Sulfur Mustard-Induced Ocular Surface Disordersbaradaran-rafii.com/files/articles/16.pdfSulfur...
Transcript of Sulfur Mustard-Induced Ocular Surface Disordersbaradaran-rafii.com/files/articles/16.pdfSulfur...

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 163
Sulfur Mustard-Induced Ocular Surface DisordersAlireza Baradaran-Rafii, MD,1 Medi Eslani, MD,1 and
Scheffer C. G. Tseng, MD, PhD2
Clinical PracticeJohn E. Sutphin, MD, editor
©2011 Ethis Communications, Inc. The Ocular Surface ISSN: 1542-0124. Baradaran-Rafii A, Eslani M, Tseng SCG. Sulfur mustard-induced ocular surface disorders. 2011;9(3):163-178.
ABSTRACT Sulfur mustard is a vesicant agent with severe
irritating effects on living tissues, including skin, mucous
membranes, eyes, and respiratory tract. The eyes are the most
susceptible tissue to mustard gas effects, and varying degrees
of ocular involvement are seen in 75% to 90% of exposed indi-
viduals. Most cases resolve uneventfully; however, a minority of
exposed patients will have a continuous process, which mani-
fests clinically either as a persistent smoldering inflammation
(chronic form) or late-onset lesions appearing many years after a
variable “silent” period (delayed form). Distinctive features com-
mon to most cases with chronic involvement include chronic
blepharitis, meibomian gland dysfunction, dry eye, limbal
ischemia, limbal stem cell deficiency, aberrant conjunctival ves-
sels, corneal neovascularization, and secondary degenerative
changes, including lipid and amyloid deposition and corneal
irregularity, thinning and scarring. Most cases can be managed
with conservative measures, eg, preservative-free artificial
tears, lubricants, and topical steroids. Punctal plugs or punctal
cauterization is helpful in moderate and severe forms of injury.
Surgical modalities, including lateral or medial tarsorrhaphies,
amniotic membrane transplantation, lamellar or penetrating
keratoplasty, and stem cell transplantation have been used.
KEY WORDS chemical warfare agents, corneal burns,
corneal transplantation, mustard gas, oxidative stress, sulfur
mustard
I. INTRODUCTION
ustard gas was first produced by Meyer in 1886. It was used initially as a vesicant agent for chemical warfare in World War I by the German army.1,2
It is a vesicant agent with severe irritating effects on living tissues, including skin, mucous membranes, eyes, and respi-ratory tract.3, 4 Because of its use as a weapon in World War I and in over 10 subsequent conflicts, including the Iraq-Iran war (1980-1988), its properties became more widely known in the 20th century.3, 4 Its late-onset, progressively destructive effects were recognized 15-20 years after its use.5 A minor-ity of exposed patients will develop late destructive ocular complications, which are usually progressive and permanent and can lead to reduction of visual acuity and even corneal blindness.3, 4 The ubiquitous production, simple and cheap chemical synthesis, easy stockpiling, and toxic nature of this agent make it a worldwide threat. Because of its destructive properties, combined with the lack of an effective antidote, some experts have classified mustard gas as one of the most significant chemical warfare agents.6-8
II. PHARMACOLOGY
The mustard agent is a straw-colored, oily liquid and has the odor of onion, garlic, or mustard, hence its name.9 It mainly consists of two chemical forms: sulfur mustard [S(CH2-CH2-Cl)2 or (2,2’-dichlorethyl sulphide; HD)], and nitrogen mustard [N(CH2-CH2-Cl) or (N-methyl-2,2’-dichlorodiethylamine; HN2)].2, 10 The former is longer acting and more commonly used in chemical warfare, but the latter is more toxic.2, 4,5,11 The popular term “mustard gas” is a misnomer, as this agent actually appears as an aerosol of small oily droplets.12 The toxicity of sulfur mustard (SM) as an incapacitating agent is of much greater importance than its capacity to kill via a lethal dose 50% (LD50).12,13 The LD50 for humans is about 200 mg when the substance is swallowed, 4-5 g when it is applied to the bare skin over a long exposure time, and 1500 mg/min/m3 when inhaled.2,14 It is a stable compound in low temperatures, which can persist in clothing or on the ground for months.3 On contact with human skin, 80% of the liquid evaporates and 20% penetrates; half of this remains in the skin and the other half is absorbed systemically.2 Additionally, due to free hydrolization by the interface organs, SM causes systemic effects only at very high doses.15
Accepted for publication May 2011.From the 1Ophthalmic Research Center, Department of Ophthalmology, Labbafinejad Medical Center, Shahid Beheshti University of Medical Sci-ences, and 2Ocular Surface Center, Ocular Surface Research and Education Foundation, Miami, Florida, USA.Dr. Tseng and his family are more than 5% shareholders of TissueTech. Inc., which owns US patents 6 152 142 and 6 326 019 on the method of preparation and clinical uses of human amniotic membrane and ProKera™ distributed by Bio-Tissue Inc. Other authors have no proprietary or commercial interests in any concept or product discussed in this article.Single-copy reprint requests to: Alireza Baradaran-Rafii, MD (address below).Corresponding author: Alireza Baradaran-Rafii, MD, Labbafinejad Medical Center, Department of Ophthalmology, Boostan 9 St., Pasdaran Ave., Tehran 16666, Iran. Tel-fax: +98-21-22587317. E-mail: [email protected].
M

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com164
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al
The measurement of biochemical markers in aqueous humor is a tool for evaluating SM-induced damages even before the onset of clinical signs. The concentration of protein in aqueous humor increases 4-6 hours following exposure; although it decreases after 28 hours, it still re-mains higher than in non-exposed controls. This increase, together with the presence of cellular lymphocytic infiltra-tion, is indicative of an inflammatory reaction. Aqueous humor glutathione at the very early stages of SM exposure may change in a similar pattern.16,17Alkylation products of SM with DNA and proteins (eg, hemoglobin and albu-min), as well as its urinary metabolites,18-22 have proved to be useful targets for diagnosing SM exposure in humans. Urinary markers are readily accessible, although their rapid elimination limits their use for retrospective detection. Ad-ducts with macromolecules such as proteins offer longer lasting (possibly up to several months) biological markers of exposure to SM.23,24 The DNA adducts can also be detected in urine, processed skin, and blood samples.25-29
III. PATHOPHYSIOLOGY
Mustard gas damages viable tissues only, and the exact mechanism for this is not clear. Theories include liberation
of intracellular hydrochloric acid, formation of new com-pounds acting as alkylating agents, and, finally, formation of oxidative derivatives, which collectively can lead to more cellular damage.9,11,30-34 Mustard gas causes additional in-jury via skin and eye damage after absorption through the integument and the ocular surface; respiratory damage after inhalation; and systemic toxicity after ingestion or high exposures. As a result, it may further cause gastrointestinal, circulatory, and bone marrow toxicity.34 Hence, the destruc-tive effects of SM are not localized to the site of application, as remote cells and tissues also become affected.3 The high sensitivity of the eye to SM is due to the readily accessible aqueous-mucous surface of the cornea and conjunctiva, as well as the high turnover rate and intense metabolic activity of corneal epithelial cells.35
SM causes a cross-linking of the 2 complementary strands in the DNA molecule by a monofunctional alkyla-tion of the nitrogenous bases. The major alkylating site of nucleic acids is the nitrogen residue of guanine.36 The results are manifested in chromatid aberrations; inhibition of DNA, RNA, and protein synthesis; blocking of the cell’s cycle in the G2-M phase; and, eventually, cell death.2,37-40 SM tends to undergo intramolecular cyclization to create a hyperac-tive compound.41 Conversion to this derivative is facilitated in an aqueous solution, which accounts for the sensitivity of mucosal tissues (such as in the eye) to its action.42 The cyclic intermediate reacts with and alkylates electron-rich molecular structures, such as the sulfhydryl (-SH), amino (-NH2), carboxyl, hydroxyl, and primary phosphate groups of proteins and nucleic acids.12,42-44 Additionally, the alkyl-ated DNA activates poly-ADP-ribose polymerase, which leads to cellular depletion of nicotinamide adenosine dinucleotide (NAD), thus inhibiting multiple reactions in the cell.6,7 The depletion of NAD also leads to upregula-tion of the hexosemonophosphate shunt, which stimulates protease activity in the cell. These proteases are thought to play a role in blister formation, compounded by the death of multiple keratinocytes.6,7,43 It also directly inhibits various glycolytic and respiratory enzymes,36 impairs glucose uptake mechanisms,45 and generates oxidative stress through the formation of free radicals.2,46
Inhibition of cellular respiratory enzymes resulting in the formation of free radicals has been suggested as another pathophysiologic mechanism affecting predominantly pro-liferative epithelial cells in the ocular surface.11 Evidence for oxidative stress in tissues exposed to SM or its analogs includes increased formation of reactive oxygen species and the presence of peroxidized lipid products and proteins. Although there is an increase in antioxidant enzymes, eg, superoxide dismutase, catalase, and glutathione-S-trans-ferase, suggesting the presence of cellular defense, further inhibition of antioxidant enzymes, including thioredoxin reductase, by SM disrupts such cellular redox homeostasis.32 A dramatic increase (30-fold) in copper levels and a decrease in ascorbic acid is observed within the anterior chamber after ocular exposure to mustard compounds, and both of these are indicators of oxidative stress.17,47
OUTLINE
I. Introduction II. Pharmacology III. Pathophysiology IV. Immunologic mechanisms V. Systemic manifestations
A. SkinB. Respiratory tractC. Bone marrowD. Other organ damage
VI. Ocular involvementA. Acute phaseB. Chronic phaseC. Pathologic findingsD. Confocal microscopy
VII. Initial management following sulfur mustard exposure VIII. Management of ocular injuries
A. Acute phaseB. Chronic phase
1. Medical treatment2. Surgical intervention
a. Tarsorrhaphyb. Amniotic membrane transplantationc. Stem cell transplantationd. Corneal transplantation
3. Treatment algorithm4. Postoperative medical regimen and surgical
outcomeC. Novel and potential therapies for mustard gas injury
IX. Summary

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 165
Free radicals have already been shown to play a role in corneal inflammation after exposure to other ocular ir-ritants, such as alkali substances.48,49 In such cases, tissue damage after corrosive injury to the cornea is exacerbated by penetration of reactive oxygen species to the corneal stroma, leading to fragmention of DNA chains, polymeriza-tion or depolymerization of proteins and hyaluronate, and destruction of lipid membranes.49 Reactive oxygen species reduce ferric iron and copper and produce the highly reac-tive hydroxyl radicals. These reduced metal ions, in turn, can react with H2O2 to produce the hydroxyl radical, which causes further damage.50
Other potential mechanisms of cell death are related to rapid inactivation of sulfhydryl-containing proteins and pep-tides, such as glutathione. These sulfhydryl compounds are critical for maintaining the appropriate oxidation-reduction state of cellular components. Glutathione is also thought to be critical for reducing reactive oxygen species in the cell and preventing peroxidation and loss of membrane integrity, which, in turn, prevents cytokine-mediated inflammatory response.6,51-53 Clinically impaired corneas display increased matrix metalloproteinase (MMP) activity, in particular, MMP-9 in the acute phase.54 There is a potential role for nitric oxide in tissue injury induced by SM and related ana-logs. Of particular importance is the reaction of nitric oxide with the reactive oxygen species superoxide anion, forming peroxynitrite. Peroxynitrite is a strong oxidant and nitrating agent and is known to trigger oxidative injury.32
IV. IMMUNOLOGIC MECHANISMS
