Collapse and syncope
-
Upload
drianturner -
Category
Health & Medicine
-
view
201 -
download
0
Transcript of Collapse and syncope

CollapseandSyncopeDR IAN TURNER FACEM

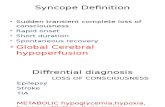
Definitions
▪ Transient LOC + loss of postural tone + full spontaneous recovery
▪ Loss of postural tone +/- LOC

Multiple causes
Toxicological
Conduction blocks
Aortic dissection
Addison’sSeizure
CVA
Psychogenic
Bradydysrhythmias
Tachydysrhythmias
Autonomic dysfunction
Aortic stenosis
HOCM
Vasovagal
Orthostatic hypotension
Pulmonary embolus
Hypoglycaemia
Subarachnoid haemorrhage
Iatrogenic
GI bleed

Case 1
▪ 80 male▪ PHx – T2DM, HPT,
hypercholesterolaemia▪ Witnessed collapse with LOC when
walking down the street after having got up to leave the hairdressers▪ Now well

Case 1 – Important Questions
History▪ Previous episodes▪ Associated symptoms▪ Medications
Examination▪ Vitals (postural changes)▪ Murmurs▪ Neuro (posterior circulation)▪ PR for blood

Case 1 – Useful Tests
Bedside Tests▪ BSL▪ ECG▪ VBG▪ MSU
Other Investigations▪ As indicated


Case 1 – Now what?
▪ Admit?▪ Indications for PPM?

Case 2
▪ 82 female▪ Usually well▪ Nauseated, dizzy for last 2 hours▪ Afeb, HR 48, SBP 89/51, RR 20,
SaO2 100%


Case 2 - Interventions
Inferior STEMI▪ Definitive – reperfusion▪ Symptom control▪ Antiplatelet agents▪ Anticogaultion
Bradydysrhythmia▪ Atropine▪ Isoprenaline▪ Adrenaline▪ Pacing▪ Reperfusion

Case 3
▪ 54 female▪ At work, sudden onset headache
with collapse▪ Headache persisting, much less
severe, otherwise feels well

Case 3 – Important Questions
History▪ Headache details▪ Neurological symptoms▪ Family history
Exam▪ Vitals▪ Focal neurology▪ Meningism▪ Papilloedema

Case 3 – Important Questions
Bedside Tests▪ The usual
Other investigations▪ CT +/- A▪ MRI/A▪ LP – timing?



Case 3 – Should I do an LP?
▪ http://www.thennt.com/risk/high-risk-headache-in-the-emergency-department/▪ We probably do more than we need▪ Often subspecialty driven▪ Can find other diagnoses

Case 3 – Should I do an LP? Complications
▪ CommonBack pain (25%)Headache (22%)Radicular pain (15%)▪ Unlikely
Paraparesis (1.5%)▪ Rare
Infection (<1%)Bleeding (<1%)

Case 4
▪ 74 male referred by GP with 2/7 dizziness and bradycardia▪ Normotensive but ambulance
officers concerned by rhythm strip


Case 4 – What interventions will you consider?
▪ Cardiac monitoring▪ IV access▪ Temporising medications▪ Electrolyte corrections▪ Pacing

Case 5
▪ 67 female collapse at home▪ 1/52 of dizziness, nausea, and
visual changes▪ PHx – AF, MVR (endocarditis)▪ Meds – aspirin, warfarin, digoxin


Case 5 – Choose two blood tests
▪ Digoxin = 3.7nmol/L (2.8ng/mL)▪ Potassium = 4.2mmol/L

Case 5 – What interventions are indicated?
▪ Cardiac monitoring▪ With-hold digoxin▪ Antidotes?▪ What if the potassium was 7.1mmol/L?

Case 6
▪ 71 male BIBA following witnessed loss of consciousness at lunch whilst sitting▪ Now feels fine and determined to
go home▪ PHx – HPT, CCF▪ Meds – prazosin, irbesartan,
frusemide, metoprolol▪ SHx – lives alone

Case 6 – ED workup
History and exam▪ Dizzy, followed by
witnessed period of unresponsiveness, then return to normal GCS
Usual investigations▪ Normal

Case 6 – Discharge or Admit
▪ Gestalt▪ Decision rules▪ Social circumstances

Case 6 – Decision Rules
▪ San Francisco syncope rule (“CHESS)”▪ Boston syncope rule▪ Rose criteria▪ STePS criteria
▪ Generally good sensitivityAverage to poor specificity

Case 7
▪ 19 male collapse and LOC whilst running▪ Usually fit and well▪ Brief CPR by bystanders with swift
return of consciousness▪ FHx – unexplained deaths in father
and uncle▪ Now well▪ Normal examination

Case 7 – Red flags?
▪ Young▪ Exertional syncope▪ Family history

Case 7 – Differentials?
▪ Conduction abnormalities▪ Structural heart disease▪ Channelopathies




Case 7
▪ Exertional syncope and abnormal ECG – admit!▪ Will need further cardiology workup▪ A lot end up with AICD

Case 8
▪ 47 male▪ Usually well▪ Palpitations since yesterday▪ Now dizzy and nauseated▪ Afeb, HR 195, BP 89/50


Case 8 – what are your actions?
▪ Cardiac monitor▪ Defib pads▪ IV access▪ Fluid bolus▪ Rate or rhythm control – why?


Case 8 – Rhythm control, how?
▪ Electrical▪ Synced▪ Sedation determined by urgency and cardiovascular
stability


Case 8 – Discharge or admit?
▪ Completely asymptomatic▪ Decision for anticoagulation▪ Need for ongoing rhythm control


Case 9
▪ 72 F▪ Witnessed collapse at the Italian
Club▪ Headache and persistent nausea▪ “Doctor, doctor, dizzy, dizzy”▪ PHx – AF, HPT, T2DM▪ Meds – aspirin, perindopril,
metformin, gliclazide▪ SHx – home with husband, ESL▪ O/E – Hypertensive, nystagmus, left
sided weakness

Case 9 – Red flags?
▪ Sudden onset▪ Persistent symptoms▪ Headache▪ ESL▪ Multiple cardiovascular risk factors

Case 9 – Investigations
▪ Normal ECG▪ Normal bloods▪ CT…



Case 9 - Management
▪ Analgesia and antiemetics▪ Neuro obs – risk of raised ICP with larger posterior fossa
strokes▪ Blood pressure control▪ Neurology opinion and consideration of thrombolysis▪ Stroke unit