SERAN BI OJ URNAL OF ANESTHEA SI AND INTENSIVE...
Transcript of SERAN BI OJ URNAL OF ANESTHEA SI AND INTENSIVE...


Teh nič ki ured nik / Tech ni cal Edi torMilan Bog da no vić
Izvrš ni izda vač / Exe cu ti ve Publis herUdru že nje ane ste zi o lo ga i inten zi vi sta Srbi je
Dizajn korica / Cover Design Predrag Petković
Prelom i kompjuterska obradaStu dio znak, Ivan ko vač ka 10/2
Otvoreni pristup / Open Access
Adre sa ured niš tva / Edi to rial Offi ceČaso pis SJA IT
Kli ni ka za ane ste zi o lo gi ju i inten ziv nu tera pi juVoj no me di cin ska aka de mi ja, 11000 Beo grad, Crno trav ska 17,
E-mail: jour nal.sja [email protected]
SER BIAN JOUR NAL OF ANEST HE SIA AND INTEN SI VE THE RAPYOffi cial Jour nal of Ser bian Asso ci a tion of Anest he si o lo gists and Inten si vists
Volu me 40; October – December 2018; Issue 7–8
SRP SKI ČASO PIS ANE STE ZI JA I INTEN ZIV NA TERA PI JAČaso pis Udru že nja ane ste zi o lo ga i inten zi vi sta Srbi je
Godiš te 40; Oktobar – Decembar 2018; Broj 7–8
Glav ni i odgo vor ni ured nikEdi tor in Chi ef
Neboj ša Lađe vić
Zame nik ured ni ka / Assi stant Chi ef Edi torDuši ca Sta men ko vić
Sekre tar / Sec re taryGoran Rondović
Ure đi vač ki odbor / Edi to rial Board
Nada Popo vić, SRBRad mi lo Jan ko vić, SRBVoji sla va Neš ko vić, SRBMiodrag Milenović, SRBIva na Budić, SRBMir ko Gra jić, SRBBilja na Sto šić, SRBSve tla na Apo sto lo vić, SRBNemanja Rančić, SRBDragana Unić Stojanović, SRB
Lek tor za srp ski jezikSer bian lan gu a ge edi tor
Mari ja Bog da no vić
Zoka Milan, UKOli ve ra Pot pa rić, UKŽika Petro vić, UKNeboj ša Nick Kne že vić, USAKara ni ko las Mene la os, USAIvan Kan gr ga, USAAndre as Kopf, GER MANYCar sten Ban tel, GR MANYSanja Marić, BIHIvana Likić Lađević, SRB
Mihail Y. Kirov, RUS SIAXavi ar Gar cia Fer nan dez, SPAINZolt Mol nar, HUN GARYSte fan de Hert, BEL GI UMArash Asfa ri, DEN MARKSha ron Einav, ISRAELDani e la Fili pe scu, ROMA NIAMas si mi li a no Sor bel lo, ITALYDan Lan gri os, FRAN CE
Lek tor za engle ski jezikEnglish lan gu a ge edi tor
Milan Miljko vić

SADR ŽAJ CONTENTS
Preoperative high-sensitive troponin t and n-terminal pro b-type natriuretic peptide in prediction of short-term mortality after non-cardiac surgery (high-sensitive troponin t and n-terminal pro b-type natriuretuc peptide in prediciton of mortality after non-cardiac surgery)Nenad Savić, Ilija Golubović, Milena Stojanović, Anita Vuković, Danica Marković, Radmilo Janković 163
Is cesarean myomectomy in patients with large multiple myomas always a hazardous procedure? a case reportRadmila Sparić, Milan Dokić, Ivana Likić Lađević, Dragiša Šljivančanin, Milica Stojičić, Snežana Vidaković 171
Application of cerebral oxymetry in carotid surgery (Cerebral oximetry and carotid surgery)Dragana Unić-Stojanović 177
Lung ultrasound – part two (lung ultrasoind part 2)Marija Milenković, Jovana Stanisavljević, Adi Hadžibegović, Gregor Prosen, Dragan Mašulović Milica Stojadinović 183
Total knee arthroplasty in a patient with severe von willebrand disease (perioperative treatment of von willebrand disease)Lazar Bralušić, Svetlana Dinić, Andrijana Cvijović 193
Izveštaj o XIII Kongesu anesteziologa i intenzivista Srbije I am here / Ja sam ovdeVojislava Nešković 201
5th European Airway Management CongressDušica Stamenković 205
Otežan disajni put – radionicaDušica Stamenković 213
Godište: 40 X-XII 2018 Broj: 7-8 Volume: 40 X-XII 2018 Issue: 7-8
Preoperativno visoko senzitivni troponin t i n-terminal pro b tip natriuretskog peptida u predikciji mortaliteta u kratkom periodu posle nekardiohirurških operacija (visoko senzitivni troponin t i n-terminal pro b tip natriuretskog peptida u predikciji mortaliteta posle nekardiohirurških operacija)Nenad Savić, Ilija Golubović, Milena Stojanović, Anita Vuković, Danica Marković, Radmilo Janković 163
Miomektomija u toku carskog reza kod pacijentkinja sa velikim multiplim miomima: koliki je rizik? prikaz slučaja.Radmila Sparić, Milan Dokić, Ivana Likić Lađević, Dragiša Šljivančanin, Milica Stojičić, Snežana Vidaković 171
Primena cerebralne oksimetrije u karotidnoj hirurgiji (Cerebralna oksimetrija i karotidna hirurgija)Dragana Unić-Stojanović 177
Ultrazvuk pluća – drugi deo (ultrazvuk pluća deo 2)Marija Milenković, Jovana Stanisavljević, Adi Hadžibegović, Gregor Prosen, Dragan Mašulović, Milica Stojadinović 183
Totalna aloartroplastika kolena kod bolesnice sa teškom formom von willebrandove (fon vilebrandove) bolesti (perioperativni tretman kod von willebrandove bolesti)Lazar Bralušić, Svetlana Dinić, Andrijana Cvijović 193
Izveštaj o XIII Kongesu anesteziologa i intenzivista Srbije I am here / Ja sam ovdeVojislava Nešković 201
Izveštaj sa Petog Evropskog kongresa posvećenog disajnom putuDušica Stamenković 205
Otežan disajni put – radionicaDušica Stamenković 213

Original work
PREOPERATIVE HIGH-SENSITIVE TROPONIN T AND N-TERMINAL PRO B-TYPE NATRIURETIC PEPTIDE IN PREDICTION OF SHORT-TERM MORTALITY AFTER
NON-CARDIAC SURGERY (HIGH-SENSITIVE TROPONIN T AND N-TERMINAL PRO B-TYPE NATRIURETUC
PEPTIDE IN PREDICITON OF MORTALITY AFTER NON-CARDIAC SURGERY)
Nenad Savić1, Ilija Golubović2, Milena Stojanović1, Anita Vuković1, Danica Marković1, Radmilo Janković1
1Clinic for anesthesia and intensive therapy, Blvd. dr. Zorana Đinđića 48, Clinical Center Niš, 18000 Niš, Serbia 2Department of General surgery, Clinical Center Niš, Blvd. dr. Zorana Đinđića 81, 18000 Niš, Serbia
Corresponding author: Milena Stojanović, Dr. Milutina Ivkovića 8, 18000 Niš, Serbia, Telephone: +381606240788, E-mail: [email protected]
doi:10.5937/sjait1806117JISSN 2466-488X (Online)
Summary
Background and Aims: The aim of this study was to evaluate potential of prognostic cardiac biomarkers by predicting fatal events during perioperative period and the significance of their increased values in all patients and with coronary artery disease (CAD). Methods: The study included 87 patients who underwent major abdominal and vascular surgery. Blood samples were taken from all patients prior to surgery and levels of high-sensitive troponin T (hsTnT) and N-Terminal Pro B-type natriuretic peptide (NT-proBNP) were measured. It was analyzed how their increased values (above the prede-fined cut-offs of > 14 ng/L and > 300 pg/mL respectively) was associated with perioperative mortality in both all subjects and in patients with CAD. Results: Median value of hsTnT in survival group was 11.29 ng/L (interquartile range – IQR, 6.03–18.57) vs. 26.62 ng/L (IQR, 21.48–76.31) in non-survival group, p = 0.045 and for NT-proBNP in survival group was 259.05 pg/mL (IQR, 93.03–447.45) vs. 759.2 pg/mL (IQR, 433–6095) in non-survival group, p = 0.017. The odds ratio of mortality was presented in the form of direct association for both measured biomarkers - not only in patients with CAD but also in all included patients. Conclusions: Preoperatively increased hsTnT and NT-proBNP indicate high mortality risk during perioperative period. Because of the association between increased cardiac biomarker and mortality events in patients with CAD, special attention is necessary in preparation for major surgery.
Key words: cardiac biomarkers; short-term mortality; perioperative risk; non-cardiac surgery; coronary artery disease
Introduction
Non-cardiac surgery is usually performed on ele-ctive basis. However, this type of surgery can be associated with significant cardiovascular morbi-dity and mortality. One of the most important pre-dictors of complications is Coronary Artery Disea-se (CAD)1,2. When a patient with ischemic cardiac disease undergoes a high-risk surgery, the risk of cardiac complications rises almost tenfold3. There are powerful biomarkers that reflect myocardial injury, specifically heart failure, valvular heart di-sease, as well as CAD. From a group of potential biomarkers, B-type Natriuretic Peptide (BNP) and N-Terminal Pro B-type natriuretic peptide (NT-proBNP), and troponins seem to be the most important4, 5.
Several studies have demonstrated that BNP and NT-proBNP provide strong prognostic infor-mation in both documented cardiovascular pa-tients and apparently healthy individuals6,7. Cardi-ac troponins have also been used for a long time as a golden standard for diagnosing myocardial infarction. However, since the implementation of high-sensitive troponin T (hsTnT) assays, they proved to be useful for the detection of minor car-diovascular injuries and these markers can be used for providing significant prognostic information8, 9.
The aim of this study was to investigate the as-sociation between preoperative levels of hsTnT and NT-proBNP and short-term mortality events in patients who underwent major non-cardiac surgery. Additionally, we performed an analysis to determine the mortality risk in a subgroup of pa-

164 SJAIT 2018/7-8
tients with documented CAD according to cut-offs of these cardiac biomarkers values.
Subjects and methodsThe study was conducted as a single-center,
prospective, observational study. It included 87 pa-tients who underwent major abdominal and vas-cular surgery under general anesthesia. All patients were recruited in 2008 and 2009 at the Department of Surgery, The Clinical Center of Niš. The surger-ies were performed according to clinical standards of our hospital. Besides the type of surgery, other inclusion criteria were age >55 years, and the pres-ence of at least one of cardiovascular risk factors – arterial hypertension, family history of cardiac disease, hyperlipidemia, active smoking status or diabetes mellitus. Inabilities to understand or sign an informed consent as well as emergency surgery, were taken as exclusion criteria.
Each patient had to sign an informed consent that included biomarker analysis. The study was approved by the local Ethical Committee of Clini-cal Center Niš.
Follow-up period for postoperative mortality, as the primary clinical outcome of our study, was within 30 days. All-cause mortality was included following: acute myocardial infarction, ventricu-lar fibrillation, cardiac arrest, cardio-pulmonary resuscitation, and acute cardiac decompensation. Coronary artery disease was defined on the basis of positive laboratory tests, clinical risk factors, prior bypass surgery, coronary intervention or pri-or myocardial infarction. Acute myocardial infarc-tion was diagnosed according to universal defini-tion of myocardial infarction7.
Laboratory analysisBlood samples for laboratory assessment were
taken no more than seven days before the surgery. Immediately after venipuncture from antecubital region, tubes with blood were processed without additives. Prior to analyses, serum was separated and frozen to -70°C. The samples were sent to pre-defined investigating laboratory center at the Uni-versity of Basel, Switzerland.
Cardiac TnT was measured by a newly de-veloped highly-sensitive electrochemilumines-cence-immunoassay (hsTnT) on an Elecsys ana-lyzer (Roche Diagnostics, Mannheim, Germany).
The lower limit of detection for this assay was 3 ng/L, the 99th percentile of a healthy reference pop-ulation was 14 ng/L, and the concentration with a coefficient of variation (CV) of 10% was 13 ng/L. NT-proBNP was measured by an electrochemilu-minescence-immunoassay (ElecsysproBNP, Roche Diagnostics, Mannheim, Germany). The analytical range extended from 5 to 35 000 pg/mL. The total CV was 3.3% (n ¼ 28) at a level of 252.6 pg/mL and 3.7% (n ¼ 25) at a level of 6130.8 pg/mL of NT-proBNP.
Statistical analysisValues are expressed as the mean ± SD (standard
deviation), median with interquartile range, odds ratio (OR) or hazard ratio (HR). Because there was no normal distribution of some variables in the subjects with CAD, differences in survival were tested with the Mann-Whitney U test for indepen-dent samples. Also, Z-test and Students t-test were used as appropriate and Chi-square test was used for categorical variables. Differences of laborato-ry parameter between two groups were assessed with Students t-test and median test. To evaluate test performance for NT-proBNP and hsTnT, an area under the curve (AUC) for the receiver op-erating characteristics (ROC) was calculated. OR and 95% confidence interval (CI) was measured for all patient to determine risk of mortality in re-lation to cut-off values of biomarkers. HR for all variables were analyzed with multivariant Cox re-gression analyses. A value of P ≤ 0.05 was consid-ered statistically significant. Statistical analysis was performed using SPSS software (version 10) and Comprehensive Meta-Analysis (version 3; Biostat Inc, Englewood, NJ).
ResultsOut of 87 patients, 39 (45%) were women.
Mean age of our patients was 68. Nine of all in-cluded patients (10%) had history of CAD. Most of our patients – 65 (75%) underwent abdominal surgery and the rest 22 (25%) had major vascular surgery. Majority of the patients were on cardio-vascular medical treatment and had one or more cardiovascular risk factors. General features of the patients are presented in Table I.
The median value of high-sensitive troponin levels for entire cohort was 11.45 ng/L, with IQR

