The effect of vagus nerve stimulation on migraine in patient with intractable epilepsy: case report
Transcript of The effect of vagus nerve stimulation on migraine in patient with intractable epilepsy: case report

LETTER TO THE EDITOR
The effect of vagus nerve stimulation on migraine in patientwith intractable epilepsy: case report
Silvio Basic • Davor Sporis • Darko Chudy •
Gordan Grahovac • Branimir Nevajda
Received: 3 September 2011 / Accepted: 5 June 2012 / Published online: 22 June 2012
� Springer-Verlag 2012
Keywords Epilepsy therapy � Chronic pain � Headaches �Migraine � Vagus nerve stimulation
Abbreviations
VNS Vagus nerve stimulation
EEG Electroencephalography
IED Interictal epileptiform discharges
SPECT Single photon emission computed tomography
EEG Electroencephalography
MRI Magnetic resonance imaging
V-EEG Video EEG
VAS Visual analogue scale
NTS Solitary tract nucleus
LC Locus coeruleus
Dear Editor,
A 42-year-old female had a long history of partial complex
seizures dating from the age of 13. She was treated with the
following anti-epileptic drugs (AEDs): primidone and
phenytoin. In 2003, she had stopped AED treatments vol-
untarily due to ineffective medical therapy, and shortly
after she was admitted again because of convulsive epi-
leptic status. By 2003, she was experiencing six or seven
seizures monthly. Magnetic resonance imaging (MRI)
demonstrated a localized atrophy of the left middle frontal
gyrus with a subcortical area of encephalomalacia.
Electroencephalography (EEG) disclosed left fronto-centro-
temporal interictal epileptiform discharges (IED) with diffuse
paroxysmal dysrhythmic changes and elements of slow spike-
wave complexes. Single photon emission computed tomog-
raphy (SPECT) showed an area of hypoperfusion in the left
frontal area.
In 2008, she experienced ten partial seizures per
month, and by that time, the following AEDs failed for the
patient: primidone, phenytoin, carbamazepine, lamotrigine,
oxcarbazepine, vigabatrin, and gabapentin. She was eval-
uated for 14 days by video EEG (V-EEG) monitoring,
which confirmed that the origin of the seizures was from
the left frontal region.
The patient also experienced typical common migraine
attacks since puberty, with two or three episodes of
migraine attacks per week, which were resistant to acute
treatment. Migraines were characterized by unilateral pul-
sating headaches with photophobia followed by nausea and
vomiting. Scintillating scotoma preceded attacks. These
migraine attacks were not related to the epileptic seizures.
The average intensity of headache on visual analogue scale
(VAS) was eight to nine and the migraine disability
assessment score (MIDAS) was about 50.
In 2008, the patient refused grid electrode placement
and possible neocortical resection.
In 2009, she was offered VNS (NCP; Cyberonics,
Webster, TX, USA) implantation. VNS was implanted in
May, 2009. VNS was turned on seven days after surgery,
and parameters were 0.25 mA, 30 Hz, 500 ls, with an ‘on’
time of 30 s every 5 min. These settings were well toler-
ated by the patient. After this implantation, the patient was
discharged with these AEDs: oxcarbazepine (2,400 mg),
vigabatrin (1,500 mg), and gabapentin (2,400 mg). Six
months after the surgery, the VNS settings were corrected to
1.75 mA, 30 Hz, 500 ls, and ‘on’ time of 30 s every 5 min.
S. Basic � D. Sporis � D. Chudy � G. Grahovac (&) �B. Nevajda
Department of Neurosurgery, Clinical Hospital Dubrava,
Av. Gojka Suska 6, 10000 Zagreb, Croatia
e-mail: [email protected]
123
Neurol Sci (2013) 34:797–798
DOI 10.1007/s10072-012-1135-5

According to the patient’s seizure diary, 18 months after
the surgery, the patient noted a significant decline in the
number and intensity of migraine attacks. She reported a
mean of one migraine attack per month that responded
quickly and effectively to symptomatic treatment. The
average intensity of headache after the surgery was on
VAS 1–2 and MIDAS was 2. The control EEG became free
of IED after the surgery.
