Victoria & Mapperley Practice Scheduled Report ... · •...
Transcript of Victoria & Mapperley Practice Scheduled Report ... · •...

This report describes our judgement of the quality of care at this service. It is based on a combination of what we foundwhen we inspected, information from our ongoing monitoring of data about services and information given to us fromthe provider, patients, the public and other organisations.
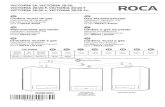
Ratings
Overall rating for this service Good –––
Are services safe? Good –––
Are services effective? Good –––
Are services caring? Good –––
Are services responsive to people’s needs? Good –––
Are services well-led? Good –––
VictVictoriaoria && MapperleMapperleyy PrPracticacticeeQuality Report
Victoria Health Centre, Glasshouse Street,NottinghamNG1 3LWTel: 0115 883 9080Website: www.victoriamapperley.co.uk
Date of inspection visit: 03 November 2014Date of publication: 24/02/2015
1 Victoria & Mapperley Practice Quality Report 24/02/2015

Contents
PageSummary of this inspectionOverall summary 2
The five questions we ask and what we found 4
The six population groups and what we found 6
What people who use the service say 8
Areas for improvement 8
Detailed findings from this inspectionOur inspection team 9
Background to Victoria & Mapperley Practice 9
Why we carried out this inspection 9
How we carried out this inspection 9
Detailed findings 11
Overall summaryLetter from the Chief Inspector of GeneralPracticeWe inspected this practice on 03 November 2014, as partof our new comprehensive inspection programme. Thepractice had not previously been inspected.
The overall rating for this service is good.
Our key findings were as follows:
• The staff team were committed to meeting patients’diverse needs and placed their best interests at thecentre of everything they did.
• Patients expressed high levels of satisfaction with thecare and service they received.
• Patients received effective care and treatment. Theywere also treated with kindness, dignity and respect.
• Systems were in place to keep patients safe and toprotect them from harm. However, robust procedureswere not always followed in practice in respect of staffrecruitment, infection control and chaperone duties.Following the inspection, we received written
assurances that these issues had been addressed.
• The practice responded to patients’ needs. Theappointment system was flexible and enabled patientsto access care and treatment when they needed it.
• Staff felt valued, well supported, and involved indecisions about the practice. There was strongteamwork and a commitment to improving the qualityof care and services for patients.
• The practice had undergone considerable changes inthe last 18 months, which had affected the ability todrive improvements and oversee the quality ofservices provided.
However, there were also areas of practice where theprovider needs to make improvements.
The provider should:
• Ensure that the learning and improvements fromsignificant events are shared with all relevant staff.
• Review the recruitment policy to ensure thatinformation required by law is obtained prior to staffcommencing employment at the practice.
Summary of findings
2 Victoria & Mapperley Practice Quality Report 24/02/2015

• Keep essential records to show that all nurses and GPsare registered to practice with the relevantprofessional body prior to their employment, andremain registered and fit to practice.
• Keep essential records to show that all relevant staffare protected from Hepatitis B infection.
• Provide a designated person to lead on infectioncontrol. Ensure systems are in place to monitor theprevention and control of infection and that policiesare being followed appropriately.
• Ensure all staff receive sufficient training to enablethem to undertake their specific roles.
• Ensure that arrangements are in place to enablepeople whose first language is not English, to accessinformation about services.
Professor Steve Field (CBE FRCP FFPH FRCGPChief Inspector of General Practice
Summary of findings
3 Victoria & Mapperley Practice Quality Report 24/02/2015

The five questions we ask and what we foundWe always ask the following five questions of services.
Are services safe?The practice is rated as good for providing safe services. There wereenough staff to keep people safe. Arrangements were in place toensure that the practice was clean, safe and adequately maintained.The practice was open and transparent when things went wrong.Staff understood and fulfilled their responsibilities to raise concerns,and report incidents and near misses.
Learning took place and appropriate action was taken to minimiserisks. We found that systems were in place to keep patients safe andto protect them from harm. However, robust procedures were notalways followed in practice in respect of staff recruitment, infectioncontrol and chaperone duties. Following the inspection, wereceived written assurances that these issues had been addressed.
Good –––
Are services effective?The practice is rated as good for providing effective services. Thepractice had an established staff team, who ensured continuity ofcare and services. Staff worked with partner health and social careservices to meet patients’ needs. Patients’ needs were assessed andtheir care and treatment was delivered in line with evidence basedpractice. Patients were regularly reviewed to assess the effectivenessof their care and treatment. Clinical audits were carried out tomonitor and improve the care and outcomes for patients.
Good –––
Are services caring?The practice is rated as good for providing caring services. Patientsdescribed the staff as friendly and caring and said that they weretreated with respect. Patients were involved in decisions about theirhealth and treatment, and their wishes were respected. Staffsupported patients to cope emotionally with their health andcondition. People were supported to manage their own health andcare and to maintain their independence, where possible. Patients’privacy, dignity and confidentially were maintained; staff wererespectful and polite when dealing with patients.
Good –––
Are services responsive to people’s needs?The practice is rated as good for providing responsive services. Thepractice had an established staff team, providing continuity of careand access to appointments. The appointment system was flexible.Patients were able to get an appointment, or were offered atelephone consultation, where needed. The services were planned
Good –––
Summary of findings
4 Victoria & Mapperley Practice Quality Report 24/02/2015

and delivered in a way that met the needs of the local population.There was a culture of openness and people were encouraged toraise concerns. Patients concerns and complaints were listened toand used to improve the service.
Are services well-led?The practice is rated as good for being well-led. Patients told us theywere asked for their views, and their feedback was acted on toimprove the service. The PPG was re-established in July 2014 andwas working with the practice to improve the services.
Staff said that they felt valued, well supported, and involved indecisions about the practice. There was strong teamwork and acommitment to improving the quality of care and services forpatients. The practice had undergone considerable changes in thelast 18 months, which had affected the ability to driveimprovements. Various systems were in place to assess and managerisks and to monitor the quality of services provided. However, therewere areas where robust systems were not in place to driveimprovements and provide assurances that policies were beingfollowed. Following the inspection, we received assurances that themonitoring arrangements had been strengthened to oversee allaspects of the service.
Good –––
Summary of findings
5 Victoria & Mapperley Practice Quality Report 24/02/2015