165NEKRITIČNA PRIMENA NESTEROIDNIH ANTINFLAMATORNIH LEKOVA U TERAPIJI HRONIČNOG NEMALIGNOG BOLA
6.28–19.5, and the median value for NT-proB-NP was 280.3 pg/mL (Interquartile Range - IQR 99.71–450.1). There were statistically significant differences between levels of hsTnT and NT-proB-NP in group of survivors (S) and non-survivors (NS). Median value of hsTnT in S group was 11.29 ng/L (6.03–18.57) vs. 26.62 ng/L (21.48–76.31) in NS group, p = 0.045 and for NT-proBNP in S group was 259.05 pg/mL (93.03–447.45) vs. 759.2 pg/mL (433–6095) in NS group, p = 0.017. Thirty-four of all included patients (39%) in study were with hsT-nT values above 14 ng/L while NT-proBNP values were above 300 pg/mL in 40 patients (41%). Pa-
tients with diagnosed angina pectoris, atrial fibril-lation, diabetes mellitus, as well as active smok-ers, had increased mortality events. Other tested parameters showed no statistical significance for survival.
The OR of mortality was presented in the form of direct association for both measured biomark-ers, not only in patients with CAD, but also in all included patients. The OR in all patients with mea-sured hsTnT was 11.14 (95% CI, 1.28–97.23; p = 0.03), and in patients with CAD was 75.00 (95% CI, 1.15–4868.64; p = 0.04). For all patients with measured NT-proBNP, the OR was 21.27 (95% CI,
Table I: General features
All patients Survivors Deceased p-value survivors vs. deceased
n (%) 87 (100) 80 (92) 7 (8)Gender (female), n (%) 39 (44.83) 37 (46.25) 2 (28.57) 0.178Age (years) ± SD 67.95 ± 7.97 68.04 ± 7.94 67.02 ± 8.88 0.749
BMI (kg/m2) median (IQR) 24.77 (23.091–27.68)
24.80 (2.36–27.68)
22.66 (19.60–27.78) 0.694
CAD, n (%) 9 (100) 7 (8.75) 2 (28.57) < 0.001Dyspnoea, (NYHA II-IV) n (%)1 56 (64.37) 54 (667.5) 2 (28.57)
0.0532 27 (31.03) 22 (27.5) 5 (71.43)3 4 (4.6) 4 (5) 0 (0)Angina pectoris, n (%)1 69 (78.75) 66 (82.55) 3 (42.86)
0.0322 17 (16.25) 13 (16.25) 4 (57.14)3 1 (1.25) 1 (1.25) 0 (0)Atrial fibrillation, n (%) 1 (1.25) 1 (1.25) 0 (0) 0.006Diabetes mellitus, n (%) 25 (31.25) 25 (31.25) 0 (0) < 0.001Hyperlipidemia, n (%) 22 (27.5) 20 (27.5) 2 (28.57) 0.908Active smokers, n (%) 20 (21.25) 17 (21.25) 3 (42.86) 0.007Beta blocker, n (%) 45 (51.25) 41 (51.25) 4 (57.14) 0.677ACE inhibitor/AT antagonist, n (%) 49 (57.5) 46 (57.5) 3 (42.86) 0.318Diuretics, n (%) 22 (27.5) 19 (23.75) 3 (42.86) 0.027Nitrates, n (%) 7 (6.25) 5 (6.25) 2 (28.57) < 0.001BMI > 27 26 (30) 24 (30) 2 (28.57) 0.885Age > 65 50 (58.75) 47 (58.75) 3 (42.86) 0.282
Hb (g/dL) median (IQR) 11.7 (10.1–13) 11.65 (10.1–13) 12.6 (11.1–14.7) 0.874
Creatinine (mg/dL) median (IQR) 0.85 (0.7–1) 0.84 (0.7–1.01) 0.9 (0.75–0.98) 0.924
hsTNT (ng/L) median (IQR) 11.45 (6.28–19.5) 11.29 (6.03–18.57)
26.62 (21.48–76.31) 0.045
NT-proBNP (pg/mL) median (IQR) 280.3 (99.71–450.1)
259.05 (93.03–447.45)
759.2 (433–6095) 0.017
hsTNT > 14 ng/L, n (%) 34 (39.08) 28 (35) 6 (85.71) 0.008NT-proBNP > 300 pg/mL, n(%) 40 (41.25) 33 (41.25) 7 (100) < 0.001
Abbreviations: hsTnT – high-sensitive troponin T; NT-proBNP – N-Terminal Pro B-type natriuretic peptide; BMI – Body Mass Index; NYHA – New York Heart Association; ACE – Angiotensin Converting Enzyme; AT – Angiotensin; SD – Stan-dard Deviation; IQR - Interquartile Range

166 SJAIT 2018/7-8
1.17–385.25; p = 0.04), and for patients with docu-mented CAD was 75.00 (95% CI, 1.15–4868.64; p = 0.04) (Table II – Mortality events and OR in pa-tients with baseline cut-offs of > 14ng/L for hsTnT and of > 300pg/mL for NT-proBNP ).
Table III (High-sensitive troponin T related to comorbidities) presents the values of hsTnT as a prognostic indicator in accord with comorbidities. From this data, we can see that patients over the
age of 65 have statistically significant values of hsT-nT. Other comorbidities were not in association with values of hsTnT.
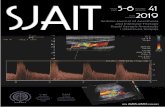
ROC curve (Figure 1 – ROC curves for hsTNT and NT-proBNP for the mortality rate) and AUC
analysis (Table IV – Area under the curve analysis of hsTNT and NT-proBNP for the mortality rate) was used to evaluate specificity and sensitivity of both values of hsTNT (p = 0.004) and NTproBNP
Table II: Mortality events and OR in patients with baseline cut-offs of > 14 ng/L for hsTnT and of > 300 pg/mL for NT-proBNP
Mortality
hsTnT (> 14 ng/L ) and NT--proBNP (> 300 pg/mL)
hsTnT (< 14 ng/L ) and NT--proBNP (< 300 pg/mL) Odds ratio and
95% CI p-Value
Events Total Number Events Total NumberMeasured hsTnT in all patients 6 34 1 53 11.14
(1.28–97.23) 0.03
Measured hsTnT in CAD patients 2 2 0 7 75.00
(1.15–4868.64) 0.04
Measured NT--proBNP in all patients
7 40 0 47 21.27(1.17–385.25) 0.04
Measured NT--proBNP in CAD patients
2 2 0 7 75.00(1.15–4868.64) 0.04
Abbreviations: hsTnT – high-sensitive troponin T; NT-proBNP – N-Terminal Pro B-type natriuretic peptide; CI – Confidence Interval; CAD – Coronary Artery Disease
Table III: High-sensitive troponin T related to comorbidities
hsTnT (ng/L)Median IQR P-value
Creatinine > 1.2 mg/dLyes 31.88 11.54–70.50 0.251no 11.28 6.25–19.15diabetesyes 11.8 5.73–19.98 0.588no 11.29 6.71–19.6smokeryes 12.02 8.12–21.31 0.183no 11.08 5.9–19.38hypertensionyes 11.55 7.84–20.82 0.883no 11.45 5.72–19.7Age > 65yes 15.35 8.46–25.94 0.003no 8.11 4.91–12.02BMI > 27yes 8.35 4.61–19.16 0.117no 11.93 7.38–21.13
Abbreviations: hsTnT – high-sensitive troponin T; BMI – Body Mass Index

167
(p = 0.002) as indicators for increased mortality risk. All the patients with values equal to or higher than cut-offs of measured biomarkers were consid-ered as positive.
Table V (Results of Cox regression analyses) presents the summary statistics for multivariant Cox regression analysis of tested parameters. The mortality risk for values of hsTNT was 1.050 with statistical significance (p = 0.010). We found no evidence of increased mortality risk among others tested parameters.
DiscussionDuring the perioperative period of major sur-
gery, patients are prone to the significant physio-logical changes and stress10. Cardiovascular system
is probably under the highest risk, especially for those who already have some type of cardiovas-cular disease. Although CAD is a well-established risk factor for perioperative complications11–13 so far there has not been published a research exam-ining the significance of CAD in relation to cardiac biomarkers in a patient undergoing major surgery.
For predicting surgical risk, CAD is usually ob-served as a part of composed risk scores3,14. This
NEKRITIČNA PRIMENA NESTEROIDNIH ANTINFLAMATORNIH LEKOVA U TERAPIJI HRONIČNOG NEMALIGNOG BOLA
Figure 1: ROC curves for hsTNT and NT-proBNP for the mortality rate Abbreviation: hsTnT – high-sensitive troponin T; NT-proBNP – N-Terminal Pro B-type natriuretic
peptide; ROC – receiver operating characteristic
Table IV: Area under the curve analysis of hsTNT and NT-proBNP for the mortality rate
Test Result Variables Area Std. Errora Asymptotic Sig.bAsymptotic 95% Confidence Interval
Lower Bound Upper Bound
hsTNT (ng/L) 0.834 0.076 0.004 0.686 0.982
NT-proBNP (pg/ml) 0.862 0.046 0.002 0.772 0.953
Abbreviations: hsTnT – high-sensitive troponin T; NT-proBNP – N-Terminal Pro B-type natriuretic peptide

