sm5 (1)
-
Upload
smitha-kapani-gowda -
Category
Documents
-
view
221 -
download
0
Transcript of sm5 (1)
-
8/12/2019 sm5 (1)
1/13
Host response in aggressiveperiodontitis
CY E L E E KU L K A R N I & DE N I S F. KI N A N E
As a preliminary to discussing the host response in
aggressive periodontitis it is worthwhile considering
briey the classication and presentation of this dis-
ease entity. There are numerous periodontal diseases
that affect children and adolescents. Previous classi-
cation systems dened the common forms of chronic
periodontal diseases by age of onset and named this
group early-onset periodontitis. Classication sys-
tems for periodontal diseases changed in recognition
of the signicant overlap between these categories.
Newer classication systems have reclassied
periodontitis into three major forms: chronic perio-
dontitis; aggressive periodontitis; and necrotizing
periodontitis (38). We now refer to early-onset peri-
odontitis as aggressive periodontitis.
The prevalence of chronic periodontal disease
increases with age, with periodontitis being quite rare
in the
rst three decades of life. Aggressive periodon-titis manifesting in children and adolescents is again
quite uncommon, affecting typically
-
8/12/2019 sm5 (1)
2/13
deciencies in host defenses.
genetic predisposition.
This volume of Periodontology 2000 includes articles
dealing in depth with microbial aspects and genetic
predisposition, and this article will focus on host
defenses and deciencies whilst discussing the
microbial etiology as it initiates disease and the
genetic background to the host-defense deciencies
in general.The term periodontal diseases encompasses the
full spectrum of inammatory periodontal diseases,
from gingivitis to all forms of periodontitis, including
chronic, aggressive and necrotizing forms. The Euro-
pean Workshop in Periodontology (32) declared gin-
givitis and periodontitis as a continuum of the same
chronic inammatory condition that affects the
supporting structures of the teeth (32). It was previ-
ously believed that gingivitis was an inevitable conse-
quence of microbial plaque accumulation on the
teeth; however, it is now recognized that inherent
patient susceptibility plays a large role in the expres-
sion of gingivitis and its progression to periodontitis.
Gingivitis occurs in a signicant percentage of the
population, whereas advanced chronic periodontitis,
leading to multiple tooth loss, develops in only a frac-
tion of the population (1015%) (30). The progression
of gingivitis to periodontitis is thought to be inu-
enced by the individuals immune and inamma-
tory responses. Chronic periodontitis and aggressive
periodontitis are among the more signicant of the
periodontal diseases as they result in tooth loss but,
given the progression from gingivitis to periodontitis,prevention of gingivitis may be more important than
previously thought.
Concept of susceptibility
Differences among individuals in the response to
bacterial plaque may be a result of variation in host
susceptibility, with some individuals being very
susceptible and developing aggressive forms of peri-
odontitis at a relatively young age, whilst others might
be resistant and will never develop periodontitis (36).The majority of the population falls within this range
and will develop a degree of gingival inammation
and possibly some periodontal disease over time
when exposed to bacterial plaque. The rate at which
this develops can vary between individuals, with
some experiencing a slow progressing disease over
the course of a lifetime and others developing more
rapid and severe periodontal tissue destruction
resulting in tooth loss. It has been suggested that an
excessive host immune response to the periodontal
microora may also be partly responsible for varia-
tion in the disease response but so far this has not
been well supported by scientic research. An exces-
sive monocyte/macrophage response can be found in
patients with periodontitis compared with subjects
with no periodontitis (22, 61). Engebretson et al. (18)
have shown that periodontal indices are strongly cor-
related with the levels of inammatory cytokines ingingival crevicular uid. However, thus far these
inammatory markers have not shown diagnostic
utility, and a better understanding of the host-
response processes is needed to furnish better diag-
nostic aids for clinical application.
Numerous etiological factors are responsible for
the ultimate expression of periodontal disease.
Clearly, bacterial plaque accounts for only a portion
of the risk of an individual and therefore other
factors must also be considered, including host
factors, environmental factors and genetic factors.
Each component modies the individuals manifesta-
tion of the severity and progression of periodontal
diseases.
Susceptibility to gingivalinammation
Susceptibility to gingivitis is supported by literature
showing that subjects have a highly variable rate of
development of gingivitis. Weidmann et al. (75)
reported a group of 62 subjects in whom a wide rangeof host responses occurred after withdrawal of oral
hygiene measures for 21 days; a susceptible group
who exhibited signicant gingival inammation
within 14 days; and an intermediate group (the
majority) who developed gingival inammation by
day 21. This separation of resistant and susceptible
individuals has been observed in several studies (1,
41, 42) with an across-studies estimate indicating
that this resistant group makes up 13% of subjects.
Trombelli et al. (73) and Engebreton et al. (18) have
shown that there are interindividual differences in
the response to dental plaque in gingivitis studies. Allsubjects expressed some gingivitis, but some devel-
oped much more severe and rapid inammation.
These interindividual differences may be explained
by genetics or environmental factors but preliminary
genetic evidence supports the possibility that there
are interindividual differences in the ability to
develop gingival inammation and showed that spe-
cic genetic characteristics (for example interleukin-
1 polymorphisms) may contribute to exacerbated
Kulkarni & Kinane
80
-
8/12/2019 sm5 (1)
3/13
gingival inammation in response to plaque accu-
mulation. The relationship between an individuals
susceptibility to gingivitis and their susceptibility to
the development of periodontitis is currently
unclear. Those who develop excessive gingivitis may
also be expected to be prone to developing aggres-
sive periodontitis. However, clinically, subjects with
aggressive periodontitis appear to have dispropor-
tionately low levels of bacterial plaque and inam-mation relative to the degree of periodontal
destruction. In the case of smokers, there are simi-
larly low levels of gingival inammation, presumably
owing to the restriction of blood ow, and yet a high
level of periodontal disease. In smokers, environ-
mental factors play a role in masking the presence of
gingivitis and in the aggravation of periodontal dis-
ease. This begs the question: is there a link between
gingivitis susceptibility and periodontitis in which
environmental or other risk factors play a role in
modifying the connection or are the two completely
independent entities with distinct etiologies?
Numerous studies have shown genetic modulation
in the susceptibility of an individual to develop
gingivitis but how this relates to periodontitis is yet
to be determined. For the clinician, the ability to
determine a patients susceptibility, either through
genetic markers or otherwise, may play a major role
in determining a course of treatment. For example,
in a susceptible child or adolescent undergoing
orthodontic treatment it can be expected that gingi-
vitis will occur much more rapidly or severely than
in other patients and thus a more rigorous recallschedule may be warranted for this patient. Or per-
haps in a patient requiring a crown, the practitioner
may opt to alter the nish line to be supragingival to
prevent an unwanted localized inammatory
response in a patient who is susceptible to gingivitis
compared with one who is resistant.
