VennDiag Lola (3)
-
Upload
elsya-paramitasari -
Category
Documents
-
view
217 -
download
0
Transcript of VennDiag Lola (3)
-
7/27/2019 VennDiag Lola (3)
1/72
-
7/27/2019 VennDiag Lola (3)
2/72
PATIENT IDENTITY
Name : Mrs. ER
Age : 39 years old
Marital state : married
Admission date : May 2nd, 2013
-
7/27/2019 VennDiag Lola (3)
3/72
10 STEPS VENNDIAG
1. Define a Chief Complaint
2. Draw a VennDiag & Fill It With Possible Disease
3. Literature Review
4. Scan on Patient Signs & Symptoms
5. Make a Working Diagnosis
6. Define Initial Treatment
7. Further Investigation
8. Make a Definitive Diagnosis
9. Define Causative Treatment10. Show a Clinical Course of the Disease
-
7/27/2019 VennDiag Lola (3)
4/72
STEP VENNDIAG
STEP 1 : Define the Chief Complaint
Step 2 : Draw a Venndiag and Fill it with Possible Diseases
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a Working Diagnosis
-
7/27/2019 VennDiag Lola (3)
5/72
STEP 1 : DEFINE THE CHIEF COMPLAINT
Female 39 years old, came with acute
diarrhea
-
7/27/2019 VennDiag Lola (3)
6/72
STEP VENNDIAG
STEP 1 : Define the Chief Complaint
Step 2 : Draw a Venndiag and Fill it with Possible Diseases
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a working diagnosis
-
7/27/2019 VennDiag Lola (3)
7/72
INFECTIOUSNON INFECTIOUS
Protozoa : Giardia, Cryptospora
Bacterial : Vibrio cholera
Viral : Rotavirus, Norwalk
Bacterial: Shigella, Campylobacter, Salmonella,
Escherchia coli, Aeruginosa
Protozoa: Entamoeba hystoliytica
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel SyndrommeThyroid Storm
Acute appendicitis
Drugs: NSAIDs
Inflammatory Bowel
Disease
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A Medical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. 2nd eds. Philadelphia : Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
ACUTE DIARRHEA
Acute Bloody
Acute Watery
-
7/27/2019 VennDiag Lola (3)
8/72
STEP VENNDIAG
STEP 1 : Define the Chief Complaint
Step 2 : Draw a Venndiag and Fill it with Possible Diseases
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a Working Diagnosis
-
7/27/2019 VennDiag Lola (3)
9/72
INFECTIOUSNON INFECTIOUS
Acute Watery
Protozoa : Giardia, Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Acute Bloody
Bacterial: Shigella, Campylobacter, Salmonella,
Escherchia coli, Aeruginosa
Protozoa: Entamoeba hystoliytica
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Acute appendicitis
Drugs: NSAIDs
Inflammatory Bowel
Disease
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A Medical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. 2nd eds. Philadelphia : Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
ACUTE DIARRHEA
-
7/27/2019 VennDiag Lola (3)
10/72
COMMON IN INFECTIOUS
ACUTE WATERRY DIARRHEA
Waterry diarrhea
Blood (-)
Abdominal pain Nausea and vomit
Fever
-
7/27/2019 VennDiag Lola (3)
11/72INFECTIOUS
Protozoa : Giardia lamblia
Symptom :Sulfurous
bleaching
Flatus
Loose stools withmucus (-)
Diagnose :
Antigens in the feces
Cysts in the feces
Trophozoites in the
feces or small intestine
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Physical :Bloating abdominal
Extra intestinal :
Urticaria Anterior uveitis
Artritis
-
7/27/2019 VennDiag Lola (3)
12/72INFECTIOUS
Protozoa : Cryptosporidium
Symptom :Immunocompetent
host
Anorexia
Weight loss
Diagnose : Small oocyts , cyst,
trophozoites in feces
Direct immunofluorescent
stains
Enzyme immunoassay
Biopsy specimen of thesmall bowel
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Physical : Low fever
Dehydration
-
7/27/2019 VennDiag Lola (3)
13/72INFECTIOUS
Bacterial : Vibrio cholera
Diagnosed by
Dark field microscopy on wet mount of freshstool : V. Cholera
Antiserum specific: serotype
Isolation with thiosulfate-citrate-bile salts-sucrose
(TCBS) agar : flat yellow colony .
