The Subserosal Elastic Lamina
-
Upload
gessyca-jey -
Category
Documents
-
view
222 -
download
0
Transcript of The Subserosal Elastic Lamina
-
8/12/2019 The Subserosal Elastic Lamina
1/7
The Subserosal Elastic Lamina: An Anatomic Landmark for Stratifying pT3Colorectal Cancer Eiji Shinto, M.D.,1,2 Hideki Ueno, M.D., 1 Yojiro Hashiguchi, M.D., 1
Kazuo Hase, M.D., 3 Hitoshi Tsuda, M.D., 2 Osamu Matsubara, M.D., 2
Hidetaka Mochizuki, M.D. 11
Department of Surgery 1, National Defense Medical College, Saitama, Japan2 Department of Pathology, National Defense Medical College, Saitama, Japan 3 Department of Surgery, Self Defense Forces Central Hospital, Tokyo, Japan
PURPOSE: Approximately 50 percent of all patients with resected colorectal carcinoma have tumors with pT3 status;however, no subclassifications of the penetration depth have been proposed. The purpose of this study is to evalu-ate the significance of histologic invasion beyond subserosalelastic lamina by colorectal carcinoma for postoperative re-currence and long-term survival after resection. METHODS:pT3 colorectal carcinomas located above the peritoneal re-flection were retrospectively classified into two depth grades (subserosal elastic laminaclassification). Namely,
pT3-shallow is defined as tumors those are confinedabove the subserosal elastic lamina, and pT3-deep is de-fined as tumors those penetrate beyond it. Based on subse-rosal elastic lamina classification, the 325 consecutive pa-tients who underwent resections were divided into twogroups, and then the clinicopathologic features, incidenceof postoperative recurrence, and survival rates were com-pared between the two groups. RESULTS: The overall post-operative recurrence rate in the pT3-deep group (35.2 per-cent) was higher than that in the pT3-shallow group (20.8percent). In detail, liver and peritoneal recurrence rates inthe pT3-deep group (19.7 percent, 7.7 percent, respec-tively) were higher than those in the pT3-shallow group(9.4 percent, 2.0 percent, respectively). There was a strongdifference ( P < 0.0001) in overall survival rate between the
pT3-deep group (5-year survival of 57.0 percent) and the
pT3-shallow group (5-year survival of 78.6 percent). Multi- variate analysis revealed that synchronous hematogenousmetastasis ( P < 0.0001), lymph node metastasis ( P < 0.05), venous invasion ( P < 0.01), and subserosal elastic laminaclassification ( P < 0.05) were the independent prognosticfactors for postoperative survival. CONCLUSIONS: Thenewly proposed subserosal elastic lamina classification is auseful subclassification to predict the prognosis of patients with resected pT3 colorectal carcinomas. [Key words: pT3colorectal carcinoma; Elastic lamina; Subclassification; Prog-nosis]
p T3 colorectal carcinomas, which are defined ascarcinomas that microscopically invade throughmuscularis propria into subserosa or into nonperito-nealized pericolic or perirectal tissues according tothe TNM classification,1 are very frequent among co-lorectal neoplasms. The proportion of pT3 carcino-mas in all operative cases has been reported to rangefrom 35.0 percent to 59.8 percent, and that to ad- vanced cases from 35.6 percent to 67.1 percent. 25 As
for rectal carcinoma alone, a prognostic classificationbased on the extent of cancer spread beyond the mus-cularis propria was reported; 6,7 however, we do nothave a prognostic depth subclassification to accountfor gradations of colorectal pT3 carcinoma. In fact, of patients with resected pT3, pN0, and M0 rectal carci-nomas and colon carcinomas, 20 percent and 13 per-cent, respectively, developed postoperative recur-rence and died. 2 Strict subclassification with positive
Presented at the 101st Annual Congress of the Japan SurgicalSociety, Sendai, Miyagi, Japan, April 11 to 13, 2001.
Correspondence to: Eiji Shinto, M.D., Department of Surgery 1,National Defense Medical College, 3-2 Namiki, Tokorozawa, 359-8513, Saitama, Japan, e-mail: [email protected] Colon Rectum 2004; 47: 467473DOI: 10.1007/s10350-003-0083-9 The American Society of Colon and Rectal SurgeonsPublished online: 4 March 2004
467
-
8/12/2019 The Subserosal Elastic Lamina
2/7
relation to prognosis will be useful to determine whether we perform adjuvant chemotherapy or not.