168 SJAIT 2018/7-8
scoring has gained popularity recently, but the specific role of CAD in predicting complications during the perioperative period is still unclear. Our study included 87 subjects from which about 10% had positive history of CAD, and one of the main purposes of the paper was to evaluate wheth-er values of cardiac markers may be used for iden-tifying high perioperative mortality risk in patients suffered from CAD.
Both markers examined in the present study are used as a proof of myocardial damage. Although most publications showed biomarker elevation in postoperative period, we could find only sever-al that evaluated the significance of their increase before the operation15,16. This is especially true for hsTnT, since only Weber et al. demonstrated that in-creased level of this marker in preoperative period indicated significant risk for the fatal cardiovascular complications both during and after the surgery17.
Using highly sensitive essays, we were able to detect even minor elevations in troponin T levels. Furthermore, such increased values of this marker may be detected even in population of apparent-ly healthy individuals. It is well documented that significant elevation of this biomarker is in direct association to patients with either CAD or other cardiovascular diseases, and it provides important prognostic information.8,9,18 Thus, detected in this way, troponin T seems to become strong prognos-tic marker, not only for the acute coronary syn-drome, but also for apparently stable CAD and other non-acute states in patients with various car-diovascular disorders.
The most interesting finding was that levels of hsTnT above the predefined margin (> 14ng/L) were significantly associated with unwanted events. More than one third of our patients (39%) had increased levels of hsTnT, and there was a clear difference between survivors and deceased. The levels of this marker were increased in more than 85% in subjects deceased. Similar trends noted for NT-proBNP. Its levels were above cut-off value in 41% of the patients from the entire cohort, and in all the subjects who did not survive, follow/up period had increased values. The most important clinically relevant finding was the possibility of applying these biomarkers to predefined protocols for risk stratification that may help to identify sub-jects with high risk for fatal complications. How-ever, measurements of hsTnT and NT-proBNP for all patients undergoing major surgery into routine biochemical profiles, would be both impractical and very expensive. For this reason we searched for the group of patients who could benefit the most from such analysis.
Although neither Mangano nor Lidsky in their studies found the association between preoperative CAD and both major cardiac events and subse-quent mortality after surgical intervention2,19, our results showed statistically significant association with fatal events in short-term follow-up. However, with a small sample size, caution must be applied. This observational study suggests that measuring of hsTnT and NT-proBNP in a patient with docu-mented CAD or without it, may help prevent the risk of mortality events. Additionally, our findings
Table V: Results of Cox regression analyses
B p-value Wald df Sig. Exp (B)
Systolic blood pressure
(mmHg)-0.008 0.021 0.164 1 0.685 0.992
Heart rate (/min) -0.038 0.039 0.961 1 0.327 0.962
NT-proBNP (pg/ml) 0.000 0.000 1.720 1 0.190 1.000
hsTnT (ng/L) 0.049 0.019 6.633 1 0.010 1.050
Lee score ≥ 2 -0.043 1.012 0.002 1 0.966 0.957
NYHA II-IV 0.970 1.251 0.601 1 0.438 2.637
Angina pectoris CCS II-IV 1.067 1.122 0.905 1 0.341 2.907
Abbreviations: hsTnT – high-sensitive troponin T; NT-proBNP – N-Terminal Pro B-type natriuretic peptide; NYHA – New York Heart Association; CCS – Canadian Cardiovascular Society

169
suggest that hsTnT was more prognostic for sub-jects age over 65, as well as statistically significance only for hsTnT among other tested parameters in multivariant regression analysis. Furthermore, these findings lead to debate about the criteria for detecting CAD. Since we defined positive laborato-ry tests, clinical risk factors, prior bypass surgery, coronary intervention or prior myocardial infarc-tion as only necessary criteria for diagnosing CAD, it is possible to apply more lenient criteria, which are not only known from the history or medical management, and that may give different results. This is an important issue for future research.
The study would have been more interesting if it had included an analysis of coronary inter-vention in patients with CAD prior to an elective major surgery. There is a number of publications that evaluate this problem20–23. The CARP trial concluded that preoperative coronary revascular-ization did not improve perioperative or long-term outcomes. The rates of postoperative myocardial infarction and mortality were similar in all includ-ed patients, and they were not dependent on prior revascularization22. Indeed, percutaneous or surgi-cal coronary procedures delayed elective vascular surgery22,23. Moreover, the delay may cause very serious consequences in both vascular and major abdominal surgery, and a definite need for balance between risks and benefits of potential delay is im-portant for every single patient. A reasonable ap-proach to tackle this issue could be to potentiate the significance of risk stratification for patients with documented CAD before a non-cardiac sur-gery.
This study has several important limitations. The major limitation of this study was the small sample size. Second, this research was conduct-ed in one center and included patients that were prepared for major surgery according to local pro-tocols. Third, more comprehensive survey would deserve strict preoperative stratification of CAD based on cardiac catheterization and/or echocar-diography, but such stratification was out of the scope in this study. Fourth, we did not measure hsTnT and NT-proBNP levels after the operations and it was not possible to evaluate whether these values would have been more prognostic for the same patients than these perioperative measures. Fifth, the study design requires that included sub-jects must have minimum one cardiovascular risk
factor and age over 55, so that our results cannot be generalized to patients who are undergoing a ma-jor non-cardiac surgery, but without those criteria. Also, the mortality was followed-up for a period of 30 days and our findings may be useful only for prognosis of short-term mortality risk. Finally, our results could not have been affected by selection bias, because of absence of marker levels during the study.
ConclusionIn summary, this study has shown that preop-
eratively increased levels of cardiac biomarkers are positively associated with short-term mortality in postoperative period after major abdominal or vascular surgery, and they can serve as important predictors of fatal events. The research has also shown that patients with CAD benefit the most from determination of hsTnT and NT-proBNP levels before the surgery. These findings suggest that increased values of examined markers denote significant risk for this group of patients. In case of a such increase, patients deserve more detailed ex-amination before the surgery and careful balancing between potential delay of the surgery and the risk that it carries with it. Although the current study is based on a small sample of participants, the find-ings suggest potentially prognostic biomarkers for patients undergoing major non-cardiac surgery. Large randomized controlled trials could provide more definitive evidence.
References 1. L’Italien GJ, Paul SD, Hendel RC, et al. Development
and validation of a Bayesian model for perioperative cardiac risk assessment in a cohort of 1,081 vascular surgical candi-dates. J Am Coll Cardiol 1996; 27:779–86.
2. Mangano DT, Layug EL, Wallace A, et al. Effect of ate-nolol on mortality and cardiovascular morbidity after non-cardiac surgery. Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med 1996; 335:1713–20.
3. Lee TH, Marcantonio ER, Mangione CM, et al. Deriva-tion and prospective validation of a simple index for predic-tion of cardiac risk of major noncardiac surgery. Circulation, 1999; 100:1043–1049.
4. Blankenberg S, Zeller T, Saarela O, et al. Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts: the MONICA, risk, genetics, archiving, and monograph (MORGAM) biomarker project. Circulation 2010; 121:2388–97.
5. Zethelius B, Berglund L, Sundstrom J, et al. Use of mul-tiple biomarkers to improve the prediction of death from car-diovascular causes. N Engl J Med 2008; 358:2107–16.
NEKRITIČNA PRIMENA NESTEROIDNIH ANTINFLAMATORNIH LEKOVA U TERAPIJI HRONIČNOG NEMALIGNOG BOLA

170 SJAIT 2018/7-8
6. Weber M, Hamm C. Role of B-type natriuretic pepti-de (BNP) and NT-proBNP in clinical routine. Heart 2006; 92:843–849.
7. Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J, 2007; 28:2525–2538.
8. Latini R, Masson S, Anand IS, et al. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 2007; 116:1242–1249.
9. Omland T, de Lemos JA, Sabatine MS, et al. A sensitive cardiac troponin T assay in stable coronary artery disease. New Engl J Med 2009; 361:2538–2547.
10. Udelsman R, Norton JA, Jelenich SE, et al. Respon-ses of the hypothalamic-pituitary-adrenal and renin-angi-
otensin axes and the sympathetic system during controlled surgical and anesthetic stress. J Clin Endocrinol Metab 1987; 64:986–94.
11. Sabaté S, Mases A, Guilera N, et al. ANESCARDIO-CAT Group. Incidence and predictors of major perioperative adverse cardiac and cerebrovascular events in non-cardiac surgery. Br J Anaesth 2011; 107:879–90.
12. van Diepen S, Bakal JA, McAlister FA, et al. Mortality and readmission of patients with heart failure, atrial fibril-lation, or coronary artery disease undergoing non-cardiac surg Heekeren DW, et al. Coronary bypass in vascular pati-ents: A relatively high-risk procedure. Ann Vasc Surg 1997; 11:612–9.

doi:10.5937/sjait1806125RISSN 2466-488X (Online)
Sažetak
Uvod:Veliki i multipli miomi su dobro poznat uzrok in-fertiliteta, ali nije neuobičajeno da i pored njihovog pri-sustva dođe do spontane trudnoće. Tretman pacijentki-nja sa velikim i multiplim miomima je kontroverzan, ne samo u toku trudnoće već i prilikom porođaja. Ovakvi miomi mogu da budu uzrok značajnog morbiditeta u puerperijumu. Carski rez je najčešći način završavanja porođaja. Prikaz slučaja: Carski rez sa polimiomekto-mijom učinjen je u 36. nedelji gestacije, kod pacijentkinje sa velikim multiplim miomima, uz upotrebu cell savera, sa dobrim fetalnim i maternalnim ishodom. Pristup do-njem segmentu uterusa je bio moguć uprkos postojanju velikih mioma. Živo novorođenče, telesne mase 2600 grama, rođeno je bez teškoća. Nakon zbrinjavanja histe-rotomije, učinjena je ekstrakcije najvećeg mioma (210 × 180 ×155 mm) i njegovo ležište je ušiveno u dva sloja. U toku miomektomije, korišćen je cell-saver i spasena je značajna količina krvi. Pošto je ustanovljena adekvatna hemostaza, odlučeno je da se ukloni i preostalih osam mioma, što je i učinjeno, bez otvaranja materične duplje. Zaključak: Mali je broj radova koji prikazuju intraope-rativno „spasavanje krvi” kao tehniku kojom se rešava intraoperativno krvarenje u toku miomektomije, tokom carskog reza. Naš slučaj dokazuje da intraoperativno „spasavanje krvi” u kombinaciji sa velikim hirurškim is-kustvom u klasičnoj miomektomiji značajno poboljšava ishod ovakvih operacija.
Ključne reči: miom; trudnoća; komplikacija; porođaj; cell-saver
Summary
Introduction: Although large multiple myomas are a well-known cause of infertility, it is not uncommon to encounter pregnancy with such myomas. Management of women with large multiple myomas is controversial, both during pregnancy and delivery. Such myomas can also cause significant morbidity during the puerperium. Caesarean section is the most common way of delivery.Case report: A patient with large multiple myomas un-derwent a cesarean myomectomy with intraoperative cell salvage at 36 weeks of gestation. Both fetal and maternal outcomes were favorable. The lower uterine segment was accessible, despite the presence of myomas, and a live fe-tus weighing 2600 g was delivered without difficulties. Following a hysterotomy suturing, the largest myoma (210 × 180 × 155 mm) was removed and the myoma bed was sutured in two layers. Cell-saver was introduced during myomectomy saving significant amount of blood. Careful inspection confirmed appropriate hemostasis, so it was decided to remove the remaining eight myomas, and this was done without breaching the uterine cavity. Conclusion: There are few literature reports on intraop-erative cell salvage as a technique of handling intraoper-ative hemorrhage during a CM. As documented by our case, the use of intraoperative cell salvage represents a significant advantage in such cases when combined with extensive surgical experience in conventional myomec-tomy.
Keywords: myoma; pregnancy; delivery complications; cell-saver
Autor za korespondenciju: Radmila Sparić, Klinika za ginekologiju i akušerstvo, Klinički centar Srbije, Višegradska 26, 11000 Beograd, Sr-bija, E-mail: [email protected]
Corresponding author: Radmila Sparić, Clinic for Gynecology and Obstetrics, Clinical Center of Serbia, Višegradska 26, 11000 Belgrade, Serbia, E-mail: [email protected]
Prikaz slučaja Case report
MIOMEKTOMIJA U TOKU CARSKOG REZA KOD P ACIJENTKINJA SA VELIKIM MULTIPLIM MIOMIMA: KOLIKI JE RIZIK? PRIKAZ SLUČAJA.
Radmila Sparić1,2, Milan Dokić1,2, Ivana Likić Lađević1,2, Dragiša Šljivančanin1, Milica Stojičić2, Snežana Vidaković1,2
1Klinički centar Srbije, Klinika za ginekologiju i akušerstvo, Beograd, Srbija; 2Univerzitet u Beogradu, Medicinski fakultet, Beograd, Srbija
IS CESAREAN MYOMECTOMY IN PATIENTS WITH LARGE MULTIPLE MYOMAS ALWAYS A HAZARDOUS PROCEDURE? A CASE REPORT (Running title: Cesarean myomectomy in the treatment of large multiple myomas)
Radmila Sparić1,2, Milan Dokić1,2, Ivana Likić Lađević1,2, Dragiša Šljivančanin1, Milica Stojičić2, Snežana Vidaković1,2
1Clinical Center of Serbia, Clinic for Gynecology and Obstetrics, Belgrade, Serbia; 2University of Belgrade, School of Medicine, Belgrade, Serbia