Animal and human studies have demonstrated that SM has short- and long-term influences on both humoral and cellular immune functions.12,55-58 The perilimbal site of the lesions, their similarity to Mooren’s ulcer, and mixed inflammatory infiltrate within substantia propria suggest the immunological basis of SM-induced delayed kerati-tis.3,59,60 Depression of cell-mediated immunity has been reported.55,56 Total white blood count and percentages of monocytes and CD3+ lymphocytes are significantly higher in SM-exposed patients.57 In addition, the percentage of NK cells (CD16+) is significantly lower in patients with severe respiratory complications up to 20 years after SM exposure.13,55,56 A significant positive correlation has been found between hemoglobin level and the severity of ocular complications.57 Increased levels of IgG, IgM, and C3 have been reported in the majority of SM-exposed patients dur-ing the first weeks and up to the sixth month after expo-sure.13,55 It has been noted that even 20 years after exposure, the percentage of patients with increased IgM, IgG, and IgE are still significantly higher than in the control group.12,55-57
In study of rabbits with SM injury, a significant increase in interleukin (IL)-1, IL-6, IL-8, tumor necrosis factor, MMP-2, and MMP-9 activities in the aqueous humor was observed.61 The analysis of inflammatory mediators over time indicates that the SM injury progresses to the posterior part of the cornea, initiating the production of cytokines/chemokines, which, in turn, may activate MMPs. MMP-2
and MMP-9 degrade collagen, thus contributing to the deterioration of the stroma.61 It remains to be determined whether SM-damaged corneal stroma might elicit alloreac-tive responses that lead to further degradation, similar to Mooren’s ulcers. Abnormalities in the immune system may contribute to recurrent infections, septicemia, and a higher incidence of malignancies in these patients.12,56,62
V. SYSTEMIC MANIFESTATIONS
Acute toxic effects appear after variable periods of la-tency, depending on the dose, mode of exposure, environ-mental temperature, and personal susceptibilities.2,3,6,12,34,63 Victims may have multiple sites of injury, including skin, eye, and respiratory systems.12 Organ damage is influenced by different concentrations of mustard gas exposure. The eye damage starts with exposure doses of 50 mg/min/m3. At 100-400 mg/min/m3 of exposure, respiratory and cutaneous systems are affected. At a dose of more than 200 mg/min/m3, severe ocular and respiratory afflictions are observed. Skin burns occur at 200-1000 mg/min/m3, and severe incapacitation from skin burns ensues at 750–10,000 mg/min/m3.12 The reported fatality rates are less than 2% of the exposed soldiers during World War I and 3% to 4% in the Iraq-Iran conflict.2,3 Death usually results from either respiratory failure due to chemical bronchitis/pneumonia or bone marrow suppression.2,3
A. Skin
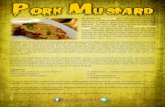
The cutaneous effects of SM exposure begin after a latent period lasting for 0-24 hours. The characteristic skin lesion of SM is erythema followed by blisters.64,65 At higher doses, vesicles form at the periphery of the erythematous areas, which later merge into pendulous bullae containing large volumes of clear yellow fluid.6,7 Bullous lesions are particularly likely to occur on warm, moist areas, such as axilla, genitalia, and areas where tight clothing is worn.7,8 They tend to form within 24 hours of exposure, but some-times appear 7–12 days later. Large blisters usually break, leading to erosions and full-thickness ulceration (Figures 1 A and B). Necrosis may occur at these sites, followed by
Figure 1. Facial bullous lesions in acute phase with use of silver sulfadiazine ointment (A) and without it (B).
A B
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com166
formation of a scar at 72 hours post-exposure. In the case of extensive bullae formation, fluid and elec-
trolyte imbalance combined with secondary infection may complicate recovery.64, 65 Blistering and necrotic wounds may lead to permanent residual effects, including hyper- or hypo-pigmentation, atrophy, hypertrophy, dermal scar, dryness of the skin, erythematous papular rash, multiple cherry angiomas, local hair loss, eczema, chronic urticaria, vitiligo, psoriasis, and discoid lupus erythematous.12,14,34,63-68
Healing time varies depending on the extent of cellular damage and the ability of the body to replenish scavengers of electrophilic stress and reactive oxygen species.6,7 SM-induced lesions tend to heal slowly, and often ulcerate and vesicate repeatedly for reasons that are still unclear.6,7 One likely explanation is the propensity for SM to affect rapidly dividing cells, such as the basal cell layer of keratinocytes in the epidermis.6,7
Other clinical forms of cutaneous lesions are pigmentary exfoliation, superficial vesicular to bullous form, bullous necrotization, deep necrotizing non-bullous form, allergic and toxic contact reactions. The pigmentary exfoliative form is often combined with severe lung damage.12,14,34,63-68
B. Respiratory Tract
Depending on the dose of SM and duration of the contact, pain and discomfort may develop in the nose or sinuses with increasing secretions, sneezing, nonproductive hacking cough, and sore throat 4-16 hours after exposure. This can develop into epistaxis, aphonia, tracheobronchitis, dyspnoea, and possible hemorrhage into the alveoli and microbial bronchopneumonia.12 Necrosis of the mucosa with associated inflammation can lead to the formation of a diphtheritic-like membrane in the most severe cases, ob-structing any level of the airways,69 and later, to the clinical picture of adult respiratory distress syndrome.35,70,71 Several years later, patients may be left with obstructive and restric-tive pulmonary functions, bronchiectasis and bronchiolitis obliterans, chronic bronchitis, asthma, large airway nar-rowing, and pulmonary fibrosis.72-80 Chronic bronchitis has been reported as the most common late complication of the respiratory system.72,74-76,79,80 Progressive hypoxemia and hypercapnea are commonly observed in moderate-to-severe cases, leading to corpulmonale and respiratory failure.53,63,80 The infection of the respiratory tract is a common problem, often complicated by septicemia.42
C. Bone Marrow
Bone marrow suppression can develop within 3-5 days of high-dose SM exposure, manifested as aplastic or ineffec-tive hematopoiesis, leukopenia, and thrombocytopenia.57 In some cases, chronic bone marrow suppression appears 7-15 days after exposure, resulting in sepsis and pneumonia6,7 and higher mortality rates.12
D. Other Organ Damage
Gastrointestinal symptoms in the acute phase of SM injury include nausea and vomiting, which is often accom-
panied by respiratory distress resulting from immediate bronchospasm.6,7 Clinical findings are acute gastroduodeni-tis with hemorrhagic erosions, acute desquamative enteritis, and severe hemorrhagic necrotic colitis.6,12 Central nervous system involvement includes headache, anxiety, fear of the future, restlessness, confusion, lethargy, and convul-sions.6,12 In addition, patients can develop pulmonary, na-sopharyngeal and laryngeal cancers, basal cell and Bowen’s carcinomas, adenocarcinoma of the stomach, and acute myeloblastic and lymphoblastic leukemia.66,81-86 Although an association between exposure to this chemical agent and ocular surface malignancies has not been reported, confocal microscopic findings have exhibited bizarre and abnormally enlarged pleomorphic keratocytes in all cases with SM-induced keratopathy.14,87,88
VI. OCULAR INVOLVEMENT
The moistness of the ocular surface, the extreme lipo-philic nature of the gas, and the high turnover rate and meta-bolic activity of corneal epithelial cells make the eye the most susceptible part of the body to the effects of SM exposure.2,6,11 Varying degrees of ocular involvement are seen in 75% to 90% of individuals exposed to mustard gas.6 The acute symptoms usually resolve completely without further inflammation after 2-6 weeks. However, photophobia may persist for some time. In a minority of patients, a continuous process clinically appearing either as a persistent smoldering inflammation (chronic form) or late-onset lesions appearing many years af-ter a variable “silent” period (delayed form) may develop.2,3,6
It remains unclear whether mustard gas actually induces a continuous process of progressive inflammation on the ocular surface with different speeds of individual progression. In the chronic form of injury, severe acute lesions abate, but symp-toms such as photophobia, dry eye, and foreign body sensation persist, and sequelae such as corneal epithelial erosions, lim-bal ischemia, and, occasionally, peripheral corneal thinning and neovascularization may slowly progress.3 In the delayed form, patients become asymptomatic and enjoy improvement of their lesions several weeks after initial exposure, only to experience resurgence of symptoms several years later.2,3,6
A. Acute Phase
Within several hours of SM exposure, symptoms begin to appear.6,15,53 The severity and timing of clinical symptoms and signs seem to be related to dose, concentration, and duration of contact.6,15 As early as 1 hour after exposure, clinical manifestations start with a sensation of grittiness, progressive soreness, and a bloodshot appearance before proceeding to edema and giving rise to “acute conjunctivi-tis.” At 2-6 hours, patients complain of severe ocular pain, lacrimation, photophobia, blepharospasm, and decreased visual acuity.6,12 The gradual spontaneous recovery usually occurs after 48 hours, with full regeneration of the corneal epithelium occurring within 4-5 days, although complete symptomatic recovery may take 6 weeks or longer.2,6,7,63
Based on severity, immediate lesions can be divided into three groups: mild, moderate, and severe.2
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 167
Mild lesions are caused by exposure to 12-70 mg/min/m3 and manifest as mild eyelid erythema/swelling and con-junctival engorgement without significant chemosis.2,34 The cornea usually is spared, and recovery is complete within a few days.2
Moderate lesions are caused by exposure to 100-200 mg/min/m3 mustard gas. The eyelid, conjunctival, and corneal lesions are of the same type that occur with mild injury, but are more severe.2,34,89 Symptoms include a dry sensation, severe ocular pain, photophobia, and severe blepharo-spasm.2,5,17,34,90 The corneal epithelium begins to vesicate and slough predominantly in the interpalpebral fissure, leading to superficial punctate keratitis, corneal abrasions, superficial infiltrations, corneal ulcers, and even perfora-tion.9,12,61,90 The superior cornea is relatively spared, probably due to the protective effect of the upper lid.91 After 48 hours, pain and blepharospasm gradually decrease and the corneal epithelium usually heals completely within 4-5 days. Full resolution of symptoms may take up to 6 weeks or longer.2
Severe lesions occur after exposure to more than 200 mg/min/m3 mustard gas.2,3,6 Patients with such exposure often sustain associated systemic toxicity in the respira-tory, gastrointestinal, and integumentary systems.3 In addition to the moderate lesions, limbal vasculature and deeper layers of the cornea are also involved. The eyelids may become ulcerated. The nasal and temporal limbi lose their normal vasculature and become white and necrotic. In addition to having marked congestion and chemosis, severe conjunctival lesions are characterized by areas of ischemia and necrosis, particularly in the interpalpebral fissure.2,3,6 There may be low-grade iridocyclitis, which usu-ally leaves no synechia or cataract formation, and, rarely, the intraocular pressure is transiently elevated.2,4,89 Because conjunctival lesions are limited to the interpalpebral fissure, adhesions between the globe and eyelid are unlikely.3 The corneal epithelial irregularity and stromal edema combine to create an orange peel appearance, which usually does not stain with fluorescein; however, epithelial erosions and small corneal ulcers may be noted (Figure 2).2,3 They are prone to bacterial superinfection, including Pseudomonas aeruginosa, which can lead to severe intraocular infection necessitating evisceration or urgent tectonic penetrating keratoplasty (PKP).2,3 Corneal sensation may be affected to varying degrees.3 There may be pupillary constriction,
iris vasodilatation, hemorrhages, and necrosis, with de-velopment of anterior uveitis. Improvement often begins within 1-2 weeks, when the corneal edema resolves and the uveitis subsides. A few weeks later, neovascularization begins. These tortuous blood vessels tend to bleed into the corneal subepithelial space and stroma. They eventually undergo rapid degeneration, leaving white opacities in the otherwise clear cornea.2,3
B. Chronic Phase
