1 IMCI. Features of IMCI… not necessarily dependent on the use of sophisticated and expensive...
-
Upload
ross-gordon -
Category
Documents
-
view
213 -
download
0
Transcript of 1 IMCI. Features of IMCI… not necessarily dependent on the use of sophisticated and expensive...
Features of IMCI…Features of IMCI…
not necessarily dependent on the use of sophisticated and expensive technologies
a more integrated approach to managing sick children
move beyond addressing single diseases to addressing the overall health and well-being of the child
2
Features of IMCI…Features of IMCI…
careful and systematic assessment of common symptoms and specific clinical signs to guide rational and effective actions
integrates management of most common childhood problems (pneumonia, diarrhea, measles, malaria, dengue hemorrhagic fever, malnutrition and anemia, ear problems)
includes preventive interventions
3
Features of IMCI…Features of IMCI…
adjusts curative interventions to the capacity and functions of the health system (evidence-based syndromic approach)
involves family members and the community in the health care process
4
Objectives of IMCIObjectives of IMCI
(1) reduce deaths and the frequency and severity of illness and disability; and
(2) contribute to improved growth and development
5
IMCI ComponentsIMCI Components
1. Improving case management skills of health workers
◦ standard guidelines◦ training (pre-service/in-service)◦ follow-up after training◦ role of private providers
6
IMCI ComponentsIMCI Components
2. Improving the health system to deliver IMCI
◦ essential drug supply and management◦ organization of work in health facilities◦ management and supervision◦ referral system
7
IMCI ComponentsIMCI Components
3. Improving family and community practices
◦ for physical growth and mental development
◦ for disease prevention◦ for appropriate home care◦ for seeking care
8
IMCI ComponentsIMCI Components
3. Improving family and community practices
-For physical growth and mental development Breastfeeding Complementary feeding Micronutrient supplementation Psychosocial stimulation
9
IMCI ComponentsIMCI Components
3. Improving family and community practices - For disease prevention
immunizationhandwashingsanitary disposal of fecesuse of insecticide-treated bednetsdengue prevention and control
10
IMCI ComponentsIMCI Components
3. Improving family and community practices
- For appropriate home care continue feeding increase fluid intake appropriate home treatment
11
IMCI ComponentsIMCI Components
3. Improving family and community practices
- For seeking care
Follow health workers adviceWhen to seek carePrenatal consultationPostnatal (postpartum) consultation
12
The Integrated Case Management ProcessThe Integrated Case Management Process
13
Treatment•treat local infection
•give oral drugs•advise and teach
caretaker•follow up
Outpatient Health Facility
Home
Caretaker is counselled on:
•home treatment•feeding &fluids•when to return
•immediately•follow-up
•check for danger signs•assess main symptoms
•assess nutrition and Immunization status and potential feeding problems
•Check for other problems•classify conditions and
• identify treatment actions
Outpatient Health Facility
Urgent referral•pre-referral treatment
•advise parents•refer child
Outpatient Health Facility
•emergency triage &treatment
•Diagnosis & treatment•monitoring & ff-up
Referral facility
Target Groups Target Groups
Sick young infant◦1 week up to 2 months
Sick young children◦2 months up to 5 years
14
Assessing the Sick ChildAssessing the Sick Child
15
General Danger Signs
• lethargy or unconsciousness• inability to drink or breastfeed
• vomiting
• convulsions
Checking the Main Checking the Main SymptomsSymptoms
- cough and difficult breathing - diarrhea - fever - ear problem
16
Checking the Main Checking the Main SymptomsSymptoms
1. Cough or difficult breathing 3 clinical signs
◦ Respiratory rate◦ Lower chest wall indrawing◦ Stridor
17
Checking the Main Checking the Main SymptomsSymptoms
2. Diarrhea Dehydration
◦ General condition◦ Sunken eyes◦ Thirst◦ Skin elasticity
Persistent diarrhea Dysentery
18
Checking the Main Checking the Main SymptomsSymptoms
3. Fever Stiff neck Risk of malaria and other endemic
infections, e.g. dengue hemorrhagic fever
Runny nose Measles Duration of fever (e.g. typhoid
fever)
19
Checking the Main Checking the Main SymptomsSymptoms
4. Ear problems Tender swelling behind the ear Ear pain Ear discharge or pus (acute or
chronic)
20
Checking Nutritional Status, Checking Nutritional Status, Feeding, Immunization StatusFeeding, Immunization Status
Malnutrition ◦visible severe wasting◦edema of both feet◦weight for age
Anemia◦palmar pallor
Feeding and breastfeeding Immunization status
21
Assessing Other ProblemsAssessing Other Problems
Meningitis Sepsis Tuberculosis Conjunctivitis Others: also mother’s (caretaker’s) own
health
22
IMCI Essential Drugs and IMCI Essential Drugs and SupplySupply
Appropriate antibiotics Quinine Vitamin A Paracetamol Oral antimalarial Tetracycline eye ointment ORS Mebendazole or albendazole Iron Vaccines Gentian violet
23
24
Overall Case Management ProcessOverall Case Management Process
Outpatient 1 - assessment 2 - classification and identification of treatment 3 - referral, treatment or counseling of the child’s caretaker (depending on the classification
identified 4 - follow-up careReferral Health Facility 1 - emergency triage assessment and treatment 2 - diagnosis, treatment and monitoring of patient progress
25
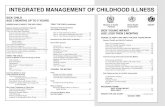
SUMMARY OF THE INTEGRATED CASE MANAGEMENT PROCESS
For all sick children age 1 week up to 5 years who are brought to a first-level health facility
ASSESS the child: Check for danger signs (or possible bacterial infection). Ask about main symptoms. If a main symptom is reported, assess further. Check nutrition and immunization status. Check for other problems.