In contrast to gingivitis, susceptibility to advanced
periodontitis with multiple tooth-loss is seen in only
a subset of the population (1015%) (6). It is vari-
able in that it does not affect all teeth to the same
extent, but has both a subject and a site predilec-
tion. Aggressive periodontitis is most commonwithin the rst three decades of life and, speci-
cally, localized aggressive periodontitis is typically
localized to the permanent rst molars and incisors
and often occurs circumpubertally. Retrospective
data in some studies of patients with localized
aggressive periodontitis have suggested that bone
loss in the primary dentition may be an early sign
of disease (63). The review on genetics in this vol-
ume of Periodontology 2000 may give a more com-
plete understanding of genetic susceptibility as it
pertains to clinical disease entities but at the same
time there is considerable complexity in that sus-
ceptibility to gingivitis may be related to susceptibil-
ity to aggressive or chronic periodontitis and our
clear ability to diagnose and categorize disease ef-
ciently will impact on our ability to discover and
prove underlying genetic causes.
Risk factors
The presence of a risk factor implies a direct
increase in the probability of a disease occurring.
Periodontal disease is considered to have multiple
risk factors (4). The term risk factor refers to an
aspect of personal behaviour or lifestyle, an envi-
ronmental exposure, or an inborn or inherited char-
acteristic, which on the basis of epidemiological
evidence is known to be associated with a health
related condition. Risk factors are part of the causal
chain for a particular disease or can lead to expo-
sure of the host to a disease. In periodontal disease
there are numerous pathogens that have been iden-
tied as potential key risk factors; however, it has
become clear that although necessary, the presence
of the pathogens is not sufcient for disease to
occur. The presence of microorganisms is a crucial
factor in inammatory periodontal disease, but the
progression of the disease is related to host-based
risk factors. Aggressive periodontal disease is a mul-
tifactorial process that results from a combination ofgenetic, environmental, host and microbial factors
(37).
Specic inammatory and immuneprocesses in periodontal disease
Variation in susceptibility to periodontitis is well rec-
ognized. However, the pathological basis of this
range of disease expression is poorly understood. In
particular, despite the availability of signicant infor-
mation regarding the inammatory and immuneprocesses involved in periodontitis, the differences
between the pathology of chronic periodontitis vs.
aggressive periodontitis have not been clearly identi-
ed. Thus, the task of deriving clinically important
messages is unpromising from the outset. In contrast
to gingivitis, the host response in periodontal disease
produces plasma-cell-dominated lesions. Genetic
and environmental factors modify and affect the
host response; however, it has yet to be determined
Aggressive periodontitis host factors
81
-
8/12/2019 sm5 (1)
4/13
how, and to what degree, these factors inuence
immune and inammatory processes. Aspects of the
inammatory and immune processes both
humoral and cellularwhich develop in response to
the microbial insult from dental plaque could be
important areas for therapeutics and diagnostics in
the future but are currently too poorly understood
to be of use. Whilst some inammatory and immune
responses are expected in the presence of a micro-bial biolm, the excessive plasma-cell inltrate seen
in periodontitis may be illustrative of an individuals
inability to defend against periodontal pathogens
and thus may indicate a predisposition to periodon-
titis. However, short of excising tissue we have little
way of utilizing this information diagnostically and
prognostically.
Bacterial risk factors
Examples of microbes implicated as risk factors in
periodontitis are numerous. Carlos et al. (12) found
that the presence ofPrevotella intermedia, along with
gingival bleeding and calculus, was correlated with
attachment loss in a group of Navajo adolescents,
1419 years of age. Grossi et al. (26) found that Por-
phyromonas gingivalisand Tannerella forsythiawere
associated with increased risk for attachment loss as a
measure of periodontal disease, after adjustment for
age, plaque, smoking and diabetes. The problem with
these types of microbial disease-association studies is
that the microbial plaque microbiome which is impli-cated in initiating disease has a vast and varied num-
ber of microorganisms (21), possibly also including
viruses and even, in some cases, protozoa.
In the past, the predominant microorganism found
in localized aggressive periodontitis was reported as
A. actinomycetemycomitans, but the supporting litera-
ture does not survive close scrutiny and in the paper
by Faveri et al. (20) the level ofA. actinomycetemyco-
mitans was below the detection limit of their well-
conducted study. Multiple studies showed markedly
elevated levels of serum antibody to A. actinomycete-
mycomitansin patients with localized aggressive peri-odontitis (7, 16, 43). In patients with localized
aggressive periodontitis who were treated success-
fully, there was signicant reduction or elimination
of A. actinomycetemycomitans. In those who failed
treatment, persistent levels ofA. actinomycetemycom-
itanswere found in the affected sites (47, 58). The rea-
son for this nding may be explained by the presence
of antibodies that are cross-reactive across gram-neg-
ative species, and therefore although the titers of anti-
body to A. actinomycetemycomitans were reduced,
this was a reection more of a broad reduction in
antibody titers against gram-negative anaerobic rods
than specic support for the importance of one par-
ticular bacterium over the many others in the oral
microbial biolm relevant to periodontal disease.
An important aspect of any pathogens ability to
affect a host is its virulence factor. A. actinomycete-
mycomitans has been shown to produce a leuko-toxin an exotoxin with the primary toxic effect of
leukocyte destruction, specically of polymorpho-
nuclear neurophils of the host (65, 79). This quality
has been regarded as one of the key reasons for
this species predominance in localized aggressive
periodontitis. Despite these compelling studies, the
idea that A. actinomycetemycomitans is the causa-
tive agent of localized aggressive periodontitis has
not gone undisputed. Numerous studies have
shown that although highly prevalent in most cases
of localized aggressive periodontitis, A. actinomycet-
emycomitans is not present in all cases of localized
aggressive periodontitis. Several cross-sectional
studies (13, 17, 25, 49, 75) showed that there is a
generally high prevalence of A. actinomycetemycom-
itans in many populations, particularly in develop-
ing countries. Studies have also indicated that
A. actinomycetemycomitans has been detected in
subgingival plaque in the absence of localized
aggressive periodontitis. Conversely, there have also
been reports of patients with localized aggressive
periodontitis without detectable A. actinomycetemy-
comitans, and in the comprehensive molecularstudy of the aggressive periodontitis microbiome
performed by Faveri et al. (20) they could not
detect A. actinomycetemycomitans and dismissed it
as a relevant microorganism in their population.