A continuous process leading to a chronic form or a delayed form of injury develops in less than 1% of exposed individuals up to 40 years after their exposure.2,3,6,12,34,92 In contrast to acute lesions, chronic and delayed mustard gas lesions usually cause permanent reduction in visual acuity and can even lead to blindness.3 Distinctive features include chronic blepharitis, meibomian gland dysfunction, dry eye, limbal ischemia, limbal stem cell deficiency (LSCD), corneal neovascularization, lipid and amyloid deposition, and ir-regularity, thinning and scarring of the cornea.2,3,6,12,34,61 It remains unknown whether disease activity correlates with hotter and drier climates.3
In the chronic form of injury, patients suffer from photophobia, injection, tearing, and foreign body sensa-tion.12,91 Impaired corneal sensation, damaged limbal vas-culature, and recurrent epithelial erosions produce corneal irregularity, thinning, and neovascularization, leading to descemetoceles and perforation.2,3,6,12,34,50,61,91 Corneal neo-vascularization can lead to intrastromal exudation of plasma lipids and deposition of amyloids.59,93 Despite the ongoing inflammation, the eye may appear quiet. Nonetheless, this should not be considered as quiescence, as it may be the result of vascular necrosis resulting in ischemia.2,3, 50,59,91
In the delayed-onset form of injury, after a silent period of several years, patients begin to suffer from foreign body sensation, tearing, redness, and severe photophobia.12,91 In early stages, the limbal region frequently presents a marbled appearance in which porcelain-like areas of ischemia are surrounded by blood vessels of irregular diameter.2,3,6
Varicose, tortuous, ampulliform and leaking vessels that characteristically are accompanied by blood islands and hemorrhages surround perilimbal ischemic areas.2,94 This may lead to lipoid depositions in the adjacent cornea and trigger chronic stromal inflammation and thinning.2,3,95 It may also aggravate the clinical situation and produce severe photophobia and tearing.59,93 Later, vascularized scars of the cornea are covered with crystal and cholesterol deposits, leading to worsening of opacification, recurrent ulcerations, and sometimes corneal perforation.2,3,6,12,34,61,93 Opacification of the central and lower portions of the cor-nea is typical, while the upper sections are often protected by the eyelids.2,9,91 These lesions even recur after corneal transplantation.96 A minority of patients might develop corneal perforation and phthisis bulbi.2
The presence of ischemic conjunctival areas, intrastro-mal corneal and conjunctival hemorrhages and bloody islands, lipoid and amyloid depositions, and aberrant neo-Figure 2. Corneal stromal edema in acute severe exposure.
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com168
vascularization may be signs of chronic vasculitis induced by mustard gas. The chronic conjunctival and corneal in-flammation can lead to chronic blepharitis with lid margin thickening and meibomian gland dysfunction.35 No cases with keratinization have been reported to date.3,59
Ocular surface involvement can be graded as mild, moderate, or severe. Conjunctival vessel changes, including telangiectasia, tortuosity, and segmentation, are character-istics of the mild form, and the adjacent corneal quadrant is clear in this form. Limbal ischemia and peripheral vessel invasion with or without corneal opacity are features of the moderate form. If previous findings are accompanied by severe corneal thinning and melting, the involvement is considered severe (Figures 3 A-D).3,59 The clinical picture of SM-induced ocular surface disease is a continuous spectrum of manifestations that make it difficult to clearly grade its severity. LSCD gradually begins in moderate forms and finally ends in total LSCD in most severe cases.
It appears that late clinical manifestations of SM kera-topathy result from several underlying mechanisms. LSCD progresses from partial and asymmetric to total LSCD be-cause of a direct and progressive detrimental effect of mus-tard gas or chronic limbal ischemia.3,95 We cannot ignore the likelihood that chronic ischemia or the detrimental effect of mustard gas may disturb the stem cell niche, resulting in progressive stem cell attrition. Damage to corneal nerves leading to the loss of corneal sensation also contributes to this detrimental process over time.1,17 In an animal study, degeneration of nerve fibers with a typical subsequent Wallerian degeneration was observed after exposure, and continued for weeks to months afterwards.54
Autoimmune reactions to the corneal antigens altered
by the mustard agent (collagen-mustard compound) have also been proposed.2,97 In delayed mustard gas keratopathy, limbal ischemia plays a significant role in the corneal neu-rotrophic and trophic changes, including thinning, desce-metocele formation, and perforation.59 The role of known angiogenic factors in SM-induced angiogenesis has not been yet elucidated.17,98-103 Inflammation may play a role in propagating the SM-delayed response; animal experiments have shown that anti-inflammatory treatment decreases the primary inflammatory reaction, as well as the extent of neovascularization.17,54,104
The clinical course of corneal injuries like alkaline/acidic burns is quite similar in all victims.105 The question of why some eyes are more vulnerable than others to the late response of SM is still unanswered. Vulnerability may be re-lated to concentrations, total doses, contact duration, mode of exposure, environmental temperature, the extent of use of protective equipment, personal susceptibilities, individual closeness to the ground, age, and other factors.2,3,6,30,59,63,106 Generally, children are more severely affected by SM expo-sure than adults, most likely because children have thinner skin and are closer to the ground, where mustard vapors accumulate.6,106 Reports of late response to SM exposure would also be related to type and duration of follow-up.
A puzzling feature in delayed mustard gas keratitis regards the unpredictable exacerbations and remissions in the clinical course, with peripheral corneal infiltrations, at times extending to the central cornea, mimicking Mooren’s ulcer.3,60 Corneal infiltrations usually are accompanied by neovascularization (morphologically similar to conjunctival vessels), which is an unfavorable prognostic factor.3,60 Infil-trations may be accompanied by intrastromal hemorrhages,
Figure 3. A. Mild form of ocular involvement with tortu-ous, telangiectatic, conjunctival vessels surrounding some areas of severe perilimbal conjunctival ischemia. B. Invading leaking, aberrant telangiectatic ampul-liform vessels with lipid deposi-tion (moderate form). C. A patch of severe peripheral corneal thinning with amyloid deposi-tion adjacent to perilimbal tel-angiectatic vessels (severe form). D. Severe nasal and temporal corneal thinning with invading segmented leaking vessels and lipid deposition (severe form).
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 169
corneal necrosis, thinning, descemetocele formation, and perforation.3,54 Recurrent episodes lead to centripetal and deeper infiltrations, and degenerative changes finally take place and crystalline deposits are noted over time.2,3,6,12,60
Stem cell deficiency is one of the main factors con-tributing to mustard gas-induced keratopathy.59 However, corneal manifestations are not typical of the partial or total LSCD seen with severe chemical burns. With SM-induced keratopathy, the cornea is not covered by a total vascular-ized pannus; instead, corneal thinning with amyloid and lipoid depositions are prominent. In some areas, leaking telangiectatic vessels invade peripheral cornea. Corneal involvement is often asymmetric between the two eyes, and in each eye, severity of involvement is not the same in all quadrants. Most often, the interpalpebral (exposure) area of the cornea that is adjacent to conjunctival ischemic areas is more severely damaged.59 This may be due to direct contact of the interpalpebral fissure during the exposure or to more severe perilimbal ischemia in these areas. In turn, perilimbal ischemia may be due to direct exposure of tissues with consequent vasculitis.59
In summary, corneal manifestations seem to be a mixture of progressive chronic limbal ischemia and stem cell deficiency.3 The differences in the clinical picture may be related to exposure pattern. In chemical burns, a high concentration of acid/alkali liquids is in direct contact with limbal stem cells, while aerosolized gas is in contact with the ocular surface during an SM attack.2,3,59 Numerous animal studies have investigated the clinical picture and pathophysiologic mechanisms of SM-induced keratopathy, but these are beyond the scope of this review.12,32,54
C. Pathologic Findings
Light microscopic observation of corneas 48 hours after SM exposure reveals epithelial denudation and marked stromal edema accompanied by cellular infiltration, mostly of eosinophils. Endothelial destruction is occasionally observed.60 Epithelial regeneration starts 72 hours after exposure by migration of remaining noninjured corneal or conjunctival cells.17,60 The latter is confirmed by the presence of goblet cells scattered diffusely in the newly regenerated epithelium.17 In moderate forms of injury, extensive loss of conjunctival mucous and goblet cells associated with occlu-sion of conjunctival blood vessels (as a result of destruction of vascular endothelial cells) are observed.97 The corneal epithelium is loosened from its stroma (at the palpebral fissure), and small vesicles are formed, in which the corneal free nerve endings are exposed.2,60
Histopathologic features of the conjunctival component in patients with chronic or delayed mustard gas keratopa-thy include chronic inflammation, perilimbal conjunc-tival ischemia, telangiectasis, vasculitis, subconjunctival hemorrhage, decreased number of goblet cells, thinning or thickening of epithelium, scar formation in substantia propria, lymphocytic infiltration, and dilated lymphatic vessels.3,8,17,50,54,60,91,107 There are no signs of dysplasia.59
Corneal pathologic findings include destruction of
the epithelium and Bowman’s layer, loss of keratocytes, conjunctivalization, superficial and stromal vasculariza-tion, squamous metaplasia, focal corneal thinning and ulceration, acute and chronic infiltration of inflammatory cells, lipoid/amyloid deposition, endothelial cell loss, calcific band keratopathy, and scarring in the stroma.3,8,17,50,54,60,91,107 Perilimbal conjunctival vasculitis and ischemia may con-tribute to the corneal cytopathologic features.59, 60 Corneal squamous metaplasia, which is mild-to-moderate in most cases and has been suggested as a diagnostic factor in cases with mild or subclinical limbal deficiency, may be a reactive response to mustard gas (Figure 4).108
D. Confocol Microscopy
Although SM cannot easily achieve deep corneal pen-etration, in the acute phase, it targets endothelial cells, in-ducing apoptosis at lower concentrations and both apoptosis and necrosis at higher concentrations. In chronic and de-layed-onset forms of injury, abnormal confocal microscopic findings are observed in all corneal layers. The anterior and middle portions are affected more severely than the pos-terior parts.88 The mosaic pattern of basal epithelial cells is not apparent. Their density decreases and most of the cells look pleomorphic, with damaged or irregular high-contrast boundaries. Generalized decreased density of keratocytes has been reported, but their gradient pattern is controver-sial.88,91,109 Keratocyte density decreases progressively from the anterior to the posterior stroma in normal cornea. Within the anterior corneal stroma, spindle-like keratocytic nuclei (perhaps representing necrotic keratocytes) close to Bowman layer could be delineated. Normal keratocytes are capable of dividing and migrating after injury.110
It has been suggested that the genetically altered kerato-cytes may lose their ability to repopulate the injured stroma in mustard gas keratopathy.88 Bizarre and abnormally enlarged pleomorphic keratocytes are observed in almost all cases.88,91,109 Intrastromal microdots, which are compat-ible with foci of stromal necrosis, may be observed.88 Foci of amyloid degeneration and lipid deposition and stromal neovascularization, have been reported, as well.88
Degenerative processes seem to dominate in chronic and
Figure 4. Markedly attenuated corneal epithelium, loss of Bowman’s layer, foci of mild chronic inflammation around intrastromal vascular-ization, foci of stromal degeneration and severe loss of endothelial cells (H&E, x 200).
