Talk about COPD - Ready to challenge your COPD? | … can work with your healthcare team to develop...
Transcript of Talk about COPD - Ready to challenge your COPD? | … can work with your healthcare team to develop...
Welcome,Having a lifelong condition like chronic obstructive pulmonary disease (COPD) doesn’t mean you have to stop doing all the things in life that you love.
With some planning and the support of family and friends, it’s possible to work with your healthcare team to manage COPD and reduce its impact on your day-to-day life. That means being aware of what’s causing your symptoms, learning how to manage them – and finding out how to stop them getting worse. It may be that your symptoms are changing and you need your doctor to assess if there is a more effective solution for you.
In short, it’s possible to take charge of COPD and not let it control your life. You can use this planner to help you:• Manage your condition• Track your symptoms• Prepare for your appointments• Record your treatments• Set goals to help you get more out of every day• Identify if a new treatment plan might be needed. We hope you find this Action Planner useful in managing COPD both now and in the future.
Best wishes,Your ‘Talk About COPD’ Team
Section 1
What is COPD?ContentsSection 1:pg 3 What is COPD?pg 5 Managing COPDpg 6 Living with COPDpg 8 Exercise
Section 2:pg 10 Managing your
symptomspg 14 Treating COPD
Section 3:pg 16 Goal setting
Section 4:pg 18 Appointment Tracker
Section 5:pg 20 Symptom Trackerpg 28 Your notes
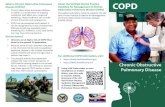
Chronic obstructive pulmonary disease (or COPD) is a lifelong lung condition that makes breathing difficult. It is caused by long-term exposure to irritants that damage the lungs and airways.
key to COPD
HOW LUNGS WORK
Healthy Lung with normal air ways
COPD Effected Lung with reduced airways
COPD damaged alveoli
Inflamed airway blocked by
Mucus
Normal healthy alveoli
Normal healthy airway
2 3
COPD can affect you in many ways: it can be physically debilitating and prevent you doing the things you enjoy. It can also be emotionally draining, creating uncertainty about the future or affecting relationships with family and friends.
However, with the right advice and support, it’s possible to come up with a treatment plan that helps you to manage COPD and reduce its impact on your day-to-day life.
A good COPD treatment plan aims to:
• Assess and monitor the condition • Reduce risk factors• Support medication use• Manage COPD day-to-day • Manage flare-ups when they occur.
Your doctor may have spoken to you about ways to manage COPD.
Managing COPD
Who gets COPD?Smoking is the no.1 cause of COPD. As such, most people with COPD are smokers or ex-smokers.
Breathing in air from other smokers (secondhand smoke), chemical fumes, or dust can also cause COPD.
The symptoms of COPD Symptoms vary from person to person, but can include the following:• A chronic cough
(sometimes called a ‘smoker’s cough’)
• Excess phlegm production• Breathlessness • Wheezing and/or tightness
in the chest.
The more lung damage you have, the more serious your symptoms may be.
Self-managementTreatment for COPD may help to manage symptoms and prevent the condition becoming worse. See page 10 for more advice on managing your symptoms.
Lifestyle plays a big partin COPD. There are somechanges you can make to helpmanage COPD and to reduce the impact it has on your day-to-day life. See page 6 for more information on this.
COPD FACTSI
This Action Planner can not only help you to follow your treatment plan, but it can also help you to monitor it, to ensure it remains the best management plan for you.
COPD can have a serious impact on your day-to-day quality of life if it is not appropriately treated. Other names for COPDCOPD is an umbrella term to describe a group of conditions, including chronic bronchitis and emphysema. You may also hear COPD called chronic obstructive airway disease or chronic obstructive lung disease.
4 5
• Eat high-fibre foods like vegetables and whole grains
• Do not eat a lot of salt, use herbs instead
• Stay away from foods that cause gas or bloating (soda or fried foods).
For people with COPD, it is important not to be overweight or underweight. Ask your doctor what your goal weight should be and work with him or her to come up with a diet and exercise plan to get there!