The six population groups and what we foundWe always inspect the quality of care for these six population groups.
Older peopleThe practice is rated as good for the care of older people. Allpatients 75 years and over were allocated a named GP to providecontinuity of care, and were also offered an annual health check.Care plans were provided for patients over 75 years who hadcomplex needs or were at high risk, to help avoid unplannedadmissions to hospital.
The practice kept a register of older people who were identified asrequiring additional support, and monthly multi-disciplinarymeetings were held to discuss patients’ needs. Carers wereidentified and supported to care for older people. Home visits werecarried out for elderly housebound patients.
Good –––
People with long term conditionsThe practice is rated as good for the care of people with long termconditions. All patients were offered an annual review including areview of their medication, to check that their health needs werebeing met. When needed, longer appointments and home visitswere available. Where possible, patients’ long term conditions andany other needs were reviewed at a single appointment, rather thanhaving to attend various reviews. Patients with complex needs had anamed GP to provide continuity of care. Referrals to specialists andother secondary services were made in an appropriate and timelyway. Emergency processes were in place for patients who had asudden deterioration in their health.
Good –––
Families, children and young peopleThe practice is rated as good for the care of families, children andyoung people. Systems were in place for identifying andfollowing-up children and young people who were vulnerable or atrisk. Immunisation rates were high for all standard childhoodimmunisations. The practice worked in partnership with midwives,health visitors and school nurses. A weekly baby clinic was held atthe practice. Appointments were available outside of school hoursto enable children to attend. The practice shared the building with acontraception and sexual health clinic, which offered direct accessto teenage clinics, contraception and sexual health screening.
Good –––
Summary of findings
6 Victoria & Mapperley Practice Quality Report 24/02/2015

Working age people (including those recently retired andstudents)The practice is rated as good for the care of the working-age people.The practice provided extended opening hours to enable patients toattend on a Saturday morning. Patients were also offered telephoneconsultations and were able to book non urgent appointmentsaround their working day by telephone or on line.
The practice offered a ‘choose and book’ service for patients referredto secondary services, which provided greater flexibility over whenand where their test took place. This enabled patients to choosewhich hospital or clinic they wished to be seen in, and to book theirown outpatient appointments, where able. NHS health checks wereoffered to patients aged 40 to 74 years, which provided anopportunity to review their health needs and to identify early signsof medical conditions. The practice also offered health promotionand screening appropriate to the needs for this age group.
Good –––
People whose circumstances may make them vulnerableThe practice is rated as good for the care of people whosecircumstances may make them vulnerable. The practice held aregister of patients living in vulnerable circumstances includingpeople with learning disabilities. Patients with a learning disabilitywere invited to attend an annual health review. A significant numberof patients at the practice had a learning disability. The clinical staffwere able to demonstrate extensive knowledge, skills andunderstanding of patients’ needs. They worked with local carehomes and the learning disability health facilitator, to provideinnovative ways of meeting individual’s needs. A weekly substancemisuse clinic was held at the practice, which one of the GPs ran.
Patients in vulnerable circumstances were discussed at monthlymulti-disciplinary meetings to ensure they received appropriate careand support. When needed, longer appointments and home visitswere available. Carers were identified and offered support, includingsignposting them to external agencies.
Good –––
People experiencing poor mental health (including peoplewith dementia)The practice is rated as good for the care of people experiencingpoor mental health. The practice held a register of patientsexperiencing poor mental health. Patients were invited to attend anannual health check. The practice worked with mental health andsocial care services to ensure that patients’ needs were regularlyreviewed, and that appropriate risk assessments and care planswere in place. Patients were supported to access emergency careand treatment when experiencing a mental health crisis.
Good –––
Summary of findings
7 Victoria & Mapperley Practice Quality Report 24/02/2015

What people who use the service sayPrior to the inspection, we received comment cards fromfour patients. We also spoke with five patients includingthree members of the Patient Participation Group (PPG).The patient participation group are a group of patientswho work with the practice staff to represent the interestsand views of patients, to improve the service provided tothem.
Patients expressed a high level of satisfaction about theircare and treatment and the way the services wereprovided. They said that they were usually able to get anappointment, or were offered a telephone consultation,where needed. They were also involved in decisionsabout their care and treatment.
Patients considered that the premises were clean, andthat the facilities were accessible and appropriate fortheir needs. They described the staff as friendly andcaring, and felt that they treated them with dignity andrespect. They also said that they felt listened to, and ableto raise any concerns with staff if they were unhappy withtheir care or the service.
We also spoke with senior staff at three care homeswhere patients were registered with the practice. Theypraised the care and service patients received. They saidthat patients were promptly seen and their needs wereregularly reviewed.
Records showed that the practice/PPG carried out apatient survey in February 2012. The responses weremostly positive; 89% of people said that they were happywith the service. The practice planned to carry out afurther survey in 2015.
Representatives from the PPG told us the group hadrecently re-formed, and was working with the practice toimprove the service for patients. For example, patientshad expressed the need for further information on theextended hours and the out-of-hours service, and thishad been provided. The practice’s website had also beenupdated and photographs of staff were being displayed.
We looked at the 2014 national GP survey, which 118patients completed. The findings were compared to theregional average for other practices in the local area. Thepractice scored highest in the following areas; patientsusually got to see or speak to their preferred GP, and thelast GP they saw or spoke to was good at involving themin decisions about their care and at explaining tests andtreatments. The practice scored lowest in the followingareas; patients experience of making an appointmentand getting through to the surgery by phone.
Areas for improvementAction the service SHOULD take to improveEnsure that the learning and improvements fromsignificant events are shared with all relevant staff.
Review the recruitment policy to ensure that informationrequired by law is obtained prior to staff commencingemployment at the practice.
Keep essential records to show that all nurses and GPsare registered to practice with the relevant professionalbody prior to their employment, and remain registeredand fit to practice.
Keep essential records to show that all relevant staff areprotected from Hepatitis B infection.
Provide a designated person to lead on infection control.Ensure systems are in place to monitor the preventionand control of infection and that policies are beingfollowed appropriately.
Ensure all staff receive sufficient training to enable themto undertake their specific roles.
Ensure that arrangements are in place to enable peoplewhose first language is not English, to access informationabout services.
Summary of findings
8 Victoria & Mapperley Practice Quality Report 24/02/2015