Clearly, A. actinomycetemycomitans has, in the past,
been considered to play an important role in local-
ized aggressive periodontitis but this is question-
able in non-black populations and calls into
question the clinical recommendation to use tetra-
cycline in the treatment of aggressive periodontitis
and the clinical relevance of the extensive studies
on leukotoxin and cytolethal distending toxin.The inammatory and immune responses in the
gingival pocket of periodontal patients are presumed
to be initiated and perpetuated by gram-negative
anaerobic rods and spirochetes. Knowledge of the
causal bacteria in periodontitis, other than the appre-
ciation that a biolm containing predominantly
gram-negative anaerobic rods and anaerobic spiro-
chetes pertains, does not as yet help in the manage-
ment of periodontitis other than suggesting that if an
Kulkarni & Kinane
82
-
8/12/2019 sm5 (1)
5/13
-
8/12/2019 sm5 (1)
6/13
Genco (64), Tanner et al. (71) and recently Dewhirst
and colleagues (15) identied several gram-negative
bacterial species as putative pathogens in oral tissue
destruction.
Innate immunity to oral pathogens
Theeld of innate immunity has mushroomed during
the past decade, mainly because of the identication
of pathogen-recognition receptors and mechanisticcellular signaling pathways related to it. Several of
these pathogen-recognition receptors have been
identied and characterized, including toll-like
receptors, Nod-like receptors, RIG-like receptors and
dectins as pathogen sensors (50). More recently,
co-operation between different receptors (including
chemokine receptors, integrins, G-protein coupled
receptors and the complement system) and their cel-
lular signaling pathways in recognizing pathogens
and mounting an innate immune response, particu-
larly to oral pathogens have been elucidated (19). In
the context of polymicrobial infection, the immune
response triggered may be a result of the simulta-
neous activation of several cellular signaling path-
ways and it is unlikely that a signaling pathway is
activated in isolation. All of these pathways and
receptors may have a critical role in the etiology of
aggressive periodontitis and, similarly, variations in
these molecules may be induced by genetic variants
that might be the critical predisposing genetic factors
in aggressive periodontitis hereditability. Thus, they
are worthy of study.
Toll-like receptors are among the most studiedpattern-recognition receptors as a result of their role
in detecting varied pathogen-associated molecular
patterns. So far, 10 human toll-like receptors have
been identied with the ability to recognize specic
microbial structures (31). Specically, toll-like recep-
tor 4 recognizes the lipopolysaccharide of gram-
negative bacteria, and toll-like receptor 2 forms
heterodimers with toll-like receptor 1 or toll-like
receptor 6 and recognizes peptidoglycan, lipopeptide
and lipoproteins. Double-stranded RNA is recognized
by toll-like receptor 3, whereas toll-like receptor 5 can
detect bacterial agellin. Toll-like receptor 7, toll-likereceptor 8 and toll-like receptor 9 recognize bacterial
and viral molecules. Once these receptors, with the
help of co-receptors or adaptor molecules, recognize
pathogen-related biomolecules, several intracellular
signaling events occur, leading to the production of
inammatory cytokines, antimicrobial peptides, co-
stimulatory molecules, type I interferons and chemo-
kines to mount the innate immune response (11).
Any of these defensive response molecules could be
defective and be part of the specic susceptibility
associated with aggressive periodontitis [see Fig. 1
(10)].
The innate immune response is also critical in acti-
vating antigen-presenting cells and thus in stimulat-
ing the adaptive immune responses. Polymicrobial
infection seems to be much more complicated, in
terms of cellular activation, than originally thought
and again this complicates our understanding of theetiology and susceptibility in aggressive periodontitis.
Considering the diversity of microorganisms in bio-
lm colonization, activation of multiple signaling
pathways simultaneously seems to be relevant in
polymicrobial-related persistent inammation, as in
aggressive periodontitis.
Thus, the role of innate immune cells is generally to
detect microbes and maintain hostmicrobe immune
homeostasis and to induce antimicrobial defense
mechanisms. Innate immune cells, such as epithelial
cells, broblasts, dendritic cells, macrophages and
neutrophils, act as the rst line of defense against
invading pathogens and, through the actions of anti-
gen-presenting cells (dendritic cells and macro-
phages), mount an adaptive immune response. Of
these cells, the most discussed in the context of the
etiopathology of aggressive periodontitis is the poly-
morphonuclear neutrophil. A large body of literature
in the 1970s and 1980s supported the concept of pre-
disposition to juvenile periodontitis (as it was then
called) as a result of a polymorphonuclear neutrophil
chemotactic defect (24). Kinane et al. (33, 34) per-
formed an extensive study of polymorphonuclearneutrophil chemotaxis from a series of these patients
with aggressive periodontitis and found not only no
defect, but rather an overactivation of these cells in
the peripheral blood of patients with aggressive
periodontitis. Thus, although polymorphonuclear
neutrophils are critical in the defense of the peri-
odontium, as evidenced by the rapid destruction in
conditions such as leukocyte adhesion deciency, a
neutrophil chemotactic defect does not appear to be
the key mechanism. There are, however, systemic dis-
eases, in addition to leukocyte adhesion deciency,
which have defective polymorphonuclear neutrophilsas a result of the absence of a crucial trafcking mole-
cule. Such diseases include PapillonLefevre syn-
drome, in which a neutrophil antimicrobial molecule,
cathepsin C, is missing and this renders the patient
also susceptible to an early-onset form of periodontitis,
which is similar to, but different from, aggressive peri-
odontitis (37). Clearly, researchers attempting to uncover
the genetic etiology of aggressive periodontitis have
researched, and continue to research, these promising
Kulkarni & Kinane
84
-
8/12/2019 sm5 (1)
7/13
molecules and pathways in the search for the underlying
genetic predisposition to aggressive periodontitis.
Immune responses
Even in a state of general health, periodontal tissues
will almost always exhibit a degree of leukocyte inl-
trate because of the constant pressures of microbial
biolm and deposits adjacent to tissues. In a state ofdisease the tissues of the periodontium show
increased tissue turnover and cellular activity associ-
ated with inltrating inammatory cells (54). It has
been suggested in the literature that signicant num-
bers of B-cells and T-cells accumulate in these tissues;
however, the functions of these cells in the periodon-
tal-disease process in not well understood.