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com170
delayed mustard gas keratopathy. The presence of dendritic cells without their dendrites and activated keratocyte nuclei may indicate ongoing inflammation at the microscopic level.109 These changes in the interstitial matrix of the cornea may be a potential barrier for repopulation of stromal kera-tocytes.88 Decreased sub-basal nerve plexus is observed in most of the cases, which could be secondary to destruction of the Bowman layer, occurrence of subepithelial fibrosis, and associated dry eye.88 However, the thickness of the midstromal irregular circular node-like nerve structure may increase (Figures 5 A-D).88,109
VII. INITIAL MANAGEMENT OF SYSTEMIC
MANIFESTATIONS
There is no effective antidote for mustard gas exposure, so prevention is the most effective management strategy. Special protective garments and gas masks containing a charcoal layer to absorb penetrating sulfur mustard are highly effective in preventing dermal, respiratory, and ocular injuries.2,6,8 However, chemical goggles, gas masks, and protective clothing are cumbersome and inefficient for daily use in military or civilian populations.111
The first priority of treatment after mustard gas ex-posure is to remove victims from the contaminated areas and initiate decontamination procedures. Contaminated clothes must be removed and destroyed. Rapid riddance from the skin is critical, as mustard penetrates the tissues within minutes of exposure, and its effects become ir-reversible.2,12,111 When available, absorbent powders such as calcium chloride, magnesium oxide, activated charcoal, talcum powder, Fuller’s earth, and flour, should be used to decontaminate the skin. The powder is sprinkled onto the
exposed skin and allowed to absorb the mustard, and is then washed off with water.2, 111
When mustard exposure is suspected, the victim should be washed with hypochlorite 0.5%, calcium hypochlorite (72 g/L), neutrogenic soap/shampoo (pH around 7.0), and copi-ous amounts of warm water for a prolonged period of time. Complete hydrolysis of mustard renders it nontoxic. Washing of the affected area with oil, kerosene, or gasoline, followed by washing with soap and water, has also been advocated.12,112
Even in asymptomatic patients, the eyes should be washed as soon as possible with generous amounts of water, normal saline, and Ringer solution.12 Sodium bicarbon-ate1.5%, dichloramine-T 0.5%, and saturated solutions of sodium sulfate or magnesium sulfate, as well as zinc or boric acid, have also been suggested.12 Because of the rapid and irreversible reaction of SM with ocular tissues, it may seem that irrigation would not be useful more than 10-15 minutes after exposure; however, irrigation at this later point is recommended, as it does no harm and may help.2 Of the many fluids studied for use in ocular irrigation, none has proved more effective than tap water.2
Upon arrival at a medical facility, the victims should be quickly examined by medical doctors for severity grading of SM intoxication. The mild cases that do not reveal any sign of intoxication should be kept under observation and may be discharged after 24 hours. Those who show any sign of SM poisoning during observation should, along with moderate and severe victims, receive emergency management. If a large surface area is affected, fluid and electrolyte balance must be maintained. The management of skin lesions focuses on the prevention of secondary bacte-rial infections by applying sulfamylon (mefenide acetate),
Figure 5. Confocal microscope scans, x 500. A. Moderate loss of stromal keratocytes with a few residual keratocytes and pleomophic nuclei. B. Severe loss of stromal keratocytes and presence of hyper-reflective microdots. C. Hyper-reflective crystals of lipid keratopathy. D. Moderately reflective reticular pattern due to amyloid deposits in the stroma.
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 171
silvadene (silver sulfadiazine), povidone iodine or bacitracin zinc to the affected areas, and administration of systemic antibiotics to prevent secondary infections.6,12, 113,114 Bio-syntheic dressings, ie, hydrogels and hydrocolloiods, may accelerate healing. Steam inhalation, cough suppressants, oxygen therapy, assisted ventilation, early intubation, and bronchodilators are immediate measures for respiratory involvement. Systemic steroids and antibiotics may be help-ful for severe affliction.6
Medical treatment can be divided into antidotal/gen-eral treatments and care of specific organs. In the antidotal treatment, up to 500 mg/kg sodium thiosulphate should be administered as soon as possible. It reacts with mustard gases when these agents are in the cyclized form. Thus, it is an effective antidote against systemic intoxication, especially when taken before exposure.6,12 Sodium thiosulphate can also be combined with a number of other drugs, such as cysteine, sodium citrate, dexamethasone, promethazine, heparin and vitamine E, to increase its protective activity against SM.115
VIII. MANAGEMENT OF OCULAR INJURY
A. Acute Phase
The ocular lesions can be differentiated into conjunc-tival only and corneal involvement by fluorescein staining performed immediately after ocular washings. Medical therapies in this stage include topical antibiotics, preser-vative-free lubricants, and corticosteroids.2,6,12 In the case of corneal involvement, close observation is necessary. Treatment should include daily ocular irrigation, artificial tears, therapeutic contact lenses, mydriatics (to reduce ocular pain produced by spasm of the ciliary muscle and to prevent posterior synechiae), antibiotic drops (to prevent secondary bacterial infections), and topical antiglaucoma medications (to control intraocular pressure).2,6,50,63 The use of lubricants is controversial, as they may concentrate mustard gas particles trapped under the eyelids.2 Ocular bandages should be avoided, as they might raise the corneal temperature and accelerate the toxic effects.2,12 Topical cor-ticosteroids should be cautiously used.2,6,12 Although they may reduce eyelid, conjunctival, and corneal swelling and improve anterior uveitis, they may predispose the cornea to infection.6,12 Petroleum jelly can be used on the follicu-lar margins to prevent sticking. However, it should not be used immediately after exposure, as mustard can become concentrated in this oily medium.2,34, 113 Dark glasses and patient reassurance are very important, as the eye lesions produce severe photophobia and fear.9,113
Amniotic membrane transplantation can suppress in-flammation and scarring and promote healing in patients suffering from a variety of ocular surface diseases.116-121 Used during the acute stage of Stevens-Johnson syn-drome122 and acute chemical burn,123-127 its healing and anti-inflammatory effects have been shown to prevent late sight-threatening cicatricial complications. Therefore, it may be beneficial in the control of acute stages of SM-induced ocular surface disorders.
B. Chronic Phase
1. Medical TreatmentNo definitive treatment for chronic and delayed mus-
tard gas-induced ocular surface disorders is available.2,3,6,12 Current therapy is mainly conservative and directed at symptomatic relief, as it addresses tear deficiency and ocular surface instability (ie, artificial tears, temporary or perma-nent punctal occlusion, blepharorrhaphy, tarsorrhaphy and therapeutic contact lenses).2,3,6 Because the ocular surface is compromised, especially in the moderate and severe forms of injury, preservative-free artificial tears or gels should be used. Punctal plugs are usually beneficial.1,50,61 Permanent occlusion of one or both puncti of each eye by electrocautery may be preferable.95
Topical steroids can be used to control ocular surface inflammation and acute episodic corneal inflammatory infiltrates.2,3 Preservative-free topical steroids are benefi-cial, especially for short-term usage.3 Although systemic steroids are not usually necessary, in the case of severe corneal inflammations, they may be combined with topi-cal steroids.3 However, long-term steroid-induced com-plications, including cataract and glaucoma, should be considered.2,6,12 Because of the loss of corneal integrity with mustard gas keratitis, the ocular surface is prone to secondary microbial infection; thus, topical steroids should be used cautiously.95,96
High DK silicone hydrogel contact lenses can improve punctate epithelial erosions and keratitis, as well as per-sistent epithelial defects (PEDs) in the context of partial LSCD. With total LSCD, they are not effective, and they can increase the risk of secondary microbial infections.2,3,6,12 Treatment of associated blepharitis is recommended in all cases. To improve visual acuity, spectacles and high DK soft/hard contact lenses may be cautiously used.3,5 Most cases with severe and recurrent inflammatory infiltrates respond well to conservative measures, including topical/systemic steroids.95,96 Adjuncts such as lubricants and topical antibiotics may help.2,3,61
2. Surgical Interventionsa. Tarsorrhaphy
In the case of nasal or temporal progressive corneal thin-ning with or without PEDs, medial or lateral tarsorrhaphy may halt progression of corneal thinning.3,95 It can also dra-matically improve the symptoms of patients with chronic oc-ular surface irritation and dry eye.59 It is highly recommend-ed after any type of stem cell or corneal transplantation.95,96
b. Amniotic Membrane TransplantationAmniotic membrane transplantation can be used to treat
PEDs that occur with partial LSCD.54,95 However, it is not useful when LSCD is severe or total.54 In severely irritated eyes with annoying photophobia due to corneal lipoid de-position, superficial keratectomy combined with amniotic membrane transplantation is very beneficial (Figures 6 A and B).95 Amniotic membrane transplantation may also be used as a patch or graft as an adjunct to various kinds of
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com172
stem cell transplantation.54,59,95,128-134 It may also be used as an adjunct to medical therapy in cases with recurrent corneal inflammatory infiltrates to decrease ocular surface inflammation and reduce scarring.59,134 Multilayered am-niotic membrane transplantation can be used in corneas with severe thinning.135,136
c. Stem Cell TransplantationCandidates for stem cell transplantation include patients
suffering from chronic irritation, redness, and tearing of the eyes with PEDs associated with severe corneal thinning, who are unresponsive to conservative treatments (artifi-cial tears, lubricants, punctal occlusion, blepharorrhaphy and tarsorrhaphy).95 Limbal areas adjacent to the thinnest peripheral corneal areas with epithelial defects are selected as potential surgical sites. In some situations, simultaneous penetrating or lamellar keratoplasty can be performed.95,96
Limbal stem cells can be harvested from immediate family members, including parents, siblings, or children (living-related conjunctival-limbal allograft [lr-CLAL]) or cadaveric eyes (keratolimbal allograft [KLAL]). Human leu-kocyte antigen (HLA) matching is not obligatory. Various surgical techniques have been previously described.95,137-142
Tissue harvested from one or both eyes of an immediate family member is fresher and has closer genetic composi-tion than KLAL. On the other hand, a KLAL graft is more accessible and has more stem cells. However, besides being less fresh than an lr-CLAL graft, it is more prone to chronic stem cell attrition and rejection. Due to partiality, bilateral-ity, and asymmetry of LSCD; and discrepancy in severity of quadrant involvement, complete 360-degree coverage of the limbal area by graft is unnecessary.95 Sectoral KLAL/lr-CLAL in areas with the most severe thinning and LSCD appears to be adequate (Figures 7 A and B).
