A Pound of Cure: Vaccines to Stop the COVID19 Pandemic
Transcript of A Pound of Cure: Vaccines to Stop the COVID19 Pandemic
Rapid Response Vaccines to Stop the COVID19 Pandemic
Phil & Sandra Nudelman Endowed Lecture
November 16, 2020
Deborah Fuller, PhD
Professor, Department of Microbiology
University of Washington
Division Chief, Infectious Diseases and Translational Medicine
Washington National Primate Research Center
Disclosures
I am a co-founder of Orlance, Inc. a biotechnology company that aims to commercialize gene gun delivered DNA and RNA vaccine technologies that will be presented.
I do not have financial interests in HDT Bio, the biotechnology company that aims to commercialize the novel LION/repRNA-CoV2S vaccine that will be presented.
Stopping COVID-19
Social distancing & masks
• Slow transmission
Testing• Quarantine the infected
Vaccines are coming• Stop the pandemic by
providing immunity to the population
November 19, 2020
https://coronavirus.jhu.edu/map.html
Vaccines are:
A way of priming the immune system (immunization) to provide protection from disease caused by a
pathogen without subjecting that person to the disease
Vaccines: An ounce of prevention, a pound of cure
It is estimated that vaccines have saved more lives worldwide than all other medical interventions combined
Herd immunity is achieved(70-90% of population immune)
Herd Immunity
Measles vaccine
Vaccines induce immune memory to a specific pathogen
• Deliberate exposure to Ag that will not produce disease
• Stimulate primary immune response
• Memory cells produced
• Rapid, longer lasting secondary response when we encounter thesame pathogen later (specificadaptive immunity).
Most vaccines protect us from an infection by inducing antibody responses
How will vaccine-induced antibody responses protect us from COVID-19?
ACE2 is a molecule on human cells and it’s what SARS-CoV-2 attaches to in order to infect our cells
SARS-CoV-2 is the virus that causes COVID-19
The virus binds ACE2 via it’s receptor binding domain (RBD) on the viral spike protein
Vaccines aim to induce antibodies that bind the RBD, block viral binding to ACE2 and prevent infection
Vaccines under development for COVID-19
RNA
Candidate COVID-19 vaccines include traditional and new approaches
• mRNA• DNA • Inactivated• Live viral vector• Rec. protein
SinophramSinovac
NovavaxMedicagoClover/GSKU of Queensland
Oxford/AstraZJ&JCanSino
ModernaPfizer/BioNtecHDT/UWInnovioCureVacSanofi
U of Melbourne
https://www.nature.com/articles/d41573-020-00073-5
Current landscape of leading vaccines in phase 3 clinical trials
• The current high rate of transmission is accelerating this timeline
• Timelines for public rollout are moving up by about 3-4 weeks.
Limits of the lead vaccines
• Cold Chain may limit distribution world-wide• Pfizer’s vaccine requires storage at ultra-cold (-80C)
• Limited demographics• Adenovirus-based vaccines (J&J, AstraZeneca and the lead vaccines in Russia and China) are generally
less potent in the elderly
• Short durability• All the lead vaccines are focused on antibody responses that may wane quickly, requiring frequent
booster doses to sustain immunity• Adenovirus-based vaccine induce responses that compromise potency of booster doses.
• Multiple doses• Need to manufacture more doses• Takes longer to induce immunity (at least 6 weeks)
Key attributes for an effective pandemic vaccine
Induces immunity quickly
(Ideally with one dose but two is ok)
Induces antibody and T cell responses
(Antibody, Killer T cells, Type 1 T helper cells)
Effective across different demographics
(Elderly, immune-compromised, co-morbidities)
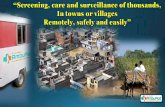
Fast and cost-effective scale-up, stable at room temperature
We are designing the next generation vaccines to address limits of the 1st wave of vaccines.
• Stable at room temperature
• More effective in the elderly
• Long-term immunity
• One dose
• Needle free - self administration could increase vaccine coverage
“New” kids on the block: DNA and RNA vaccines instruct our own cells to produce vaccine antigens
DNA vaccine RNA vaccine
DNA & RNA vaccines can be rapidly designed and produced: Only need the genetic sequence of a pathogen
They induce both antibody and T cell responses – two weapons of the immune system
Antibodies and T cells work together to fight against SARS-CoV-2 infection
Cytotoxic T cells find and kill cells that become infectedAntibodies block the virus from infecting a cell
Helper T cells help B cells make antibody and activate killer T cells
2nd generation vaccines under development at the University of Washington
Vaccine platforms• Replicating RNA vaccines delivered IM
by LION (HDT Bio Corp)
• DNA and RNA vaccines delivered to the epidermis by needle-free gene gun (Orlance, Inc.)