Literature describing the host response, at a cellular
level, in periodontal disease is often fraught with con-
tradictory remarks including periodontitis is a B-cell
lesion and the immunoregulatory role of T-cells in
periodontitis (46, 51, 52, 59). These observations are
often a result of immunohistochemical methods used
to determine lymphocyte subsets. While specic
observations are noted using these methods, the
inter-relationship between various types of cells can-
not be directly elucidated. For example, while T-cells
are implicated in immunoglobulin synthesis in vitro
(29, 51, 53), the results of these studies do not easilyextrapolate to in-vivo situations where complex
interactions between a variety of inltrated inamma-
tory cells occur. In these studies it is often difcult to
assess the role of the different cell types based on lim-
ited observations and immunochemical analysis, and
so the true function and inter-relationship between
the various types of cells often remains unknown.
Data suggest that both B-cells and T-cells are long
lived in gingival tissues and in periodontal granula-
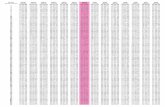
Fig. 1. A simplied signaling cascade in the oral biolm,
activated by toll-like receptors and by the toll-like receptor
cross-talk pathway. Cellular signaling to oral biolms may
activate several unidentied pathways, leading to the release
of cytokines, chemokines, interferon and antimicrobial pep-
tides. These released molecules amplify the inammation
and help to kill the bacteria of the biolm, and also aid in
the recruitment of phagocytes to perform this task and ulti-
mately aid in the restoration of homeostasis to the recovered
tissues. Adapted from Benakanakere & Kinane (10). cAMP,
cyclic AMP; CXCR, CXC chemokine receptor; EDGR, epider-mal growth factor receptor; IL, interleukin; iNOS, inducible
nitric oxide synthase; IPAF, ICE protease-activating factor;
IRF, interferon regulatory factor; mTOR, mammalian target
of rapamycin; MyD88, myeloid differentiation primary
response gene (88); NALP, NALP inammasome; NF-jB,
nuclear factor-kappaB; NOD, nucleotide oligomerization
domain; PAR, protease-activated receptor; PI3K, phospho-
inositide 3-kinase; PKA, protein kinase A; RIG-1/MDA5, reti-
noid-inducible gene 1/melanoma differentiation-associated
protein 5; S1P, sphingosine-1-phosphate; Sphk1, sphingo-
sine kinase 1; TNFR, tumor necrosis factor receptor; TLR,
toll-like receptor; TRIF, TIR-domain-containing adapter-inducing interferon beta.
Aggressive periodontitis host factors
85
-
8/12/2019 sm5 (1)
8/13
tion tissues. These cells probably have the ability to
migrate between blood and lymph pathways in order
to participate in the immune response (39). This is
supported by the ndings that: (i) CD5-positive B-
cells are present in the gingiva at higher proportions
than in the blood(68); (ii) activated B-cells are present
in the periodontium(76); and (iii) CD5-positive B-cells
do not proliferate (2).
T-cells behave as a double-edged sword; whilstnecessary for host protection from bacterial invasion,
the release of excessive amounts of cytokines from T-
cells will result in damage to the host because of their
tissue-degradative properties. The function of the T-
cell in a lesion can be determined by the cytokines
that they release. T-helper (CD4+) cells can be catego-
rized into three subgroups based on their cytokine
prole: T-helper 1 cells (which secrete interleukin-2,
interleukin-12, tumor necrosis factor alpha and inter-
feron gamma); T-helper 2 cells (which secrete inter-
leukin-4, interleukin-5, interleukin-6, interleukin-10
and interleukin-13); and T-helper 17 cells (which
secrete interleukin 17 and are transforming growth
factor beta-related) (27). Numerous studies have
focused on the roles of these T-cells, particularly T-
helper 1 cells and T-helper 2 cells, in the periodon-
tium. Recent studies suggest that whilst both T-helper
1 cells and T-helper 2 cells exist in the periodontium,
T-helper 2 cells are more abundant than T-helper 1
cells in periodontal-disease sites (9, 23, 40, 48, 62, 78).
Recent studies conrm that cytokines from both T-
helper 1 cells and T-helper 2 cells are found in peri-
odontitis gingiva and granulation and that T-helper 2cells outnumber T-helper 1 cells. In particular, inter-
leukin-10, an anti-inammatory cytokine, is found in
abundance in periodontal lesions. The role of T-
helper 1 cells and T-helper 2 cells, as well as the
importance of the presence of various proinamma-
tory and anti-inammatory cytokines, is still unclear.
The possibility that the population of inltrative cells
and the types of cytokines change over the progres-
sion of the disease has been considered and, if this
concept can be further dened, could be very valu-
able in identifying the prognosis of early lesions and
susceptible individuals (21, 45, 56, 57, 60, 77).
Differences in chronic andaggressive periodontitishistopathology
In both chronic periodontitis and aggressive peri-
odontitis the cytokine proles are similar in dis-
eased tissues (57). Increased numbers of T-cells and
decreased numbers of macrophages have been
found in aggressive periodontitis compared with
chronic inammatory periodontal disease (15). It is
difcult to assess the importance of these similari-
ties because it is possible that there are temporal
changes in the prole as the disease progresses
from an early stage to a more advanced stage. Typi-
cally, only the chronic stages of disease have been
assessed, so it is possible that earlier stages mayshow a variation in cellular or cytokine proles.
These differences may also be associated with
genetic variation between subjects who have aggres-
sive periodontitis compared with those who develop
chronic periodontitis. Other considerations, includ-
ing the presence or absence of certain microorgan-
isms and the severity and duration of the disease,
may also affect cell populations.
In the progression from gingivitis to periodontitis
there is a distinct shift from a primarily T-cell lesion
to a B-cell lesion (60). There has been some consider-
ation regarding whether the progression of early
periodontal lesions to more advanced stages involves
a similar shift from cell-mediated immunity to
humoral immunity. Thus far the evidence has been
circumstantial, but the concept of this shift suggests
that T-cells may determine an individuals suscepti-
bility to advanced and possibly aggressive forms of
periodontal diseases.
The humoral immune response to
periodontal pathogensAntibodies to all known periodontal pathogens are
present in both gingival crevicular uid and serum.
The titers of these antibodies have been measured
in patients with disease and in those who have
recovered from disease. The pattern of antibody
titers appears to vary between individuals. However,
titers typically increase immediately after therapy
and then decrease thereafter, an indication of a
favorable response. Several theories have been pro-
posed regarding the interpretation of the antibody
response. A high titer could presumably indicate apositive immune response and thus an appropriate
ability to attack and remove the pathogen. On the
other hand, a high titer could be caused by the
bodys inability to remove the pathogenic source
and thus to overproduce the antibody. There is sig-
nicant interindividual variation in the antibody
response; whether this response is related to indi-
vidual genetic inuences is yet to be seen. If a cor-
relation is determined to exist, this may be a crucial
Kulkarni & Kinane
86
-
8/12/2019 sm5 (1)
9/13
way in which genetics and periodontal diseases are
linked (70).