Biochemical confirmation : oxidase +
Monoclonal Ab in PCR : V. Cholerae O1 and O 139
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Symptom :
- Incubation 24 - 48 hour- Fever (-)
- Sudden painless quickly become
voluminous
- The stool: nonbilious, gray, slightly
cloudy fluid with fleck s of mucus =
rice water stool
- Odor sweet
Physical :
- Muscle cramps electrolyte
imbalance
-
7/27/2019 VennDiag Lola (3)
14/72INFECTIOUS
Virus : Rotavirus and Norwalk
Diagnosed
EIAs (Enzyme immunoassay) PCR
WBC normal, rarely leucocytosis with
relative lymphopenia
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Symptom :
- Incubation 1-3 day, abrupt onset- Mostly in children
- Chill and myalgia
- Mucus (-)
- Self limiting
Physical :
- High fever > 39 c
-
7/27/2019 VennDiag Lola (3)
15/72INFECTIOUS
Virus : Rotavirus and Norwalk
Diagnosed
EIAs (Enzyme immunoassay) PCR
WBC normal, rarely leucocytosis with
relative lymphopenia
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Symptom :
- Incubation 1-3 day, abrupt onset- Mostly in children
- Chill and myalgia
- Mucus (-)
- Self limiting
Physical :
- High fever > 39 c
-
7/27/2019 VennDiag Lola (3)
16/72
INFECTIOUSNON INFECTIOUS
Protozoa : Giardia, Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella, Campylobacter,
Salmonella, Escherchia coli, AeruginosaProtozoa: Entamoeba hystoliytica
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Acute appendicitis
Drugs: NSAIDs
Inflammatory Bowel
Disease
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A Medical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. 2nd eds. Philadelphia : Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
ACUTE DIARRHEA
Acute Bloody
Acute Watery
-
7/27/2019 VennDiag Lola (3)
17/72
COMMON IN INFECTIOUS
ACUTE BLOODY DIARRHEA
Bloody diarrhea
Blood (+)
Mucus (+/-)
Abdominal pain Nausea and vomit
Fever
Malaise
Diagnosed with oocyst/trophozoit in feces, high PMN in feces Leucocytosis peripher
-
7/27/2019 VennDiag Lola (3)
18/72
INFECTIOUS
Protozoa : Entamoeba hystolitica
Symptom
Incubation : 2-6 weeks
May pass 10-12 stools per day
The stool: little fecal material, consist
mainly blood and mucus
Diagnosed by
- Culture of stool forE. Hystolytica
tropozoites
- PCR assay for DNA in stool
- ELISA ag E. hystolytica
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
PhysicalWeight loss
Diffuse lower abdomen or back pain,
cramping
-
7/27/2019 VennDiag Lola (3)
19/72
Bacterial : Shigella
INFECTIOUS
Symptom : 4 stages
Incubation Period
- Lasts 1-4 days- Transient fever (40-41c)
Watery Diarhhea
Mild abdominal discomfort severe cramps,
tenesmus
Dysentry
Follow hours or days. Uninterupted excretion
of small volume ofbloody mucopurulent
stool diarrhea with increased tenesmus and
abdominal cramps
Post infection
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Diagnosed
- Isolation pathogen from fecal material
Medium: agar mac conkey:nonlactose fermeting colonies: 0,5-1mm in
diameter, convex, translucent, smooth
surface
-
7/27/2019 VennDiag Lola (3)
20/72
Bacterial : Campylobacter
INFECTIOUS
Symptom
Prodorme 12-48 hour before onset ofdiarrheal
- Degree of diarrhea varies from several
loose stool to grossly blood stool,
> 10 bowel movement
- Abdominal pain: cramping, general/local
Diagnosed
- Direct microscopy: vibroid morphology- Isolate from culture of stool, blood
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Physical
- Abdominal pain: cramping, general/local
-
7/27/2019 VennDiag Lola (3)
21/72
Bacterial : Salmonella
INFECTIOUS
Symptom
Incubation 10-14 days (3-21 days)- High fever characteristic
- Coated tongue, splenomegaly,
abdominal tenderness
Diagnosed by
- Leukopenia, neutropenia- Elevated liver function test and muscle
enzyme level
- Isolation of S. Typhi or S. Paratyphi from
blood, bone marrow
- Widal test
- PCR and DNA assay : S.typhi in blood
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17th
eds.