Our inspection teamOur inspection team was led by:
Our inspection team was led by a CQC inspector andincluded a GP, practice manager and an expert byexperience. This is a person who has personalexperience of using or caring for someone who uses thistype of care service.
Background to Victoria &Mapperley PracticeVictoria and Mapperley Practice is a partnership betweenseven GPs, providing primary medical services toapproximately 7,800 patients across two locations in theinner city of Nottingham and Mapperley. Approximately2,800 of these patients use the Victoria and MapperleyHealth Centre as their main surgery, although all patientsmay access primary medical services at both locations.Mapperley Practice is registered as a separate location. Wedid not visit this practice as part of this inspection.
Victoria and Mapperley Practice provides a range ofservices including minor surgery, minor injuries, familyplanning, maternity care, blood testing, vaccinations andvarious clinics for patients with long term conditions. It is apractice for doctors in training.
The staff team includes seven GP partners, a lead nurse,two practice nurses, a treatment room nurse, a health careassistant, eight administrative staff, two office managers, apractice manager and a deputy practice manager, most ofwhom work across the two practices. Two GPs are male.
The practice holds the General Medical Services (GMS)contract with the NHS to deliver essential primary care
services. The practice opted out of providing theout-of-hours services to their own patients. Informationwas available on the website and on the practice answerphone advising patients of how to contact the out of hoursservice outside of practice opening hours.
Why we carried out thisinspectionWe carried out a comprehensive inspection of this serviceunder Section 60 of the Health and Social Care Act 2008, aspart of our regulatory functions. The practice had notpreviously been inspected and that was why we includedthem. This inspection was planned to check whether theprovider was meeting the legal requirements andregulations associated with the Health and Social Care Act2008, to look at the overall quality of the service, and toprovide a rating for the service under the Care Act 2014.
Please note that when referring to information throughoutthis report, for example any reference to the Quality andOutcomes Framework data, this relates to the most recentinformation available to the CQC at that time.
How we carried out thisinspectionPrior to our inspection we reviewed information about thepractice and asked other organisations to share what theyknew about the service. We also spoke with three partnerhealth and social care services who worked closely with thepractice.
We carried out an announced visit on 03 November 2014.During our visit we checked the premises and the practice’srecords. We spoke with the lead nurse, a practice nurse,
VictVictoriaoria && MapperleMapperleyy PrPracticacticeeDetailed findings
9 Victoria & Mapperley Practice Quality Report 24/02/2015

three GP’s, reception and clerical staff, the practicemanager and the deputy practice manager. We alsoreceived comments cards and spoke with patients andrepresentatives who used the service.
To get to the heart of patients’ experiences of care, wealways ask the following five questions of every service andprovider:
• Is it safe?• Is it effective?• Is it caring?• Is it responsive to people’s needs?• Is it well-led?
We also looked at how well services are provided forspecific groups of people and what good care looks like forthem. The population groups are:
• Older people• People with long-term conditions• Families, children and young people• Working age people (including those recently retired
and students)• People whose circumstances may make them
vulnerable• People experiencing poor mental health (including
people with dementia)
Detailed findings
10 Victoria & Mapperley Practice Quality Report 24/02/2015

Our findingsSafe Track RecordPatients told us they felt safe when using the service.Records showed that safety incidents and concerns wereappropriately dealt with. Risks to patients were assessedand appropriately managed. A system was in place toensure that staff were aware of national patient safetyalerts (NPSA) and relevant safety issues, and where actionneeded to be taken. NPSA are managed by a central teamin England, which forwards information about safetyincidents to all NHS organisations to help ensure the safetyof patients.
We reviewed incident reports and minutes of meetings forthe last 12 months. This showed the practice hadmanaged incidents consistently over time, and so couldevidence a safe track record.
Staff we spoke with were aware of their responsibilities toraise concerns, and how to report incidents and nearmisses. For example, staff had identified that a patient’sabnormal test results had not been followed up. This wasreported, the patient was informed and treated and morerobust systems were put in place to ensure that abnormalresults were acted on.
Learning and improvement from safety incidentsStaff told us that the practice was open and transparentwhen things went wrong. We saw that a system was inplace for reporting, investigating and monitoring incidents,accidents and significant events. Significant event analysisis used by practices to reflect on individual cases andwhere necessary, make changes to improve the quality andsafety of care. Records of incidents and events that hadoccurred were kept for a minimum of 10 years.
We looked at four recent significant events. These werecompleted in a comprehensive and timely way, andincluded action taken. Records showed that appropriatelearning and improvements had taken place. For example,staff had identified that a test had been carried out on apatient using out-of-date equipment. This was reported,investigated and followed up with relevant staff to addressthe error and prevent further incidents. The test wasrepeated and checks were put in place to ensure that allequipment remained in-date.
The minutes of recent business meetings showed thatsignificant events were discussed. The practice manager
and the GP partners attended the meetings. A system wasnot in place for ensuring that the learning from significantevents was shared with all relevant staff. One nurse told usthat the learning was not shared with them.
Reliable safety systems and processes includingsafeguardingThe practice had systems to manage and review risks tovulnerable children, young people and adults. Recordsshowed that all staff had received safeguarding trainingspecific to their role. For example, all GPs had completedlevel three training. Staff we spoke with knew how torecognise signs of abuse in older people, vulnerable adultsand children. They were also aware of their responsibilitiesto share information, record safeguarding concerns andcontact the relevant agencies.
Staff showed us the system in place to highlight vulnerablepatients on the practice’s electronic records system,including children and young people who were lookedafter, or on a child protection plan. The alert systemensured that they were clearly identified and reviewed, andthat staff were aware of any relevant issues when patientsattended appointments, or contacted the practice.
One of the GPs was appointed as the lead in safeguardingvulnerable adults and children. Staff we spoke with wereaware of who to speak to if they had a safeguardingconcern. The lead GP for safeguarding was aware ofvulnerable children and adults registered with the practice.Records showed that the practice worked with relevantprofessionals and partner agencies such as children’s socialcare and their health visitor and midwife to share essentialinformation about vulnerable children. They met at regularintervals to discuss safeguarding issues to ensure thatvulnerable patients were safe and protected from harm.
A chaperone policy was in place, which was visible in thewaiting area and consulting rooms. The policy referred tothe need for non-clinical staff to receive appropriatetraining to undertake chaperone duties. One of thereception staff said that they carried out chaperone dutieson occasions, which indicated that they met the criteria fora disclosure and barring (DBS) check. A DBS check helpsprevent unsuitable people, from working with vulnerablepeople, including children.
The staff member was not clear as to their responsibilitieswhen acting as a chaperone, including where to stand tobe able to observe the examination. The practice manager
Are services safe?
Good –––
11 Victoria & Mapperley Practice Quality Report 24/02/2015