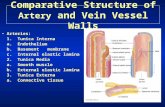
Concerning lung cancer, several researchers haveindicated the prognostic significance of invasion tothe pleural elastic lamina, which is located above the visceral pleura and covers the pulmonary paren-chyma. 8,9 For example, one retrospective study foundpoorer survival in patients with cancer invasion thanin a matched control group in cases of squamous-cellcarcinoma. 9 Therefore, in lung cancer, a categoriza-tion of the primary tumor extension based on thecancerous involvement of the elastic lamina has beenestablished. 10,11 The colon and rectum have an ana-tomic analogy to the lung in that the colorectumabove the peritoneal reflection is also surrounded by a subserosal elastic lamina (SS-EL) located above peri-toneum. 12 Figure 1A shows the normal position of SS-EL. As for this report, we defined the peritoneum
as the external surface made by flattened mesothe-lium, and the subserosa as the layer of connectivetissue between the peritoneum and the muscularispropria, which is equal to an area of pT3. With theprogression of a tumor into the subserosal layer, SS-ELaround the tumor is lifted toward the invasive front of the carcinoma, because of the proliferation of stromaltissue in the region between the peritoneum and SS-EL (Fig. 1B). The aim of this study is to clarify thesignificance of a new depth subclassification on thebasis of the tumor invasion to the SS-EL (SS-EL clas-sification) in a single-institution series.
PATIENTS AND METHODS
Patients and Operations
Between January 1987 and December 1993, 606 pa-
tients underwent surgery for primary carcinoma lo-cated in the colon and rectum above the peritonealreflection at the Department of Surgery I of the Na-tional Defense Medical College Hospital. Of these,325 consecutive patients with pT3 carcinoma wereincluded in this study. Patients with rectal carcinomabelow the peritoneal reflection, which is not anatomi-cally covered by the peritoneum, were not included.Curative operations were performed on 291 patients(89.5 percent), and palliative operations were per-formed on 34 patients (10.5 percent).
In our comparison of survival rates, we also in-
cluded as subjects 39 consecutive pT2 patients withtumor invasion of muscularis propria and 113 con-secutive pT4 patients with tumor penetration into the visceral peritoneum who underwent resection in thesame period and whose tumors were located in thesame area. In the pT2 group, all patients underwentcurative operations, whereas in the pT4 group, cura-tive operations were performed on 69 patients (61.1percent) and palliative operations were performed on44 patients (38.9 percent).
To determine adjuvant therapy, histories of 360 pa-tients (75.5 percent) were examined using medicalrecords. Systemic chemotherapy was administered to2.3 percent (8/342) of patients with curative opera-tions, all of whom had distant metastasis resected atthe primary surgery. Patients who were free of distantmetastasis did not receive systemic chemotherapy inthis period. Of patients with palliative operations, 39percent (7/18) received systemic chemotherapy.None of the patients received chemotherapy or irra-diation therapy preoperatively.
Figure 1. A. Normal position of subserosal elastic lamina(SS-EL) which is located above the peritoneum. B. Pres-ervation of SS-EL (arrows), which shifts toward the mus-cularis propria around the tumor (Victoria-blue hematoxy-lin and eosin stain; x20).
468 SHINTO ET AL Dis Colon Rectum, April 2004
-
8/12/2019 The Subserosal Elastic Lamina
3/7
Follow-up
Patients were regularly followed at our outpatientclinic and were monitored for recurrence by physicalexamination every month; chest X-ray, serum carcino-embryonic antigen (CEA), and carbonhydrate antigen(CA) 19-9 level were monitored every three months;
abdominal ultrasound examination was performedevery 6 months and colonoscopy was done every year. A contrast computed tomography (CT) scan wasperformed when suspicious findings of recurrenceappeared. If patients did not come to our clinic, weresearched their health condition by telephone once a year.
Among patients with pT3 carcinomas, the medianfollow-up of survivors was 65 months (range, 7 to 124months). By the date of the last follow-up, 111 pa-tients had died, with the median time from surgery todeath of 22 months (range, 0.3 to 73 months). Ninety patients died from recurrence of colorectal carci-noma, and 21 died from other reasons or from unclearcauses. In the pT2 group, six patients had died by thedate of the last follow-up, and two of those patientsdied from recurrence. The median follow-up of sur- vivors was 71 months. In the pT4 group, 81 patients were dead, 70 of whom had died from recurrence.The median follow-up of survivors was 89 months. Inthis study we used overall survival as the measure of survival.
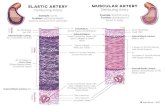
SS-EL Classification by MicroscopicExamination
Sections in which a tumor had invaded into thesubserosal layer were stained with Victoria-blue he-matoxylin and eosin staining or Elastica van Giesonstaining (EVG), to identify the SS-EL for this study.pT3 carcinomas were retrospectively classified intotwo depth grades according to whether the tumor hadinvaded beyond the SS-EL (pT3-deep) or not (pT3-shallow) (Fig. 2A, B).
Other Clinicopathological ParametersIn addition to the SS-EL classification, the histologic
type, nodal status, grade of lymphatic invasion, and venous invasion were available for analysis. Histo-logic type, nodal status, and grade of lymphatic inva-sion were judged by microscopical examination of sections with hematoxylin and eosin staining.