172 SJAIT 2018/7-8
Introduction
Although large multiple myomas are a well-known cause of infertility1, it is not uncom-
mon to encounter pregnancy with such myomas2,3. The management of pregnants with large multiple myomas is controversial. Мyomectomy during pregnancy is considered to be a hazardous proce-dure associated with possible subsequent fetal loss and significant maternal morbidity3. Moreover, large myomas (50 mm) may cause both maternal and fetal complications during pregnancy and deli-very4. Significant perioperative hemorrhage might occur in these patients if a cesarean section (CS) is performed, especially with associated cesarean myomectomy (CM)5,6. However, such myomas are a frequent indication for CS, and it is reasonable to believe that CS rates will rise in such women due to the worldwide trend of delayed childbearing7.
Looking at the early history of CM, immediate cesarean hysterectomy was considered to be the treatment of choice in such patients8. Even some recent publications report cesarean hysterectomy in women with multiple myomas, who were not interested in further reproduction9. Conversely, over the past decades, numerous publications re-port favorable outcomes of CM, even in cases of multiple myomas, if the procedure is performed by experienced surgeons5,10,11.
We present a patient who had large multiple myomas and underwent a CM, without any com-plications and with a favorable fetal and maternal outcome.
Case reportA 34-year-old primipara was referred to our
institution in her 23rd week of pregnancy with abdominal pain, suggesting red degeneration of previously diagnosed multiple myomas. Largest myoma was estimated to be 140 mm at the first tri-mester scan. The patient underwent complete clin-ical, sonographic, laboratory and microbiological work-up. Uterine size was not correspondent with gestational age, and the paraumbilical mass was palpable through the abdominal wall, correspon-dent with myoma location in the fundal region and to the right. Ultrasonography confirmed the pres-ence of multiple myomas, ranging from 30 to 170 mm in diameter. Placental insertion was just below the largest myoma. The fetus was in transverse lie;
fetal biometry was appropriate for gestational age, and no fetal abnormalities were diagnosed. Labo-ratory findings revealed anemia with a red blood cell count (RBC) 3.25, hemoglobin level 101 g/l and hematocrit level of 27.5%. C-reactive protein (CRP) was elevated 101.8 ml/l (normal range ˂ 5 mg/L), and the fibrinogen level was 6.4 g/l (normal range 2–4 g/l). The microbiological results docu-mented Klebsiella Enterobacter in cervical culture. She was treated with bed rest, analgesics and an-tibiotics according to her microbiological results, which resolved her complaints. Low molecular weight heparin was introduced for prophylactic reasons. Anemia was treated with iron tablets and folic acid.
Available treatment options were discussed with the patient. She decided to preserve the pregnancy and refused the myomectomy during pregnancy. Due to advanced gestational age and the presence of multiple myomas, myomectomy in pregnancy was not considered to be an appropriate therapeu-tic approach. Since intermittent irregular uterine contractions were registered, progesterone was administered. In the 28th week of pregnancy, ar-tificial fetal lung maturation was conducted. As se-rial ultrasound examinations documented normal fetal growth, development and oxygenation, with-out significant worsening of the maternal status, she further received regular antenatal care in our hospital with fetal surveillance. Ultrasound follow up documented myoma growth, and the size of the largest myoma at 33 weeks of gestation was found to be approximately 200 mm. At 36 weeks of ges-tation, considering deformation of uterine cavity, breech presentation and maternal cachexia, it was decided to perform CS.
Prior to CS, the patient was informed about the possibility of feasible and safe myomectomy, but also possibility of a massive hemorrhage and an inevitable cesarean hysterectomy.
The patient was operated under general anes-thesia. The abdomen was opened by infraumbil-ical median laparotomy, and several subserous myomas were identified, of which the biggest was subserosal in the fundal region and on the right (Figure 1). Despite myoma presence, the lower uterine segment (LUS) was accessible, and a live fetus weighing 2600 g was delivered without diffi-culties. Following LUS suturing, the largest myoma was removed and the myoma bed was sutured in

173AKUTNA MEZENTERIJALNA ISHEMIJA KOD KARDIOHIRURŠKIH BOLESNIKA – PRIKAZ SLUČAJA I PREGLED LITERATURE
two layers. Inspection confi rmed appropriate he-mostasis, so it was decided to remove the remain-ing eight myomas. Myomactomy was performed without breaching the uterine cavity (Figure 2). An abdominal drain was put in place for prophylactic reasons. Th e surgery lasted 170 minutes in total, and it was performed by a senior surgeon (S.V.) with vast experience in conventional myomec-tomy. Intraoperative cell salvage was introduced from skin incision and further onward. Th e pa-tient received a total of 2450 ml of autologous and 820 ml of heterologous blood transfusion during the operation, 395 ml of fresh frozen plasma, 10 units of cryoprecipitate together with colloid and crystalloid solutions, and 0.5 g of tranexamic acid. Aft er the surgery, she spent one day in the obstetric intensive care unit and received one unit of packed red blood cells (RBC). Th e patient’s recovery was uneventful, and she was discharged with her baby on the seventh postoperative day.
Th e histopathology report documented a myo-ma size, ranging from 20 mm up to 210 × 180 × 155 mm and weighing 3300g in total. Th e microscop-ical examination of the enucleated myomas found the presence of hyaline degeneration, hemorrhage, necrosis, and calcifi cation (Figure 3).
DiscussionHere we present a favorable fetal and maternal
outcome of CS combined with multiple myomec-
tomies in a patient with large myomas, performed by an experienced surgeon with intraoperative cell salvage.
Classic obstetric textbooks generally consider CM to be a risky procedure, particularly in the case of multiple myomas5, 6. Moreover, it is documented that myoma size, even in the event of a single myo-mectomy and particularly in the case of multiple myomas, signifi cantly infl uences the frequency of intraoperative hemorrhage, which is reported to be as high as 35.29%6.
Large multiple myomas are particularly diffi -cult to handle as they can sometimes present an obstacle for cesarean delivery, limiting access to the normal myometrium and, thus, necessitating a CM in order to conduct the delivery itself, even by means of corporeal cesarean section5,10,12. Further-more, they could be challenging for hysterotomy suture, regardless of its location at LUS or uterine corpus5,10. Hence, early CM reports suggested ce-sarean hysterectomy, concluding „it will usually be wise to remove the uterus, especially if it is the seat of multiple tumors”8.
In cases when delivery and uterine suturing is possible without a myomectomy, as in the pre-sented case, most surgeons would consider inter-val myomectomy as the treatment of choice12,13. Nevertheless, numerous literature reports describe successful CMs in these patients11,14. Our case sup-ports these observations. Apart from high-dose oxytocin usage, literature reports of various surgi-cal techniques used to reduce perioperative hem-orrhage5,10. Th ere is a lack of data on intraoperative
Figure 1: а. preoperative image – abdomen of the patient; b. uterus and the myomas – fi nding aft er laparotomy

174 SJAIT 2018/7-8
cell salvage as an additional technique enabling CM in cases of large multiple myomas15. Ma et al.2 enucleated a 3645 g myoma, using bilateral liga-tion of the uterine arteries aft er closing the corpo-ral uterine incision. Given that the patient was a 32-year-old primigravida, such an approach might be questionable considering the patient’s age and parity, despite the fact that the estimated blood loss in this particular case was 1400 ml. On the other hand, because of the presence of abundant vascu-lar anastomosis between the uterine and ovarian blood vessels, this technique is questionable when there is uncontrollable hemorrhage in the case of multiple myomas. Moreover, the use of intraoper-ative cell salvage in our case enabled multiple myo-mectomy. It could be an alternative to vascular li-gations in cases of multiple myomas, as sometimes these can even present an obstacle in applying both tourniquets and stitches for vascular occlusion to reduce intraoperative hemorrhage10. Despite the
conclusions in the literature of usefulness of this approach in the reduction of postoperative hemor-rhage, as well as myoma recurrence, its use is ques-tionable in women of the reproductive age5.
In some instances, CM is inevitable12. Yuddan-di et al.16 described a case of caseous degeneration of a myoma 170 × 140 mm in diameter during a CS performed for suspected placental abruption. Th e myoma was so extensively degenerated that it emerged from the uterus following a LUS incision, necessitating an inverted T-shape incision for fetal extraction.
Literature also showed that avoiding CM in such instances could cause signifi cant maternal morbidity in the postpartum period, including sepsis, postpartum hemorrhage, and hysterecto-my7. Yellamareddygari et al.17 described a case of uneventful CS in a woman with a 120 mm pos-terior myoma, necessitating emergency vaginal myomectomy six weeks postpartum by morcella-
Figure 2: а. uterus aft er CM, posterior wall; b. uterus aft er CM, anterior wall and fundus; c. removed myomas

175
tion and the use of electrosurgery for hemostasis. Histopathology confi rmed the necrosis of the re-moved myoma. Major maternal complications of multiple infarcted myomas aft er CS were also de-scribed by Narayan et al18. Th ey presented a case of a 36-year-old woman who underwent right hemi-colectomy, small bowel resection, end ileostomy, and total abdominal hysterectomy 19 days post-partum. Th e myomas were found to be pus-fi lled and densely adherent to intraabdominal organs; their separation from the bowel was not possible. Th e possibility of developing such complications was prevented by CM in our case.
Recent medical innovations, such as intraopera-tive cell salvage, provide skillful obstetric surgeons with an option to perform CM in women with a my-omatosic uterus, thus preserving fertility, avoiding the risks of massive transfusion, and ensuring the mother’s uneventful recovery. Moreover, avoiding the use of various hemostatic techniques described in literature prevents possible complications that could arise from compromised uterine vasculariza-tion, which is inevitable in cases of suturing and/or the embolization of major blood vessels.
Literature reports on intraoperative cell sal-vage as a method of handling intraoperative hem-orrhage during CS in women with myomas are scarce15. Th e reason for this can be that most CM reports originate from low-income countries. De-spite the reports on favorable outcomes of CMs in women with a large myomatosic uterus, most of
these are case reports, underlining surgical expe-rience as the only factor infl uencing a good out-come. Nevertheless, reports on unfavorable out-comes are lacking, most probably due to insuffi -cient reporting. Although literature on CM safety and feasibility is abundant4,19, there are few reports on major CM complications20,21. True incidence of life-threatening complications in such cases re-mains unknown.
Th e use of intraoperative blood cell salvage for CMs, in combination with surgical expertise in conventional myomectomy it provides good peri-natal outcome in challenging cases like pregnancy accompanied with multiple large myomas.
References1. Aćimovic M, Jeremić K, Petković S, et al. Th e role of
myomectomy in female infertility. Acta Chir Iugosl. 2008; 55(4):81–6.
2. Ma PC, Juan JC, Wang ID, Chen CH, Liu WM, Jeng CJ. A huge leiomyoma subjected to myomectomy during a cesarean section. Taiwan Obstet Gynecol. 2010; 49(2):220–2.
3. Goldman LR, Valentine LN, Falcone T. Myoma in pregnancy. In: Tinelli A, Malvasi A. Uterine myoma, myo-mectomy and minimally invasive treatments. Springer, Ber-lin, 2015:219–236.
4. Pergialiotis V, Sinanidis I, Louloudis IE, Vichos T, Per-rea DN, Doumouchtsis SK. Perioperative complications of Cesarean Delivery Myomectomy: A meta analysis. Obstet Gynecol 2017; 130(6):1295–303.
5. Malvasi A, Stark M, Tinelli A. Cesarean myomectomy. In: Tinelli A, Malvasi A. Uterine myoma, myomectomy and mini-mally invasive treatments. Springer, Berlin, 2015; 237–252.
AKUTNA MEZENTERIJALNA ISHEMIJA KOD KARDIOHIRURŠKIH BOLESNIKA – PRIKAZ SLUČAJA I PREGLED LITERATURE
Figure 3: Histological appearance of the largest myoma (hematoxylin eosin staining): a. hyalinization; b. necrosis; c. hemorrhage; d. calcifi cations