• Nanoparticle recombinant protein vaccines delivered by IM (Neil King, David Veesler)
Nucleic acids (DNA and RNA) are new rapid response vaccine platforms for pandemics
Traditional vaccinesRequire pathogen and cell-based
manufacturing processes before they can be injected
DNA vaccines insert a code into cells to instruct them
to make vaccineRequires delivery into cell
AND the nucleus
RNA vaccines insert a code into cells to instruct them
to make vaccinerequires delivery into cell
Requires only gene sequence of the pathogen to design (Fast!) Rapid scale-up (Fast! Low cost) Stable at room temperature (DNA, certain formulations of RNA) (helps worldwide distribution) Induces both antibody and T cell responses (two weapons of defense against the virus)
Second generation RNA vaccine: Self-amplifying replicon RNA vaccines (repRNA)
Amplifies amount of antigens and the immune response
DNA is easily manipulated Viral RNA is immunogenic
More immunogenic More effective in the immunocompromised and elderly More durable immunity
Nucleic acid vaccines can rapidly respond to new pandemics
Metagenomicanalysis
Full genome sequence available Jan 10, 2020
Ag design, cloning, &
pilot DNA or RNA lots
7 days
Preclinical down selection
(animal studies)14-120 days
GLP/Tox, Formulation and manufacturing
30-90 days
Human clinical testing (HDT301)
Phase I
FAST! We designed, produced and started testing a candidate replicating RNA vaccine within 7 days after the sequences of SARS-CoV-2 were published
Nov 2020-Jan 2021Jan 2020 Feb-May 2020 June-Oct 2020
Getting RNA into cells: LION and Lipo-nanoparticles (LNP)
LION (our vaccine) LNPs (Moderna, Pfizer, J&J)
Formulation RNA on particle surfaceSimple mixing process – Rapid scale up
RNA inside particleComplex process – Slower scale up
Scale up No cholesterol – all components easily sourced Uses cholesterol – limited supply
Stability Longer shelf life - room temp stable Short shelf life – needs a freezer
Promising pre-clinical results in nonhuman primates with our LION/repRNA vaccine
• Protective levels of antibody are sustained for 4+ months (and counting) after a single shotRapid immunity to block the virus
• T cell responsesClear virus if some gets past antibody
• Strong responses in aged animalsElderly are highly vulnerable but
respond poorly to vaccines
Getting DNA and RNA into cells – another way
Formulate DNA or RNA ontoMicroscopic 1-3 uM Gold Particles
Helium Gas Jet Acceleratesthe Particles to Supersonic Speed
into Skin
Penetration of the micron-sized particles is painless
Research Device Clinical Device
DNA needs to get in nucleus.Not all cells that get a gold particle
will express antigen but the ones that do express protein longer
RNA
DNA
RNA only needs to get into cytoplasm.
All cells that get a gold particle will express antigen
Gene gun (Orlance)
Needle-free delivery – pain-free, self-administration Stable at room temperature – supports worldwide distribution
Clinical development of a new vaccine: How long does it take?
A new vaccine requires multiple phases of development and clinical testing to:
• Make sure it works• Make sure it’s safe
6 COVID-19 vaccines to date have been rapidly advanced to phase I clinical trialsSome vaccine platforms were in pre-clinical development for a related viruses (MERS) at the time of the outbreak
But this still takes at least 5 years!
Accelerated timeline to get a vaccine into the population as soon as possible
License or BustMassive
scale-up
SAFETY FIRST! No safety checkpoints are skipped
Where are we now?
LION/repRNA vaccine
• Sinopharm (China) – 2 inactivated vaccines• Sinovac (China) –inactivated• Moderna (US) – mRNA• Oxford/AstraZeneca (UK) – ChAd5• Pfizer/BioNTec (US/Germany) – mRNA• CanSino (China) – Ad5• J&J – Ad26• Novavax – recombinant protein
CanSino (China)-Ad5Gamaleya (Russia) – Ad5/Ad26Sinopharm (China) – 2 inactivated vaccinesBektop (Russia)Sinovac (China) -inactivated
Three ways a COVID-19 vaccine can protect
From infection From disease From transmission
Hodgson et al, Lancet Infectious Disease 2020
FDA requirements for COVID-19 vaccine
EFFICACY• Minimum 50% efficacy
• Document a minimum number of cases (130-160)
• Positive for COVID19 AND positive for 1-2 symptoms
• Efficacy in protection from disease• Pfizer and Moderna report > 90%!
• Document a minimum number of severe cases (at least 5)
• Protection from severe disease
SAFETY• Minimum 2 months follow-up
• Mild/moderate reactogenicity• This is normal – indicates the vaccine is
working!
• No vaccine-associated adverse events
• No evidence of enhancement of disease
Once we have vaccines, how will they be used to stop the pandemic? Who will get it first?
Getting an effective vaccine into billions of people is the next hurdle
Emergency Use Authorization (limited roll-out)High risk groups (elderly)
Medical teams
First responders
Ring vaccination – used when vaccines are in short supply
• Identify cases & vaccinate close contacts.
• Close contacts are protected
• Chain of transmission is broken
Vaccinating the rest of us
• Even a highly effective vaccine (i.e. > 80% efficacy) will require 55-60% of the population gets immunized to stop the pandemic.
• Social distancing + masks + vaccination are need to accelerate the timeline to stop the pandemic
• The coming mass vaccination campaign will be unprecedented.
No single silver bullet (or arrow)
Induces immunity quickly (single shot)
Effectiveacross
demographics(i.e. elderly)
Fast, cost-effective scale-up
Stable at room temperature
Strongest antibody and
T cellsLong-term immunity
5-7 effective vaccines that work together will likely be needed to stop the pandemic
Acknowledgments
Megan O’Connor
Fuller lab (UW)Patience MurapaJim FullerThomas LewisKevin DravesSamantha Randall
Michael Gale Jr. (UW)Emily Hemann
David Veesler (UW)Alexandra (Lexi) Walls
Washington National Primate Research CenterKathryn Guerriero
HDT Bio CorpAmit KhandharMalcolm DuthieDarrick CarterSteven ReedPeter Berglund
NIH Rocky Mountain LabsHeinz FeldmanDavid HawmanShanna LeventhalElizabeth Fischer
FundingNIH ORIPNIH NIAIDCIIIDCEIRSFAST grantsPew Biomedical ScholarsWashington Research FoundationHDT Bio Corp
Jesse Erasmus