confirmed that a satisfactory DBS check had not beenobtained in regards to non-clinical staff; this had recentlybeen applied for. Staff had also not received formal trainingto enable them to carry out chaperone duties effectively.They agreed to ensure that non-clinical staff did not carryout the above duties, until a satisfactory DBS check hadbeen obtained and they had received appropriate training.
We saw that patients’ individual records were managed in away to keep people safe. The practice’s electronic systemheld essential information about patients’ health andwelfare.
Medicines ManagementSeveral patients and representatives told us that thesystem for obtaining repeat prescriptions generally workedwell, to enable them to obtain further supplies ofmedicines. There were plans to introduce electronicprescribing to further improve medication safety,prescribing, efficiency and access to medicines. This willenable the practice to send a patient’s prescriptionelectronically to a pharmacy of their choice, saving thepatient time.
Systems were in place to ensure that medicines weremanaged safely and appropriately. We found thatmedicines were stored securely. Policies and procedureswere in place to protect patients against the risksassociated with the unsafe use of medicines. For example,regular checks were carried out to ensure that medicineswere within their expiry date and suitable for use. All themedicines we checked were in date. Expired and unwantedmedicines were disposed of in line with waste regulations.
We saw that arrangements were in place to ensure that theprescription forms were kept secure, and to ensure thesecurity of those being collected. We saw a recent emailfrom a GP, which identified a number of patients who hadnot had certain medicines reviewed for several years.Following the inspection, we received assurances thatthese related to minor medicines such as creams, whichhave since been reviewed.
A system was in place to oversee the management of highrisk medicines. The practice worked with the ClinicalCommissioning Group (CCG) medicines team, to ensurethat patients’ medicines were managed safely. A memberof staff from the medicines team regularly visited thepractice and carried out audits, to check that medicineswere prescribed appropriately.
Cleanliness & Infection ControlWe observed the premises were visibly clean and tidy.Cleaning schedules were in place and cleaning recordswere kept, to ensure that the practice was hygienic. Severalpatients told us they always found the practice clean andhad no concerns about cleanliness.
We saw that the infection control policy covered essentialaspects of infection control, and had been reviewedrecently. Records showed that the cleaning provider carriedout regular checks to monitor the standard of cleanliness,and ensure that appropriate practices were being followed.They also completed an infection audit on 11 August 2014,which was due to be re-audited in November 2018. Thepractice received a copy of the above reports, and sharedthe findings and any remedial actions with the staff team.However, the practice did not complete their own regularchecks or audits to provide assurances as to the standardof cleanliness. The practice manager agreed to review this.
Senior managers told us that the senior nurse was the leadfor infection control. However, the nurse said that she didnot undertake this role. It is essential that the practice has adesignated person to lead on infection control and overseethe standards. Staff we spoke with said they had receivedtraining on infection control and hand washing. Records welooked at showed that several staff had received recenttraining. The remaining staff were due to attend refreshertraining on 18 November 2014.
Staff had access to the procedures and personal protectiveequipment including disposable gloves, aprons andspillage kits, to enable them to apply infection controlmeasures.
We checked various stock supplies of clinical and medicalitems; all items were in date. Records showed that relevantstaff checked the supplies at regular intervals to ensurethey remained in date, were sealed where required, andwere used appropriately to ensure patients’ welfare.
The practice had a policy relating to the control ofLegionella (bacteria found in the environment which cancontaminate the water systems in buildings). Recordsshowed that regular checks were carried out in line withtheir policy, to help reduce the risk of infection to staff andpatients.
Following the inspection, we received a copy of the staffimmunisation policy. This stated that all health workers atrisk of exposure to Hepatitis B infection, which could be
Are services safe?
Good –––
12 Victoria & Mapperley Practice Quality Report 24/02/2015

acquired through their work should be immunised againstthis. However, complete records were not available duringor following the inspection to show that all relevant staffwere protected from Hepatitis B. The practice managerassured us that staff’s immunity status had been checked;this was recorded on their pay records. We were unable toindependently verify this.
EquipmentClinical staff we spoke with confirmed that all equipmentwas safe to use, and that they had sufficient equipment toenable them to carry out diagnostic examinations,assessments and treatments. Records showed thatequipment was regularly tested and maintained, includingitems requiring calibration such as weighing scales. Thepractice was located in shared premises. Some equipmentsuch as the wall mounted mercury sphygmometersbelonged to another provider, and they were responsiblefor maintaining them. We received confirmation that theywere checked and calibrated in March 2014. The practicemanager had requested that the above equipment beremoved from Victoria and Mapperley surgery, in view ofsafety issues relating to the use of items containingmercury.
Staffing & RecruitmentThe recruitment policy did not ensure that informationrequired by law was obtained prior to staff commencingemployment at the practice. We found that robustrecruitment procedures were not followed in practice toensure that new staff were suitable to carry out the work.
We looked at two files; both staff had been employed in thelast six months. Both files did not include the followinginformation specified in Schedule 3 of the Health andSocial Care Act 2008 (Regulated Activities) Regulations 2010to ensure they were suitable to work with vulnerable adultsor children: Satisfactory information about any physical ormental health conditions, which are relevant to theperson’s ability to carry out their work. One person’s fileincluded a gap in their employment history; there was noexplanation as to the reason for this. It also did not includeproof of their identity including a recent photograph.
Following the inspection, we received written assurancesthat the above information had been obtained. We willreview recruitment procedures at the next inspection.
The recruitment policy stated that applicants wererequired to complete an application form. However, both
staff files included a copy of their curriculum vitae (CV),which contained limited information to support theirsuitability to carry out the work. Following the inspection,the practice manager told us that further staff applying fora position would be required to complete an applicationform.
A policy for checking nurses and GPs qualifications andregistration to practice was available. The practicemanager assured us that she followed the policy. However,records were not available during or following theinspection to clearly show this. She agreed to address thisissue.
In the last 18 months the practice had appointed three newGP partners to replace partners that had retired or left. Adeputy practice manager was also appointed in April 2014;which was a new post to support the needs of the service.Where possible, the GPs covered each other’s absences. Inthe event that locum cover was required, GPs who wereknown to the practice were used.
The practice manager told us that it had been difficult tomaintain the staffing cover over recent months due to staffchanges, sickness and other circumstances. However, theteam had continued to provide cover to ensure sufficientstaff were available to meet patients’ needs. We wereassured that the staffing situation was improving.
Monitoring Safety and Responding to RiskWe found that the practice had systems in place to identifyand monitor various risks to patients, visitors and staff. Forexample, the equipment was regularly tested andmaintained to ensure it was safe to use. The practice had ahealth and safety policy, which staff had access to. Thepractice manager was the health and safety representative.
The building management company was responsible forensuring that the premises were appropriately maintainedand safe. Arrangements were in place to inform them of anyconcerns or safety issues the practice had.
Staff were able to identify and respond to risks to patientsincluding deteriorating health and well-being or medicalemergencies. For example, emergency procedures were inplace to deal with patients that experienced a suddendeterioration in health, including pregnancy complicationsand acutely ill children and young people and patients
Are services safe?
Good –––
13 Victoria & Mapperley Practice Quality Report 24/02/2015

experiencing a mental health crisis, to enable them toaccess urgent care and treatment. The practice alsomonitored repeat prescribing for patients receiving highrisk medicines.
Arrangements to deal with emergencies and majorincidentsWe saw that the business continuity plan covered a rangeof emergencies that may impact on the running of thepractice. A fire safety risk assessment had been completed,which included actions required to maintain fire safety.Following the inspection, we received confirmation that allstaff were due to attend refresher fire training and a fire drillby 9 December 2014, to ensure they knew how to evacuatethe premises and what to do in the event of a fire.
Staff we spoke with said that they had receivedcardiopulmonary resuscitation (CPR) training, and wereable to describe the action they needed to take in the eventof a medical emergency. Records showed that all staff weredue to attend refresher CPR training on 4 November 2014.We saw that various emergency equipment was available
including oxygen, a defibrillator, pulse oximeters andairway equipment for adults and children. A pulse oximeteris a medical device that monitors the oxygen levels of apatient's blood.
A system was in place to oversee that that the equipmentwas in date and appropriate to use. Clinical staff assured usthat they had received training to use the aboveequipment.
We saw that some emergency medicines were available forGPs to use in the event of a sudden deterioration inpatients’ health. The senior partner told us that the GPshad reviewed essential emergency medicines they neededto keep at a meeting in September 2014. This took intoaccount the location of the inner city practice, the nearbycommunity pharmacy, patients’ needs and where theylived and access to emergency services. Following theinspection we received a copy of the above minutes, whichshowed that the GPs had discussed and agreed a list ofmedicines they needed to keep.
Are services safe?
Good –––
14 Victoria & Mapperley Practice Quality Report 24/02/2015