176 SJAIT 2018/7-8
6. Sparic R. Intraoperative hemorrhage as a complication of cesarean myomectomy: analysis of risk factors. Intraopera-tive hemorrhage as a complication of cesarean myomectomy: analysis of risk factors. Vojnosanit Pregl. 2016; 73(5):415–21.
7. Sparić R. Uterine myomas in pregnancy, childbirth and puerperium. Srp Arh Celok Lek. 2014; 142(1–2):118–24.
8. Spencer HR. Caesarean section and total abdominal hysterectomy for retroflection of the uterus at term by fibro-myoma adherent in Douglas’s pouch. Proc R Soc Med. 1909; 2(Obstet Gynaecol Sect):74–80.
9. Li H, Du J, Jin L, Shi Z, Liu M. Myomectomy during ce-sarean section. Acta Obstet Gynecol Scand. 2009; 88(2):183–6.
10. Sparic R, Malvasi A, Kadija S, Babovic I, Nejkovic L, Tinelli A. Cesarean myomectomy trends and controversies: an appraisal. J Matern Fetal Neonatal Med. 2017; 30(9):1114–23.
11. Tinelli A, Malvasi A, Mynbaev OA, et al. The surgical outcome of intracapsular cesarean myomectomy. A match control study. J Matern Fetal Neonatal Med. 2014; 27(1):66–71.
12. Sparić R, Lazović B. Inevitable cesarean myomectomy following delivery through posterior hysterotomy in a case of uterine torsion. Med Arch. 2013; 67(1):75–6.
13. Haskins RD Jr, Haskins CJ, Gilmore R, Borel MA, Mancuso P. Intramural leiomyoma during pregnancy be-coming pedunculated postpartally. A case report. J Reprod Med. 2001; 46(3):253–5.
14. Sparic R, Malvasi A, Tinelli A. Analysis of clinical, bio-logical and obstetric factors influencing the decision to per-form cesarean myomectomy. Ginekol Pol. 2015; 86(1):40–5.
15. Sparić R, Lazović B, Sulović N, Buzadzić S. Our expe-rience with intraoperative cell salvage during cesarean de-livery in women with uterine myomas – four case reports. Med Pregl. 2014; 67(3–4):111–7.
16. Yuddandi N, Gleeson R, Gillan J, Geary M. Manage-ment of massive caseous fibroid at caesarean section. J Obstet Gynaecol. 2004; 24(4):455–61.
17. Yellamareddygari S, Chakrabarti M, Ravuri S, Ahlu-walia A. Leaving fibroids at cesarean section, is it safe? Gyne-col Surg. 2010; 7:173–5.
18. Naryan B, McCatrhy F, Nelson-Piercy C. Chronic anorexia and weight loss due to extensive fibroid compressi-on of the bowel: an unusual complication of uterine fibroids in a patient with twin pregnancy. BMJ Case Rep. 2016; pii: bcr2016214858.
19. Song D, Zhang W, Chames MC, Myomectomy during cesarean delivery. Int J Gynaecol Obstet. 2013; 121(3):208–13.
20. Exacoustos C, Rosati P. Ultrasound diagnosis of uteri-ne myomas and complications in pregnancy. Obstet Gynecol. 1993; 82(1):97–101.
21. Seffah JD. Re-laparotomy after cesarean section. Int J Gyn Obstet. 2005; 88(3):253–7.

doi:10.5937/sjait1806133SISSN 2466-488X (Online)
Autor za korespondenciju: Dragana Unić-Stojanović, Institut za kar-diovaskularne bolesti „Dedinje”, 11 000 Beograd, Milana Tepića 1, Te-lefon: 064/843 11 03, E-mail: [email protected]
Corresponding author: Dragana Unić-Stojanović, Institut za kardio-vaskularne bolesti „Dedinje”, 11 000 Beograd, Milana Tepića 1, Tele-fon: 064/843 11 03, E-mail: [email protected]
Revijalni članak Review article
PRIMENA CEREBRALNE OKSIMETRIJE U KAROTIDNOJ HIRURGIJI (Cerebralna oksimetrija i karotidna hirurgija)
Dragana Unić-Stojanović1
1Klinika za anesteziju i intenzivno lečenje, Institut za kardiovasku-larne bolesti „Dedinje”, Beograd, Medicinski fakultet Univerziteta u Beogradu
APPLICATION OF CEREBRAL OXYME-TRY IN CAROTID SURGERY (Cerebral oximetry and carotid surgery)
Dragana Unić-Stojanović1
1Klinika za anesteziju i intenzivno lečenje, Institut za kardiovasku-larne bolesti „Dedinje”, Beograd, Medicinski fakultet Univerziteta u Beogradu
Sažetak
Cerebralni neuromonitoring, tokom operacije unutrašnje ka-rotidne arterije, ima nekoliko modaliteta: elektroencefalogram, merenje retrogradnog pritiska, transkranijalni dopler, somato-senzorni evocirani potencijali, „Near infrared” spektroskopija (NIRS-rSO2) i monitoring budnog bolesnika. NIRS je neinva-zivna metoda monitoringa, koja pruža korisne informacije o odgovarajućem terapijskom pristupu, tokom i posle operacije unutrašnje karotidne arterije. Ne postoji definisana specifična apsolutna vrednost rSO2 koja bi se koristila kao kritična vred-nost ispod koje se razvija cerebralna ishemija. Sniženje rSO2 u odnosu na bazalnu početnu vrednost, posle klemovanja unu-trašnje karotidne arterije, veće od 20% ima visoku negativnu prediktivnu vrednost – ako se rSO2 ne snižava, ishemija je malo verovatna; ali nisku pozitivnu prediktivnu vrednost – pad rSO2 ne ukazuje uvek na prisustvo cerebralne ishemije.
Ključne reči: cerebralna ishemija; cerebralna oksimetrija; hirurgija, karotidna endarterektomija
Summary
(Cerebral oximetry and carotid surgery)During carotid endarterectomy and carotid artery cross-clamp-ing, various methods for monitoring of cerebral perfusion and function are suggested, including electroencephalography, measurement of the stump pressure, transcranial Doppler, so-matosensory evoked potentials, regional cerebral oxygen sat-uration monitoring (NIRS-rSO2) or direct neurological mon-itoring of the awake patient during carotid cross-clamping. NIRS is a non-invasive monitoring method that may provide useful information on the most appropriate management dur-ing the procedure and postoperative recovery period in carotid endarterectomy patients. It is not possible to specify an abso-lute rSO2 reading as the critical value below which cerebral ischemia may develop. A relative decrease of rSO2 > 20% after carotid occlusion has an elevated negative predictive value – if rSO2 does not decrease, ischemia is unlikely, but a low positive predictive value – a decrease in rSO2 may not always indicate cerebral ischemia.
Key words: cerebral ischemia; cerebral oximetry; surgery, ca-rotid endarterectomy
Uvod
Karotidna arterijska bolest je lokalna manifesta-cija sistemske bolesti. Primarni uzrok stenoze
unutrašnje karotidne arterije je aterosklerotični plak, sa lokalizacijom na bifurkaciji zajedničke ka-rotidne arterije, koji dovodi do suženja arterije i/ili embolizacija trombotičnim materijalom sa pra-tećim neurološkim manifestacijama (tranzitorni ishemijski atak ili cerebrovaskularni insult)1.
Endarterektomija unutrašnje karotidne arterije
Indikacije za karotidnu endarterektomiju obu-hvataju prisustvo simptomatske stenoze unutra-šnje karotidne arterije veće od 50%, i asimptomat-ske stenoze veće od 70%2.
Karotidna endarterektomija je hirurška proce-dura koja se izvodi prvenstveno u cilju sniženja incidence embolijskog i trombotičnog cerebrova-skularnog insulta. Iako karotidna endarterektomi-ja predstavlja preventivnu proceduru, prisutan je rizik nastanka značajnih perioperativnih kompli-kacija (infarkt miokarda, neurološki deficit, smrtni

178 SJAIT 2018/7-8
ishod, perioperativna hemodinamska nestabilnost – hipertenzija, hipotenzija, tahikardija, poremećaji srčanog ritma)3–5.
Iako je incidenca perioperativnog morbiditeta i mortaliteta relativno niska, a terapijska uspešnost karotidne endarterektomije visoka, suptilna neu-rološka oštećenja i rani postoperativni poremećaji neurokognitivnih funkcija nastaju kod više od 24 do 28% bolesnika posle operacije karotidne arte-rije3. Smatra se da postoperativne kognitivne dis-funkcije predstavljaju formu ishemičnog ataka sa sličnim patofiziološkim mehanizmom nastanka3. Najčešće se navode sledeća tri mehanizma nastan-ka: 1) ipsilateralno, tranzitorno smanjenje krvnog protoka kroz a. cerebri media tokom klemovanja karotidne arterije, što je u skladu sa smanjenom cerebralnom električnom aktivnošću tokom peri-oda klemovanja karotidne arterije; 2) embolizacije delovima aterosklerotskog plaka; 3) cerebralna hi-perperfuzija posle operacije, i kod asimptomatič-nih bolesnika3.
Monitoring moždane funkcijeU medicinskim krugovim postoji mišljenje da
je tokom operacije karotidne arterije neophodan monitoring cerebralnog krvnog protoka i cere-bralne funkcije, posebno tokom klemovanja unu-trašnje karotidne arterije, kako bi se blagovremeno donela odluka o neophodnosti primene šanta4,5. Takođe, smatra se da je zlatni standard za cerebral-ni monitoring, kontinuirano praćenje neurološke funkcije budnog pacijenta tokom operacije funk-cija (senzorna, motorna, više mentalne funkcije)6. To je osnovna prednost izvođenja operacije u lo-kalnoj ili regionalnoj anesteziji7,8. Kod pacijenata koji se operišu u opštoj anesteziji, mogu da se kori-ste sledeće tehnike cerebralnog neuromonitoringa: merenje retrogradnog pritiska, elektroencefalo-gram (EEG), somatosenzorni evocirani potencijali (SSEP), „Near infrared” spektroskopija (NIRS) i transkranijalni dopler (TCD)4–10. Izbor intraope-rativnog monitoringa za detekciju prisustva cere-bralne ishemije, hipoperfuzije i cerebralnih embo-lizacija tokom opšte anestezije je kontroverzan5,6. Sve metode neuromonitoringa imaju relativno nisku senzitivnost i specifičnost za detekciju ne-adekvatne cerebralne perfuzije i cerebralne ishe-mije, sa mogućnošću nastanka lažno-pozitivnih i lažno-negativnih signala6. Rezultati metaanalize
koja je uključila šest randomizovanih studija (1270 bolesnika) pokazali su da nijedna tehnika monito-ringa, koja se koristi u cilju postavljanja indikacije za selektivno plasiranje šanta, ne dovodi do boljih rezultata i boljeg ishoda hirurškog lečenja11.
„Near infrared” spektroskopija „Near infrared” spektroskopija (NIRS) koristi
principe spektrofotometrije i meri regionalnu ce-rebralnu oksigenaciju (rSO2) u predelu frontalne kore, koja je pokazatelj ukupne arterijske, venske i kapilarne oksigenacije, mada predominantni uticaj ima venska krv12.
Glavne prednosti NIRS-a su neinvazivnost, jed-nostavnost primene i to što ne zahteva specijalizo-vani trening i prisustvo posebno obučenog tehnič-kog osoblja tokom primene9,12. Vrednosti saturaci-je se prikazuju kao apsolutne vrednosti, procenat promene u odnosu na početnu (bazalnu) vrednost i kao kumulativna vrednost saturacije ispod pra-govne vrednosti (bazalna vrednost – 25%), koja je određena dužinom vremena koliko je vrednost iz-merene saturacije bila niža od definisane granične vrednosti i veličine tih promena (izražava se u min %). (Slika 1)
Kod zdravih osoba, vrednosti cerebralne oksi-metrije su u opsegu izmedju 58% i 82%13. Bazalne vrednosti značajno variraju među pacijentima, te je za svakog bolesnika neophodno definisanje ba-zalne vrednosti pre uvoda u anesteziju. Dijagno-za prisustva kritične cerebralne ishemije bazira se na odstupanju izmerene vrednosti od bazalne, pre nego na određenoj apsolutnoj vrednosti.
Tokom operacije karotidne arterije, NIRS se koristi u cilju ranog dijagnostikovanja kako sma-njenog cerebralnog protoka (hipoperfuzija) tako i povećane cerebralne perfuzije (hiperperperfuzija).
Slika 1: Prikaz vrednosti cerebralne oksimetrije