Making gains with your healthCOPD is a very common lung disease. Quitting smoking, exercising, and eating healthy are key to reducing and managing the symptoms of COPD. This section will help you learn about living a healthy life and to gain a better understanding of the benefits of:• A healthy diet• Exercise
Tips on eating and energyEating a healthy diet is important for everyone, especially if you have COPD. Your body needs fuel in the form of food for activities like breathing. If you have COPD, your body needs more energy to breathe. There are many things you can do to get the right nutrients while maintaining a healthy weight:• Drink a lot of water
and avoid alcohol and caffeinated drinks
Living with COPD
If you feel like your COPD is progressing, or the symptoms are affecting you more than they should, speak to your doctor to see if a change in your treatment plan is necessary.
Quitting smoking, exercising, and eating healthily are key to reducing and managing the symptoms of COPD.
Tell your doctor
6 7
• Stand up from a sitting position using the arm rests for support only
• Stand with hand weights or water bottles
• Stand with your arms up at shoulder height and elbows bent
Exercise: What’s in it for me?A common symptom of COPD is breathlessness. Breathlessness is feeling short of breath or having trouble breathing. It may feel uncomfortable, but you should not be less active because of it. As part of your COPD treatment plan, your doctor may suggest you start exercising.
Regular exercise has many benefits and can:• Reduce breathlessness• Reduce hospital stays• Lower blood pressure• Reduce anxiety and
depression• Lower rates of
infection• Improve circulation• Increase your energy
for daily tasks• Strengthen your heart
and muscles• Improve sleep• Help you lose weight.
All kinds of exercise are good for people with COPD. By exercising frequently, you could hope to see improvements in your COPD symptoms including breathlessness and fatigue
Exerciseand find exercising easier than before. It’s important to choose an exercise you enjoy. Take a walk with your dog, do some gardening, or dance to your favourite music. The less exercising feels like work, the more you’ll want to do it.
Tips for Safe Exercise1. Please consult
your healthcare professional before starting any new exercise regime
2. Do not exercise if you feel unwell
3. Drink plenty of water during the day
4. 500ml bottles of water are ideal hand weights
5. You should always be able to talk whilst exercising
6. Stop if you become too breathless or feel unwell
Work with your doctor to choose a type of exercise that you’ll enjoy.
EXERCISE NO. 1 Sit to Stand
• Raise your arms up and down to shoulder height
• Raise your arms up and down to shoulder height
• Hold a hand weight or bottle of water in each hand
• March on the spot at the same time• Repeat as many times as is comfortable
• March on the spot at the same time• Repeat as many times as is comfortable
• Pull your elbows back and squeeze shoulder blades as if you are squeezing something between them
• Release your arms and repeat
EXERCISE NO. 2Shoulder Raises
EXERCISE NO. 3Chest and Shoulder Exercises
8 9
You can work with your healthcare team to develop techniques that can help you better identify individual symptoms as they arise.
Here are some suggestions.
1 Managing breathlessnessBreathlessness is normal
for most people at some stage – for example when they’ve been doing strenuous exercise.
Section 2
Managing your symptoms Breathing control techniques These are usually taught as part of pulmonary rehabilitation (above) but they can also be learnt on their own.Learning how to better control your breathing can help reduce breathlessness, but it can also help you to breath easier day-to-day.
What else can help with breathlessness?• Maintain a healthy
weight • Make day-to-day
activities achievable and try not to over-do things (try setting a goal for this – see page 16)
• Try and save energy when you’re not active
• Take time out when you’re breathless and start the activity again after you’ve had a rest
• Ask for help when you need it
• Follow your treatment plan as directed by your doctor and revise the plan regularly, but in particular when you start to feel your COPD symptom is not well controlled.
Your doctor will have more advice and ideas. Don’t forget to record any breathlessness on your Symptom Tracker (see page 22) to help your doctor better understand how it’s affecting you.
Learning about COPD and understanding how it affects your lungs can help you to better control and manage the condition.
However the breathlessness caused by COPD can be more regular and become a problem even when doing ‘normal’ everyday activities such as climbing stairs or walking to the bus stop.
Ways to manage breathlessness:Pulmonary rehabilitation is one of the best ways to reduce your breathlessness.
It’s a wide-ranging programme that can help with:• Exercise training• dietary advice• Advice and information
about COPD and how to manage it
• breathing techniques • Energy-saving
techniques• counselling and group
support.
