SYNCOPE Nora Goldschlager, M.D.
description
Transcript of SYNCOPE Nora Goldschlager, M.D.

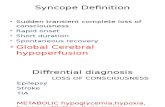
SYNCOPE
Nora Goldschlager, M.D.MACP, FACC, FAHA, FHRS
Cardiology – San Francisco General HospitalUCSF
Disclosures: None

SCOPE OF THE PROBLEM
•Cumulative lifetime incidence in general population up to 35%
•1% of all hospital admissions•3% of all ER visits; up to 65% are vasovagal•6% incidence in institutionalized elderly•Prevalence: 7 - 47% in young, healthy
subjects; unknown in elderly•Up to 30% of patients may have no
diagnosis established at hospital discharge
•6% annual mortality if no cause established•12 - 25% recurrence

Kapoor Medicine 69:1990 N = 433 Sudden death: 37%
Mo
rtal
ity
%
50
40
30
20
10
0
Cardiac
Noncardiac
Unknown
Yr. of FU: 0 1 2 3 4 5No. at risk: 433 380 349 295 179 44

SURVIVAL IN SYNCOPAL PATIENTS
Follow-up (yr)Soteriades et al NEJM 2002;347:878 (Framingham) N = 822/7814
0 5 10 15 20 25
Pro
bab
ility
of
surv
ival 1.0
.8
.6
.4
.2
0
No syncope
Vasovagal & other causes (OH, med Rx)
Unknown cause
Neurologic cause
Cardiac cause

PREVALENCE OF SYNCOPE BY AGE
50
40
30
20
10
0
Ganzeboom et al AJC 4.15.03
Pre
vale
nce
(%
)
Age (yrs)
MalesFemales
0 7 14 21

YOUNGER ADULTS ELDERLY
15% 15%
40%30%30% 25%
15%30%
Vasovagal
Undetermined
Cardiogenic
Other causes
OH, situational,seizures, drugs
1° arrhythmia
OH, CSS, situational, seizures, drugs
1° arrhythmia,LV obstruction

ETIOLOGY OF FIRST SYNCOPEIN PATIENTS > 65 YEARS
%• Reflex-mediated
(VVS, CSS, situational) 13-30%• Orthostatic 12• Cardiac
Arrhythmic 8Nonarrhythmic 3
• Drug-induced 8• CNS 6• Unexplained 49
Roussanov et al, Am J Geriatric Cardiol 2007;16:249 N=304 (VA patients)

FEATURES OF UNEXPLAINEDSYNCOPE IN OLDER PATIENTS
• High incidence of comorbid conditions• 24% recurrence rate• Concurrent BP and HF Rx increases
susceptibility to + HUT• Only 9% had an etiology established
during follow-up• Lower diagnostic yield of history and
tests compared in younger patients
Roussanov et al, Am J Geriatric Cardiol 2007;16:249 N=304 (VA patients)

PROGNOSIS IN UNEXPLAINED SYNCOPEIN PATIENTS > 65
Pro
po
rtio
n o
f p
ts a
live
1.0
.75
.50
.25
00 1 2 3
Yrs FU
Roussanov et al Am J Geriatric Cardiol 2007; 16:249 N = 304 VA pts
Control
Syncope

EVALUATION OF SYNCOPE: PERTINENT HISTORY
• Precipitating factors- Posture changes (orthostatic hypotension)- Cough, swallowing, micturition, defecation
(“situational” syncope)- Exercise (consider aortic stenosis, HOCM, VT)- Head turning, Valsalva (suggests carotid
sinus syndrome)• Prodromal symptoms• Speed of onset and recovery (prolonged
recovery suggests vasovagal syncope)• Aura (suggests seizure)• Hx heart disease (predicts cardiac syncope:
95% specificity <50%>)

NATURAL HISTORY OF AORTIC STENOSIS%
Su
rviv
al
100
75
50
25
0
Onset of SxWith AVR
Without AVR
Asx stage
CHFAnginaSyncope
10 20 30Years