179PERIPROTETSKE INFEKCIJE – ČINIMO LI SVE DA IH PREPOZNAMO I SPREČIMO?
Može da se koristi u različitim fazama operacije, od uvoda u opštu anesteziju, adekvatnog pozicio-niranja glave i vrata, tokom operacije, do postope-rativnog oporavka u jedinici intenzivnog lečenja12. Korisna je metoda za prepoznavanje hipoperfuzije tokom klemovanja karotidne arterije, neadekvatnog funkcionisanja šanta ili detektovanja cerebralne is-hemije uzrokovane drugim izvorima, kao što su po-remećaji srčanog ritma i dekompenzacija, odsustvo ventilacije pluća i neželjeni efekti anestetika12,14.
Baikossis i saradnici13 su sproveli studiju u kojoj su evaluirali bazalne vrednosti cerebralne oksime-trije i faktore koji utiču na preoperativne vrednosti kod bolesnika podvrgnutih karotidnoj i kardiohi-rurgiji13. Pacijenti podvrgnuti karotidnoj hirurgiji su bili stariji i imali su više bazalne vrednosti ce-rebralne oksigenacije i veću učestalost moždanog udara13. Učestalost dijabetesa i hiperholesterolemi-je je bila viša u grupi bolesnika koji su podvgnuti kardiohirurškim procedurama13. Ovo istraživanje je ukazalo da su prisustvo dijabetesa, pušenje i hiperholesterolemija značajno povezani sa vred-nošću cerebralne oksimetrije: bazalne vrednosti su obostrano bile značajno niže kod bolesnika sa dijabetes melitusom (60,08 ± 9,03% levo, 57,00 ± 6,90 % desno) u poređenju sa pacijentima bez di-jabetesa (68,80 ± 6,82 levo, 68,55 ± 6,34 desno, P < 0,001). Starost, pol, istorija preležanog cerebro-vaskularnog insulta, hipertenzija, ishemijska koro-narna bolest, astma, stepen stenoze i strana operi-sane unutrašnje karotidne arterije nisu bili značaj-no povezani sa izmerenom vrednošću cerebralne oksimetrije.
Smanjenje rSO2 za 20% nakon klemovanja ka-rotidne arterije je udruženo sa senzitivnošću 80% i specifičnošću 82% za intraoperativnu detekciju moždane ishemije. Prema sadašnjim preporuka-ma, smanjenje rSO2 za 20% se uzima kao kritična vrednost koja upozorava i kada treba da se započ-ne sa interventnim merama9,12. Samra i saradnici su sproveli istraživanje sa ciljem utvrđivanja sen-zitivnosti i specifičnosti različitih nivoa cerebral-ne saturacije kiseonikom, sa ciljem da se proceni intraoperativna cerebralna ishemija kod pacije-nata podvrgnutih operaciji karotidne arterije u regionalnoj anesteziji (cervikalni blok)9. Utvrdi-li su da smanjenje rSO2 više od 20% od početnih vrednosti, nakon klemovanja karotidne arterije, ima pozitivnu prediktivnu vrednost 33% i 97,4% negativnu prediktivnu vrednost. Drugim rečima, u
njihovom istraživanju dobijena negativna predik-tivna vrednost 97,4% znači da ako je tokom klemo-vanja karotidne arterije vrednost rSO2 unutar 20% od početnog nivoa, mala je verovatnoća da postoji kritična ishemija i da je potrebno plasiranje šan-ta, odnosno kod samo 2,6% pacijenata koji imaju pad vrednost rSO2 do 20% od početnih vrednosti tokom klemovanja karotidne arterije će se razvi-ti značajna cerebralna ishemija. Sa druge strane, pozitivna prediktivna vrednost 33,3% označava da je 66,7% lažno pozitivnih rezultata, tj. 66,7% paci-jenta će imati pad vrednosti rSO2 viši od 20%, ali bez razvoja značajne ishemije, što ukazuje na to da ukoliko se vrednost cerebralne oksimetrije koristi za postavljanje indikacije za intraoperativno plasi-ranje šanta, onda u toj grupi pacijenata šant može biti nepotrebno plasiran9.
Mille i saradnici su ispitivali NIRS u cilju odre-đivanja specifičnosti, senzitivnosti i prediktivne vrednosti različitih graničnih (cut off) nivoa rSO2 za predikciju nastanka neuroloških komplikaci-ja i potrebe za plasiranjem šanta15. U studiju su uključili 596 pacijenta operisanih u opštoj aneste-ziji. Prema njihovim rezultatima, cut off vrednost 11,7% (odnosno smanjenje rSO2 za više od 12%) nakon klemovanja karotidne arterije, u odnosu na bazalnu vrednost, ima prihvatljivu senzitivnost 75% i specifičnost 77% u detetekciji prisustva ce-rebralne ishemije. S druge strane, cut off vrednost 20% (smanjenje rSO2 > 20% u odnosu na bazalnu vrednost) ima nižu senzitivnost (30%) i višu speci-fičnost (98%), sa negativnom prediktivnom vred-nošću 98% i pozitivnom prediktivnom vrednošću 37% za rano prepoznavanje pacijenata koji će ra-zviti neurološke komplikacije15.
Na osnovu rezultata navedenih istraživanja, do-lazi se do saznanja da bi primena cerebralne oksi-metrije kod nekih bolesnika, s obzirom na nisku pozitivnu prediktivnu vrednost, dovela do nepo-trebne primene šanta tokom operacije karotidne arterije, kod pada rSO2 većeg od 15–20% u odnosu na bazalnu početnu vrednost. Iz navedenih razlo-ga, u većini centara rSO2 se koristi primarno, u cilju optimizacije kardiovaskularnog statusa bolesnika, a ne kao indikacija za plasiranje šanta12.
Prema našem iskustvu, pad rSO2 može da pret-hodi epizodi cerebralne ishemije i neophodnosti plasiranja šanta u roku od nekoliko minuta12. Ali pre odluke da li je šant potrebno plasirati ili ne, ne-ophodna je primena drugih mera za optimizaciju

180 SJAIT 2018/7-8
rSO212. Naime, pad rSO2 predstavlja upozoravajući
znak za nastanak cerebralne ishemije, koja je u po-četku reverzibilna, ukoliko se primene mere koje utiču na dotok kiseonika do mozga i nivo moždane potrošnje kiseonika12,16–18. Dejstvom na faktore koji utiču na dopremenje kiseonika do moždanih ćelija (povećanje cerebralnog i sistemskog srednjeg arte-rijskog pritiska, povećanje parcijalnog pritiska ki-seonika u arterijskoj krvi, minutnog volumen srca, inspiratorne frakcije kiseonika, nivoa hemoglobina u krvi) ili smanjenjem cerebralne potrošnje kiseo-nika (povećanje dubine anestezije) primena šanta može i da se izbegne12,18,19. U skladu sa navedenim, razvijen je i algoritam za primenu cerebralne ok-simetrije kod bolesnika podvrgnutih karotidnoj hirurgiji, a na osnovu već ustanovljneog algoritma za primenu cerebralne oksimetrije kod kardiohi-rurških bolesnika18,19.
Naše iskustvoU našoj bolnici smo analizirali 94 pacijenata
kod kojih je operisana unutrašnja karotidna arte-rija u opštoj anesteziji i kod kojih je korišćena ce-rebralna oksimetrija (INVOS; Somanetics Corp) za cerebralni monitoring. Smanjenje rSO2 > 20% posle klemovanja unutrašnje karotidne arterije je korišćeno kao kritična granična tačka za primenu mera koje utiču na hemodinamski profil i eventu-alno plasiranje šanta. Od 94 bolesnika, 9 je poka-zalo smanjenje rSO2 veće od 20% posle klemovanja unutrašnje karotidne arterije12. Kod svih bolesnika je postignuta optimizacija odnosa cerebralnog do-toka kiseonika i potrošnje kiseonika i operacija je uspešno završena, bez neželjenih neuroloških do-gađaja u različitim fazama postoperativnog perio-da12.
Ograničenja primeneBrojni su faktori koji limitiraju upotrebu ove
metode za intraoperativni neuromonitoring kod bolesnika u karotidnoj hirurgiji. Pre svega, senzori su postavljeni iznad frontalnih režnjeva i ne mogu da detektuju promene krvnog protoka u zadnjoj moždanoj arteriji. Takođe, NIRS nije koristan za detekciju embolizacija, a koje su značajan uzrok neurološkog neželjenog ishoda operisanih bole-snika. Pored toga, na signal koji se registruje može da utiče krvni protok iz okolnih tkiva, kao i osve-tljenje iz ambijentalnog okruženja.
ZaključakMonitoring promena rSO2 merenih NIRS-om
tokom operacije unutrašnje karotidne arterije je koristan kao monitoring trenda za predikciju ra-zvoja cerebralne ishemije u ograničenom obimu. Ne postoji specifična apsolutna vrednost rSO2 koja bi se definisala kao kritična vrednost ispod koje se razvija cerebralna ishemija. Smanjenje rSO2 posle klemovanja unutrašnje karotidne arterije veće od 20% ima visoku negativnu prediktivnu vrednost – ako se rSO2 ne smanjuje, ishemija je malo verovat-na; ali nisku pozitivnu prediktivnu vrednost – pad rSO2 ne ukazuje uvek na prisustvo cerebralne ishe-mije.
Reference:1. Ritter JC, Tyrrell MR. Carotid endarterectomy: where
do we stand at present? Curr Opin Cardiol 2013; 28:619–24.2. Ricotta JJ, AbuRahma A, Ascher E, et al. Updated Soci-
ety for Vascular Surgery guidelines for management of extra-cranial carotid disease. J Vasc Surg 2011; 54:e1–e31.
3. Unić-Stojanović DR. Uloga kopeptina kao dijagno-stičkog i prognostičkog biomarkera u karotidnoj hirurgiji [Doctoral Dissertation]: Univerzitet u Beogradu, Medicinski fakultet; 2016.
4. Unic-Stojanovic D, Babic S, Neskovic V. General versus regional anesthesia for carotid endarterectomy. J Cardiotho-rac Vasc Anesth 2013; 27:1379–83.
5. Unić-Stojanović D, Radak D, Gojković T, et al. Anest-hesia for carotid endarterectomy: where do we stand at pre-sent? Signa Vitae 2015; 10:22–35.
6. Guay J, Kopp S. Cerebral monitors versus regional anesthesia to detect cerebral ischemia in patients undergo-ing carotid endarterectomy: a meta-analysis. Can J Anaesth 2013; 60:266–79.
7. Group GTC. General anaesthesia versus local anaest-hesia for carotid surgery (GALA): a multicentre, randomised controlled trial. The Lancet 2009; 372:2132–42.
8. Pandit JJ, Bree S, Dillon P, et al. A comparison of super-ficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: a prospective, randomized study. Anesth Analg 2000; 91:781–6.
9. Samra SK, Dy EA, Welch K, et al. Evaluation of a cere-bral oximeter as a monitor of cerebral ischemia during caro-tid endarterectomy. Anesthesiology 2000; 93:964–70.
10. Jović M, Unić-Stojanović D, Isenović E, et al. Anest-hetics and cerebral protection in patients undergoing carotid endarterectomy. J Cardiothorac Vasc Anesth 2015; 29:78–84.
11. Chongruksut W, Vaniyapong T, Rerkasem K. Routine or selective carotid artery shunting for carotid endarterecto-my (and different methods of monitoring in selective shun-ting). Cochrane Database Syst Rev 2014; 23(6):CD000190.
12. Radak D, Sotirović V, Obradović M, et al. Practical use of near-infrared spectroscopy in carotid surgery. Angio-logy 2014; 65(9):769–72.
13. Baikoussis NG, Karanikolas M, Stavros Siminelakis S, et al. Baseline cerebral oximetry values in cardiac and va-

