weave into the activities of everyday nursing practice.The question that remains is: How can we bring the aware-ness of the underpinnings of nursing theory to the forefrontso that bedside nurses can become inspired and build uponthe theoretical knowledge of the nursing theorists?
Building Bridges from Theory to Practicecontinued from page 1
• Triad Team Nursing – An Overview Of a Pilot Hybrid Staffing Model
• Nursing Students Having a Voice in Medical-Surgical Units
• Fighting the Flames of Nursing Burnout
• The Importance of Certification: Cost as a Barrier
• End-of-Life Care in a Medical-Surgical Setting
CNE
Coming soon in…

Empowering Clinical Nurses with TheoryFraming nursing theory and conveying its applicability to
daily nursing practice facilitates the engagement of bedsidenurses. One way to accomplish this is to present opportuni-ties where nurses can experience for themselves the benefitsof theory in practice. Many institutions have adopted nursingtheorists’ conceptual frameworks and integrated them withintheir foundational philosophies.An example of nursing theorybeing introduced into operations of the nursing departmentoccurred when “Senior nursing executives in a Chicago-basedhealthcare system comprising eight hospitals decided that anew standardized nursing philosophy would be adopted foruse by all facilities” (Rosenberg, 2006, p. 53). The nurse exec-utives conceded that “…nursing theory should be part of thenursing philosophy and determined that the organization’smission and core values were congruent with Watson’sTheory of Caring” (Rosenberg, 2006, p. 53).
Building Theoretical Models That HelpGuide Practice
Encouraging clinical nurses to participate in theory build-ing through developing theoretical models is an innovative andexciting modality to gain interest, support, and contributionsfrom nurses who apply critical thinking skills, clinical reasoning,problem-solving, and high-level communication skills in everyactivity they do. Linking the connections between practice andtheory will provide opportunities for bedside nurses to recog-nize the value of theory and its vital role in advancing bothpatient care and nursing science. An instrumental example ofhow theory building can impact nursing and patient care in atransformational manner is the ACE Star Model of KnowledgeTransformation (Stevens, 2004). According to Stevens (2013),the model was “…developed to offer a simple yet comprehen-sive approach to translate evidence into practice.” Asexplained in the ACE Star Model, “one approach to under-standing the use of EBP in nursing is to consider the nature ofknowledge and knowledge transformation necessary for utilityand relevance in clinical decision-making” (Stevens, 2013).Additionally, theory building provides an avenue to empowernurses within the profession to acquire a ‘sense of accomplish-ment’ from an activity once viewed as negligible but which nowhas the potential to provide connections for an infinite numberof applications in nursing.
In conclusion, nursing theory is essential to the disciplineof nursing. Nursing theory serves as a foundation to buildupon institutional missions and core values (Rosenberg,2006). Increasing the value of nursing theory facilitatesempowerment for clinical nurses in the profession.Procurement of new theories benefits patient care and pro-fessional nursing.
ReferencesCurrentNursing.com. (2012). Application of theory in nursing process.
Retrieved April 7, 2017, from http://currentnursing.com/nursing_theory/application_nursing_theories.html
Masters, K. (2014). Nursing theories: A framework for professional practice(2nd ed.). Burlington, MA: Bartlett and Jones Publishers.
Newman, M. (1999). Health as expanding consciousness (2nd ed.). NewYork, NY: National League for Nursing Press.
Rosenberg, S. (2006). Utilizing the language of Jean Watson’s CaringTheory within a computerized clinical documentation system.CIN: Informatics Nursing, 24(1), 53-56.
Roy, C. (1984). Introduction to nursing: An adaptation model (2nd ed.).Englewood Cliffs, NJ: Prentice-Hall.
Stevens, K.R. (2004). Star Model research: ACE Star Model of knowledgetransformation. San Antonio: Academic Center for Evidence-BasedPractice, University of Texas Health Science Center San Antonio.Retrieved from www.acestar.uthscsa.edu
Stevens, K.R. (2013). The impact of evidence-based practice in nursingand the next big ideas. OJIN: The Online Journal of Issues in Nursing,18(2), Manuscript 4. Retrieved from http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-18-2013/No2-May-2013/Impact-of-Evidence-Based-Practice.html
Sheri Jacobson, PhD, MS, RN, is a Professor, ChamberlainCollege of Nursing, Prelicensure Online Educational Program.She resides in Winston-Salem, NC.