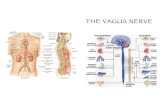
VNS is a well-established method for treating refractory
epilepsy, but the exact mechanism of action of VNS is still
unknown [1]. We can assume that the neuromodulation
potential of the VNS is responsible for restoring normal
brain function not only in brain areas responsible for epi-
lepsy attacks and depression but also in brain regions
responsible for pain that was demonstrated in animal
models.
A retrospective study by Hord et al. [2] showed
improvement of migraine in patients treated with VNS for
intractable epilepsy and concomitant chronic pain.
Migraine attacks showed reduction in both frequency and
intensity which is consistent with our results. The VNS
impact on chronic pain was noticed briefly after VNS
implantation, 1–3 months in the study of Hord et al. We
also noticed an almost immediate effect of VNS to
migraine after the initiation of therapy in our case. A case
report by Sadler et al. [3] also had similar findings as we
have, the number of migraine attacks was significantly
lower after VNS implantation, and yet again VNS effect on
migraine was achieved 2 months after the initiation of
therapy. Although VNS parameters were changed due to
insufficient seizure control, the effect of VNS to migraine
remained constant, as it was in our case also. Mauskop [4]
presented six patients with severe drug-refractory migraine
and chronic cluster headaches. In all of them, VNS was
implanted, and in five of them, there was a dramatic
improvement of their headache. A detailed literature search
revealed several smaller clinical series and case repots such
as ours that VNS can reduce migraine attacks in population
of patients who had VNS device implantation for epilepsy.
[2–5].
Improvement of IED in EEG in our case were compa-
rable with results of study of Wang et al. [6]. They found
that interictal EEG activity was influenced by long-term
VNS, and IEDs in the EEGs progressively decreased with
months of action, which was also observed in our case.
That can explaine mechanism of action of VNS as ‘‘neural
network regulation’’ by desynchronization of abnormal
synchronous epileptic activity.
The result from our case and other small series offers
novel approach in therapy of intractable migraine but fur-
ther randomized trials are necessary to evaluate true
validity of VNS in treatment of intractable migraine.
Conflict of interest The authors have no relevant affiliations or
financial involvement with any organization or entity with a financial
interest in or financial conflict with the subject matter or materials
discussed in the manuscript. This includes employment, consultan-
cies, honoraria, stock ownership or options, expert testimony, grants
or patents received or pending, or royalties. No writing assistance was
utilized in the production of this manuscript.
References
1. Penry JK, Dean JC (1990) Prevention of intractable partial seizures
by intermittent vagal stimulation in humans: preliminary results.
Epilepsia 31(Suppl 2):S40–S43
2. Hord ED, Evans MS, Mueed S, Adamolekun B, Naritoku DK
(2003) The effect of vagus nerve stimulation on migraines. J Pain
4(9):530–534 [pii: S1526590003008095]
3. Sadler RM, Purdy RA, Rahey S (2002) Vagal nerve stimulation
aborts migraine in patient with intractable epilepsy. Cephalalgia
22(6):482–484. doi:10.1046/j.1468-2982.2002.00387.x
4. Mauskop A (2005) Vagus nerve stimulation relieves chronic
refractory migraine and cluster headaches. Cephalalgia 25(2):82–86.
doi:10.1111/j.1468-2982.2005.00611.x
5. Lenaerts ME, Oommen KJ, Couch JR, Skaggs V (2008) Can vagus
nerve stimulation help migraine? Cephalalgia 28(4):392–395. doi:
10.1111/j.1468-2982.2008.01538.x
6. Wang H, Chen X, Lin Z, Shao Z, Sun B, Shen H, Liu L (2009)
Long-term effect of vagus nerve stimulation on interictal epilep-
tiform discharges in refractory epilepsy. J Neurol Sci 284(1–2):
96–102. doi:10.1016/j.jns.2009.04.012
798 Neurol Sci (2013) 34:797–798
123