Using sections stained by EVG or Victoria-blue he-matoxylin and eosin stain, we evaluated the grade of
venous invasion according to the number of veins with carcinoma infiltration in the slide where the mostfrequent venous invasions were observed. Subse-quently, the intensity of venous invasion was classi-fied into two grades, as follows: low-grade, 0 4 ve-nous vessels involved by carcinoma cells; high-grade,5 or more vessels involved.
Statistical Analysis
Comparisons between groups were performed with the chi-squared test or Fisher s exact method. We used the unpaired t -test for continuous variables.Survival curves were created with the Kaplan-Meiermethod, 13 and we used a log-rank test for compari-sons. 14 The Cox proportional hazard model was usedfor multivariate analysis. 15 All statistical analyses wereperformed using statistical software (Statview 5, SASInstitute, Cary, NC), and P < 0.05 was considered sta-tistically significant.
Figure 2. Identical lesions of pT3-shallow group and pT3-deep group. A. pT3-shallow: cancer cells do not reachSS-EL (EVG, x40). B. pT3-deep: cancer cells infiltrate be-yond the SS-EL (Victoria-blue hematoxylin and eosinstain; x40).
469SUBCLASSIFICATION FOR pT3 CRC Vol. 47, No. 4
-
8/12/2019 The Subserosal Elastic Lamina
4/7
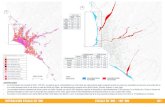
RESULTS
SS-EL Classification and ClinicopathologicFindings
Microscopically, carcinomas met the pT3-deep re-quirement in 171 (52.6 percent) patients (pT3-deepgroup); the others (154 patients, 47.4 percent) wereclassified into pT3-shallow group. In six cases, whichshowed minimum invasion to nonperitonealized peri-colic or perirectal tissues, SS-EL was not found be-cause the shift of SS-EL from the peritonealized area was not sufficient to reach the area adjacent to a tu-mor. We then thought that this type of tumor did notinvade beyond the SS-EL and classified them into thepT3-shallow category. Table 1 shows the compari-sons of clinicopathologic data in these two groups.There were no significant differences in age, sex, tu-mor location, histologic type, or vessel invasions;however, the incidence of lymph node metastasis wasmuch higher ( P < 0.0001) in the pT3deep group (64.3
percent [110/171]) than that in the pT3-shallow group(40.9 percent [63/154]). The rates of synchronous he-matogenous metastasis and peritoneal disseminationin the pT3-deep group (17.5 percent [30/171], 5.8 per-cent [10/171], respectively) were significantly higher( P < 0.01, P < 0.05) than those in the pT3-shallow group (7.1 percent [11/154], 0.6 percent [1/154], re-spectively).
Relation to Postoperative Recurrence(Table 2)
With regard to patients who received curative sur-gery, the overall recurrence rate in the pT3-deepgroup (35.2 percent [50/142]) was higher than that inthe pT3-shallow group (20.8 percent [31/149]). In de-tail, liver and peritoneal recurrence rates in the pT3-deep group (19.7 percent [28/142], 7.7 percent [11/142], respectively) were higher than those in the pT3-shallow group (9.4 percent [14/149], 2.0 percent[3/149], respectively). We avoided statistical analysis
Table 1.Clinicopathologic Features of Patients in pT3-Shallow Group and pT3-Deep Group
pT3-Shallow Group (n = 154) pT3-Deep Group (n = 171) P Value
Age, mean SD (years) 61.2 10.6 61.3 12.2 0.9281Sex
Male 82 104 0.1682Female 72 67
Tumor locationCecum 5 16 0.1210Ascending 25 21Transverse 12 9Descending 11 9Sigmoid 43 60Rectum 58 56
Histologic typeWell, moderately 152 163 0.1088*Poorly, mucinous 2 8
Lymphatic invasionModerate, significant 32 51 0.0619None, mild 122 120
Venous invasionHigh-grade 35 55 0.0577Low-grade 119 116
Nodal statusPositive 62 110 0.0001Negative 91 61
Synchronous hematogenous metastasisPositive 11 30 0.0048Negative 143 141
Synchronous peritoneal disseminationPositive 1 10 0.0116 a
Negative 153 161Curative potential of resection
Curative 149 142 0.0001Palliative 5 29
a Fishers exact test.
470 SHINTO ET AL Dis Colon Rectum, April 2004
-
8/12/2019 The Subserosal Elastic Lamina
5/7
of recurrence rates because follow-up time variedfrom patient to patient.
Relation to Survival
Figures 3 and 4 show the Kaplan-Meier overall sur- vival curves for all patients and for curative cases,respectively. The pT3-deep group (5-year survival of 57.0 percent [95 percent confidence interval, 49.2 64.8] in all patients, 68.1 percent [59.9 76.3] in cura-tive cases) had significantly worse survivals ( P