EVALUATION OF SYNCOPE: PERTINENT HISTORY• Drugs
- Diuretics ( hypokalemia, hypomagnesemia)- Digitalis (AVB, VT-classically bidirectional)- Antihypertensives- Antiarrhythmic agents (proarrhythmia)- Ophthalmic -blockers- Antianginal medications (preload and afterload reduction)- QT prolonging drugs (www.torsades.org)- OTC drugs- Herbs- Illicit drugs, alcohol- β-blockers
• Family history of sudden death (congenital long QT syndrome, hypertrophic obstructive cardiomyopathy)
• Known rhythm abnormality (e.g., WPW)

Exercise-induced RVOT VT

Tussive bradycardia


Deglutition bradycardiaContinuous strips

CONGENITAL LQTS
• 1:10,000 is a gene carrier• 3-4,000 sudden deaths/yr, mostly young
patients• 10% sudden deaths in untreated patients• 30% of sudden or aborted sudden deaths
occur as 1st event• Female gender• About 10% have normal QTC; about 30%
have borderline QTC


CLUES TO ETIOLOGY OF SYNCOPE FROM PHYSICAL EXAMINATION
• Left ventricular impulse abnormalities suggesting past myocardial infarction
• Ventricular hypertrophy (need for AV synchrony)
• Ventricular gallops• Murmurs (aortic stenosis, hypertrophic
obstructive cardiomyopathy)• Pulmonary hypertension• Mitral valve prolapse
(PSVT, VT, autonomic dysfunction)• Carotid sinus massage indicating CSH

• Generally accepted contraindications - Carotid bruits- Prior endarterectomy- Prior TIA or CVA- Known cerebrovascular disease
• Responses to CSM- Bradycardia / asystole usually abrupt- Hypotension often not abrupt, and
outlasts the CSM- Complications (< 1%): TIA, transient
paresis, visual disturbances
CAROTID SINUS MASSAGE

CLUES TO ETIOLOGY OF SYNCOPE FROM 12-LEAD ECG
• Long QT interval• Prior MI (substrate for VT)• Epsilon wave, anterior (V1-3) T inversion, QRS
duration V1-3 / V4-6 > 1.2, suggesting RV dysplasia
• Brugada pattern• Short QT interval (with tall symmetric T waves)• Ectopy• Bradycardia• AV conduction delay / block• Bifascicular block• Ventricular hypertrophy (need for AV synchrony)

Epsilon wave of RV dysplasia
Marcus, Fontaine PACE 6.95
V1
V2
V3

RV DYSPLASIA
• Young pt• Can present as syncope or aborted
sudden death• ECG:
- Anterior T inversion V1-3
- Prominent anterior forces- RIVCD
- Delayed S wave V1-2
• MRI is usually (but not always) diagnostic (fat replacement)

RV dysplasia


BRUGADA SYNDROME

BRUGADA SYNDROME

OUTCOME IN PTS WITH BRUGADA ECGF
ree
of
even
ts(S
D, V
F)
1.0
.8
.6
.4
.2
0
Brugada et al Circulation 2002; 105:73 N = 334, all EPS 63% of syncopal pts had VT induced
Asymptomatic (57%)
Syncope (22%)
Sudden death (21%)
p = 0.00001
0 100 200 300Mos

Follow-up (mos)
Antzelevitch et al Circulation 2005; 111:659 N=258 (Registry)
PROGNOSIS OF SYNCOPE IN BRUGADA SYNDROME
Fre
e o
f A
pp
rop
ria
te IC
D R
x
1.0
.8
.6
.4
.2
0
Asymptomatic
Syncope
Sudden death
0 12 24 36 48 60

ROLE OF ECHOCARDIOGRAPHY IN SYNCOPE
• Aortic stenosis• Hypertrophic cardiomyopathy
(especially obstructive)• Regional wall-motion disorders
(substrate for VT)• Right ventricular dysplasia• Calcified mitral / aortic annulus
( AV block incidence)• Intracardiac tumor• Mitral valve prolapse• Repaired congenital heart disease• Normal echo

NONARRHYTHMIC CARDIAC SYNCOPE:OBSTRUCTION TO FLOW
• Aortic stenosis- LV baroceptor stimulation with
reflex peripheral vasodilation- Ventricular arrhythmias- Transmural ischemic injury with
LV dysfunction
• Hypertrophic obstructive cardiomyopathy• Tumor• Primary pulmonary hypertension, pulmonic stenosis• Pulmonary embolism

Syncope in aortic stenosisRecorded during syncopal spell. BP unobtainable.