Deciencies in host defenses
Particularly in the diagnosis of cases of early-onset
forms of periodontitis, systemic conditions must be
eliminated. Multiple systemic conditions may beassociated with periodontal attachment loss and
bone destruction and these need to be excluded
before a diagnosis of aggressive periodontitis is made.
Aggressive periodontitis ideally should present in
patients with a clear medical history but this is not
always the case and there is always the possibility that
a patient with, for example, leukemia, may also have
aggressive periodontitis, but this clearly complicates
the diagnosis and thankfully is rare. In some cases,
despite the absence of a signicant medical history,
there may still exist an underlying medical problem
(e.g. a polymorphonuclear neutrophil dysfunction)
and aggressive periodontitis-like features may be the
only manifestation of this disturbance. Leukocyte
adhesion deciency and PapillonLefevre syndrome
are two examples where the oral picture is inuenced
by defective leucocyte function and the diagnosis
may be confused with generalized aggressive peri-
odontitis.
During infection, polymorphonuclear neutrophils
move from blood vessels toward a chemotactic
source. In order to traverse the blood vessel, adhesion
molecules are expressed on endothelial cells andpolymorphonuclear neutrophils. This results in a
preponderance of polymorphonuclear neutrophils
within the periodontal tissues during disease, and
close examination of the histopathological features of
periodontal disease indicates that the polymorpho-
nuclear neutrophil is a critical feature of the host
defense; furthermore, in neutropenias or in leukocyte
adhesion deciency where the quantity or function of
the polymorphonuclear neutrophils are impaired,
periodontal destruction is excessive. Thus, polymor-
phonuclear neutrophils have been considered impor-
tant in aggressive periodontitis and it is necessary toevaluate deciencies and abnormalities in polymor-
phonuclear neutrophil function as they will have a
direct connection to effects on the periodontium.
However, this does not mean that we know for de-
nite that aggressive periodontitis is caused by dys-
functional polymorphonuclear neutrophils or even
by other leukocytes.
A high percentage of those with localized aggressive
periodontitis have been reported to show abnormal
chemotaxis. This has not been shown to occur in all
individuals with localized aggressive periodontitis but
there does appear to be a familial aggregation pattern
associated with this defect, suggesting that this may
be an inherited abnormality (24, 33, 34).
As mentioned previously, multiple systemic condi-
tions are associated with early-onset forms of peri-
odontal disease. PapillionLefevre syndrome is
characterized by hyperkeratosis of the palms and ofthe soles of the feet and with severe, aggressive
destruction of the periodontal tissues, resulting in
early tooth loss in both the primary and permanent
dentitions. PapillionLefevre syndrome is a result of
mutations in the cathepsin C gene. This mutation is
inherited in an autosomal-recessive manner. It has
been suggested that polymorphisms in the cathepsin
C gene may be associated with a nonsyndromic type
of aggressive periodontitis. However, despite several
studies this possibility has yet to be seen with consis-
tency.
Genetic predisposition
Aggressive periodontitis is a multifactorial disease
process in which several etiological factors are neces-
sary for clinical presentation. Bacterial and host
defenses clearly play a major role in disease. How-
ever, there is signicant support to show that a
genetic component exists in the pattern of disease
presentation within families. This has a major impli-
cation in the method in which aggressive periodonti-
tis is screened for by the practitioner. Oncediagnosed, the siblings of the child or adolescent
should also be screened.
Although bacterial invasion of the periodontal
pocket and a host immune response to the spe-
cies is necessary in the pathogenesis of periodon-
tal disease, it does not fully explain the variation
in the degree to which the disease process is
expressed in some individuals compared with oth-
ers with similar risk factors. Additionally, the
familial aggregation of cases of aggressive peri-
odontitis indicates that there may be a signicant
genetic component involved in the susceptibilityto this disease. Genetic studies in families with
aggressive periodontitis show an inheritance pat-
tern consistent with a gene of major effect. In
some cases the likelihood of a sibling having the
condition was as high as 50%. However, many of
these studies have been limited to African-Ameri-
can populations, so other patterns of inheritance
may exist in different populations. It is more likely
that aggressive periodontitis is caused by a num-
Aggressive periodontitis host factors
87
-
8/12/2019 sm5 (1)
10/13
ber of polymorphisms resulting in a similar clinical
appearance.
Pathology
Aggressive periodontitis presents very similarly to
chronic periodontitis but with some key exceptions.
As mentioned previously, there may be a dispropor-tionate amount of microbial deposits compared with
the level of tissue destruction. Additionally, in local-
ized aggressive periodontitis the areas of disease
will be limited to the incisors and the rst molars.
This localization suggests that the disease itself may
be limited in some way, either by local factors or by
age.
The most frequently affected teeth the molars and
the incisorsare the rst teeth to erupt into a mixed
dentition and this pattern may be important in the
disease process. In a typical eruption pattern the
incisors and the molars erupt in children of 6
8 years
of age. There is then a gap for approximately 12 years
before the remaining teeth erupt into the mouth
until a permanent dentition is reached by the age of
1214 years. The fact that the disease limits itself to
only the rst set of teeth may suggest that tolerance
develops to the pathogenic cause over time.
Other conditions affecting children and adoles-
cents, such as juvenile arthritis and juvenile discitis,
are time limited. These children outgrow the condi-
tions as adults. The temporality of aggressive peri-
odontitis in some patients may be caused by similarprocesses in which there is an immunological toler-
ance over time to the source or a burnout of the
lesion, resulting in a self-limiting pattern.
Relevance of the host response indiagnosis and therapy
Clinical diagnosis is the primary method by which
aggressive periodontitis is recognized but may be
supplemented with microbiological and family segre-
gation analysis. Ideally we would have a genetic diag-nostic test but this has so far been elusive and it may
be that a haplotype or group of polymorphisms may
be what genetically predisposes to aggressive peri-
odontitis. Because of the rare, yet potentially serious,
consequences of early onset forms of periodontitis,
early recognition and diagnosis is very important (3).
A thorough periodontal examination is necessary
for the diagnosis of aggressive periodontitis. Because
of the rarity of the condition it is not practical to com-
plete a thorough periodontal examination for every
child or adolescent. However, patients should be rou-
tinely screened for periodontal disease and a more
comprehensive periodontal examination would be
warranted if screening suggests that periodontal dis-
ease could be present.