15
866-877-2676 Volume 26 – Number 3
AMSN Corporate Members
Philips Healthcare3000 Minuteman RoadAndover, MA 01810
1-800-934-7372 • www.philips.com/healthcare
Wolters KluwerTwo Commerce Square
2001 Market StreetPhiladelphia, PA 19103
215-521-8999 • www.wolterskluwer.com / www.lww.com
Hospital Corporation of America2545 Park Plaza, Building 2, 4-East
Nashville, TN 37203615-344-9551 • www.hcanursing.com
Dale Medical Products7 Cross Street
Plainville, MA 027621-800-343-3980 • www.dalemed.com
Gold Level
Silver Level

AMSN BOARD OF DIRECTORS
PresidentLinda Yoder, PhD, MBA, RN, AOCN, FAAN
Immediate Past PresidentJill Arzouman, DNP, RN, ACNS-BC, CMSRN
TreasurerMarisa Streelman, MSN, RN, CMSRN
SecretaryRobin Hertel, EdS, MSN, RN, CMSRN
DirectorSummer Bryant, MSN, RN, CMSRN
DirectorHeather Craven, PhD, RN, CMSRN
DirectorJennifer Kennedy, MS, RN-BC, CMSRN
DirectorJulie Kennedy, MSN, RN, CMSRN
Chief Executive OfficerCynthia Hnatiuk, EdD, RN, CAE, FAAN
Director, Association ServicesSuzanne Stott, BS
MedSurg Matters!
EditorMolly McClelland, PhD, MSN, RN,
CMSRN, ACNS-BC
Editorial CommitteeMillicent G. De Jesus, MSN, RN-BCDeidra B. Dudley, DNS, MN, MS,
RN-BC, NEA-BCDianne J. Gibbs, DNP, RN
Stephanie Huckaby, MSN, RN-BCSally S. Russell, MN, RN, CMSRNCatherine A. Santori, RN, CMSRN
Elizabeth Thomas, MSN, RN, ACNS-BC
Managing EditorKatie R. Rayburn, ELS
Layout and Design SpecialistRobert Taylor, AS
Education DirectorRosemarie Marmion, MSN, RN-BC, NE-BC
The purpose of MedSurg Matters! is to disseminateinformation that will provide or enhance nursing
knowledge, practice, and professional developmentrelated to medical-surgical nurses.
Please think GREEN and recycle!
www.twitter.com/MedSurgNurses
www.facebook.com/MedSurgNurses
The mission of AMSN is to promote excellence in medical-surgical nursing.
Box 56, Pitman, NJ 08071-0056 • 866-877-AMSN (2676)[email protected] • www.amsn.org
Volume 26 – Number 3 • May/June 2017
Malnutrition in the Hospitalized Patient:Helpful Resources
While many of us are planning picnics or backyard barbecues, our patients aremissing the nutrition needed to fully heal and recover quickly. They are continuing toexperience longer lengths of stay, higher costs, additional complications, and anincreased risk of death as a result of being undernourished.An Agency for HealthcareResearch and Quality initiative mined data from a 2013 national inpatient repositoryto evaluate the “Characteristics of Hospital Stays Involving Malnutrition.” The result-ing Healthcare Cost and Utilization Project (HCUP) Statistical Brief confirms that mal-nutrition is adversely influencing patient outcomes (HCUP, 2016). The data alsoreveals that the most prevalent form of malnutrition (protein-calorie malnutrition) isassociated with a higher average cost of hospitalization ($25,200). As clinicians, wehave an opportunity to use this data to improve our care. By targeting the most nutri-tionally at-risk (those who are 85 years or older, black, low income, or rural), we canbegin to reduce these numbers and provide a healthier future for our patients.Through early assessment and intervention, we can develop nutritional plans to meettheir needs and bridge the gap to establish a firm plan for nutrition care upon dis-charge.
Efforts to eliminate hospital-based malnutrition and change these startling statis-tics begin with cohesive interprofessional initiatives.Teams are encouraged to explorethe toolkit available at the Malnutrition Quality Improvement Initiative (MQii) website(mqii.defeatmalnutrition.today). The resources are free and designed to meet theneeds of all team members.
Much like mapping out your favorite picnic or barbecue menu, taking time to mapout a strategy to defeat malnutrition will be incredibly meaningful to those you serve.What’s your summer strategy?
ReferenceHealthcare Cost and Utilization Project (HCUP). (2016, September). Statistical brief #210:
Characteristics of hospital stays involving malnutrition, 2013. Retrieved from https://www.hcup-us.ahrq.gov/ reports/statbriefs/sb210-Malnutrition-Hospital-Stays-2013.jsp
Beth Quatrara, DNP, RN, CMSRN, ACNS-BC, is Director of PNSO ResearchProgram, Clinical Assistant Professor, and Clinical Nurse Specialist – Advanced PracticeNurse 3, University of Virginia Health System, Charlottesville, VA. She is the “Nutrition toImprove Outcomes” Column Editor.
Nutrition to Improve Outcomes