In a recent study, the rejection-free graft survival rate was reported to be 39.1% in the lr-CLAL group and 80.7% in the KLAL group at month 40, with a mean follow-up period of 24.9 and 68.8 months, respectively.143 Because simultane-ous systemic problems exist in patients after mustard gas exposure, minimal necessary immunosuppression should be used.95,96 In some cases with severe ischemia, simultane-ous resection of ischemic conjunctiva and advancement of near normal conjunctiva may be beneficial. It is not clear whether conjunctival advancement or tenonplasty should be used to correct ischemia before stem cell transplantation.
Figure 6. A. Inferior corneal lipid deposition with leaking aberrant vessels. B. Three months after superficial keratectomy and amniotic membrane transplantation, the eye is quiet.
Figure 7. Sector keratolimbal allograft in a case with severe per-ilimbal corneal thinning and persistent epithelial defect before (A) and after (B) surgery.
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 173
d. Corneal TransplantationPenetrating or lamellar keratoplasty may be sufficient
when LSCD is not severe and when visual acuity is de-creased due to central corneal opacification caused by amy-loid/lipoid deposition.3,96 In such circumstances, perilimbal conjunctival ischemia is usually mild. Due to the recurrent and chronic nature of the disease, it is advisable to spare the posterior stroma and corneal endothelium, avoiding the associated ocular surface derangements; thus, lamellar keratoplasty (LKP) is preferred.88
A full-thickness graft is required for deeper lesions. Tectonic PKP may be needed in eyes with severe corneal thinning, large descemetoceles, and impending or frank corneal perforation. Tectonic LKP may also be performed in cases with small descemetoceles.3,96 Conventional LKP, or deep anterior lamellar keratoplasty (DALK; Melles and Anwar techniques) can be performed.144,145 The rejection-free graft survival rate has been reported to be 39.0% in PKP patients and 90.3% in LKP patients at month 28, with a mean follow-up length of 29.6 and 85.0 months, respectively.143 Most often, due to corneal scar formation and variability of corneal thickness and its irregularity, conventional LKP and Melles techniques are preferred. Although, corneal transplantation can be simultaneously performed with limbal stem cell transplantation, it is advisable to perform it at least 3 months after stem cell transplantation.95 Because of the compromised ocular surface, corneal transplantation in cases with SM-induced keratopathy is considered high-risk.59,96 Cases with severe LSCD and severe limbal ischemia with peripheral corneal thinning may have a high rate of graft failure due to rejection reactions, recurrent opacity, and corneal thinning.95,96
3. Treatment Algorithm (Figure 8)Conservative management, which is the main modality
in the mild form of SM injury, should be applied in all grades of delayed-onset SM-induced ocular surface disease. In the moderate form with partial stem cell deficiency, corneal opacity can be managed with corneal transplantation alone. In this grade, PED due to partial stem cell deficiency and lim-bal ischemia can be treated by AMT. In severe forms with se-vere LSCD associated with severe corneal thinning and melt-ing, stem cell transplantation is the best option. Subsequent corneal transplantation can be used to improve visual acuity.
4. Postoperative Medical Regimen and Surgical OutcomeTopical antibiotic and steroid drops (especially pre-
servative-free) are used when indicated, but tapered and discontinued when corneal epithelialization is complete and ocular surface inflammation declines. Topical 20% autologous serum, preservative-free artificial tears, and lubricating gels or ointments are also useful. Oral pred-nisolone 1 mg/kg should be started and tapered off during 6-8 weeks with decreasing inflammation, and antiglaucoma medications should be used as necessary.95,96 Because of the progressive nature of the disease, regular follow-up visits
Figure 8. Treatment algorithm for chronic/delayed-onset sulfur mustard-induced ocular surface disorders. See text for details. AMT = amniotic membrane transplantation; LSCT = limbal stem cell trans-plantation; PKP = penetrating keratoplasty; LKP = lamellar keratoplasty.
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al
are highly recommended.In general, optimization of the ocular surface by the
aforementioned measures is required after corneal trans-plantation. The dose of systemic steroids should be in-creased for a period after corneal transplantation to decrease ocular surface inflammation. Immunosuppressive therapy may be required in the case of recurrent rejections, previous failure, or the presence of other risk factors.96,146-148
Different systemic and topical immunosuppressive regi-mens have been suggested for allogenic stem cell transplan-tation.3,130,131,138,149,150 Systemic cyclosporine A 3 to 5 mg/kg has been used in patients with SM-induced ocular surface disease.95,96,109 Combined systemic immunosuppression us-ing more potent and safer immunosuppressives, including mycophenolate mofetil 1 to 2 gr/day and tacrolimus 2-6 mg/day, has been shown to be more effective than cyclosporine A in promoting survival in solid organ transplantations, as it lessens acute rejection.151 Doses should be adjusted accord-ing to ocular surface inflammation and systemic adverse effects.131 Given the multiple organ involvement in patients with SM-induced ocular surface disease, the optimal dose, combination, and duration of therapy should be carefully adjusted and evaluated in further studies. Because of the potential side effects of systemic immunosuppression, close collaboration with an immunosuppressive therapy expert is highly recommended.
Living-related limbal stem cell transplantation has been shown to be an effective way to stabilize the severely inflamed ocular surface in patients with advanced mustard gas keratopathy. This can markedly decrease subjective complaints, heal PEDs, and lead to regression of peripheral corneal neovascularization.95 The long-term results of sec-toral KLAL have not yet been reported in such cases. Acute rejection, which is more prevalent in the early months after

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com174
surgery, is manifested by the occurrence of limbal and peri-limbal engorgement of vessels associated with conjunctival chemosis in the limbal transplant area. This can be treated by increasing the dose and frequency of topical and systemic steroids. The dose is gradually tapered with the elimination of vascular engorgement and local chemosis.95,96 Graft failure due to acute rejection is rare.88 Whether acute stem cell rejection(s) predispose the patient to chronic rejection has yet to be elucidated.
The results of PKP or LKP alone or combined with stem cell transplantation has been shown to be promising with proper case selection.88,96 Success may be related to the lack of structural defects in the ocular adnexa, symblepharon formation, partiality of stem cell deficiency, mildness of dryness, and absence of corneal exposure.3,59,88,95,96 Corneal transplantation in these patients is high-risk due to the com-promised ocular surface, especially LSCD and perilimbal conjunctival ischemia, chronic inflammation, and decreased sensation.152-155 However, with appropriate management, graft clarity and visual outcomes have been reported to be favorable in long-term follow-up.96
Even with successful corneal transplantation, SM-induced ocular surface disease may progress and recur (Figures 9 A and B). A rate of endothelial rejection up to 59% has been reported.96 Although endothelial immune rejections were relatively common in these patients, most of them did not lead to graft failure. Optimization of the ocular surface and keeping it free of inflammation are critical for survival of the transplanted stem cells and corneal graft. It has been observed that corneal grafts performed after stem cell transplantation have better results than corneal grafts alone.95,96,138 Graft rejection may be more frequent in eyes that receive simultaneous corneal graft and stem cell transplantation than in those that have had the procedures sequentially.96 The major vision-limiting factors after a successful corneal transplantation are corneal epithe-lial breakdown, tear film instability, corneal astigmatism, steriod-induced glaucoma, and cataracts.96,156
C. Novel and Potential Therapies for Mustard
Gas Injury
Although progress has been made in understanding how the cornea responds to acute insults, the design of treatment strategies for SM injury is complicated by the lack of knowledge regarding the etiology of recurrent corneal disorders. In some animal studies, topical use of corticosteroids and nonsteroidal anti-inflammatory drugs,104 colchicine,157 a calcium-blocker (diltiazem),158 and MMP inhibitors (such as doxycycline)54 have been shown to reduce ocular inflammation. Reduced dermal and systemic injury has been reported after treatment with thiosulfate, nicotinamide, flavonoids, and topically applied iodine.46,50,159-161 Colchicine was found to inhibit the acute ocular response to nitrogen mustard in rabbits.157 Increased survival was noted in rats treated parenterally with vitamin E or dexamethasone within 15 minutes of exposure,162 while pre-exposure treatment of rats with nicotinamide (NAD+
precursor) decreased the severity of skin damage induced by sulfur mustard.2,163
Thymosin β4 is a highly conserved, 43 amino-acid polypeptide that has been shown to influence cell migra-tion, proliferation, and differentiation, promoting corneal wound healing, decreasing inflammation, and modulating activity of MMP when applied ectopically.61,164-169 This has been suggested as an antidote for SM injuries.61 Metal-locomplexes, such as zinc- or gallium-desferrioxamine, are known to inhibit the formation of highly reactive free radicals. It has been hypothesized that either complex ex-erts its protective effect by intervening in a critical step of hydroxyl radical formation during acute phase damage.50
Nitric oxide synthase inhibitors, including topical iodine preparations and aminoguanidine, have been reported to protect or rescue cells in vitro from SM-induced toxicity.170 Ebelson, a peroxynitrite scavenger that did not affect nitric oxide synthase activity, has also been reported to be an effec-tive inhibitor of SM–induced toxicity.32 Several studies have shown that glutathione or the its prodrug N-acetylcysteine can reduce oxidative stress and toxicity induced by SM or its analogs.31,32,171-174
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al
Figure 9. A. Successful lamellar keratoplasty in a patient with moderate form of SM-induced ocular surface disease and decreased visual acuity due to extensive central corneal amyliod deposition. B.
Recurrence of keratopathy 1.5 years after surgery.

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 175
IX. SUMMARY
The vesicant agent sulfur mustard has been used as a weapon in several wars. Acute ocular manifestations of exposure include conjunctival redness, lacrimation, photophobia, blepharospasm, corneal edema, ulcer, iris vasodilatation/hemorrhages, and anterior uveitis. Most cases resolve uneventfully; however, a minority of exposed patients develop a continuous process manifesting as a persistent smoldering inflammation (chronic form) or late-onset lesions appearing many years after a variable “silent” period (delayed form). Distinctive clinical features are chronic blepharitis, meibomian gland dysfunction, dry eye, limbal ischemia, vasculitis, stem cell deficiency, corneal neovascularization, lipid and amyloid deposition, corneal irregularity, thinning and scarring. The main pathophysi-ologic mechanisms of injury consist of progressive DNA alkylation and formation of reactive oxygen species that ultimately lead to limbal stem cell deficiency and severe perilimbal conjunctival ischemia/vasculitis.