Physical
- Coated tongue, splenomegaly,abdominal tenderness
-
7/27/2019 VennDiag Lola (3)
22/72
INFECTIOUS
Symptom
Incubation 24 - 72 hours. Other symptoms may include:
Distension abdominal
Bacterial : Escherchia.coli
Diagnosed by
- E. coli strains O157, is the most
common method currently used to
detect STEC/EHEC
- Testing forShiga toxins or toxin genes
is more sensitive, specific, and rapid. It
detects both non- O157 STEC/EHEC
and sorbitol-fermenting strains ofO157:H7difficult to identify.
Vorvick LJ. E.coli Enteritis. US National Library of Medicine NIH. Medline. 2011
Physical
Gas in abdominal
Bruises that happen easily
Pale skin
Red or bloody, reduced amount
urine
-
7/27/2019 VennDiag Lola (3)
23/72
Bacterial : Aeruginosa
- Immunocompromised
host- Antibiotic associated
- Profuse diarrhea, mucus
+, blood +
- Low-grade fever
Diagnosed
- Innoculation on blood agar platesand Mac Conkey agar plates, then
incubated at 370c for 18-24 hours
InfectiousPorco EV, Visconte EB. Pseudomonas Aeruginosa as a Cause of Infectious Diarrhea Successfully Treated With Oral Ciprofloxacin. Department of Internal
Medicine. Pubmed. USA. 1995 Nov;29(11):1122-3
Brad GF et al. Pseudomonas Aeruginosa and Antibiotic Associated Diarrhea In Children. Department of Pediatric, Victor Babes University Medicine andPharmacy. Timisora. Jan 2011.
-
7/27/2019 VennDiag Lola (3)
24/72
INFECTIOUSNON INFECTIOUS
Protozoa : Giardia, Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella, Campylobacter, Salmonella,
Escherchia coli, Aeruginosa
Protozoa: Entamoeba hystoliytica
Drugs
Toxins
Dietary: Intoleransi lactosaIrritable Bowel Syndromme
Thyroid Storm
Acute appendicitis
Drugs: NSAIDs
Inflammatory Bowel
Disease
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A Medical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. 2nd eds. Philadelphia : Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
ACUTE DIARRHEA
Acute Bloody
Acute Watery
-
7/27/2019 VennDiag Lola (3)
25/72
COMMON IN NON INFECTIOUS
WATERY DIARRHEA
Fever (-)
Watery diarrhea
Abdominal pain
Nausea and vomit
Hematology routine : normal
Feses routine :
Erytrocyte (-)
Leucocyte (-)
-
7/27/2019 VennDiag Lola (3)
26/72
NON INFECTIOUS
Drugs and Toxin
- Antibiotics: cephalosporin,
amynoglicoside, amoxillin clavulanate,
clarithomycin
- Cardiac antidysrhthmics,
antihypertensive
- certain depressant, chemotherapeutic
agent
- Brochodilator- Antacid
- Laxatives
Toxin caused acute watery diarrhea
- Organophospate inseticides
- Amanita and other mushroom- Arsenic
- Preformed in seafood
Physical History of consumption/ingest
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Diagnose Hematology routine : normal Feses routine :
- Erytrocyte (-)- Leucocyte (-)
-
7/27/2019 VennDiag Lola (3)
27/72
NON INFECTIOUS
Lactose Intolerance
Symptom
- Flatus
- History of ingest carbohydrates that
contain actively transported
monosaccharide (ec: glucose, galactose)
Diagnosed by Stool fat/steatorrhea quantitative Test- Sudan III stain Blood breath and isotopic test Blood routine: depletion iron, folate,
cobalamin, vitamins D and K Schilling test, D-xylose test, duodenal
mucosal biopsy, small intestinal RO, test ofpancreatic exocrine function