ALTER YOUR POSITION
Some positions make it easier to breathe than others. Why not try these positions and see what works for you?
You may also find a walking stick can lend extra support when you’re out and about.
Pursed Lip BreathingThis technique will help you if you feel breathless
1 Breathe in through your nose
2 Breathe out through pursed lips like you are blowing out a candle. Ensure that your breath out is twice as long as your breath in• Relax and repeat
until you feel less breathless
Relaxed BreathingA breathing technique that will help you relax. This iscalled tummy breathing or diaphragmatic breathing.
1 Sit and relax your shoulders and chest• If it feels
comfortable, put one hand on your tummy, just above your belly button
2 Breathe gently in and out through your nose at rest• Your tummy should
rise as you breathe in and fall as you breathe out
10 11
2 Managing coughing and phlegm
Coughing is your body’s way of trying to remove mucus from your airways, and of protecting the airways from irritants. Speak to your doctor about ways to better manage coughing. They may suggest over-the-counter remedies like throat lozenges and cough syrups, or prescribe a suppressant.
Section 2
Managing your symptoms
What else can you do?• Drink lots of fluids to try
and help thin the mucus. • You can also try
techniques such as distraction to help you relax and take your mind off the coughing.
• Minimise irritants – in particular stop smoking and avoid second-hand cigarette smoke.
Always let your doctor know when your symptoms suddenly get worse so you can get the right treatment
Daily Breathing Exercises to Clear Your ChestRepeat until your chest is clear and you no longer hear the “rattle” of phlegm. Stop if you feel tired or your chest begins to feel tight or wheezy and return to them later when you feel better.
The Active Cycle of BreathingTechnique is a breathing exercise used daily in COPD to loosen and clear any phlegm you may have and it is gentler than just coughing. Phlegm in the lungs can lead to chest infections.
It is a good routine to clear your chest with these exercises every morning and evening increasing this every 1 or 2 hours when you are feeling unwell, and have lots of phlegm.
AM I HAVING AN EXACERBATION?
Some people with COPD may experience episodes where symptoms get much worse. These episodes are called exacerbations. The signs and symptoms of an exacerbation may include:
• Increased breathlessness• Increased coughing• Increased mucus• Change in mucus colour• Wheezing• Chest tightness• Fever.
Exacerbations are usually caused by an infection or inhaling some pollution. But sometimes the cause is not found. Being able to recognize an exacerbation is important. Treating them early is the key to a successful recovery. Having a plan for what to do in case of an exacerbation is very helpful. Work with your doctor to make an action plan that is right for you.
1 Tummy BreathingRelaxed breathing (or tummy breathing)• Sit comfortably and
relax your shoulder and neck
2 Three Deep BreathsThree deep breaths (to the bottom of lungs) and hold each breath for a count of 3• Repeat until your
chest is clear
3 HuffingHuffing followed by cough if needed to remove phlegm.
Huffing:• Take a medium
breath in, then breathe out through a very open mouth (as if fogging up a mirror to clean it)
• You can do this 2 or 3 times until the “rattle” of phlegm is gone.
12 13
Stick, don’t skipSticking to your prescribed treatment is an important part of treating COPD symptoms, along with diet, exercise and not smoking. Skipping treatments may make breathing difficult, cause more hospitalisations, and worsen your overall health.If you’re having problems with taking COPD treatment or using an inhaler correctly, talk to your doctor immediately, who may be able to help.
How can COPD be treated?There are different inhalers used to treat COPD. Your doctor will prescribe the treatment they feel is right for you, based on your symptoms. • Short-acting bronchodilators
These are the most commonly prescribed inhalers and help make breathing easier by opening up your airwaves. They can be taken regularly, throughout the day, as
Treating COPD
There are many things you can do to open up your airways, including exercising, eating healthy, and taking your medication as prescribed.
prescribed to prevent or reduce symptoms.
• Long-acting bronchodilators These are prescribed for treating COPD over a longer period of time in people who experience regular symptoms. They can be used once or twice per day.
• Corticosteroids (steroid) inhalersYour doctor may suggest combining long-acting bronchodilators with a steroid inhaler; these help to treat COPD flare-ups by reducing lung inflammation.
• Methylxanthines
For more severe cases of COPD, methylxanthines may be prescribed. They tend to be effective when taken in large doses, however they have very strong side effects.