Conservative treatment, including preservative-free artificial tears, lubricants, topical steroids, and punctal plugs/cauterization are sufficient in most patients. Lateral or medial tarsorrhaphy, amniotic membrane transplanta-tion, lamellar or penetrating keratoplasty and stem cell transplantation may be necessary for visual rehabilitation in eyes with moderate-to-severe disease.
ACKNOWLEDGMENTThe authors appreciate Naser Emadi, MD, Kumars Movafaghi-Toossi, BSc, and Mojgan Rezaei-Kanavi, MD, for their kind assistance.
REFERENCES 1. Blodi FC. Mustard gas keratopathy. Int Ophthalmol Clin 1971;11:1-13 2. Solberg Y, Alcalay M, Belkin M. Ocular injury by mustard gas. Surv
Ophthalmol 1997;41:461-6 3. Javadi MA, Yazdani S, Sajjadi H, et al. Chronic and delayed-onset
mustard gas keratitis: report of 48 patients and review of literature. Ophthalmology 2005;112:617-25
4. Safarinejad MR, Moosavi SA, Montazeri B. Ocular injuries caused by mustard gas: diagnosis, treatment, and medical defense. Mil Med 2001;166:67-70
5. Mann I. A study of eighty-four cases of delayed mustard gas keratitis fitted with contact lenses. Br J Ophthalmol 1944;28:441-7
6. Saladi RN, Smith E, Persaud AN. Mustard: a potential agent of chemical warfare and terrorism. Clin Exp Dermatol 2006;31:1-5
7. Smith KJ, Skelton H. Chemical warfare agents: their past and continuing threat and evolving therapies. Part I of II. Skinmed 2003;2:215-21
8. Smith KJ, Skelton H. Chemical warfare agents: their past and continuing threat and evolving therapies. Part II of II. Skinmed 2003;2:297-303
9. Dahl H, Gluud B, Vangsted P, Norn M. Eye lesions induced by mustard gas. Acta Ophthalmol Suppl 1985;173:30-1
10. Watson AP, Griffin GD. Toxicity of vesicant agents scheduled for de-struction by the Chemical Stockpile Disposal Program. Environ Health Perspect 1992;98:259-80
11. Aasted A, Darre E, Wulf HC. Mustard gas: clinical, toxicological, and mutagenic aspects based on modern experience. Ann Plast Surg 1987;19:330-3
12. Balali-Mood M, Hefazi M. The pharmacology, toxicology, and medi-cal treatment of sulphur mustard poisoning. Fundam Clin Pharmacol
2005;19:297-315 13. Balali-Mood M, Hefazi M, Mahmoudi M, et al. Long-term complications
of sulphur mustard poisoning in severely intoxicated Iranian veterans. Fundam Clin Pharmacol 2005;19:713-21
14. Dacre JC, Goldman M. Toxicology and pharmacology of the chemical warfare agent sulfur mustard. Pharmacol Rev 1996;48:289-326
15. Smith KJ, Hurst CG, Moeller RB, et al. Sulfur mustard: its continuing threat as a chemical warfare agent, the cutaneous lesions induced, progress in understanding its mechanism of action, its long-term health effects, and new developments for protection and therapy. J Am Acad Dermatol 1995;32(5 Pt 1):765-76
16. Riley MV, Meyer RF, Yates EM. Glutathione in the aqueous humor of human and other species. Invest Ophthalmol Vis Sci 1980;19:94-6
17. Kadar T, Turetz J, Fishbine E, et al. Characterization of acute and de-layed ocular lesions induced by sulfur mustard in rabbits. Curr Eye Res 2001;22:42-53
18. Black RM, Brewster K, Clarke RJ, et al. Biological fate of sulphur mustard, 1,1‘-thiobis(2-chloroethane): isolation and identification of urinary metabolites following intraperitoneal administration to rat. Xenobiotica 1992;22:405-18
19. Black RM, Read RW. Detection of trace levels of thiodiglycol in blood, plas-ma and urine using gas chromatography-electron-capture negative-ion chemical ionisation mass spectrometry. J Chromatogr 1988;449:261-70
20. Black RM, Read RW. Biological fate of sulphur mustard, 1,1‘-thiobis(2-chloroethane): identification of beta-lyase metabolites and hydrolysis products in human urine. Xenobiotica 1995;25:167-73
21. Wils ER, Hulst AG, de Jong AL, et al. Analysis of thiodiglycol in urine of victims of an alleged attack with mustard gas. J Anal Toxicol 1985;9:254-7
22. Wils ER, Hulst AG, van Laar J. Analysis of thiodiglycol in urine of victims of an alleged attack with mustard gas, Part II. J Anal Toxicol 1988;12:15-9
23. Black RM, Clarke RJ, Harrison JM, Read RW. Biological fate of sulphur mus-tard: identification of valine and histidine adducts in haemoglobin from casualties of sulphur mustard poisoning. Xenobiotica 1997;27:499-512
24. Noort D, Benschop HP, Black RM. Biomonitoring of exposure to chemi-cal warfare agents: a review. Toxicol Appl Pharmacol 2002;184:116-26
25. Benschop HP, van der Schans GP, Noort D, et al. Verification of exposure to sulfur mustard in two casualties of the Iran-Iraq conflict. J Anal Toxicol 1997;21:249-51
26. Fidder A, Moes GW, Scheffer AG, et al. Synthesis, characterization, and quantitation of the major adducts formed between sulfur mustard and DNA of calf thymus and human blood. Chem Res Toxicol 1994;7:199-204
27. Fidder A, Noort D, de Jong LP, et al. N7-(2-hydroxyethylthioethyl)-guanine: a novel urinary metabolite following exposure to sulphur mustard. Arch Toxicol 1996;70:854-5
28. Langenberg JP, van der Schans GP, Spruit HE, et al. Toxicokinetics of sulfur mustard and its DNA-adducts in the hairless guinea pig. Drug Chem Toxicol 1998;21 Suppl 1:131-47
29. van der Schans GP, Scheffer AG, Mars-Groenendijk RH, et al. Immuno-chemical detection of adducts of sulfur mustard to DNA of calf thymus and human white blood cells. Chem Res Toxicol 1994;7:408-13
30. Livingston PC, Walker HM. A study of the effects of liquid mustard gas upon the eyes of rabbits and of certain methods of treatment. Br J Ophthalmol 1940;24:67-97
31. Gould NS, White CW, Day BJ. A role for mitochondrial oxidative stress in sulfur mustard analog 2-chloroethyl ethyl sulfide-induced lung cell injury and antioxidant protection. J Pharmacol Exp Ther 2009;328:732-9
32. Laskin JD, Black AT, Jan YH, et al. Oxidants and antioxidants in sulfur mustard-induced injury. Ann N Y Acad Sci 2010;1203:92-100
33. Jampol LM, Axelrod A, Tessler H. Pathways of the eye‘s response to topical nitrogen mustard. Invest Ophthalmol 1976;15:486-9
34. Borak J, Sidell FR. Agents of chemical warfare: sulfur mustard. Ann Emerg Med 1992;21:303-8
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com176
35. Etezad-Razavi M, Mahmoudi M, Hefazi M, Balali-Mood M. Delayed ocular complications of mustard gas poisoning and the relationship with respirato-ry and cutaneous complications. Clin Experiment Ophthalmol 2006;34:342-6
36. Wheeler GP. Studies related to the mechanisms of action of cytotoxic alkylating agents: a review. Cancer Res 1962;22:651-88
37. Graham JS, Schomacker KT, Glatter RD, et al. Efficacy of laser de-bridement with autologous split-thickness skin grafting in promoting improved healing of deep cutaneous sulfur mustard burns. Burns 2002;28:719-30
38. Requena L, Requena C, Sanchez M, et al. Chemical warfare. Cutaneous lesions from mustard gas. J Am Acad Dermatol 1988;19:529-36
39. Ruhl CM, Park SJ, Danisa O, et al. A serious skin sulfur mustard burn from an artillery shell. J Emerg Med 1994;12:159-66
40. Savage JR, Breckon G. Differential effects of sulphur mustard on S-phase cells of primary fibroblast cultures from Syrian hamsters. Mutat Res 1981;84:375-87
41. Gilman A, Philips FS. The biological actions and therapeutic applications of the B-chloroethyl amines and sulfides. Science 1946;103(2675):409-36
42. Somani SM, Babu SR. Toxicodynamics of sulfur mustard. Int J Clin Pharmacol Ther Toxicol 1989;27:419-35
43. Lindahl T. DNA glycosylases, endonucleases for apurinic/apyrimi-dinic sites, and base excision-repair. Prog Nucleic Acid Res Mol Biol 1979;22:135-92
44. Crathorn AR, Roberts JJ. Mechanism of the cytotoxic action of alkylating agents in mammalian cells and evidence for the removal of alkylated groups from deoxyribonucleic acid. Nature 1966;211(5045):150-3
45. Gross CL, Meier HL, Papirmeister B, et al. Sulfur mustard lowers nico-tinamide adenine dinucleotide concentrations in human skin grafted to athymic nude mice. Toxicol Appl Pharmacol 1985;81:85-90
46. Elsayed NM, Omaye ST, Klain GJ, Korte DW Jr. Free radical-mediated lung response to the monofunctional sulfur mustard butyl 2-chloroethyl sulfide after subcutaneous injection. Toxicology 1992;72:153-65
47. McGahan MC, Bito LZ. The pathophysiology of the ocular microenvi-ronment. I. Preliminary report on the possible involvement of copper in ocular inflammation. Curr Eye Res 1982;2):883-5
48. Nirankari VS, Varma SD, Lakhanpal V, Richards RD. Superoxide radical scavenging agents in treatment of alkali burns. An experimental study. Arch Ophthalmol 1981;99:886-7
49. Pfister RR, Haddox JL, Yuille-Barr D. The combined effect of citrate/ascorbate treatment in alkali-injured rabbit eyes. Cornea 1991;10:100-4
50. Banin E, Morad Y, Berenshtein E, et al. Injury induced by chemical warfare agents: characterization and treatment of ocular tissues exposed to nitrogen mustard. Invest Ophthalmol Vis Sci 2003;44:2966-72
51. Rankin PW, Jacobson MK, Mitchell VR, Busbee DL. Reduction of nicotinamide adenine dinucleotide levels by ultimate carcinogens in human lymphocytes. Cancer Res 1980;40:1803-7
52. Eklow L, Moldeus P, Orrenius S. Oxidation of glutathione during hy-droperoxide metabolism. A study using isolated hepatocytes and the glutathione reductase inhibitor 1,3-bis(2-chloroethyl)-1-nitrosourea. Eur J Biochem 1984;138:459-63