In many cases of aggressive periodontitis there is a
disproportionate amount of disease progression in
comparison with the amount of localized microbialdeposits. Consequently, there may be little clinically
visible sign of disease, particularly in the early stages.
Bitewing radiographs are routinely taken in children
and adolescents and may be used for initial screening
purposes. Once aggressive periodontitis is suspected
a comprehensive periodontal examination should be
completed.
Given the high incidence of aggressive periodontitis
in families, all siblings, parents and offspring should
also be screened for the condition, as there is 50%
likelihood that the disease will be present. Although
the disease may not be identical, it is important to fol-
low patients who show even minor levels of involve-
ment as this may represent the early stages of disease.
Treatment of aggressive periodontitis can be chal-
lenging. Successful treatment is associated with early
diagnosis, elimination of the infectious organism and
maintenance. Treatment with conventional debride-
ment alone has not been shown to be effective in the
long-term elimination of aggressive periodontitis.
Antibiotic as an adjunct to debridement has been
suggested for treatment. Treatment may be empiric,
or microbiological testing may be used for selectionof appropriate antibiotics. Evidence in the literature
suggests that the use of metronidazole plus amoxicil-
lin, in combination with mechanical debridement, is
very effective in chronic periodontitis and would also
be useful in aggressive periodontitis in most cases.
Other regimens have been tested, including the use of
tetracycline, but this was based on the poorly
supported contention that this disease was pre-
dominantly caused by A. actinomycetemycomitans, a
facultative anaerobe that would need an antibiotic
capable of killing aerobes and anaerobes.
Conclusions
Aggressive periodontitis affects a small, but signi-
cant, percentage of the population. Because of the
rapidly progressing and aggressive nature of the dis-
ease process these patients require early diagnosis
and treatment in order to prevent further tissue dam-
age and tooth loss. The role of the practitioner is not
Kulkarni & Kinane
88
-
8/12/2019 sm5 (1)
11/13
only to treat those who already present with signi-
cant disease but to prevent and educate those who
are at high risk.
Numerous factors play a role in aggressive peri-
odontitis. Bacterial factors are well recognized as a
key factor in the pathology of periodontitis; however,
as described previously in this article, evidence to
prove that a single pathogen,A. actinomycetemycomi-
tans, is the universial primary etiology for disease isunsupported. Similarly, although host factors can also
play an enormous role in the progression of disease,
polymorphonuclear neutrophil dysfunction does not
appear to be a cause for aggressive periodontitis in
nonsyndromic individuals.
The knowledge of genetic factors may be one of the
most important aspects in the early detection of dis-
ease. Because of the high level of familial aggregation
it behooves the practitioner to screen all siblings and
family members of an affected individual.
References
1. Abbas F, Van der Velden U, Hart AA, Moorer WR, Vroom
TM, Scholte G. Bleeding/plaque ratio and the development
of gingival inammation. J Clin Periodontol 1986: 13: 774
782.
2. Abe M, Tominaga K, Wakasa H. Phenotypic characterization
of human B-lymphocyte subpopulations, particularly human
CD5+ B-lymphocyte subpopulation within the mantle zones
of secondary follicles.Leukemia1994:8: 10391044.
3. Albandar JM. Aggressive periodontitis: case denition and
diagnostic criteria.Periodontol 20002014:65: 1326.
4. Albandar JM. Global risk factors and risk indicators for peri-odontal diseases.Periodontol 20002002:29: 177206.
5. Albandar JM, Brown LJ, Loe H. Putative periodontal patho-
gens in subgingival plaque of young adults with and without
early-onset periodontitis.J Periodontol1997:68: 973981.
6. Albandar JM, Brunelle JA, Kingman A. Destructive peri-
odontal disease in adults 30 years of age and older in the
United States, 19881994.J Periodontol1999:70: 1329.
7. Albandar JM, DeNardin AM, Adesanya MR, Diehl SR, Winn
DM. Associations between serum antibody levels to peri-
odontal pathogens and early-onset periodontitis. J Period-
ontol2001:72: 14631469.
8. Albandar JM, Tinoco EM. Global epidemiology of periodon-
tal diseases in children and young persons. Periodontol
20002002:29: 153
176.
9. Anderson HH, Rapley JW, Williams DR. Gingival over-
growth with valproic acid: a case report. ASDC J Dent Child
1997:64: 294297.
10. Benakanakere M, Kinane DF. Innate cellular responses to
the periodontal biolm.Front Oral Biol2012:15: 4155.
11. Brown J, Wang H, Hajishengallis GN, Martin M. TLR-signal-
ing networks: an integration of adaptor molecules, kinases,
and cross-talk.J Dent Res2011:90: 417427.
12. Carlos JP, Wolfe MD, Zambon JJ, Kingman A. Periodontal
disease in adolescents: some clinical and microbiologic
correlates of attachment loss. J Dent Res 1988: 67: 1510
1514.
13. Dahlen G, Manji F, Baelum V, Fejerskov O. Black-pig-
mentedBacteroidesspecies and Actinobacillus actinomyce-
temcomitans in subgingival plaque of adult Kenyans.J Clin
Periodontol1989:16: 305310.
14. Danks JA, McHale JC, Clark SP, Chou ST, Scurry JP, Ingleton
PM, Martin TJ. In situ hybridization of parathyroid hormone-
related protein in normal skin, skin tumors, and gynecologi-
cal cancers using digoxigenin-labeled probes and antibody
enhancement.J Histochem Cytochem1995: 43: 5
10.
15. Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner ACR, Yu W-
H, Lakshmanan A, Wade WG. The human oral microbiome.
J Bacteriol2010:192: 50025017.
16. Ebersole JL, Cappelli D, Sandoval MN. Subgingival distribu-
tion of A. actinomycetemcomitans in periodontitis. J Clin
Periodontol1994:21: 6575.
17. Eisenmann AC, Eisenmann R, Sousa O, Slots J. Microbio-
logical study of localized juvenile periodontitis in Panama.
J Periodontol1983: 54: 712713.
18. Engebretson SP, Grbic JT, Singer R, Lamster IB. GCF IL-
1beta proles in periodontal disease. J Clin Periodontol
2002:29: 4853.
19. Eskan MA, Rose BG, Benakanakere MR, Zeng Q, Fujioka D,Martin MH, Lee M-J, Kinane DF. TLR4 and S1P receptors
cooperate to enhance inammatory cytokine production in
human gingival epithelial cells. Eur J Immunol 2008: 38:
11381147.