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
- Flatus
- History of ingest carbohydrates thatcontain actively transported
monosaccharide (ec: glucose, galactose)
Irritable Bowel Syndromme
-
7/27/2019 VennDiag Lola (3)
28/72
Abdominal pain/discomfort (25%hypogastrium, 20% right side, 10%epigastrium. Episodic and crampy, can be
constant, nocturnal pain, exacerbate byeating, emotional stress, improved bypassage of flatus/stools
Constipation > diarrhea. Diarrhea in smallvolume 200-300 ml/d
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Th id St
-
7/27/2019 VennDiag Lola (3)
29/72
Agitation
Tachycardia
Sweating
Fever
Seizure
History of hypertiroidism
*Non Infectious
Thyroid Storm
T1 dan T4
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
A t di iti
-
7/27/2019 VennDiag Lola (3)
30/72
Anorexia
Pain in periumbilical goes to rightupper quadrant
*Non Infectious
Acute appendicitis
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
Pain in mc burney area
Rebounf tenderness
Fever 37,2 - 38
USG
Ct scan: thickened appendix with
periappendical
-
7/27/2019 VennDiag Lola (3)
31/72
INFECTIOUSNON INFECTIOUS
Protozoa : Giardia, Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus,
Norwalk
Bacterial: Shigella, Campylobacter,
Salmonella, Escherchia coli, Aeruginosa
Protozoa: Entamoeba hystoliytica
Drugs
ToxinsDietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Acute Appendicitis
Drugs: NSAIDs
Inflammatory Bowel
Disease
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A Medical Guide to the Differential Diagnosis of Symptoms, Signs, and Clinical Disorders. 2nd eds. Philadelphia : Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
ACUTE DIARRHEA
Acute Bloody
Acute Watery
-
7/27/2019 VennDiag Lola (3)
32/72
COMMON IN NON INFECTIOUS
BLOODY DIARRHEA
Fever (-)
Bloody diarrhea
Abdominal pain
Nausea and vomit
Hematology routine : normal
Feses routine :
Erytrocyte (-)
Leucocyte (-)
-
7/27/2019 VennDiag Lola (3)
33/72
NON INFECTIOUS
Drugs
- Causes: NSAIDs
- Mild side effects from short-termuse may include diarrhea
- Blood related ulcerbecause
long term use
Diagnosed by
History of consumption Hematology routine : normal Feses routine :
- Erytrocyte (-)- Leucocyte (-)
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17 th eds.
-
7/27/2019 VennDiag Lola (3)
34/72
NON INFECTIOUS
Inflammatory Bowel Disease
Crohns disease Ulcerative colitis
Clinical Findings Weight loss, low grade fever, perianal
disease, abdominal mass
Rectal bleeding,tenesmus, crampy,
liquid stool containing blood, pus
Laboratory Elevated CRP, ESR, more severe
hypoalbuminemia, anemia, leucocytosis
Rise in CRP, platelet count, ESR,
leucocyte, and decrease Hb
Spesific marker:
- fecal lactoferin intestinal
inflammation
- Fecal calprotectin histologic
inflammation, prognosis,
Endoscopy Patchy involvement, rectal sparing,
aphthous ulcers, ileal ulcers
Rectal involvement with continuous
superficial ulceration.
Radiology Stricture, fistulas, terminal ileal disease
(string sign), skip lesieon
Loss of haustra, continous ulceration,
collar button ulcer
1. Fauci, Anthony S. 2009. Harrisons Manual of Medicine. 17th
eds.