53. Greenfield RA, Brown BR, Hutchins JB, et al. Microbiological, bio-logical, and chemical weapons of warfare and terrorism. Am J Med Sci 2002;323:326-40
54. Kadar T, Dachir S, Cohen L, et al. Ocular injuries following sulfur mustard exposure--pathological mechanism and potential therapy. Toxicology 2009;263:59-69
55. Hassan ZM, Ebtekar M. Modeling for immunosuppression by sulfur mustard. Int Immunopharmacol 2001;1:605-10
56. Ghotbi L, Hassan Z. The immunostatus of natural killer cells in people exposed to sulfur mustard. Int Immunopharmacol 2002;2:981-5
57. Mahmoudi M, Hefazi M, Rastin M, Balali-Mood M. Long-term hema-tological and immunological complications of sulfur mustard poisoning
in Iranian veterans. Int Immunopharmacol 2005;5:1479-85 58. Smith KJ, Graham JS, Hamilton TA, et al. Immunohistochemical stud-
ies of basement membrane proteins and proliferation and apoptosis markers in sulfur mustard induced cutaneous lesions in weanling pigs. J Dermatol Sci 1997;15:173-82
59. Baradaran-Rafii A, Javadi MA, Rezaei Kanavi M, et al. Limbal stem cell deficiency in chronic and delayed-onset mustard gas keratopathy. Ophthalmology 2010;117:246-52
60. Rezaei Kanavi M, Javadi A, Javadi MA. Chronic and delayed mustard gas keratopathy: a histopathologic and immunohistochemical study. Eur J Ophthalmol 2010;20:839-43
61. Milhorn D, Hamilton T, Nelson M, McNutt P. Progression of ocular sulfur mustard injury: development of a model system. Ann N Y Acad Sci 2010;1194:72-80
62. Yokoyama WM. Recognition structures on natural killer cells. Curr Opin Immunol 1993;5:67-73
63. Balali-Mood M, Hefazi M. Comparison of early and late toxic effects of sulfur mustard in Iranian veterans. Basic Clin Pharmacol Toxicol 2006;99:273-82
64. Rice P. Sulphur mustard injuries of the skin. Pathophysiology and management. Toxicol Rev 2003;22:111-8
65. Momeni AZ, Aminjavaheri M. Skin manifestations of mustard gas in a group of 14 children and teenagers: a clinical study. Int J Dermatol 1994;33:184-7
66. Inada S, Hiragun K, Seo K, Yamura T. Multiple Bowen‘s disease observed in former workers of a poison gas factory in Japan, with special reference to mustard gas exposure. J Dermatol 1978;5:49-60
67. Kehe K, Szinicz L. Medical aspects of sulphur mustard poisoning. Toxicology 2005;214:198-209
68. Khateri S, Ghanei M, Keshavarz S, et al. Incidence of lung, eye, and skin lesions as late complications in 34,000 Iranians with wartime exposure to mustard agent. J Occup Environ Med 2003;45:1136-43
69. Freitag L, Firusian N, Stamatis G, Greschuchna D. The role of bronchos-copy in pulmonary complications due to mustard gas inhalation. Chest 1991;100:1436-41
70. Balali M. Clinical and laboratory findings in Iranian fighters with chemi-cal gas poisoning. Arch Belg 1984;Suppl:254-9
71. Hefazi M, Attaran D, Mahmoudi M, Balali-Mood M. Late respiratory complications of mustard gas poisoning in Iranian veterans. Inhal Toxicol 2005;17:587-92
72. Aghanouri R, Ghanei M, Aslani J, et al. Fibrogenic cytokine levels in bronchoalveolar lavage aspirates 15 years after exposure to sulfur mus-tard. Am J Physiol Lung Cell Mol Physiol 2004;287:L1160-4
73. Bagheri MH, Hosseini SK, Mostafavi SH, Alavi SA. High-resolution CT in chronic pulmonary changes after mustard gas exposure. Acta Radiol 2003;44:241-5
74. Beheshti J, Mark EJ, Akbaei HM, et al. Mustard lung secrets: long term clinicopathological study following mustard gas exposure. Pathol Res Pract 2006;202:739-44
75. Bijani K, Moghadamnia AA. Long-term effects of chemical weapons on respiratory tract in Iraq-Iran war victims living in Babol (North of Iran). Ecotoxicol Environ Saf 2002;53:422-4
76. Emad A, Rezaian GR. The diversity of the effects of sulfur mustard gas inhalation on respiratory system 10 years after a single, heavy exposure: analysis of 197 cases. Chest 1997;112:734-8
77. Emad A, Rezaian GR. Immunoglobulins and cellular constituents of the BAL fluid of patients with sulfur mustard gas-induced pulmonary fibrosis. Chest 1999;115:1346-51
78. Ghanei M, Akhlaghpoor S, Moahammad MM, Aslani J. Tracheo-bronchial stenosis following sulfur mustard inhalation. Inhal Toxicol 2004;16:845-9
79. Ghanei M, Fathi H, Mohammad MM, et al. Long-term respiratory
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com 177
disorders of claimers with subclinical exposure to chemical warfare agents. Inhal Toxicol 2004;16:491-5
80. Ghanei M, Mokhtari M, Mohammad MM, Aslani J. Bronchiolitis obliterans following exposure to sulfur mustard: chest high resolution computed tomography. Eur J Radiol 2004;52:164-9
81. Beebe GW. Lung cancer in World War I veterans: possible relation to mustard-gas injury and 1918 influenza epidemic. J Natl Cancer Inst 1960;25:1231-52
82. Easton DF, Peto J, Doll R. Cancers of the respiratory tract in mustard gas workers. Br J Ind Med 1988;45:652-9
83. Zojaji R, Balali-Mood M, Mirzadeh M, et al. Delayed head and neck complications of sulphur mustard poisoning in Iranian veterans. J Laryngol Otol 2009;123:1150-4
84. Ghanei M, Vosoghi AA. An epidemiologic study to screen for chronic myelocytic leukemia in war victims exposed to mustard gas. Environ Health Perspect 2002;110:519-21
85. Manning KP, Skegg DC, Stell PM, Doll R. Cancer of the larynx and other occupational hazards of mustard gas workers. Clin Otolaryngol Allied Sci 1981;6:165-70
86. Wada S, Miyanishi M, Nishimoto Y, et al. Mustard gas as a cause of respiratory neoplasia in man. Lancet 1968;1(7553):1161-3
87. Takeshima Y, Inai K, Bennett WP, et al. p53 mutations in lung cancers from Japanese mustard gas workers. Carcinogenesis 1994;15:2075-9
88. Jafarinasab MR, Zarei-Ghanavati S, Kanavi MR, et al. Confocal micros-copy in chronic and delayed mustard gas keratopathy. Cornea;29:889-94
89. Geeraets WJ, Abedi S, Blanke RV. Acute corneal injury by mustard gas. South Med J 1977;70:348-50
90. Mann I, Pullinger BD. A study of mustard gas lesions of the eyes of rabbits and men: (Section of Ophthalmology). Proc R Soc Med 1942;35:229-44
91. Pleyer U, Sherif Z, Baatz H, Hartmann C. Delayed mustard gas keratopathy: clinical findings and confocal microscopy. Am J Ophthalmol 1999;128:506-7
92. Blodi FC. Delayed mustard-gas keratopathy. Am J Ophthalmol 1953;36:1575-6
93. Mann I, Pullinger BD. The pathology of cholesterin and fat deposition in mustard gas injuries of the cornea. Br J Ophthalmol 1942;26:503-7
94. English F, Bennett Y. The challenge of mustard-gas keratopathy. Med J Aust 1990;152:55-6
95. Javadi MA, Baradaran-Rafii A. Living-related conjunctival-limbal allograft for chronic or delayed-onset mustard gas keratopathy. Cornea 2009;28:51-7
96. Javadi MA, Yazdani S, Kanavi MR, et al. Long-term outcomes of penetrating keratoplasty in chronic and delayed mustard gas keratitis. Cornea 2007;26:1074-8
97. Maumenee AE, Scholz RO. The histopathology of the ocular lesions produced by the sulfur and nitrogen mustard. Bull Johns Hopkins Hosp 1948;82:121-47
98. Amano S, Rohan R, Kuroki M, et al. Requirement for vascular endothelial growth factor in wound- and inflammation-related corneal neovascu-larization. Invest Ophthalmol Vis Sci 1998;39:18-22
99. Applegate LA, Ley RD. DNA damage is involved in the induction of opacification and neovascularization of the cornea by ultraviolet radia-tion. Exp Eye Res 1991;52:493-7
100. Campbell FW, Michaelson IC. Blood-vessel formation in the cornea. Br J Ophthalmol 1949;33:248-55
101. Eliason JA. Leukocytes and experimental corneal vascularization. Invest Ophthalmol Vis Sci 1978;17:1087-95
102. Lee P, Wang CC, Adamis AP. Ocular neovascularization: an epidemio-logic review. Surv Ophthalmol 1998;43:245-69
103. Sonoda K, Sakamoto T, Yoshikawa H, et al. Inhibition of corneal inflammation by the topical use of Ras farnesyltransferase inhibitors: selective inhibition of macrophage localization. Invest Ophthalmol Vis Sci 1998;39:2245-51
104. Amir A, Turetz J, Chapman S, et al. Beneficial effects of topical anti-
inflammatory drugs against sulfur mustard-induced ocular lesions in rabbits. J Appl Toxicol 2000;20 Suppl 1:S109-14
105. Ormerod LD, Abelson MB, Kenyon KR. Standard models of corneal injury using alkali-immersed filter discs. Invest Ophthalmol Vis Sci 1989;30:2148-53
106. Furlow B. Biological, chemical and radiological terrorism. Radiol Technol 2003;75:91-107; quiz 8-10
107. Rowell M, Kehe K, Balszuweit F, Thiermann H. The chronic effects of sulfur mustard exposure. Toxicology 2009;263:9-11
108. Lopez-Garcia JS, Rivas L, Garcia-Lozano I. [Corneal epithelium squamous metaplasia determination as diagnostic factor in limbal deficiency]. Arch Soc Esp Oftalmol 2006;81:281-8. Spanish
109 . Lagali N, Fagerholm P. Delayed mustard gas keratitis: clinical course and in vivo confocal microscopy findings. Cornea 2009;28:458-62
110. Wilson SE, Mohan RR, Ambrosio R Jr, et al. The corneal wound healing response: cytokine-mediated interaction of the epithelium, stroma, and inflammatory cells. Prog Retin Eye Res 2001;20:625-37
111. Smith KJ. The prevention and treatment of cutaneous injury secondary to chemical warfare agents. Application of these finding to other derma-tologic conditions and wound healing. Dermatol Clin 1999;17:41-60, viii.