20. Faveri M, Mayer MPA, Feres M, de Figueiredo LC, Dewhirst
FE, Paster BJ. Microbiological diversity of generalized
aggressive periodontitis by 16S rRNA clonal analysis. Oral
Microbiol Immunol2008:23: 112118.
21. Fujihashi K, Beagley KW, Kono Y, Aicher WK, Yamamoto M,
DiFabio S, Xu-Amano J, McGhee JR, Kiyono H. Gingival
mononuclear cells from chronic inammatory periodontal
tissues produce interleukin (IL)-5 and IL-6 but not IL-2 and
IL-4.Am J Pathol1993:142: 12391250.
22. Garrison SW, Nichols FC. LPS-elicited secretory responsesin monocytes: altered release of PGE2 but not IL-1 beta in
patients with adult periodontitis.J Periodontal Res1989:24:
8895.
23. Gemmell E, Seymour GJ. Gamma delta T lymphocytes in
human periodontal disease tissue. J Periodontol1995: 66:
780785.
24. Genco RJ, Zambon JJ, Murray PA. Serum and gingivaluid
antibodies as adjuncts in the diagnosis of Actinobacillus
actinomycetemcomitans-associated periodontal disease.
J Periodontol1985:56: 4150.
25. Gmur R, Guggenheim B. Interdental supragingival plaque
a natural habitat ofActinobacillus actinomycetemcomitans,
Bacteroides forsythus, Campylobacter rectus, and Prevotella
nigrescens.J Dent Res1994:73: 1421
1428.26. Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Mach-
tei EE, Norderyd OM, Genco RJ. Assessment of risk for peri-
odontal disease. I. Risk indicators for attachment loss.
J Periodontol1994:65: 260267.
27. Hatton O, Phillips LK, Vaysberg M, Hurwich J, Krams SM,
Martinez OM. Syk activation of phosphatidylinositol 3-
kinase/Akt prevents HtrA2-dependent loss of X-linked
inhibitor of apoptosis protein (XIAP) to promote survival of
Epstein-Barr virus+ (EBV+) B cell lymphomas. J Biol Chem
2011:286: 3736837378.
Aggressive periodontitis host factors
89
-
8/12/2019 sm5 (1)
12/13
28. Heller D, Silva-Boghossian CM, do Souto RM, Colombo
APV. Subgingival microbial proles of generalized aggres-
sive and chronic periodontal diseases.Arch Oral Biol2012:
57: 973980.
29. Ito H, Harada Y, Matsuo T, Ebisu S, Okada H. Possible role
of T cells in the establishment of IgG plasma cell-rich
periodontal lesionaugmentation of IgG synthesis in the
polyclonal B cell activation response by autoreactive T cells.
J Periodontal Res1988:23: 3945.
30. Jenkins WM, Kinane DF. The high riskgroup in periodon-
titis.Br Dent J1989:167: 168
171.
31. Kawai T, Akira S. TLR signaling. Semin Immunol 2007: 19:
2432.
32. Kinane DF, Attstrom R. Advances in the pathogenesis of
periodontitis. Group B consensus report of the fth Euro-
pean Workshop in Periodontology. J Clin Periodontol2005:
32(Suppl 6): 130131.
33. Kinane DF, Cullen CF, Johnston FA, Evans CW. Neutrophil
chemotactic behaviour in patients with early-onset forms
of periodontitis (I). Leading front analysis in Boyden cham-
bers.J Clin Periodontol1989:16: 242246.
34. Kinane DF, Cullen CF, Johnston FA, Evans CW. Neutrophil
chemotactic behaviour in patients with early-onset forms
of periodontitis (II). Assessment using the under agarosetechnique.J Clin Periodontol1989:16: 247251.
35. Kinane DF, Hajishengallis G. Polymicrobial infections,
biolms, and beyond.J Clin Periodontol2009:36: 404405.
36. Kinane DF, Hart TC. Genes and gene polymorphisms asso-
ciated with periodontal disease. Crit Rev Oral Biol Med
2003:14: 430449.
37. Kinane DF, Marshall GJ. Periodontal manifestations of sys-
temic disease.Aust Dent J2001:46: 212.
38. Lang NPBP, Cullinam M, Jeffcoat M, Mombelli A, Murakami
S, Page R, Papapanou P, Tonetti M, Van Dyke T. Interna-
tional classication workshop. Consensus report: aggressive
periodontitis.Ann Periodontol1999:4: 53.
39. Lappin DF, Koulouri O, Radvar M, Hodge P, Kinane DF.
Relative proportions of mononuclear cell types in periodon-tal lesions analyzed by immunohistochemistry. J Clin Peri-
odontol1999:26: 183189.
40. Lappin DF, MacLeod CP, Kerr A, Mitchell T, Kinane DF.
Anti-inammatory cytokine IL-10 and T cell cytokine pro-
le in periodontitis granulation tissue. Clin Exp Immunol
2001:123: 294300.
41. Lie MA, Danser MM, van der Weijden GA, Timmerman MF,
de Graaff J, van der Velden U. Oral microbiota in subjects
with a weak or strong response in experimental gingivitis.
J Clin Periodontol1995:22: 642647.
42. Lie MA, van der Weijden GA, Timmerman MF, Loos BG,
van Steenbergen TJ, van der Velden U. Oral microbiota
in smokers and non-smokers in natural and experimen-
tally-induced gingivitis. J Clin Periodontol 1998: 25:677686.
43. Listgarten MA, Wong MY, Lai CH. Detection ofActinobac-
illus actinomycetemcomitans, Porphyromonas gingivalis,
and Bacteroides forsythus in an A. actinomycetemcomi-
tans-positive patient population. J Periodontol 1995: 66:
158164.
44. Loe H, Theilade E, Jensen SB. Experimental Gingivitis In
Man.J Periodontol1965:36: 177187.
45. Lundqvist C, Baranov V, Teglund S, Hammarstrom S, Ham-
marstrom ML. Cytokine prole and ultrastructure of intra-
epithelial gamma delta T cells in chronically inamed
human gingiva suggest a cytotoxic effector function.
J Immunol1994:153: 23022312.
46. Mackler BF, Waldrop TC, Schur P, Robertson PB, Levy BM.
IgG subclasses in human periodontal disease. I. Distribu-
tion and incidence of IgG subclass bearing lymphocytes
and plasma cells.J Periodontal Res1978:13: 109119.
47. Mandell RL, Ebersole JL, Socransky SS. Clinical immuno-
logic and microbiologic features of active disease sites
in juvenile periodontitis. J Clin Periodontol 1987: 14:
534
540.