Syncope in aortic stenosisLead III: During syncopal spell

SYNCOPE IN HYPERTROPHIC CARDIOMYOPATHY - 1
• Causes - SVT (especially AF)- VT- LV outflow tract gradient- Abnormal baroreceptor reflexes- Ischemia
• EP studies unreliable• -blockers, disopyramide and Ca++ channel
blockers do not reduce incidence of SD

SYNCOPE IN HYPERTROPHIC CARDIOMYOPATHY - 2
• ICD indicated for high risk patients
- Family hx syncope/sudden death- LVH > 3 cm- Aborted sudden death- Nonsustained VT on Holter

SYNCOPE IN PULMONARYHYPERTENSION
• Usually exertional or immediately post-exercise• “Fixed” right sided obstruction due to
high pulmonary vascular resistance• Inability to increase CO in response to SVR • Decreased cerebral perfusion

SYNCOPE IN SYSTOLIC HEART FAILURE• In patients with syncope, heart failure is
an independent predictor of mortality• Syncopal patients with ICDs have
appropriate therapies delivered • SCD-HeFT:
- Predictors of syncope: QRSd > 120 ms, NYHA III, no beta blocker
- Not predictors: EF, NSVT, AF, other HF Rx- 16% with ICD had syncope; 41% had
appropriate shock (vs 12% with no syncope)- Syncope was predictor of total and CV
mortality, but not sudden death and did not differ among ICD, amio, or placebo pts
- ICDs did not reduce mortality in syncope patients

NEUROCARDIOGENIC (VASOVAGAL) SYNCOPE
• Occurs at all ages• 17 - 35% suffer significant injury• 5 - 7% have fractures• Up to 4% of pts diagnosed with
VVS may have cardiac syncope

FEATURES OF HISTORY IN VVS
• Usually occurs in upright position• Rare during exercise• 3 phases: prodrome, loss of consciousness, postsyncopal period• May have specific triggers:
pain, trauma, stress, “situational” (swallow, micturition, defecation)
• Peri-event amnesia common• Association with chronic fatigue syndrome,
depression, somatic disorders• May run in families• frequency around menses

Male < .001
Age > 54 < .001
Supine NS
Upright NS
Precipitant < .001
No presyncope NS
Warning NS
Diaphoresis < .001
VASOVAGAL vs ARRHYTHMIC* SYNCOPE
*VT + AVBCalkins et alAJM 98:1995
0 20 40 60 80 100
P
VV (%) Arrhythmic (%)

VASOVAGAL vs ARRHYTHMIC* SYNCOPE
Fatigue Post < .001
Confusion NS
Palpitations NS
Incontinence .02
Injury NS
Major Injury NS
Recovery > 0” < .001
0 20 40 60 80 100
P
VV (%) Arrhythmic (%)*VT + AVBCalkins et alAJM 98:1995

NEUROCARDIOGENIC SYNCOPE LV
volume
Venous return
Peripheral venous pooling
HEADUPTILT
Peripheral vasodilation
Hypotension
adrenergic tone
LV contractility
Mechanoreceptor stimulation
(myocardial C fibers)
Vasomotorcenter
Vagal tone
Bradycardia or asytole

* Watch for urinary retention, torsades de pointes VT
VVS: PHARMACOLOGIC THERAPY• Anticholinergic agents
- Disopyramide* (effect vs placebo is controversial)
- Scopolamine• Negative inotropic agents
- Disopyramide*• Fludrocortisone• Vasopressin
• Alpha-adrenergic agonists
- Ephedrine- Etilephrine- Theophylline- Dexedrine- Midodrine
• Serotonin reuptake inhibitors

VVS: PACEMAKER THERAPY
Effect vs placebo is controversial and not supported in RCTs
- Dual chamber
- Rate-drop response or other algorithm which detects heart rate, then tachypaces while periodically searching for spontaneous rhythm

VVS: PACING vs -BLOCKADE (SYDIT)%
syn
cop
e fr
ee p
ts 1.0
0.9
0.8
0.7
0.6
Ammirati et al Circulation 2001; 104:52 N = 93
0 200 400 600 800 1000 Days
Pacemaker
Atenolol
P = 0.0031