Our findingsEffective needs assessmentPatients we spoke with told us they received appropriatecare and treatment. Comment cards we received frompatients, and feedback from three care homes we spokewith supported this.
Clinical staff told us that they received updates relating tolocal guidelines and current best practice from theirClinical Commissioning Group (CCG). They also receivedguidelines electronically from the National Institute forHealth and Care Excellence (NICE). The aim of theguidelines is to improve health outcomes for patients.
We saw one of the clinical staff refer to the latest guidelinesin regards to a patient they had seen that day, to ensuretheir ongoing treatment remained appropriate. Staff saidthat changes to practice and NICE guidelines werediscussed at clinical meetings. We did not see evidence ofthis in the minutes of meetings we looked at.
The practice had an established staff team who knew theirpatient groups well. They worked with local services andorganisations to meet patients’ diverse needs. The GPs andnurses had lead clinical roles relevant to their skills andknowledge, which enabled them to focus on specificconditions and to help drive improvements.
We found that patient needs were assessed and that theyreceived effective care and treatment to meet their needs.They were referred appropriately to secondary andcommunity care services on the basis of need.
Patients over 75 years of age, with complex needs, at risk ofharm or admission to hospital or receiving end of life carehad a designated GP to ensure continuity of care andtreatment. A system was in place to recall older people,those in vulnerable circumstances, those with long termconditions, or experiencing poor mental for an annualhealth review. Records showed that regularmulti-disciplinary meetings were held to review thosepatients’ needs and care plans.
As part of their General Medical Services (GMS) contractwith NHS England, the practice provided an enhancedservice to help avoid unplanned hospital admissions.Enhanced services are additional services provided by GPs
to meet the needs of their patients. We found that thepractice worked closely with partner health and social careservices, to improve outcomes for patients and enablethem to remain at home, where possible.
The senior partner told us that the practice’s rates forunplanned/emergency hospital admissions and A& Eattendance were below the regional average for otherpractices in the local Clinical Commissioning Group (CCG).
Staff worked closely with the local mental health teams toensure that patients experiencing poor mentalhealth, received appropriate care and treatment andwere regularly reviewed. Where there were signs of acutedeterioration or risk, they were supported to access urgentcare and treatment.
A significant number of patients at the practice had alearning disability. External staff we spoke with told us thatthe clinical staff had extensive knowledge andunderstanding of patients’ needs. They worked inpartnership with local care homes and the learningdisability health facilitator, to provide innovativeapproaches to meeting individuals’ needs. Patients wereoffered an annual health check. At the end of the reviewthey received a copy of their health action plan in an easyread form to meet their needs.
Staff also worked closely with the designated midwife andhealth visitor to provide antenatal and postnatal care andsupport to mothers and young children. A baby clinic washeld alternate weeks at the practice, which usually involvedthe health visitor, a practice nurse and a GP.
Babies received a new born and six week developmentassessment in line with the Healthy Child Programme.
Management, monitoring and improving outcomesfor peopleSenior staff had lead roles in monitoring and improvingoutcomes for patients. The GPs told us clinical audits wereoften linked to medicines information, safety alerts or as aresult of information from the quality and outcomesframework (QOF). QOF is a national performancemeasurement tool. The data for 2013/14 showed that thepractice achieved a total of 97.5%, which was above theaverage score for other practices in the local ClinicalCommissioning Group (CCG).
The management team made use of audit tools, peersupport and clinical supervision to assess the performance
Are services effective?(for example, treatment is effective)
Good –––
15 Victoria & Mapperley Practice Quality Report 24/02/2015

of clinical staff. We saw that a system was in place forcompleting clinical audit cycles to provide assurances as tothe quality of care, and to improve the outcomes forpatients.
Various audits and reviews had been completed in the lasttwo years, and the practice was able to demonstrate thechanges resulting from these. For example, an epipen (adisposable, pre-filled device that administers a medicine totreat a severe allergic reaction) audit was completed inJune 2014 following the publication of new guidance. Thisresulted in action been taken to ensure that relevantpatients had access to two epipens to use in the event ofan emergency, in line with the new guidance.
The practice was registered to carry out minor surgicalprocedures. The registered manager acknowledged that arecent audit of surgical procedures had not beencompleted, to evaluate the effectiveness of the diagnosis,treatment, and the incidence of complications. Theyplanned to carry out an audit in 2015.
Staff told us that the outcome of audits was communicatedthrough the clinical meetings. The meetings enabled thestaff to discuss clinical issues and peer review each other’spractice, driving improvements in care.
Effective staffingThe majority of staff had worked at the practice a numberof years, which ensured continuity of care and services.Staff told us they had received appropriate inductiontraining to enable them to carry out their work. They alsoworked well together as a team. We saw that new staffcompleted a generic induction programme. This was notdetailed or relevant to specific roles to ensure that staffreceived essential information to carry out their work.
Records showed that new staff received a copy of the staffhandbook, which included information they needed toknow. However, we found that the handbook did notinclude all essential information such as safeguarding andwhistle blowing. There was no review date to indicate whenit was last updated. The practice manager told us that itwas due to be updated in the New Year.
The practice closed for half a day each month to enable allstaff to receive time for learning. Staff told us that theywere supported to maintain and develop their skills andknowledge, and that they attended regular essentialtraining such as safeguarding, basic life support andinfection control. Records we reviewed supported this.
Staff were due to attend refresher training on fire safety,infection control and basic life support in November 2014.Staff told us that they received an annual appraisal, whichidentified their learning needs and agreed action plans.
The practice manager assured us that all GPs were up todate with their professional development requirements,and had either been revalidated or had a date forrevalidation. Revalidation is the process by which licenseddoctors are required to regularly demonstrate that they areup to date and remain fit to practice.
The surgery was a training practice. Two GPs hadundertaken training to be trainers, and other GPs weretraining to be clinical supervisors for doctors, who aretraining to be a GP. Their first GP registrar was due to jointhe practice in December 2014.
Working with colleagues and other servicesThe practice had strong links locally with other serviceproviders to aid communication and multidisciplinaryworking. For example, the senior partner also worked forthe out-of-hours service.
Staff worked with partner health and social care services tomeet patients’ needs. It was clear from discussions withstaff that considerable work went into supporting people toremain at home, and receive appropriate support ondischarge from hospital. For example, the practice workedclosely with the community matron, care coordinator andthe district nursing services to achieve this.
Information sharingA system was in place with the local out-of-hours service toenable essential information about patients to be shared ina secure and timely manner. The practice used Emis Web,which is a centralised clinical system, which helps staff tomanage patients’ records effectively. All staff were trainedon the system, which enabled scanned papercommunications, such as those from hospital, to be savedfor future reference. Electronic systems were also in placefor making referrals to secondary care.
For patients requiring emergency assessment or admissionto hospital from the practice, the GPs provided a printedsummary record for the patient to take with them. Thepractice had also signed up to the electronic SummaryCare Record. Summary Care Records provide healthcarestaff treating patients in an emergency or out-of-hours withfaster access to key information.
Are services effective?(for example, treatment is effective)
Good –––
16 Victoria & Mapperley Practice Quality Report 24/02/2015

