ACLS MI
-
Upload
joshua-kosowsky -
Category
Documents
-
view
218 -
download
0
Transcript of ACLS MI
-
8/8/2019 ACLS MI
1/34
Acute Coronary Syndromes:
STEMI
Joshua M. Kosowsky, MD
Brigham & Womens Hospital
Emergency Medicine Physician
-
8/8/2019 ACLS MI
2/34
ACS Lecture Overview
Definition and pathophysiology
ACS case
Reperfusion therapy
Adjunctive medications
Shock & CHF
Right Ventricular Infarct
AHAACS Prevention Goals
-
8/8/2019 ACLS MI
3/34
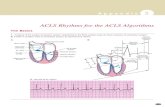
Acute Coronary Syndrome:
Definition & Pathophysiology
ACS = range of myocardial ischemic states:
Unstable angina Non-ST segment MI STEMI
Pathophysiology:
A
therosclerotic plaque disruption Intracoronary thrombus formation
BMJ 2003;326:1259-1261 (7 June), doi:10.1136/bmj.326.7401.1259
-
8/8/2019 ACLS MI
4/34
-
8/8/2019 ACLS MI
5/34
Yeghiazarians et al., NEJM2000; 342: 101
-
8/8/2019 ACLS MI
6/34
65 yo male with 1 hour
of left sided chest pain
Diaphoretic
H/o diabetes and
hyperlipidemia
T: 98.2 HR: 74
BP: 128/69 RR: 20
-
8/8/2019 ACLS MI
7/34
-
8/8/2019 ACLS MI
8/34
How to treat ACS:
** iv and cardiac monitor **
MONA:
M- morphine
O- oxygen
N- nitratesA- aspirin
-
8/8/2019 ACLS MI
9/34
-
8/8/2019 ACLS MI
10/34
Time is Muscle
Door
Data
Decision
Drug/Balloon
Goals:
Lytic therapy: 30 minutesPCI: 90 minutes
-
8/8/2019 ACLS MI
11/34
ReperfusionReperfusionSTEMI patients presenting to a hospital with PCISTEMI patients presenting to a hospital with PCIcapability should be treated with primary PCIcapability should be treated with primary PCIwithin 90 minutes of first medical contact.within 90 minutes of first medical contact.
STEMI patients presenting to a hospital withoutSTEMI patients presenting to a hospital withoutPCI capability and who cannot be transferred to aPCI capability and who cannot be transferred to aPCI center for intervention within 90 minutes ofPCI center for intervention within 90 minutes of
first medical contact should be treated withfirst medical contact should be treated withfibrinolytic therapy within 30 minutes of hospitalfibrinolytic therapy within 30 minutes of hospitalpresentation, unless contraindicated.presentation, unless contraindicated.
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
-
8/8/2019 ACLS MI
12/34
Benefit of Thrombolytic Therapy
49
37
8
-14
35
2519 18
BBB Ant
STo
Inf
STo
ST Depr 0-1hr 2-3hr 4-6hr 7-12hr
-20
-10
0
10
20
30
40
50
ECG Findings Time to TreatmentLancet 343:311,1994
Lives Saved per Thousand Treated
-
8/8/2019 ACLS MI
13/34
Fibrinolytic Therapy: Indications
ST elevation > 1 mm in 2 contiguous leads
or new or presumed new LBBB.
Signs and symptoms of MI.
Symptoms < 12 hours.
OK even if Q waves have appeared.
-
8/8/2019 ACLS MI
14/34
Fibrinolytic Therapy:
Absolute Contraindications
Active internal bleeding
Suspected aortic dissection
Known intracranial neoplasm
Any hemorrhagic stroke ever of other stroke
within the past year.
-
8/8/2019 ACLS MI
15/34
Fibrinolytic Therapy:
R
elative Contraindications Severe hypertension on presentation (BP>180/110)
History of chronic severe hypertension
History of priorC
VA
or other intracranial pathology Recent trauma (
-
8/8/2019 ACLS MI
16/34
Fibrinolytic Therapy: Risk of
Intracerebral Hemorrhage Overall risk ~0.5%.