48. Manhart SS, Reinhardt RA, Payne JB, Seymour GJ, Gemmell
E, Dyer JK, Petro TM. Gingival cell IL-2 and IL-4 in early-
onset periodontitis.J Periodontol1994:65: 807813.
49. McNabb H, Mombelli A, Gmur R, Mathey-Dinc S, Lang NP.
Periodontal pathogens in the shallow pockets of immi-
grants from developing countries. Oral Microbiol Immunol
1992:7: 267272.
50. Medzhitov R. Innate immunity: quo vadis? Nat Immunol
2010:11: 551553.
51. Meng HX, Zheng LF. T cells and T-cell subsets in periodon-
tal diseases.J Periodontal Res1989:24: 121126.
52. Okada H, Ito H, Harada Y. T-cell requirement for establish-
ment of the IgG-dominant B-cell lesion in periodontitis.J Periodontal Res1987:22: 187189.
53. Okada H, Kida T, Yamagami H. Identication and distribution
of immunocompetent cells in inamed gingiva of human
chronic periodontitis.Infect Immun1983:41: 365374.
54. Page RC, Schroeder HE. Pathogenesis of inammatory peri-
odontal disease. A summary of current work. Lab Invest
1976:34: 235249.
55. Paster BJ, Dewhirst FE. Phylogenetic foundation of spiro-
chetes.J Mol Microbiol Biotechnol2000:2: 341344.
56. Roberts FA, McCaffery KA, Michalek SM. Prole of cytokine
mRNA expression in chronic adult periodontitis. J Dent Res
1997:76: 18331839.
57. Salvi GE, Lawrence HP, Offenbacher S, Beck JD. Inuence
of risk factors on the pathogenesis of periodontitis. Period-ontol 20001997:29: 173201.
58. Sandholm L, Tolo K, Olsen I. Salivary IgG, a parameter of
periodontal disease activity? High responders to Actinobac-
illus actinomycetemcomitansY4 in juvenile and adult peri-
odontitis.J Clin Periodontol1987:14: 289294.
59. Seymour GJ, Greenspan JS. The phenotypic characteriza-
tion of lymphocyte subpopulations in established human
periodontal disease.J Periodontal Res1979:14: 3946.
60. Seymour RA, Heasman PA. Tetracyclines in the manage-
ment of periodontal diseases. A review. J Clin Periodontol
1995:22: 2235.
61. Shapira L, Soskolne WA, Sela MN, Offenbacher S, Barak V.
The secretion of PGE2, IL-1 beta, IL-6, and TNF alpha by
adherent mononuclear cells from early onset periodontitispatients.J Periodontol1994:65: 139146.
62. Sigusch B, Klinger G, Glockmann E, Simon HU. Early-onset
and adult periodontitis associated with abnormal cytokine
production by activated T lymphocytes. J Periodontol1998:
69: 10981104.
63. Sjodin B, Matsson L, Unell L, Egelberg J. Marginal bone loss
in the primary dentition of patients with juvenile periodon-
titis.J Clin Periodontol1993:20: 3236.
64. Slots J, Genco RJ. Black-pigmented Bacteroides species,
Capnocytophaga species, and Actinobacillus actinomyce-
Kulkarni & Kinane
90
-
8/12/2019 sm5 (1)
13/13
temcomitans in human periodontal disease: virulence
factors in colonization, survival, and tissue destruction.
J Dent Res1984:63: 412421.
65. Slots J, Rams TE, Schonfeld SE. In vitro activity of chlorhexi-
dine against enteric rods, pseudomonads and acinetobacter
from human periodontitis. Oral Microbiol Immunol 1991:
6: 6264.
66. Socransky SS, Haffajee AD. The bacterial etiology of
destructive periodontal disease: current concepts.J Period-
ontol1992:63: 322331.
67. Socransky SS, Tanner AC, Goodson JM, Haffajee AD, Walker
CB, Ebersole JL, Sornberger GC. An approach to the deni-
tion of periodontal disease syndromes by cluster analysis.
J Clin Periodontol1982:9: 460471.
68. Sugawara M, Yamashita K, Yoshie H, Hara K. Detection of,
and anti-collagen antibody produced by, CD5-positive B
cells in inamed gingival tissues.J Periodontal Res1992:27:
489498.
69. Susin C, Haas AN, Albandar JM. Epidemiology and demo-
graphics of aggressive periodontitis. Periodontol 20002014:
65: 2745.
70. Takahashi K, Mooney J, Frandsen EV, Kinane DF. IgG
and IgA subclass mRNA-bearing plasma cells in periodon-
titis gingival tissue and immunoglobulin levels in thegingival crevicular uid. Clin Exp Immunol 1997: 107:
158165.
71. Tanner ACR, Paster BJ, Lu SC, Kanasi E, Kent R, Van Dyke
T, Sonis ST. Subgingival and tongue microbiota during early
periodontitis.J Dent Res2006:85: 318323.
72. Tonetti MS, Mombelli A. Early-onset periodontitis. Ann
Periodontol1999:4: 3953.
73. Trombelli L, Tatakis DN, Scapoli C, Bottega S, Orlandini E,
Tosi M. Modulation of clinical expression of plaque-
induced gingivitis. II. Identication of high-responder
and low-responder subjects. J Clin Periodontol2004: 31:
239252.
74. Wiedemann W, Lahrsow J, Naujoks R. The effect of peri-
odontal resistance on experimental gingivitis. Dtsch Zah-
narztl Z1979:34: 69.
75. al-Yahfou Z, Mombelli A, Wicki A, Lang NP. The effect of
plaque control in subjects with shallow pockets and high
prevalence of periodontal pathogens. J Clin Periodontol
1995:22: 7884.
76. Yamazaki K, Nakajima T, Aoyagi T, Hara K. Immunohisto-
logical analysis of memory T lymphocytes and activated B
lymphocytes in tissues with periodontal disease. J Periodon-
tal Res1993:28: 324334.
77. Yamazaki K, Nakajima T, Hara K. Immunohistological anal-
ysis of T cell functional subsets in chronic inammatory
periodontal disease.Clin Exp Immunol1995:99: 384391.
78. Yamazaki K, Nakajima T, Kubota Y, Gemmell E, Seymour
GJ, Hara K. Cytokine messenger RNA expression in chronic
in
ammatory periodontal disease.Oral Microbiol Immunol1997:12: 281287.
79. Zambon JJ, Umemoto T, De Nardin E, Nakazawa F, Chris-
tersson LA, Genco RJ. Actinobacillus actinomycetemcomi-
tansin the pathogenesis of human periodontal disease. Adv
Dent Res1988:2: 269274.
Aggressive periodontitis host factors
91