Electronic systems were also in place for making referrals tosecondary care.
Consent to care and treatmentPatients told us that they were involved in decisions andhad agreed to their care and treatment. They also said thatthey had the opportunity to ask questions and felt listenedto. Staff told us that they obtained patients consent beforethey provided care or treatment. Written consent wasobtained for specific interventions such as minor surgicalprocedures, together with a record of the possible risks andcomplications.
Patients with learning disabilities and those with dementiawere supported to make decisions through the use of careplans. Staff gave examples of how a patient’s best interestswere taken into account if a patient did not have capacity.Clinical staff understood the importance of determining if achild was ‘Gillick’ competent, when providing treatmentand advice. (A Gillick competent child is a child under 16who is capable of understanding implications of theproposed treatment, including the risks and alternativeoptions).
Staff we spoke with were aware of the Mental Capacity Act(2005) and their responsibilities to act in accordance withlegal requirements. However, they had not received formaltraining to ensure they understood the principles of the actand the safeguards. There were no plans to provide thistraining for all staff.
All patients receiving end of life care had a ‘Right Care’ planto ensure that their wishes were respected, includingdecisions about resuscitation and admission to hospital.This information was available to the out-of-hours service,ambulance staff and local hospitals.
Health Promotion & PreventionWe saw that a wide range of health promotion informationwas available to patients and carers on the practice’swebsite, and the noticeboards in the surgery. It was thepractice’s policy to offer new patients registering had aninitial health check with the practice nurse. This ensuredthat staff had access to essential information aboutpeople’s health needs, and that any tests or reviews theyneeded could be arranged.
The practice offered a full range of immunisations forchildren, travel vaccines, shingles and flu vaccinations inline with current national guidance. The 2013/14 data forimmunisations showed that the practice was aboveaverage for the area CCG, and there was a system in placefor following up patients who did not attend.
The practice offered NHS Health Checks to all patients aged40 to 74 years. Patients were also encouraged to attendrelevant screening programmes including bowel, breastand cervical smears. A recall system was in place forfollowing-up patients who did not attend the screening.
All patients with a learning disability, poor mental health,long standing conditions or aged 75 years and over wereoffered an annual health check, including a review of theirmedication.
Are services effective?(for example, treatment is effective)
Good –––
17 Victoria & Mapperley Practice Quality Report 24/02/2015

Our findingsRespect, Dignity, Compassion & EmpathyPatients described the staff as friendly and caring, and feltthat they were treated with dignity and respect. They alsosaid that they felt listened to and that their views andwishes were respected. Staff and patients told us that allconsultations and treatments were carried out in theprivacy of a suitable room.
Representatives from three care homes we spoke withwhere patients were registered with the practice, also saidthat they felt that the staff were caring and considerate andtreated patients with respect.
Staff and patients highlighted various examples of staffproviding a caring approach. For example, a patient livingalone who did not have regular contact with family, friendsor services, received a call each week from the practicemanager to check they were alright as part of amulti-disciplinary decision.
The 2014 national GP survey showed that 63% of patientssurveyed were satisfied with the level of privacy whenspeaking to receptionists at the practice. This was belowthe Clinical Commissioning Group (CCG) regional average.
We observed that patients were treated with dignity,respect and kindness during interactions with staff.Patients privacy and confidentially was also maintained. Asign was displayed in the reception area informing patientsthat they could speak privately with staff, if required. Stafftold us that if they observed any instances ofdiscriminatory or disrespectful behaviour they would raisethis with the practice manager.
Care planning and involvement in decisions aboutcare and treatmentPatients said that they felt listened to, and were supportedto make decisions about their care and treatment. The2014 national GP survey showed that 77% of peoplesurveyed said that the last GP they last saw or spoke to,was good at involving them in decisions about their care.84% also felt the GP was good at explaining treatment andresults, and 86% felt that they were good at listening tothem.
Clinical staff told us that patients at high risk of beingadmitted to hospital had a care plan in place to help avoidthis, including elderly patients and people with complexneeds or in vulnerable circumstances. The care plansincluded patient’s end of life wishes, including decisionsabout resuscitation. This information was available to theout-of-hours service, ambulance staff and local hospitals.The practice used an alert system to ensure that theout-of-hours service was aware of the above patients’needs when the surgery was closed.
Staff told us that some patients attending the practicerequired support to make decisions about their care andtreatment, including people who had dementia or alearning disability. We saw that patients and carers hadaccess to information about local advocacy and supportservices.
Patient/carer support to cope emotionally withcare and treatmentPatients said that they received support and information tocope emotionally with their condition, care or treatment.They described the staff as caring and understanding.Where able, they were supported to manage their own careand health needs, and to maintain their independence.
The 2014 national GP survey showed that patients weresatisfied with the support they received from staff. Forexample, 83% of patients surveyed said the last GP theysaw or spoke to was good at treating them with care andconcern, and 88% said that they were good at listening.86% also said that the last nurse they saw or spoke to wasgood at treating them with care and concern. These resultswere above the CCG regional average.
The computer system identified patients who had carerresponsibilities to enable the staff to offer them support.We found that importance was given to supporting carersto care for relatives, including patients receiving end of lifecare. Bereaved carers known to the practice weresupported by way of a personal visit or phone call from aGP, to determine whether they needed any practical oremotional support.
Are services caring?
Good –––
18 Victoria & Mapperley Practice Quality Report 24/02/2015