Higher risk with :
Age> 65
Weight 180/110
-
8/8/2019 ACLS MI
17/34
Measuring Fibrinolytic Success:
No perfect indicators, but use:
Pain resolved?
Amount of ST elevation improved by >70%?
Start to worry if youre not seeing these by 45-60
minutes after the initiation of the lytic.
If no reperfusion, move to rescue angioplasty.
-
8/8/2019 ACLS MI
18/34
Benefits relative to lytic therapy:
Successful in >90% of patients
More complete restoration of arterial patency
Less re-occlusion
Fewer strokes
Probably better outcomes in shock
Limitations: Time
Lack of widespread availability
Percutaneous Coronary Intervention
(PCI) inAcute MI
-
8/8/2019 ACLS MI
19/34
Facilitated PCIFacilitated PCI
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII A planned reperfusion strategy using fullA planned reperfusion strategy using full--dosedose
fibrinolytic therapy followed by immediate PCI may befibrinolytic therapy followed by immediate PCI may be
harmful.harmful.
-
8/8/2019 ACLS MI
20/34
Immediate or EmergencyImmediate or Emergency
Invasive Strategy and Rescue PCIInvasive Strategy and Rescue PCICoronary angiography with intent to perform PCI (orCoronary angiography with intent to perform PCI (oremergency CABG) is recommended for patients whoemergency CABG) is recommended for patients whohave received fibrinolytic therapy and have any of thehave received fibrinolytic therapy and have any of thefollowing:following:
Cardiogenic shock in patients less than 75 years whoCardiogenic shock in patients less than 75 years who
are suitable candidates for revascularization.are suitable candidates for revascularization.
Severe congestive heart failure and/or pulmonary edemaSevere congestive heart failure and/or pulmonary edema
(Killip class III).(Killip class III).
Hemodynamically compromising ventricular arrhythmias.Hemodynamically compromising ventricular arrhythmias.
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
-
8/8/2019 ACLS MI
21/34
Coronary angiography with intent to perform rescue PCI isCoronary angiography with intent to perform rescue PCI isreasonable for patients in who fibrinolytic therapy has failedreasonable for patients in who fibrinolytic therapy has failed
STST--segment elevation
-
8/8/2019 ACLS MI
22/34
Anticoagulants as Ancillary TherapyAnticoagulants as Ancillary Therapy
Patients undergoing reperfusion withPatients undergoing reperfusion withfibrinolytics should receive anticoagulantfibrinolytics should receive anticoagulanttherapy for a minimum of48 hours, andtherapy for a minimum of48 hours, and
preferably for the duration of the indexpreferably for the duration of the indexhospitalization, up to 8 days.hospitalization, up to 8 days.
Regimens other than UFH are recommendedRegimens other than UFH are recommended
if therapy is given for more than4
8 hoursif therapy is given for more than4
8 hoursbecause of risk of heparinbecause of risk of heparin--inducedinducedthrombocytopenia.thrombocytopenia.
Regimens with established efficacy include:Regimens with established efficacy include:
UFH, enoxaparin, fondaparinuxUFH, enoxaparin, fondaparinux
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
-
8/8/2019 ACLS MI
23/34
Heparin
Recommended in:
Patients receiving fibrinolytics (not
SK/APSAC) All patients undergoing PCI.