181scular surgery patients: a prospective observational study. J Cardiothorac Surg 2010; 5(41).
14. Zarić B, Obradović M, Unić-Stojanović D, et al. Near--Infrared Spectroscopy as a Tool to Detect Cerebral Ischemia during Carotid Surgery. In Advances in Medicine and Bio-logy, Editors: Leon V. Berhardt, E-book ISBN: 978-1-53613-348-6, 2018; 129.
15. Mille T, Tachimiri ME, Klersy C, et al. Near infrared spectroscopy monitoring during carotid endarterectomy: which threshold value is critical? Eur J Vasc Endovasc Surg 2004; 27(6):646–50.
16. Obradović M, Bogdanović N, Stanimirović J, Unić--Stojanović D, et al. Hypothesis related to the regulation of in-
ducible nitric oxide synthase during carotid endarterectomy. Medical Hypotheses (2018), doi: https://doi.org/10.1016/j.mehy. 2018. 10. 011 (u štampi).
17. Denault A, DeschampsA, MurkinJM. A proposed algorithm for the intraoperative use of cerebral near-infra-red spectroscopy. Semin Cardiothorac Vasc Anesth 2007; 11(4):274–81.
18. Zogogiannis ID, IatrouCA, Lazarides MK, et al. Eva-luation of an intraoperative algorithm based on near-infrared refracted spectroscopy monitoring, in the intraoperative de-cision for shunt placement, in patients undergoing carotid en-darterectomy. Middle East J Anaesthesiol 2011; 21(3):367–73.
PERIPROTETSKE INFEKCIJE – ČINIMO LI SVE DA IH PREPOZNAMO I SPREČIMO?

doi:10.5937/sjait1806143MISSN 2466-488X (Online)
Autor za korespondenciju: Marija Milenković, Centar za anestezi-ologiju, Klinički centar Srbije, Pasterova 2, 11000 Beograd, Telefon: +381658266740, E-mail: [email protected]
Corresponding author: Marija Milenković, Centar za anesteziolo-giju, Klinički centar Srbije, Pasterova 2, 11000 Beograd, Telephone: +381658266740, E-mail: [email protected]
Revijalni članak Review article
ULTRAZVUK PLUĆA – DRUGI DEO (ULTRAZVUK PLUĆA deo 2)
Marija Milenković1, Jovana Stanisavljević1, Adi Hadžibegović1, Gregor Prosen2, Dragan Mašulović3, Milica Stojadinović3
1Centar za anesteziologiju, Klinički centar Srbije, Beograd, Srbija 2Storitve-Enote-Nujna Medicinska pomoč, Zdravstveni dom dr. Adolfa Drolca, Maribor, Slovenija 3Centar za radiologiju i MR, Klinički centar Srbije, Beograd, Srbija
LUNG ULTRASOUND – PART TWO (LUNG ULTRASOIND part 2)
Marija Milenković1, Jovana Stanisavljević1, Adi Hadžibegović1, Gregor Prosen2, Dragan Mašulović3, Milica Stojadinović3
1Center for anesthesia, Clinical Center Serbia, Belgrade, Serbia 2Storitve-Enote-Nujna Medicinska pomoč, Zdravstveni dom dr. Adolfa Drolca, Maribor, Slovenia 3Center for radiology and MRI, Clinical Center Serbia, Belgrade, Serbia
Sažetak
Klinička upotreba ultrazvuka pluća (lung ultrasound – LUS), u hitnim stanjima i pri lečenju kritično obolelih, poprima sve veći značaj i sve više se proučava. LUS je neinvazivna, real-ti-me metoda, jednostavna i dostupna „pored kreveta bolesnika” tehnika (bedside), ekonomična, nema zračenja niti komplika-cija. Prednosti LUS-a mogu da dovedu do smanjenja potrebe za radiografijom pluća i kompjuterizovanom tomografijom. Prva Međunarodna koncenzus konferencija za ultrazvuk pluća (International Consensus Conferention of Lung Ultrasound – ICC-LUS) dala je preporuke za jedinstveni pristup i termine za šest glavnih polja LUS-a. BLUE protokol (Bedside Lung Ultra-sound in Emergency Protocol) prvi je LUS sistematski pristup u dijagnostici pleuralne i plućne patologije. Ovaj protokol poma-že u diferencijalnoj dijagnozi akutne dispneje (plućnog edema, pneumonije, akutnog respiratornog distres sindroma, plućne embolije, pleuralnog izliva ili pneumotoraksa). Ultrazvuk plu-ća, u cilju dijagnostike pneumotoraksa, postao je i standardni deo proširenog ultrazvučnog protokola za traumu (Extended Focused Assessment by Sonography for Trauma – E-FAST). Tumačenje ultrazvučnog nalaza na plućima se zasniva na identifikaciji glavnih patoloških supstrata plućnog parenhima: intersticijalni sindrom, intersticijalno-alveolarni sindrom, alve-olarni sindrom / konsolidacija, pleuralni izliv i pneumotoraks.
Ključne reči: ultrazvuk pluća; BLUE protokol; E-FAST; pato-loški supstrat
Summary
Clinical use of lung ultrasound (LUS) in emergency and criti-cal care is studied extensively. LUS is a non-invasive, real-time method, easily available at bedside, economical, free of radia-tion hazard and free of complications. All these features make LUS useful in reducing need for bedside chest radiography and computed tomography. The First International Conference on Lung Ultrasound (ICC-LUS) recommended approach to six major areas of LUS. The BLUE protocol (Bedside Lung Ultra-sound and Emergency Protocol) is the first LUS-based system-atic approach in diagnosing pleural and lung pathology. This protocol helps to differentiate features of acute dyspnea (pulmo-nary edema, pneumonia, acute respiratory distress syndrome, pulmonary embolism, pleural effusion or pneumothorax). LUS for pneumothorax diagnosis has become the standard part of the Extended Focused Assessment by Sonography for Trauma (E-FAST). Interpretation of lung ultrasound findings is based on the identification of the main pathological substrates of pulmonary parenchyma: interstitial syndrome, interstitial-al-veolar syndrome, alveolar syndrome / consolidation, pleural effusion and pneumothorax.
Key words: lung ultrasound; BLUE protocol; E-FAST; patho-logical substrate
Uvod
Klinička upotreba ultrazvuka pluća (lung ul-trasound – LUS) ima brojne prednosti nad
ostalim dijagnostičkim metodama i poprima značaj u diferencijalnoj dijagnostici akutne res-piratorne insuficijencije. Radiografija pluća je di-
jagnostička metoda koja se uz anamnezu i status standardno najčešće koristi u dijagnostici nasta-le dispneje. Međutim, često postoji potreba i za kompjuterizovanom tomografijom, kao zlatnim standardom. Ovi dijagnostički postupci mogu da budu od velike koristi pri lečenju, ali sa druge strane imaju i mnogo mana. To su: velike količi-

184 SJAIT 2018/7-8
ne zračenja koje pacijent primi tokom snimanja, ograničena upotreba kod trudnica, dece i agitira-nih pacijenata, potreba za većim brojem eduko-vanog osoblja i transport pacijenta sa odeljenja do uređaja za snimanje, što može da bude rizično za kritično obolele pacijente. LUS je neinvazivna metoda, ekonomična, pristupačna i bezbedna, nema komplikacija i zračenja, sa istovremenim uvidom u rezultat pretrage. Prva Međunarod-na koncenzus konferencija za ultrazvuk pluća (International Concesus Conferention of Lung Ultrasound – ICC-LUS) dala je preporuke za je-dinstveni pristup i termine za šest glavnih polja LUS1. Uvođenje BLUE protokola, kao vodiča za dijagnostiku akutne respiratorne insuficijencije, ima za cilj da smanji primenu radiografije pluća i srca i CT-a grudnog koša u jedinici intezivnog le-čenja2. Ultrazvuk pluća, u cilju dijagnostike pne-umotoraksa, postao je i standardni deo prošire-nog ultrazvučnog protokola za traumu (Extended Focused Assessment by Sonography for Trauma – E-FAST)3,4. Tumačenje ultrazvučnog nalaza na plućima se zasniva na identifikaciji glavnih pato-loških supstrata na nivou plućnog parenhima, kao što su intersticijalni sindrom, intersticijalno-alve-olarni sindrom, alveolarni sindrom/konsolidaci-ja, pleuralni izliv i pneumotoraks.
Šta treba da znamo pre početka? (3P)3P predstavlja jednostavnu tehniku memori-
sanja, započinjanja i izvođenja ultrazvučnog pre-gleda, uključujći i LUS. Obuhvata Probe – sondu, Position – poziciju za akustički prozor i Picture – sliku patološkog supstrata (Slika 1).
Prilikom pregleda zida grudnog koša i plućnog parenhima, koristi se visokofrekventna linearna son-da (5–17 MHz). Za evaluaciju pluća interkostalnim, subkostalnim i parasternalnim pristupom je najpri-kladnija konveksna sonda (3,5–5 MHz) ili sektorska sonda sa optimalnom penetracijom. Pregled se radi u M ili B modu, u zavisnosti od indikacije.
Prednjom i zadnjom aksilarnom linijom uz sternum i kičmeni stub, grudni koš je podeljen na vertikalna polja. Povlačenjem linije kroz sredinu grudnog koša, deli se i na poprečna polja. Tako se dobija 12 polja na grudnom košu, a oni odgovaraju plućnim lobusima.
LUS je zasnovan na postojanju artefakata prilikom prolaska ultrazvučnih talasa. „A linije”, „B linije” i „klizanje” pleure su nalazi koji upućuju na razne patološke supstrate u plućnom parenhimu.
Ultrazvučno tumačenje patološkog supstrata na plućima
Normalna pluća Normalan nalaz pluća na ultrazvuku karakte-
riše prisustvo „klizanja” pleure, vidljive „A linije” i odsustvo „B linija” (Slika 2).
Intersticijalni sindromIntersticijalni sindrom označava stanje u ko-
jem intersticijum sadrži više tečnosti, odnosno edem pluća koji može da bude posledica hemodi-namskog preopterećenja – edem pluća u insufici-jenciji levog srca ili povećane propustljivosti kapi-lara u ARDS-u. Ultrazvučno su vidljive „B-linije” obostrano, a vizualizuju se na 7 mm5 (Slika 3).
Intersticijalno-alveolarni sindromOvaj sindrom se odlikuje još većom količinom
tečnosti u intersticijumu, koja je delom prisutna i u alveolama. Vidljive „B linije” su prisutne jedno-strano, zastupljene su više nego u intersticijalnom sindromu, zgusnuto su raspoređene, a ponekad i konfluiraju (Slika 4).
Alveolarni sindromOznačava konsolidaciju plućnog parenhima u
kojem su alveole u celosti ispunjene tečnim sadr-žajem (eksudat, transudat, krv, voda) i ne postoji aeracija alveola. „B linije” se vizualizuju na 3 mm5. Karakterističan ultrazvučni nalaz je ehogen, pod-seća na tkivo jetre, pa se naziva znak hepatizacije (Slika 5).
Pleuralni izlivPleuralni izliv označava prisustvo tečnog sadr-
žaja (transudat, eksudat, krv, gnoj) u pleuralnoj šu-pljini. Ultrazvučno se vidi kao anehogeni prostor. U nekim slučajevima može da se vidi i kao ehoge-no područje, ukoliko se radi o eksudatu (Slika 6).
PneumotoraksPneumotoraks predstavlja prisustvo vazduha
u pleuralnom prostoru. U normalnim plućima, kretanje visceralne preko parijetalne pleure, u skla-du sa srčanom radnjom i respiratornim ciklusom, ultrazvučno se označava kako znak „klizanja” plu-ća („lung sliding”) na B modu, a kao znak „mor-ske obale” („seashore sign”) na M modu (Slika 7). Ultrazvučni nalaz pneumotoraksa, posledično, ka-rakteriše odsustvo „klizanja” pluća. Prikaz granice pneumotoraksa, odnosono mesta gde se ponovo uočava „lung sliding” je vrlo specifičan znak za pneumotoraks. Izostanak prikaza „klizanja” pleu-re, uz nalaz „A linija”, zajedno sa znakom prikaza granice pneumotoraksa, ima visoku senzitivnost i specifičnost za dijagnostiku pneumotoraksa6.