“ORTHOSTATIC TRAINING” FOR REFRACTORY NEUROCARDIOGENIC
SYNCOPE
N = 47, mean age 165 in hospital training sessions40 min BID standing against wall at home
Results: (FU 18 ± 5 mos)96% had – HUT (Control 26%)
0% had syncope (Control 57%)
Girolamo et al Circulation 1999;100:1798

LEG CROSSING AND MUSCLE TENSING TO ABORT / MITIGATE VASOVAGAL SYNCOPE•N = 21•At onset of sx, leg crossing with tensing of
abdominal, leg and buttock muscles•BP and HR stabilized in all pts in 3 - 6"•5 / 20 aborted syncope •15 / 20 had delayed onset of syncope
by 0.5 - 11'•At 10 mo FU, 16 / 19 benefited from maneuver•Similar benefit for cardiac pacing
Krediet at al, Circulation 2002;106:1684


ISOMETRIC ARM EXERCISE TO ABORT VASOVAGAL SYNCOPEControl 2 min handgrip
Brignole et al JACC 2002;40:2053 N = 19
Asx 11%Syncope 47%
Asx 63%Syncope 5%
HR112906845
BP178156133111896744

FALLS: SCOPE OF THE PROBLEM
•30% of pts > 65 fall / yr•60% of pts in long-term care facilities fall / yr•10 - 20% result in injury•2 - 6% result in fractures•Usually unwitnessed•30% have LOC with CSM; 80% had amnesia
Kenny et al SAFEPACE JACC 2001;38 N = 175

SAFE-PACE TRIAL**Syncope and Falls in the Elderly
Pacing and Carotid Sinus Evaluation
•Prospective randomized, controlled trial of 175 patients > 50 y.o. with cardioinhibitory carotid sinus hypersensitivity and unexplained falls•Randomized to pacing (with rate-drop response) vs. no pacing•Follow-up one year•Odds-ratio of falls in nonpaced patients 4:1, 0. 35 in paced patients
Kenny et al JACC 2001;38

DDD PACING FOR CAROTID SINUS SYNDROME WITH FALLS, DIZZINESS AND SYNCOPE
Crilley et al Postgrad Med J 73:1997 N = 42
100
80
60
40
20
0Syncope Falls Dizziness
Before After

SYNCOPE WORKUP
• ECG• Holter (overall yield 2-35%)• Event Monitor (patient cannot be syncopal)• Head-up tilt table testing• Electrophysiologic study
(predictive value variable)• Implantable loop recorder

TILT-TABLE TESTING FOR EVALUATION OF SYNCOPE:
SUMMARY OF PRINCIPAL INDICATIONS
Tilt-table testing warranted
• Recurrent syncope or single syncopal episode in a high risk patient, whether or not the medical history is suggestive of
neurally mediated (vasovagal) origin and:
1. No evidence of structural cardiovascular disease, or
2. Structural cardiovascular disease is present, but other causes of syncope have been excluded by appropriate testing
Benditt et al JACC July 1996

Tilt-table testing warranted
• Further evaluation of patients in whom an apparent cause has been established (e.g., asystole, atrioventricular block), but in whom demonstration of susceptibility to neurally mediated syncope would affect treatment plans
• Part of the evaluation of exercise-induced or exercise-associated syncope

Reasonable differences of opinion exist regarding utility of tilt-table testing
• Differentiating convulsive syncope from seizures
• Evaluating patients (especially the elderly) with recurrent unexplained falls
• Assessing recurrent dizziness or presyncope• Evaluating unexplained syncope in the
setting of peripheral neuropathies or dysautonomias
• Follow-up evaluation to assess therapy of neurally mediated syncope

Tilt-table testing not warranted
• Single syncopal episode, without injury and not in a high risk setting, with clear-cut vasovagal features
• Syncope in which an alternative specific cause has been established and in which additional demonstration of a neurally mediated susceptibility would not alter Rx

DIAGNOSTIC YIELD OF AMBULATORY ELECTROCARDIOGRAPHIC MONITORING
(AECG) IN SYMPTOMATIC PATIENTS Sx w/o AECG No Sx with AECG
arrhythmia (%) arrhythmia (%) No. + – + –Zeldis 37 13 34 30 23Clark 98 3 39 41 17Jonas 358 4 0 16 80Kala 108 7 7 16 69Gibson 1,512 2 15 10 79Boudoulas 119 26 13 27 34Diamond 85 44 20 4 33
TOTAL 2,651 21 48Overall yield 2%
DiMarco and Philbrick, Ann Intern Med 6/90