Dosing:
60 unit/kg bolus then 12 units/kg/hr (max4000/1000)
-
8/8/2019 ACLS MI
24/34
BetaBeta--BlockersBlockersOral betaOral beta--blocker therapy should be initiated inblocker therapy should be initiated inthe first 24 hours for patients who do not havethe first 24 hours for patients who do not havethe following:the following:
Signs of heart failureSigns of heart failureEvidence of low output stateEvidence of low output state
Increased risk for cardiogenic shockIncreased risk for cardiogenic shockAge >70 yearsAge >70 years
Systolic blood pressure 110 or < 60 bpm)
Increased time since onset of symptoms of STEMIIncreased time since onset of symptoms of STEMIRelative contraindications to betaRelative contraindications to beta--blockadeblockade
PR interval >0.24 secondsPR interval >0.24 seconds
secondsecond-- or thirdor third--degree heart blockdegree heart block
active asthma or reactive airway diseaseactive asthma or reactive airway disease
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
-
8/8/2019 ACLS MI
25/34
BetaBeta--BlockersBlockersIt is reasonable to administer an IV betaIt is reasonable to administer an IV beta--blocker at the time of STEMI presentation toblocker at the time of STEMI presentation topatients who are hypertensive and who do notpatients who are hypertensive and who do nothave any of the following:have any of the following:
Signs of heart failureSigns of heart failure
Evidence of low output stateEvidence of low output state
Increased risk for cardiogenic shockIncreased risk for cardiogenic shock
Other relative contraindications to betaOther relative contraindications to beta--blockadeblockade
IV beta blockers should not be administered to patientsIV beta blockers should not be administered to patientswho have any of the following:who have any of the following:
Signs of heart failureSigns of heart failure
Evidence of low output stateEvidence of low output state
Increased risk of cardiogenic shockIncreased risk of cardiogenic shock
Other relative contraindications to betaOther relative contraindications to beta--blockadeblockade
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
III IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIII IIaIIaIIa IIbIIbIIb IIIIIIIIIIIaIIaIIa IIbIIbIIb IIIIIIIII
-
8/8/2019 ACLS MI
26/34
Treatment of Shock and CHF
For both, PCI is choice for reperfusion therapy.
CHF:
iv diuretics
nitrates for preload and afterload reduction (keep SBP>90)
consider dobutamine
Hypotension:
if SBP
-
8/8/2019 ACLS MI
27/34
Right Ventricular Infarction
Presentation:
ST elevation inferiorly (II, III, AVF)
Hypotension (worse with preload reducing
agents: nitrates, morphine, diuretics)
Classic triad:
Jugular venous distention
Clear lungs
Hypotension
-
8/8/2019 ACLS MI
28/34
RV Infarct 10-50% of inferior wall MIs (II,III,AVF)
have associated right ventricular infarct
Contractility of the right ventricle depends
on diastolic pressure and output can
decrease dramatically with decreased
preload (volume) Also increased loss ofAV synchrony
-
8/8/2019 ACLS MI
29/34
ST elevation inferiorly in leads II, III, &AVF
ST elevation anteriorly in V1
-
8/8/2019 ACLS MI
30/34
To do a right sided EKG
place pre-cordial leads(V1-V6) across the
right side of the chest
in a mirror image ofthe standard left-sided
leads (V1R-V6R)
Lead V4T is placed in the
right 5th intercostal space
at the mid-clavicular line
Standard EKG lead placement
-
8/8/2019 ACLS MI
31/34
-
8/8/2019 ACLS MI
32/34
Key Treatment Points Give IVF to increase preload to treat
hypotension
Increased incidence ofAV block requiring
packing support
Increased in-hospital mortality to
aggressively pursue definitive treatment
-
8/8/2019 ACLS MI
33/34
2007 Goals: Secondary Prevention2007 Goals: Secondary Prevention
Smoking:Smoking: Complete cessation, no exposureComplete cessation, no exposureto environmental tobacco smoke.to environmental tobacco smoke.
Blood Pressure Control:Blood Pressure Control:
-
8/8/2019 ACLS MI
34/34
2007 Goals: Secondary Prevention2007 Goals: Secondary PreventionWeight Management:Weight Management:
Goals: BMI 18.5Goals: BMI 18.5 -- 24.9 kg/m2 and24.9 kg/m2 and
Waist circumference in men