-
7/27/2019 VennDiag Lola (3)
35/72
STEP VENNDIAG
STEP 1 : Define the Chief Complaint
Step 2 : Draw a Venndiag and Fill it with Possible Diseases
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a Working Diagnosis
C
-
7/27/2019 VennDiag Lola (3)
36/72
HISTORY TAKING
Characteristic:
- Acute Diarrhea started 12 hours before admissionDiarrhea characteristic :
- Watery - Frequency > 8 times/day
- Mucus (+) - Stool volume > 250 ml
- Blood (+), no gross, no pus
- Bad stink
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeruginosa
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. InflammatoryBowel Disease
Possible : 1, 3, 4,5,6
Less : 2
Not related : 7,8
-
7/27/2019 VennDiag Lola (3)
37/72
HISTORY TAKING
High fever 38c
Continous
No spesific characteristic
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. InflammatoryBowel Disease
Possible : 1, 3, 4,5,6
Less : 2, 3, 8
Not related : 7
-
7/27/2019 VennDiag Lola (3)
38/72
HISTORY TAKING
Nausea
Vomit (-)
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeromonas
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. InflammatoryBowel Disease
Possible : 2,4,5,6
Less : 1, 3, 7, 8
Not related :
W i ht L
-
7/27/2019 VennDiag Lola (3)
39/72
HISTORY TAKING
Weight Loss DrugsToxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli5. Aeruginosa
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. Inflammatory
Bowel Disease
Possible : 6,8
Less : 1,2,3,4,5,7
Not related :
-
7/27/2019 VennDiag Lola (3)
40/72
HISTORY TAKING
History consumption of food
in the street
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella4. Escherchia coli
5. Aeromonas
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. Inflammatory
Bowel Disease
Possible : 1,2,3,4,6
Less : -
Not related : 5, 7,8
-
7/27/2019 VennDiag Lola (3)
41/72
HISTORY TAKING
History of her children was admitted
hospital because of amoeba
diarrhea
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
Acute
Bloody7. NSAIDs
8. InflammatoryBowel Disease
Possible : 6
Less : -
Not related : 1,2,3,4, 5,7,8
f
-
7/27/2019 VennDiag Lola (3)
42/72
HISTORY TAKING
History of consumption drug
induced acute bloody diarrhea
was denided
Drugs
Toxins
Dietary: Intoleransi lactosa
Irritable Bowel Syndromme
Thyroid Storm
Protozoa : Giardia,
Cryptospora
Bacterial : Vibrio choleraViral : Rotavirus, Norwalk
Bacterial: Shigella,
Campylobacter,
Salmonella, Escherchia
coli, Aeromonas
Protozoa: Entamoeba
hystoliytica
Drugs: NSAIDs
Inflammatory Bowel
Disease
ACUTE DIARRHEA
Acute Bloody
Acute Watery
Acute
Bloody
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeromonas
Protozoa
6.Entamoeba hystoliytica
Acute Diarrhea
7. NSAIDs
8. InflammatoryBowel Disease
Possible : -
Less : -
Not related : 1,2,3,4, 5,67,8
L t h M h 30th 2013
-
7/27/2019 VennDiag Lola (3)
43/72
HISTORY TAKING
Last menarche March 30th, 2013
History of Diabetes Mellitus
Medication since 3 years ago: glimepirid 1x1 grmetformin 1x500 mg
No history of Hypertension
No history of Alergic
-
7/27/2019 VennDiag Lola (3)
44/72
PHYSICAL EXAMINATION
Vital sign:
- General appearance : moderately ill
- Conciousness : compos mentis
- Blood Pressure : 100/60 mmHg
- Pulse : 96x/min ( reguler rhythm, strong, and full in palpation )
- Respiratory rate : 22x/min
- Axillary temperature : 39,6 C
- H/W : 154 cm / 57 kg
- BMI : 24,1 kg/m2 (overweight)Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.
InflammatoryBowel
Disease
Possible : 1,2,3,4,6
Less : 5
Not related : 7,8
Acute
Bloody
H d h l
-
7/27/2019 VennDiag Lola (3)
45/72
PHYSICAL EXAMINATION
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeromonas
Protozoa
6.Entamoeba
hystoliytica
AcuteDiarrhea
7. NSAIDs
8.
InflammatoryBowel
Disease
Head : normocephaly
Eye : conjunctiva anemic -/-
Nose : normal
Ear : normal Mouth : dry mucosa lip and oral
Neck : nodul lymph not palpable
Acute
BloodyPossible : 1,2,3,4,5,6
Less : 7, 8
Not related : ----
Lungs ( normal )
-
7/27/2019 VennDiag Lola (3)
46/72
PHYSICAL EXAMINATION
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
AcuteDiarrhea
7. NSAIDs
8.
InflammatoryBowel
Disease
Acute
Bloody
Lungs ( normal )
Inspection : symetric in both static and dynamic state.
Palpation : fremitus tactile equal on both lungs.
Percussion : sonor
Auscultation : vesicular breath sounds, no additional sound. Heart :
Inspection : ictus cordis visible
Palpation : ictus cordis is palpable in ICS V linea midclavicularis sinistra
Percussion
- upper border : ICS 3 linea parasternalis sinistra
- right border : linea sternalis dextra
- left border : linea midclavicularis sinistra
Auscultation : regular heart sound, no additional sound
-
7/27/2019 VennDiag Lola (3)
47/72
PHYSICAL EXAMINATION
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
AcuteDiarrhea
7. NSAIDs
8.