Always speak with your doctor to ensure the treatment you are taking is right for you.
Use your Symptom Tracker to record how often you experience symptoms and what effect they
have on your daily life. See page 20
14 15
It’s a good idea to write your goals down, along with an outline of how you hope to achieve them. That way you can stay focused and have something to aim for.
To give yourself the best chance of success, make your goals SMART. That means they should be:
My goal When do I want to do it?
Steps I’m going to take to achieve it
When do I want to review this goal?
To record my symptoms.
Every Saturday morning after breakfast.
i) Put a note on the fridge to remind me ii) Set an alarm on my phone iii) Write down signs and symptoms as they occur through the week, so I can review and collate them each Saturday.
I’ll take my completed Tracker to my next appointment with my doctor.
To make exercise part of my daily routine
I will walk to the shops around the corner from my house
i) Put a note on the fridge to remind meii) Walk at the same time each dayiii) Walk somewhere inside if it’s raining
On the weekend I will look back at how many times I went for a short walk that previous week
Goal setting
Setting a goal can be a great way to help you achieve something that’s important to you.
SSpecific: Ensure there is enough detail to determine whether the goal has been achieved.
MMeasureable: Make sure you can judge whether you have achieved it or not.
AAchievable: Try to be realistic about what you can achieve – this can help you avoid feeling frustrated and disheartened.
RRelevant: Make sure your goal is relevant and important to you.
TTimely: Set a time by which would like to completed the goal.
Why not start setting some goals today to help you better manage COPD? You can record these on page 17.
Section 3
16 17
Section 4
Your healthcare team is there to help you make the most of your treatment and to manage COPD as well as possible.
Here are some ways you can make the most of your time:
% Always be honest and open so they can provide the best support for you.
% Prepare well for appointments by writing down any questions you have, so you don’t forget them.
% Take notes so you have a record of key points that were discussed.
% Ask your doctor to repeat anything you don’t understand.
% Take your time – don’t feel rushed; you can always ask for another appointment if you run out of time.
% Share the results of your Symptom Tracker (see page 20) with your doctor so they can better understand how you’ve been feeling.
% Report any worsening of symptoms to your doctor so your treatment plan can be reviewed.
% Take a friend or family member with you – two sets of ears are better than one.
Appointment Tracker Date Time Doctor’s name and address
Things I need to discuss
My notes from appointment
Things I need to follow up
You can use page 19 to record your appointments and to make notes to discuss with your doctor.
18 19
Section 5
Use the following pages to track some of the key symptoms of COPD, and how much impact they are having on your life.
You can then share the results with your doctor to help explain your symptoms, and describe what effect they’re having on your day-to-day life. This can help your healthcare team better understand the impact of COPD on your life and, if necessary, recommend any changes to your treatment plan.
Speak to your doctor if you notice a worsening of your symptoms between appointments, or if you’re having trouble managing them.
Symptom Tracker
On the following pages, rate how each symptom has affected your that week.
Symptom Tracker - WEEK1 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
4 DAY-TO-DAY ACTIVIITES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
18
27 6 17
Cough got better this week.
SAMPLE
Take the rating from above, and map it on the chart - this will help you to see if the symptom is progressing for you.SAMPLE
109876543210
Week 1 2 3 4 5 6
Coughing and phlegm
Scor
e
109876543210
Week 1 2 3 4 5 6
Breathlessness
Scor
e
109876543210
Week 1 2 3 4 5 6
Day-to-day activities
Scor
e
109876543210
Week 1 2 3 4 5 6
Coughing and phlegm
Scor
e
20 21
Symptom Tracker - WEEK2 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
Symptom Tracker - WEEK1 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
22 23
Symptom Tracker - WEEK4 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
Symptom Tracker - WEEK3 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
24 25
Symptom Tracker - WEEK6 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
Symptom Tracker - WEEK5 DATE: / /
1 COUGHING & PHLEGMThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
2 BREATHLESSNESSThinking about the past week, to what degree did you experience this symptom?Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
3 DAY-TO-DAY ACTIVITIES Thinking about the past week, to what degree did COPD affect this? Not at all Very severely0 1 2 3 4 5 6 7 8 9 10Comments:
26 27