112. Chiesman WE. Lesions due to vesicants: diagnosis and treatment. Br Med J 1944;2(4359):109-12
113. Murray VS, Volans GN. Management of injuries due to chemical weapons. Br Med J 1991;302(6769):129-30
114. Smith WJ, Dunn MA. Medical defense against blistering chemical warfare agents. Arch Dermatol 1991;127:1207-13
115. Callaway S, Pearce KA. Protection against systemic poisoning by mustard gas, di(2-chloroethyl) sulphide, by sodium thiosulphate and thiocit in the albino rat. Br J Pharmacol Chemother 1958;13:395-8
116. Bouchard CS, John T. Amniotic membrane transplantation in the management of severe ocular surface disease: indications and outcomes. Ocul Surf 2004;2:201-11
117. Dua HS, Gomes JA, King AJ, Maharajan VS. The amniotic membrane in ophthalmology. Surv Ophthalmol 2004;49:51-77
118. Fernandes M, Sridhar MS, Sangwan VS, Rao GN. Amniotic membrane transplantation for ocular surface reconstruction. Cornea 2005;24:643-53
119. Grueterich M, Espana EM, Tseng SC. Ex vivo expansion of limbal epithelial stem cells: amniotic membrane serving as a stem cell niche. Surv Ophthalmol 2003;48:631-46
120. Sippel KC, Ma JJ, Foster CS. Amniotic membrane surgery. Curr Opin Ophthalmol 2001;12:269-81
121. Tseng SC, Espana EM, Kawakita T, et al. How does amniotic membrane work? Ocul Surf 2004;2:177-87
122. Fu Y, Gregory DG, Sippel KC, et al. The ophthalmologist‘s role in the management of acute Stevens-Johnson syndrome and toxic epidermal necrolysis. Ocul Surf 2010;8:193-203
123. Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond) 2005;19:273-8
124. Kheirkhah A, Johnson DA, Paranjpe DR, et al. Temporary sutureless amniotic membrane patch for acute alkaline burns. Arch Ophthalmol 2008;126:1059-66
125. Meller D, Pires RT, Mack RJ, et al. Amniotic membrane transplantation for acute chemical or thermal burns. Ophthalmology 2000;107:980-9; discussion 90
126. Prabhasawat P, Tesavibul N, Prakairungthong N, Booranapong W. Ef-ficacy of amniotic membrane patching for acute chemical and thermal ocular burns. J Med Assoc Thai 2007;90:319-26
127. Tejwani S, Kolari RS, Sangwan VS, Rao GN. Role of amniotic membrane graft for ocular chemical and thermal injuries. Cornea 2007;26:21-6
128. Kheirkhah A, Casas V, Raju VK, Tseng SC. Sutureless amniotic mem-brane transplantation for partial limbal stem cell deficiency. Am J Ophthalmol 2008;145:787-94
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al

THE OCULAR SURFACE / JULY 2011, VOL. 9, NO. 3 / www.theocularsurface.com178
129. Lavker RM, Tseng SC, Sun TT. Corneal epithelial stem cells at the limbus: looking at some old problems from a new angle. Exp Eye Res 2004;78:433-46
130. Liang L, Sheha H, Li J, Tseng SC. Limbal stem cell transplantation: new progresses and challenges. Eye (Lond) 2009;23:1946-53
131. Liang L, Sheha H, Tseng SC. Long-term outcomes of keratolimbal allograft for total limbal stem cell deficiency using combined immu-nosuppressive agents and correction of ocular surface deficits. Arch Ophthalmol 2009;127:1428-34
132. Meller D, Tseng SC. [Reconstruction of the conjunctival and corneal surface. Transplantation of amnionic membrane]. Ophthalmologe 1998;95:805-13. German
133. Sangwan VS, Tseng SC. New perspectives in ocular surface disorders. An integrated approach for diagnosis and management. Indian J Oph-thalmol 2001;49:153-68
134. Tseng SC. Amniotic membrane transplantation for ocular surface reconstruction. Biosci Rep 2001;21:481-9
135. Alio JL, Abad M, Scorsetti DH. Preparation, indications and results of human amniotic membrane transplantation for ocular surface disor-ders. Expert Rev Med Devices 2005;2:153-60
136. Hanada K, Shimazaki J, Shimmura S, Tsubota K. Multilayered amniotic membrane transplantation for severe ulceration of the cornea and sclera. Am J Ophthalmol 2001;131:324-31
137. Espana EM, Di Pascuale M, Grueterich M, et al. Keratolimbal allograft in corneal reconstruction. Eye 2004;18:406-17
138. Solomon A, Ellies P, Anderson DF, et al. Long-term outcome of kera-tolimbal allograft with or without penetrating keratoplasty for total limbal stem cell deficiency. Ophthalmology 2002;109:1159-66
139. Dua HS, Azuara-Blanco A. Allo-limbal transplantation in patients with limbal stem cell deficiency. Br J Ophthalmol 1999;83:414-9
140. Daya SM, Ilari FA. Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology 2001;108:126-33; discussion 33-4
141. Kim JY, Djalilian AR, Schwartz GS, Holland EJ. Ocular surface recon-struction: limbal stem cell transplantation. Ophthalmol Clin North Am 2003;16:67-77
142. Tsubota K, Satake Y, Kaido M, et al. Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. N Engl J Med 1999;340:1697-703
143. Javadi MA, Jafarinasab MR, Feizi S, et al. Management of mustard gas-induced limbal stem cell deficiency and keratitis. Ophthalmology Mar 2011 [Epub ahead of print]
144. Alio JL, Shah S, Barraquer C, et al. New techniques in lamellar kerato-plasty. Curr Opin Ophthalmol 2002;13:224-9
145. Luengo-Gimeno F, Tan DT, Mehta JS. Evolution of deep anterior lamel-lar keratoplasty (DALK). Ocul Surf 2011;9:98-110
146. Reis A, Birnbaum F, Reinhard T. [Systemic immunosuppressives after penetrating keratoplasty]. Ophthalmologe 2007;104:373-80. German
147. Bigar F, Herbort CP. Corneal transplantation. Curr Opin Ophthalmol 1992;3:473-81
148. Pleyer U. [Immunomodulation in penetrating keratoplasty. Current status and perspectives]. Ophthalmologe 2003;100:1036-44. German
149. Holland EJ, Djalilian AR, Schwartz GS. Management of aniridic kera-topathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology 2003;110:125-30
150. Cauchi PA, Ang GS, Azuara-Blanco A, Burr JM. A systematic litera-ture review of surgical interventions for limbal stem cell deficiency in humans. Am J Ophthalmol 2008;146:251-9
151. Boratynska M, Banasik M, Patrzalek D, Klinger M. Conversion from cyclosporine-based immunosuppression to tacrolimus/mycophenolate mofetil in patients with refractory and ongoing acute renal allograft rejection. Ann Transplant 2006;11:51-6
152. Dua HS, Azuara-Blanco A. Corneal allograft rejection: risk factors, diagnosis, prevention, and treatment. Indian J Ophthalmol 1999;47:3-9
153. Hamrah P. High-risk penetrating keratoplasty. Arch Soc Esp Oftalmol 2005;80:5-7
154. Koay PY, Lee WH, Figueiredo FC. Opinions on risk factors and man-agement of corneal graft rejection in the United Kingdom. Cornea 2005;24:292-6
155. Reinhard T, Mayweg S, Sokolovska Y, et al. Systemic mycophenolate mofetil avoids immune reactions in penetrating high-risk keratoplasty: preliminary results of an ongoing prospectively randomized multicentre study. Transpl Int 2005;18:703-8
156. Richter MN, Wachtlin J, Bechrakis NE, Hoffmann F. Keratoplasty after mustard gas injury: clinical outcome and histology. Cornea 2006;25:467-9
157. Williams RN, Bhattacherjee P. Inhibition of the acute ocular responses to nitrogen mustard by colchicine. Exp Eye Res 1984;39:721-9
158. Gonzalez GG, Gallar J, Belmonte C. Influence of diltiazem on the ocular irritative response to nitrogen mustard. Exp Eye Res 1995;61:205-12
159. Vijayaraghavan R, Sugendran K, Pant SC, et al. Dermal intoxication of mice with bis(2-chloroethyl)sulphide and the protective effect of flavonoids. Toxicology 1991;69:35-42
160. Wormser U, Brodsky B, Reich R. Topical treatment with povidone iodine reduces nitrogen mustard-induced skin collagenolytic activity. Arch Toxicol 2002;76:119-21
161. Wormser U, Sintov A, Brodsky B, Nyska A. Topical iodine preparation as therapy against sulfur mustard-induced skin lesions. Toxicol Appl Pharmacol 2000;169:33-9
162. Vojvodic V, Milosavljevic Z, Boskovic B, Bojanic N. The protective effect of different drugs in rats poisoned by sulfur and nitrogen mustards. Fundam Appl Toxicol 1985;5(6 Pt 2):S160-8
163. Papirmeister B, Gross CL, Meier HL, et al. Molecular basis for mustard-induced vesication. Fundam Appl Toxicol 1985;5(6 Pt 2):S134-49
164. Sosne G, Chan CC, Thai K, et al. Thymosin beta 4 promotes corneal wound healing and modulates inflammatory mediators in vivo. Exp Eye Res 2001;72:605-8
165. Sosne G, Szliter EA, Barrett R, et al. Thymosin beta 4 promotes corneal wound healing and decreases inflammation in vivo following alkali injury. Exp Eye Res 2002;74:293-9
166. Sosne G, Christopherson PL, Barrett RP, Fridman R. Thymosin-beta4 modulates corneal matrix metalloproteinase levels and polymorpho-nuclear cell infiltration after alkali injury. Invest Ophthalmol Vis Sci 2005;46:2388-95
167. Sosne G, Qiu P, Kurpakus-Wheater M. Thymosin beta-4 and the eye: I can see clearly now the pain is gone. Ann N Y Acad Sci 2007;1112:114-22
168. Sosne G, Qiu P, Christopherson PL, Wheater MK. Thymosin beta 4 suppression of corneal NFkappaB: a potential anti-inflammatory pathway. Exp Eye Res 2007;84:663-9
169. Yarmola EG, Klimenko ES, Fujita G, Bubb MR. Thymosin beta4: actin regulation and more. Ann N Y Acad Sci 2007;1112:76-85
170. Sawyer TW, Risk D. Effects of selected arginine analogues on sulphur mustard toxicity in human and hairless guinea pig skin keratinocytes. Toxicol Appl Pharmacol 2000;163:75-85
171. Ghanei M, Shohrati M, Jafari M, et al. N-acetylcysteine improves the clinical conditions of mustard gas-exposed patients with normal pul-monary function test. Basic Clin Pharmacol Toxicol 2008;103:428-32
172. Kumar O, Sugendran K, Vijayaraghavan R. Protective effect of various antioxidants on the toxicity of sulphur mustard administered to mice by inhalation or percutaneous routes. Chem Biol Interact 2001;134:1-12
173. McClintock SD, Hoesel LM, Das SK, et al. Attenuation of half sulfur mus-tard gas-induced acute lung injury in rats. J Appl Toxicol 2006;26:126-31
174. McClintock SD, Till GO, Smith MG, Ward PA. Protection from half-mustard-gas-induced acute lung injury in the rat. J Appl Toxicol 2002;22:257-62
SULFUR MUSTARD-INDUCED OCULAR INJURY / Baradaran-Rafii, et al