InflammatoryBowel
Disease
Acute
Bloody
Abdomen:
Inspection : convex
Palpation : pain (+) lower abdominal
hepatosplenomegaly -
Percussion : timpaniAuscultation : bowel sound 12-13x/minute
Extremities : CRT < 2 second, warm
Skin : turgor normal
Possible : 1,2,3,5,6
Less : 4, 7, 8
Not related : ----
Female 39 years old came with acute diarrhea 12 hours before admission
-
7/27/2019 VennDiag Lola (3)
48/72
RESUME
Female 39 years old, came with acute diarrhea 12 hours before admission.- Diarrhea characteristic : watery+, mucus (+), blood (+) no gross, no pus, frequency >
8 times/day, stool volume >250 ml,high fever 38c =1,3,4,5, 6
- Nausea = 2,4,5,6
- Weight loss = 6, 8
- History of comsumption food in the street = 1,2,3,4, 6
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.
Inflammatory
Bowel
Disease
Acute
Bloody
-
7/27/2019 VennDiag Lola (3)
49/72
- History of her children was admitted hospital because of amoeba diarrhea = 6
- History of diabetes mellitus, her medication since 3 years ago : glimepirid 1x1 gr and
metformin 1x500 mg.
RESUME
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.Inflammatory
Bowel
Disease
Acute
Bloody
Possible : 4, 6
Less : 2,3,5
Not related : 8
-
7/27/2019 VennDiag Lola (3)
50/72
Physical examination found
-Axillary temperature 39,6 C =1,2,3,4, 6
- Dry lip and oral mucosa = 1,2,3,4,5, 6
-Abdomen seemed convex, pain in lower abdominal, = 1,2,3,5, 6
tympani, bowel sound 12 -13x/minute
RESUME
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.Inflammatory
Bowel
Disease
Acute
Bloody
Possible : 1,2,3, 6
Less Possible : 4,5
-
7/27/2019 VennDiag Lola (3)
51/72
STEP VENNDIAG
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a Working Diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
-
7/27/2019 VennDiag Lola (3)
52/72
WORKING DIAGNOSIS
Acute Gastroenteritis et causa Entamoeba hystolytica
Acute Gastroenterit is et causa Shigella
Acute Gastroenterit is et causa Campylobacter
Acute Gastroenterit is et causa Salmonella
Acute Gastroenteritis et causa Escherchia coli
EXCLUDED
Acute Gastroenteritis et causa Aeruginosa
Acute Gastroenteritis et causa NSAIDs Acute Gastroenteritis et causa Inflammatory Bowel Disease
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.Inflammatory
Bowel
Disease
Acute
Bloody
-
7/27/2019 VennDiag Lola (3)
53/72
EXCLUDED
Acute Gastroenteritis et causa NSAIDs
No history of consumption NSAIDs
Acute Gastroenteritis et causa Inflammatory
Bowel Disease
- Chrons disease
Perianal disease, low grade fever, abdominal
mass
- Colitis ulcerativa
Rectal bleeding, tenesmus, liquid stool
containing blood (+) pus (+)
Acute Gastroenteritis et causa
Aeruginosa
No history consumption antibioticNo immunocompromised host
Low grade fever
-
7/27/2019 VennDiag Lola (3)
54/72
STEP VENNDIAG
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a working diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
STEP 8 : Make a Definitive Diagnosis
STEP 9 : Define the Causative Treatment
INITIAL TREATMENT
-
7/27/2019 VennDiag Lola (3)