CLASSIFY the child’s illnesses: Use a colour-coded triage system to classify the child’s main symptomsand his or her nutrition or feeding status.
IF URGENT REFERRAL is needed and possible IF NO URGENT REFERRAL isneeded or possible
IDENTIFY URGENTPRE-REFERRAL TREATMENT(S)needed for the child’s classifications..
IDENTIFY TREATMENT needed for the child’s classifications: Identify specific medical treatments and/or advice.
TREAT THE CHILD: Give urgent pre-referral treatment (s) needed.
TREAT THE CHILD: Give the first dose of oral drugs in the clinicand/or advise the child’s caretaker. Teach the caretaker how to give oral drugs and how to treat local infections at home. If needed, give immunizations.
REFER THE CHILD: Explain to the child’s caretaker the need for referral. Calm the caretaker’s fears and help resolve any problems. Write a referral note. Give instructions and supplies needed to care for the child on the way to the hospital.
COUNSEL THE MOTHER: Assess the child’s feeding, including breastfeeding practices, and solve feeding problems, if present. Advise about feeding and fluids during illness and about when to return to a health facility. Counsel the mother about her own health.
FOLLOW-UP care: Give follow-up care when the child returns to the clinic and,if necessary, reassess the child for new problems.
26
Summary of the Integrated case Summary of the Integrated case Management ProcessManagement Process
For all sick children age 1 week up to 5 years who are brought to a first-level health facility
27
Summary of the Integrated case Summary of the Integrated case Management ProcessManagement Process
ASSESS the Child: Check for danger signs (or possible bacterial
infection). Ask about main
symptoms. If a main symptom is
reported, assess further. Check nutrition and immunization status.
Check for other problems
28
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
Classify the child’s illness: Use a color-coded triage system to classify the child’s main symptoms and his or her nutrition or feeding status.
29
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
IF URGENT
REFERRALis needed and
possible
30
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
IDENTIFY URGENT PRE-REFERRAL TREATMENT(S)Needed prior to
referral of the child according to classification
31
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
TREAT THE CHILD:Give urgent pre-referral treatment(s) needed.
32
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
REFER THE CHILD:Explain to the child’s
caretaker the need for referral.
Calm the caretaker’s fears and help resolve any problems. Write a referral note.
Give instructions and supplies needed to care for the child on the way to the hospital
33
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
IF NO URGENT REFERRAL
is needed or possible
34
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
IDENTIFY TREATMENT
needed for the child’s
classifications: identify specific
medical treatments and/or
advice
35
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
TREAT THE CHILD:Give the first dose of
oral drugs in the clinic and/or advice the child’s caretaker.
Teach the caretaker how to give oral drugs and how to treat local infections at home.
If needed, give immunizations.
36
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
COUNSEL THE MOTHER:
Assess the child’s feeding, including breastfeeding practices, and solve feeding problems, if present.
Advise about feeding and fluids during illness and about when to return to a healthy facility.
Counsel the mother about her own health.
37
Summary of the Integrated Case Summary of the Integrated Case Management ProcessManagement Process
FOLLOW-UP CARE:Give follow-up care when the child returns to the clinic and, if necessary, re-asses the child for new problems.
38
SELECTING THE APPROPRIATE CASE MANAGEMENT CHARTS
FOR ALL SICK CHILDREN age 1 week up to 5 years who are brought to the clinic
ASK THE CHILD’S AGE
IF the child is from 1 week up to 2 monthsIF the child is from 2 months up to 5 years
USE THE CHART:œASSESS, CLASSIFY AND TREAT THE SICK YOUNG INFANT
USE THE CHART:œASSESS AND CLASSIFY THE SICK CHILDTREAT THE CHILDCOUNSEL THE MOTHER