PATIENT PRESENTING WITH SYNCOPE AND SEIZURE

ADVANTAGES AND LIMITATIONS OF IMPLANTABLE LOOP RECORDERS
Advantages
• Prolonged ECG recording capability (to 2 yrs)• Memory - allows activation after syncopal event• Automatic recording, allowing automatic
acquisition of ECG events which fall outside programmable boundaries
• Elimination of technical factors which impair good quality surface ECG recording during sx
• High sx-ECG correlation yield: Dx made in 25-50% of pts, and suggested in an additional 15-25%
Benditt et al

ADVANTAGES AND LIMITATIONS OF IMPLANTABLE LOOP RECORDERS
Limitations• Surgical implantation • Does not record other potentially important
parameters (e.g., BP)• Sx - ECG correlation not available when
automatic recordings are obtained• Does not distinguish vasovagal episodes
from conduction system disease
Benditt et al

RECOMMENDATIONS FOR IMPLANTABLE CARDIOVERTER DEFIBRILLATORS
IN SYNCOPAL PATIENTSClass I
Syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at EPS
Class IIaReasonable for patients with unexplainedsyncope, significant LV dysfunction, andnonischemic dilated cardiomyopathy
Reasonable for patients with Brugada syndrome who have had syncope.
ACC/AHA/HRS Guidelines 2008

ACC/AHA/ESC 2006Management of Patients with Ventricular
Arrhythmias and the Prevention of Sudden Cardiac Death
EP Testing in Patients with Syncope
Class IPatients with syncope of unknown cause with impaired LV function or structural heart disease
Class IIa Can be useful in patients with syncope whenbrady- or tachyarrhythmias are suspected,and in whom noninvasive diagnostic studiesare not conclusive.

RECOMMENDATIONS FOR ICDS IN SYNCOPAL PATIENTS
Class IIb
May be consideered in patients with syncope and advanced structural heart disease in whom thorough invasive andnoninvasive investigations have failed to define a cause.
Class III
Syncope of undetermined cause in a patientwithout inducible ventricular tachyarrhythmiasand without structural heart disease.
ACC/AHA/HRS Guidelines 2008

ESC GUIDELINES ON SYNCOPE
For Dx: Strongly recommended
• Suspected or known significant heart disease
• ECG abnormalities suggestive of arrhythmic syncope
• Syncope during exercise
• Syncope causing severe injury
• Strong family history of sudden death
Europace 2004;6: 467-537
Hospital Admission for Syncope Management

ESC GUIDELINES ON SYNCOPE
May need to be admitted• Patients with or without heart disease but with:
Sudden palpitations shortly before syncopeSyncope in supine positionWorrisome family historySignificant physical injury
• Patients with minimal or mild heart disease when there is high suspicion for cardiac syncope
• Suspected pacemaker or ICD problem
Europace 2004;6: 467-537

For Rx:
• Cardiac arrhythmias as cause
• Syncope due to cardiac ischemia
• Syncope due to structural cardiac or pulmonary disease
• Stroke or focal neurologic disorders
• Cardioinhibitory neurally mediated syncope when pacemaker implant is planned
Europace 2004;6: 467 - 537
Hospital Admission for Syncope Management
ESC GUIDELINES ON SYNCOPE

INDICATIONS TO REFER SYNCOPAL PTTO ELECTROPHYSIOLOGIST
•Neurocardiogenic syncope, especially if refractory to avoidance of triggers and drug Rx, or associated with prolonged pauses in cardiac rhythm
•Arrhythmia identified during evaluation:- VT due to any cause - Bradyarrhythmia caused by Rx that
cannot be withheld or changed- Supraventricular tachycardia, esp. with
WPW conduction

INDICATIONS TO REFER SYNCOPAL PT TO ELECTROPHYSIOLOGIST
• Congenital long QT syndrome• Brugada syndrome• Structural heart disease• Syncope in athletes• Syncope during exercise• Short QT syndrome• Origin of syncope remains unknown and
prolonged arrhythmia monitoring by implantable loop recorder is being considered