55/72
INITIAL TREATMENT
Female 39 years old, came with acute diarrhea 12 hours before admission.1. Diarrhea characteristic : watery+, mucus (+), blood (+) no gross, no pus, frequency > 8
times/day, stool volume >250 ml, got dry lip and oral mucosa.For this condition :
REDUCE the diarrhea with
Antispasmodic (Buscopan 10 mg 1 tab)
Antidiarrheal (New Diatabs 2x 600 mg
CORRECT for mild dehydration
Begin IV fluid with isotonic fluid
Fluid theraphy = maintenance + 5% deficit of body weight
= 30 ml/kgBB + 5% BB(kg)
= (30x57) + 5/100 x 57
= 1710 + 162.45
1872.45 cc/24 jam 2000 cc/24 jam
Guillot AP. Fluid and Electrolyte Management Theraphy. University of Vermont Collenge of Medicine
INITIAL TREATMENT
-
7/27/2019 VennDiag Lola (3)
56/72
INITIAL TREATMENT
2. Her past temperature, fever 38c. Now, the temperature was 39,6 C
The theraphy was Antipyretic (Paracetamol 500 mg 3 tab)
3. She felt nausea but no vomit
Antinausea (Domperidone 10 mg 2tab)
4. She felt her weight had some loss but never been scaled
Education for eat more food, but no stimulated the stomach like spicy food
-
7/27/2019 VennDiag Lola (3)
57/72
STEP VENNDIAG
Step 3 : Make a Brief Literature Review of Each Disease
Step 4 : Scan on Patients Sign & Symptoms
STEP 5 : Make a Working Diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
FURTHER INVESTIGATION
-
7/27/2019 VennDiag Lola (3)
58/72
FURTHER INVESTIGATION
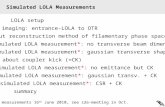
HEMATOLOGY
Hemoglobine 13 18 g% 14.4
Leukocyte 4 11 103 /ul 11.9
Erythrocyte 4.5 - 6.5 106 /ul 5.66
Hematocrit 40 54 % 41.0
Platelet 150 450 103 /ul 164
ERYTHROCYTE INDEX
MCV 80 96 fl 82.4
MCH 27 32 pg 27.4
MCHC 32 36 g/dl 35.1
RDW-CV 11.6 - 14.8 % 13.6
Kidney Function
Ureum 10 50 mg/dl 25
Creatinine 0.7 - 1.2 mg/dl 0.84
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. AeruginosaProtozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.
Inflammato
ry Bowel
Disease
Acute
Bloody
Possible : 1,2,3,4,5, 6
Exclude : 7,8
HEMATOLOGYA t
-
7/27/2019 VennDiag Lola (3)
59/72
O OG
Eosinophil 1-6 % 0
Basophil 1-2 % 0.1
Neutrophil 40-80 % 88,9
Lymphocyte 20-40 % 6.3
Monocyte 2-10 % 4.7
LED 1 jam 10 -15 mm/jam 90
LED 2 jam 10 - 15 mm/jam 107
Liver Function Test
SGOT 0-38 U/l 13
SGPT 0-41 U/l 13.9
Renal Function Test
Asam Urat 3.4-7 U/l 5.6
Diabetes
Glukosa 70 - 110 mg/dl 285
HbA1c
-
7/27/2019 VennDiag Lola (3)
60/72
Electrolyte
Natrium 136 145 % 130
Kalium 3.3 - 5.1 % 3.0
Chlorida 98-106 g/dl 99
Fat
LDL < 150 g/dl 65
HDL > 40 g/dl 15
TG < 150 g/dl 197
Bacterial
1.Shigella
2.Campylobacter.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.Inflammato
ry Bowel
Disease
AcuteBloody
Hypertrygliserida
M i
-
7/27/2019 VennDiag Lola (3)
61/72
STOOL TEST
Macroscopic
Consistency liquid
Color brown
Mucus +
Blood 0
Pus 0
Worm 0
Microscopic
Leucocytes 20 - 25Erytrocytes 10 - 15
Worm eggs 0
Amoeba Cyst +
Other parasites 0
Bacterial
1.Shigella
2.Campylobacter
.3.Salmonella
4. Escherchia coli
5. Aeruginosa
Protozoa
6.Entamoeba
hystoliytica
Acute
Diarrhea
7. NSAIDs
8.