Our findingsResponding to and meeting people’s needsSenior staff at three care homes where patients wereregistered with the practice told us that patients werepromptly seen when required. The GPs also held regularsurgeries at the care homes, to ensure that patients wereregularly seen and reviewed, which helped prevent healthissues from becoming more serious. Where possible, thesame GP visited to ensure continuity of care and treatment.
We found that the service was responsive to patients’needs. The practice provided a wide range of services tomeet patients’ needs, and enable them to be treatedlocally. The services were flexible, and were planned anddelivered in a way that met the needs of the localpopulation, with involvement of other services. Forexample, patients were able to have their blood tests doneat the practice. Staff also carried out dressing changes,wound care and electrocardiogram (ECG) tests, whichrecords the rhythm and the activity of a patient’s heart.
Records showed that regular multi-disciplinary meetingswere held, to discuss patients with complex needs or atrisk, including people with poor mental health, learningdisabilities or receiving end of life care. This helped toensure that patients and families received coordinated careand support, which took account of their needs andwishes.
The practice was involved in the enhanced service to helpprovide an early diagnosis for patients who had dementia.They were also involved in the palliative care goldstandards framework, which helps to provide the higheststandard of care for patients who are terminally ill. Thepractice worked closely with local community nursingteams and the Macmillan service to ensure that patients’end of life care took account of their needs and wishes, andresponded to changes in their needs.
The practice had a high prevalence of patients who had alearning disability, and two GP leads supported their needs.The clinical staff were able to demonstrate extensiveknowledge, skills and understanding of patients’ needs.They worked in partnership with local care homes and thelearning disability health facilitator employed by NHShealth services, to provide innovative ways of meetingindividuals’ needs. For example, a patient’s annual healthreview was carried out at a location where they felt most at
ease. They also involved health facilitators employed byNHS health services to support an individual with complexneeds to have their blood pressure checked, whopreviously had refused to have this done.
External staff we spoke with confirmed that the practiceworked in partnership with them to provide innovativeapproaches to meeting individual’s needs.
The practice also had a high prevalence of patients whohad a drug dependency. The practice had recently beenawarded the contract for providing a substance misuseclinic linked with Nottingham Crime and Drugs partnership.A GP who had undertaken relevant training held a weeklysubstance misuse surgery at the practice. This wasavailable to both patients who were registered with thepractice and others who were not. The practice had a leadGP for mental health who worked closely with localservices to support patients experiencing poor mentalhealth.
The practice worked in partnership with midwives, healthvisitors and school nurses. The practice and the designatedmidwife and health visitor provided antenatal andpostnatal care and support to young children and mothers.A baby clinic was held on alternate weeks at the practice,which usually involved the health visitors, a practice nurseand a GP.
The practice shared the building with a contraception andsexual health clinic, which offered direct access to teenageclinics, contraception and sexual health screening.
The practice had an established staff team, providingcontinuity of care and access to appointments. We saw thatsystems were also in place to ensure that patients werepromptly referred to other services, where required.
Systems were also in place to ensure that test results,information from the out-of-hours service and letters fromthe local hospitals including discharge summaries werepromptly seen, correctly coded and followed up by a GP,where required. However, we saw some actions on thesystem, which showed that patients had not been promptlyfollowed up or reviewed. The registered manager agreed toreview this. Following the inspection, we received writtenassurances that the review highlighted no risk to patients.With the exception of two tasks, actions had been taken,
Are services responsive to people’s needs?(for example, to feedback?)
Good –––
19 Victoria & Mapperley Practice Quality Report 24/02/2015

and that the two with no actions were from the previousday. The practice planned to review the effectiveness of theabove systems at the partners meeting on the 17thNovember 2014.
The Patient Participation Group (PPG) had not been activesince 2012. The deputy manager had taken on the lead roleto help re-establish the PPG, and two recent meetings hadbeen held. Members of the PPG said that they felt that theyhad the full support of the practice.
Tackle inequity and promote equalityThe practice had recognised the needs of different groupsin the planning of its services, and worked with partnerhealth and social care services to understand and meetpatients’ diverse needs. Staff informed us they operated anopen list culture, accepting patients who lived within theirpractice boundary.
Staff told us there was a wide range of diversity within thepatient population. Staff were able to describe a goodawareness of culture and ethnicity issues. Records showedthat various staff had received training on equality anddiversity. The practice had a large number of patientswhose first language was not English.
The staff were knowledgeable about language issues, andhad access to language line (a telephone translator service)to obtain assistance in consultations in different languages.Staff and patients also had access to local interpreters,where required. A folder was also available in the receptionto help staff to identify patients’ first language if this wasnot clear. However, the practice’s website did not have atranslation facility to enable people whose first languagewas not English, to access the information about theservices.
Records showed that home visits and longer appointmentswere available for patients who needed them, includingpeople in vulnerable circumstances, experiencing poormental health, with complex needs or long termconditions.
The premises and the facilities considered the needs ofpeople with disabilities. For example, the facilities wereaccessible for people in a wheelchair, and mothers withyoung children in a pushchair.
Access to the servicePatients we spoke with and comments cards we receivedshowed that patients were able to get an appointment, or
were offered a telephone consultation, where needed.None of the patients we spoke with or who completed acomment card expressed difficulty in getting through to thepractice by phone.
The 2013/2014 national GP survey showed that 82% ofpeople surveyed, were able to get an appointment to seeor speak to a clinician the last time they tried. Whilst 62%said that they had not found it easy to get through to thepractice by phone.
Staff told us that the appointment system and telephoneresponse times were regularly checked, to ensure that thepractice responded to patients’ needs. The practicemanager acknowledged that these had not been formallyreviewed or audited in the last two years, to provideassurances that it was meeting patients’ needs. She agreedto formally review these.
Patients were able to book an appointment in person, bytelephone or on line. Extended opening hours wereavailable alternative Saturdays from 8:30 am until 12:30pm, providing nurse led appointments with a GP on call.This enabled children and young people to attendappointments outside of school hours. It also enabledworking age patients and those unable to attend on weekdays, to attend at the weekend.
We saw that systems were in place to prioritise emergencyand home visit appointments, or phone consultations forpatients who were not well enough to attend the practice.We observed staff adding patients who needed to bereviewed urgently to the GPs appointments to be seen thatday, or arranging for a call back from a doctor.
Information about the appointment system, opening timesand the out-of-hours service was available in the receptionarea and on the practice’s website. The practice had a widerange of patients of culture and ethnicity issues populationis predominantly white British. Staff we spoke with wereaware that they could access a translator for patientsattending the practice whose first language was notEnglish. We saw that information in different languages wasavailable in the reception area, informing people that atranslator service was available, if required.
The practice occupied the ground floor area of a sharedbuilding. We found that the facilities and the premises wereaccessible and were largely appropriate for the servicesbeing delivered.
Are services responsive to people’s needs?(for example, to feedback?)
Good –––
20 Victoria & Mapperley Practice Quality Report 24/02/2015