Inflammato
ry Bowel
Disease
Acute
Bloody
Possible : 6
-
7/27/2019 VennDiag Lola (3)
62/72
STEP VENNDIAG
STEP 5 : Make a working diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
STEP 8 : Make a Definitive Diagnosis
STEP 9 : Define the Causative Treatment
STEP 10 : Show Clinical Course of the Disease
-
7/27/2019 VennDiag Lola (3)
63/72
DEFINITE DIAGNOSIS
Definite Diagnosis : Acute gastroenteritis ec amoeba)
(amoeba cyst +)
Milld dehydration
Diabetes mellitus type 2
Excluded:
Acute Gastroenteritis et causa Shigella
Acute Gastroenteritis et causa Campylobacter
Acute Gastroenteritis et causa Salmonella
Acute Gastroenteritis et causa Escherchia coli
-
7/27/2019 VennDiag Lola (3)
64/72
STEP VENNDIAG
STEP 5 : Make a working diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
STEP 8 : Make a Definitive Diagnosis
STEP 9 : Define the Causative Treatment
STEP 10 : Show Clinical Course of the Disease
Fluid therapy (IVFD asering 2000ml/24hr)
-
7/27/2019 VennDiag Lola (3)
65/72
DEFINE THE CAUSATIVE TREATMENT
Fluid therapy (IVFD asering 2000ml/24hr)
Antipyretic (Paracetamol 500 mg 3 tab)
Antispasmodic (Buscopan 10 mg 1 tab)
Antidiarrheal (New Diatabs 2x 600 mg)
Antinausea (Domperidone 10 mg 2tab)
Additional treatment:
Antibiotic for amoeba (Metronidazol 2 x 500mg/day)
Observation for hyperglicemia
Lowering triglicerida : fibrate 1x300 mg tab at night
-
7/27/2019 VennDiag Lola (3)
66/72
STEP VENNDIAG
STEP 5 : Make a working diagnosis
STEP 6 : Define Initial Treatment
Step 7 : Further Investigation
STEP 8 : Make a Definitive Diagnosis
STEP 9 : Define the Causative Treatment
STEP 10 : Show Clinical Course of the Disease
Fluid therapy (IVFD asering 2000ml/24hr)
-
7/27/2019 VennDiag Lola (3)
67/72
DEFINE THE CAUSATIVE TREATMENT
Fluid therapy (IVFD asering 2000ml/24hr)
Antipyretic (Paracetamol 500 mg 3 tab)
Antispasmodic (Buscopan 10 mg 1 tab)
Antidiarrheal (New Diatabs 2x 600 mg)
Antinausea (Domperidone 10 mg 2tab)
Additional treatment:
Antibiotic for amoeba (Metronidazol 2 x 500mg/day)
Lowering blood glucose with insulin drip 3 IU/hour
Lowering triglicerida : fibrate 1x300 mg tab at night
-
7/27/2019 VennDiag Lola (3)
68/72
SHOW CLINICAL COURSE OF THE DISEASE
eat contaminated/raw food
gastroenteritis
mostly recovered
(self limited)dehydration
shockdeath
-
7/27/2019 VennDiag Lola (3)
69/72
SHOW CLINICAL COURSE OF THE DISEASE
Hyperglicemia
Diabetes Mellitus
Complication chronicacuteDiabetic
Ketoacidosis
Hyperglicemic
hyperosmolar
Eye
SkinCardiovascular
Abdominal
Renal
Genitourinary
Neurophathy
Lower extremity
Dhermatologic
Infection
REFERENCES
-
7/27/2019 VennDiag Lola (3)
70/72
1. Ferri, FF. 2006. Ferris Differential Diagnosis : A MedicalGuide to the Differential Diagnosis of Symptoms,Signs, and Clinical Disorders. 2nd eds. Philadelphia :Mosby Elsevier.
2. Fauci, Anthony S. 2009. Harrisons Manual of Medicine.17th eds.
3. Stern, Scott D. C. 2010. Symptom to Diagnosis: AnEvidence Based Guide. 2nd eds.
4. Guillot AP. Fluid and Electrolyte Management Theraphy.University of Vermont Collenge of Medicine
REFERENCES
-
7/27/2019 VennDiag Lola (3)
71/72
VENNDIAGIS....
Metode yang beguna dalam menegakkan diagnosis
karena dari awal kita diajak memikirkan segala
kemungkinan diagnosa yang mungkin terjadi padapasien sehingga menemukan yang paling tepat dan
bisa memberikan terapi yang terbaik bagi pasien.
-
7/27/2019 VennDiag Lola (3)
72/72
SPECIAL THANKS to