Listening and learning from concerns andcomplaintsPatients said that they felt listened to and able to raiseconcerns about the practice. They were aware of theprocess to follow should they wish to make a complaint,but they had not had cause to do so.
We saw that the complaints procedure was accessible topatients on the practice’s website and at the surgery.This required amending to ensure that people had accessto consistent and up-to-date information. For example, thewebsite stated that a person’s complaint could also bedealt with by the local Primary Care Trust, whilst the leafletin the practice referred people to the Health ServiceOmbudsman if they were not satisfied with the practice’sresponse. There was no reference to the fact that peoplemay direct their complaint to NHS England area teamrather than the practice. The practice manager agreed toupdate the information.
We saw that a system was in place for handling complaintsand concerns. We looked at the records of complaintsreceived in the last 12 months. The records largely showedthat concerns had been acknowledged, investigated andresponded to in line with the practice’s policy. However, aclear audit trail was not available in regards to certaincomplaints. The practice manager assured us that furtherinformation was held elsewhere. She agreed to keep a clearlog and file of all complaints received to show that they hadbeen handled in line with the NHS procedure andcontractual obligations for GPs.
Staff told us that there was a culture of openness and thatthey were encouraged to raise concerns. They also said thatcomplaints were shared with staff at team meetings, andwere acted on to improve the service for patients. Recordsof meetings supported this. Staff had access to thecomplaints policy. Records showed that complaints werereviewed to identify any patterns and trends, and to ensurethey had been responded to properly.
Are services responsive to people’s needs?(for example, to feedback?)
Good –––
21 Victoria & Mapperley Practice Quality Report 24/02/2015

Our findingsVision and StrategyThe aims and values set out in the provider’s statement ofpurpose were to provide high quality care and services topatients. Most staff we spoke with were not aware of theprovider’s statement of purpose or future plans for theservice. However, all staff were clear that they placed thebest interests and welfare of their patients at the heart ofeverything they did.
Records showed that regular business meetings were held,where future plans were discussed. The senior partner toldus that due to recent partner changes and circumstances,the new partnership had yet to set out a business plan andclear plans for future development.
Governance ArrangementsThe practice had a range of policies and procedures inplace to govern the practice. These were available to staffelectronically. A system was in place to ensure that thepolicies were regularly reviewed and were up-to-date, andthat these were shared with staff.
Several policies we looked at had recently been reviewed.However, we found that certain policies were not robust togovern the practice, and ensure that staff followed therequired procedures. For example, the recruitmentprocedure did not ensure that information required by lawwas obtained prior to staff commencing employment atthe practice. In view of this, robust procedures werenot followed in practice to ensure that new staff weresuitable to carry out the work.
Records showed that the GP partners held monthlymeetings to discuss the practice’s business, finances,governance and performance. Regular meetings were alsoheld to discuss clinical issues and to share best practice.Several clinical audits were completed in the last two years,which showed that appropriate action was taken toimprove the quality of the service, and to ensure thatpatients received appropriate care and treatment.
The practice used performance data to measure theirservice against other practices and identify areas forimprovement. This included the use of Quality andOutcomes Framework (QOF), which is a nationalperformance tool designed to reward good practice. The2013/14 data for this practice showed it was performing in
line with, or above national standards. Records showedthat the QOF data was discussed at team meetings, andaction plans were produced to maintain or improveoutcomes.
Senior managers demonstrated a commitment toimproving the quality of care and services for patients.However, the practice had undergone considerablechanges in the last 18 months, which had affected theability to drive improvements.
Various systems were in place to monitor the quality ofservices, including complaints, incidents, safeguarding,and medicines management. However, we highlightedareas where robust systems were not in place to driveimprovements and provide assurances that policies werebeing followed. Following the inspection, we receivedassurances that the monitoring arrangements had beenstrengthened to oversee all aspects of the service.
Leadership, openness and transparencyWe were shown a leadership structure, which includedseven GP partners, a practice manager, a deputy practicemanager and four practice nurses. All senior staff had leadroles and responsibilities to ensure that the service waswell led. For example, one of the partners was the lead formental health, learning disabilities, finance, contracts andperformance, whilst another partner was the lead for drugsmisuse and medicines management.
Most staff we spoke with were clear about their roles andresponsibilities, and felt that the practice was well led. Theyalso said that they felt valued, well supported, and involvedin decisions about the practice. Staff described the cultureof the organisation as supportive and open, and felt able toraise any issues with senior managers as they wereapproachable. The practice manager had an ‘open door’policy to discuss any concerns or suggestions.
A whistleblowing policy was in place and staff were awareof this, but they had not had cause to use it. Recordsshowed that regular team meetings were held, whichenabled staff to share information and to raise any issues.
Practice seeks and acts on feedback from users,public and staffThe practice obtained feedback from patients throughsurveys and complaints. Patients said that they felt able toraise concerns, compliments or complaints with the staff.Information received was acted on, and changes weremade, where possible.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
22 Victoria & Mapperley Practice Quality Report 24/02/2015

The Patient Participation Group (PPG) is a group of patientswho work with the practice to represent the interests andviews of patients, to improve the service provided to them.The deputy manager had taken on the lead role to helpre-establish the PPG, which had not been active since 2012and two recent meetings had been held.
Members of the PPG said that they felt that they had the fullsupport of the practice. They were asked for their views toimprove the service, and their suggestions were acted on.For example, in response to feedback the practice’s websitehad recently been updated, and staff photographs werebeing displayed.
Records showed that the PPG/practice carried out a patientsurvey in February 2012. The responses were mostlypositive; 89% of people said that they were happy with theservice. The practice manager told us that they planned tocarry out a further patient survey in 2015, with involvementof the PPG.
As part of GPs annual appraisal of their work, recordsshowed that a number of patients had recently completedthe General Medical Council’s survey. The survey providesfeedback on a GPs conduct and skills to carry out theirwork. We looked at four GPs survey results, which showedhigh levels of patient satisfaction.
Discussions with staff and records reviewed showed thatthe practice obtained feedback from staff through teammeetings and appraisals. Staff said that they felt involvedin decisions about the practice, and were asked for theirviews about the quality of the services provided.
Management lead through learning &improvementStaff told us that they were supported to maintain anddevelop their skills and knowledge. For example, one nursewas being supported to complete the practice nursefoundation programme to develop her knowledge andskills. Several staff records we looked at did not includeevidence of all training they had received to carry out theirwork effectively. The practice manager agreed to addressthis issue.
The practice manager acknowledged for reasons that mostof the non-clinical staff and two of the nursing staff whoworked at the practice, had not received an annual reviewof their performance in the last 12 months. We were toldthat three staff members had received a recent appraisal,although the notes had yet to be completed.
A clear plan was not in place relating to the completion ofall staff appraisals. The practice manager assured us thatall staff would receive an appraisal by the end of March2015. We were shown examples of several completedappraisals of staff that worked at the provider’s otherpractice, which set out their performance, learning anddevelopment needs.
Records showed that accidents, incidents and significantevents were reviewed to identify any patterns or issues, andthat appropriate actions were taken to minimise furtheroccurrences. Records showed that appropriate learningand improvements had taken place, and that the findingswere communicated to staff.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
23 Victoria & Mapperley Practice Quality Report 24/02/2015