185SPECIFIČNOSTI TERAPIJE AKUTNOG POSTOPERATIVNOG BOLA U ZEMLJAMA U RAZVOJU
Uloga ultrazvuka pluća u diferencijalnoj di-jagnostici akutne respiratorne insuficijencije
Francuski lekar Lichtenstein je razvio dijagno-stički algoritam koji omogućava nalaženje uzroka dispneje, vodeći se prethodno opisanim principi-ma ultrazvuka pluća. Ime ovog algoritma je BLUE protokol (Bedside Lung Ultrasound in Emergen-cy) (Slika 8)7. Ukratko, BLUE protokol koristi LUS i ultrazvuk vena za postavljanje diferencijalne dija-gnoze akutne respiratorne insuficijencije8. U algo-ritmu se ultrazvukom pluća procenjuje postojanje tri osnovna nalaza: „klizanje” pleure, artefakti („A linije” i „B linije”) i alveolarna konsolidacija ili ple-
uralni izliv. Pre sprovođenja algoritma, potrebno je razlikovati ultrazvučne nalaze koje je Lichtenstein kategorizovao u sedam bazičnih tipova, odnosno profila:
1. A profil predstavlja kombinaciju „klizanja” pleure i „A linija” na prednjem zidu. A pro-fil predstavlja normalnu površinu pluća.
2. B profil odlikuje „klizanje” pleure i „B lini-je”, odnosno artefakti po tipu repa komete.
3. A’ profil je A profil uz odsustvo „klizanja” pleure.
4. B’ profil je B profil uz odsustvo „klizanja” pleure.
Slika 1: Izbor sonda, pozicija pacijenta za pregled i položaj pacijenta (3P)

186 SJAIT 2018/7-8
Slika 2: Normalan nalaz pluća sa paralelnim „A linijama”, obostrano
Slika 3: Intersticijalni sindrom – jasno vidljive hiperehogene „B linije”

187
5. C profil predstavlja konsolidaciju pluća.6. AB profil odlikuje A profil na jednom pluć-
nom krilu i B profil na drugom plućnom krilu.
7. PLAPS je engleska skraćenica za postero-lateralni alveolarni i/ili pleuralni sindrom, što predstavlja alveolarnu konsolidaciju ili pleuralni izliv.
Široka upotreba BLUE protokola se zasniva na njegovoj jednostavnosti. Na osnovu algoritma, prvo je potrebno da se utvrdi da li postoji „kliza-
nje” pleure. Ukoliko je ovaj znak prisutan, isklju-čena je dijagnoza pneumotoraksa. Sledeći korak je traženje anteriorne „B linije”. U ovom trenutku određujemo o kojem se tipu (profilu) ultrazvučnog nalaza radi. Ukoliko je prisutan A profil i posto-ji duboka venska tromboza, vrlo je verovatno da se radi o plućnom embolizmu. U slučaju da ven-ska tromboza nije verifikovana, potrebno je da se potraži PLAPS. A profil sa PLAPS-om upućuje na pneumoniju, a bez PLAPS-a na egzacerbaciju hro-nične opstruktivne plućne bolesti ili astme. B profil
SPECIFIČNOSTI TERAPIJE AKUTNOG POSTOPERATIVNOG BOLA U ZEMLJAMA U RAZVOJU
Slika 4: Intersticijalno-alveolarni sindrom – „B linije” jednostrano, ukazuju na konsolidaciju
Slika 5: Alveolarni sindrom – znak hepatizacije

188 SJAIT 2018/7-8
Slika 6: Pleuralni izliv
Slika 7: Znak „morske obale” na M modu

SJAIT 2018/7-8 189
ukazuje na postojanje edema pluća. Karakteristi-ke „B linija” pomažu pri razlikovanju kardiogenog plućnog edema i ARDS-a9. A/B, B’ i C profil upu-ćuju na pneumoniju. Ukoliko klizanje pleure nije prisutno i prisutne su A linije, potrebno je da se potraži granica pneumotoraksa. U odsutstvu gra-nice, potrebne su dalje pretrage (A’ profil).
BLUE protokol algoritam se pokazao kao tačan u pronalaženju uzroka akutne respiratorne insufici-jencije kod oko 90% slučajeva10. Senzitivnost ovog protokola je 97%, a specifičnost 95% za plućni edem, dok je za plućnu emboliju senzitivnost 81%, a specifičnost 99%. U slučaju pneumonije senzitiv-nost je 89%, a specifičnost 94%. Kada je pneumoto-
raks u pitanju, protokol daje senzitivnost od 88%, a specifičnost je 100%. Postavljanje dijagnoze za eg-zarcerbaciju HOBP ili teške astme ima senzitivnost 89%, a specifičnost 97% (Tabela 1).
BLUE protokol može da se primeni za različi-te indikacije: trauma11, neonatologija12,13,14 i ARDS. Ultrasonografija može biti korisna u merenju pluć-nog rekrutmenta15.
FALLS protokol (Fluid Administration Limi-ted by Lung Sonography)
Primena LUS-a uz pomoć FALLS protokola, koji se zasniva na Veilsovoj klasifikaciji šoka, po-maže u proceni potrebe za nadoknadom volume-
Slika 8: BLUE protokol – algoritam pokazuje diferencijalne dijagnoze akutne respiratorne insuficijencije
Tabela 1: Senzitivnost i specifičnost BLUE protokola u poređenju sa MDCT kao zlatnim standardom10
Uzrok dispneje Senzitivnost (%) Specifičnost (%)Plućni edem 97 65Egzercerbacija HOBP ili teška astma 89 97Plućna embolija 81 99Pneumotoraks 88 100Pneumonija 89 94

190 SJAIT 2018/7-8
na16. Kombinovanje BLUE protokola i orijentaci-one ehosonografije omogućava jednostavnu dife-rencijaciju vrsta šoka. On započinje potragom za perikardnim izlivom ili uvećanjem leve komore, a zatim za A’ profilom. To može da isključi perikard-nu tamponadu, emboliju pluća i pneumotoraks, što predstavlja uzorke opstruktivnog šoka. Ukoli-ko BLUE protokol ne pokaže „B linije”, možemo da isključimo plućni edem, a sledstveno tome i kardi-ogeni šok.
Pacijenti kod kojih je prisutan A profil se nazi-vaju FALLS responderi – imaće pozitivan odgovor na nadoknadu tečnosti. To upućuje na dijagnozu hipovolemijskog ili distributivnog šoka (septični šok). Ukoliko posle nadoknade tečnosti dođe do poboljšanja hemodinamskih parametara, u pitanju je hipovolemijski šok. Ako se radi o non-respon-derima, dijagnoza može da ide u pravcu distri-butivnog šoka. FALLS protokol omogućava brzu orijentaciju o primeni terapije, uključujući nadok-nadu volumena, primenu vazopresora ili diuretika (Slika 9).
ZaključakUltrazvuk pluća u okviru BLUE protokola omo-
gućava jednostavnu i brzu diferncijalnu dijagnozu akutne respiratorne insuficijencije. Brojne studije upućuju na značaj upotrebe LUS kod kritično obo-lelih pacijenata i u hitnim stanjima. Iz svega proisti-če zaključak da bi upotreba ultrasonografije pluća u našim ustanovama trebalo da bude češća. Takođe, potrebna su nova istraživanja na polju dijagnostike i upotrebe LUS-a u jedinici intezivnog lečenja.
Izjave zahvalnostiAutori se zahvaljuju doktoru Gregoru Prošenu
i Win Focus Sloveniji što su nam dozvolili da kori-stimo njihove slike.
Literatura 1. Saraogi A. Lung ultrasound: present and future. Lung
India 2015; 32 (3):250–257.2. Lichtenstein D, Meziere G. Relevance of lung ultraso-
und in the diagnosis of acute respiratory failure. Chest 2008; 134:117–125.
3. Lichtenstein D, Meziere G, Biderman P, et al. The lung point: an ultrasound sign specific to pneumothorax. Intensi-ve Care Med 2000; 26:1434–1440.
Slika 9: FALLS protokol

SJAIT 2018/7-8 1914. Podlesnik A, Privsek M, Nikolic S, Arva V, Petrovic R,
Banovic T, et al. PACE: POCUS Assisted Clinical Examina-tion – A Modular Curiculum for teaching Point-of-Care Ul-trasound to undregaduate med. Students. [email protected],first edition, september 2016.
Stojadinovic M, Filipovic A, Zakošek M, Bulatovic D, Masulovic D. Lung ultrasound – part one. SJAIT 2018; 40(5–6):149–158.
5. Staub LJ, Biscaro RRM, Kaszubowski E, Maurici R. Chest ultrasonography for the emergency diagnosis of tra-umatic pneumothorax and haemothorax: A systematic revi-ew and meta-analysis. Injury 2018; 49(3):457–466.
6. Lichtenstein D, Mezière G. The BLUE-points: three standardized points used in the BLUE-protocol for ultraso-und assessment of the lung in acute respiratory failure. Crit Ultrasound J 2011; 3:109–110.
7. Lichtenstein D, Mezière G. Relevance of lung ultraso-und in the diagnosis of acute respiratory failure. The BLUE--protocol. Chest 2008; 134:117–125.
8. Lichtenstein D.Lung ultrasound in the critically ill. Curr Opin Crit Care 2014; 20(3):315–322.
9. Lichtenstein DA, Mezière GA. Relevance of lung ultra-sound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 2008; 134(1):117–25.
10. Lichtenstein D, Courret JP. Feasibility of ultrasound in the helicopter. Intensive Care Med 1998; 24:1119.
11. Copetti R, Cattarossi L. The „double lung point”: an ultrasound sign diagnostic of transient tachypnea of the ne-wborn. Neonatology 2007; 91:203–209.
12. Lichtenstein D. Ultrasound examination of the lungs in the intensive care unit. Pediatr Crit Care Med 2009; 10:693–698.
13. Lichtenstein D, Mauriat P. Lung ultrasound in the cri-tically ill neonate. Curr Pediatr Rev 2012; 8:217–223.
14. Bouhemad B, Brisson H, Le-Guen M, et al. Bedside ultrasound assessment of positive end-expiratory pressure--induced lung recruitment. Am J Respir Crit Care Med 2011; 183:341–347.
15. Lichtenstein D. FALLS-protocol: lung ultrasound in hemodynamic assessment of shock. Heart Lung Vessels 2013; 5:142–147.

Autor za korespondenciju: Lazar Bralušić, Mitrovo brdo, Nova 1, broj 1/4, Telefon: 064/2001331, E-mail: [email protected]
Corresponding author: Lazar Bralušić, Mitrovo brdo, Nova 1, br 1/4, Telephone: 064/2001331, E-mail: [email protected]
Sažetak
Uvod: Totalna aloartoplastika kolena spada u najčešće i najopsežnije intervencije u ortopedskoj hirurgiji i udru-žena je sa mnogim komplikacijama. Von Willebrandova bolest nastaje zbog disfunkcije ili nedostatka vW faktora, a kao posledica se javlja smanjena sposobnost hemostaze na primarnom nivou koagulacije krvi. Dijagnozu i težinu bolesti određujemo vrednostima laboratorijskih analiza fVIII, vWfAc, vWfAg. Shodno ovim vrednostima, tera-pijska kontrola bolesti se vrši koncetratima vWf/fVIII, intravenskim putem. Prikaz slučaja: Prikazan je slučaj bolesnice stare 46 godina sa teškim (tip 3) oblikom vW bolesti i HIV infekcijom. Kod nje je planirana elektivna aloartroplastika kolena. Nakon prijema na IOHB, konzi-lijarni tim je utvrdio tačan plan lečenja i kontrolu stanja osnovnih bolesti kod pacijentkinje. Izvršena je preopera-tivna kontrola specifičnih laboratorijskih analiza, fVIII, vWfAc, a zatim planska nadoknada vWf/fVIII koncetra-ta u preoperativnom, intra i postoperativnom periodu. Intervencija je izvedena u uslovima opšte anestezije, sa pažljivom kontrolom perioperativnog krvarenja, antifi-brinoliticima i Turnike poveskom. U postoperativnom pe-riodu je izvršena antibiotska profilaksa cefalosporinima, antiretrovirusna terapija, analgetska terapija opioidima i paracetamolom po šemi. Antikoagulantna terapija je sprovedena IPC pumpom (aparatom za stimulaciju peri-ferne cirkulacije). Šestog postoperativnog dana, bolesnica je prevedena na hematološku kliniku KCS radi dalje kon-trole osnovne bolesti. Zaključak: Organizovan tim struč-njaka, izrada plana lečenja i sprovođenje istog prevenira nastanak komplikacija ili ih blagovremeno otklanja.
Ključne reči: aloartroplastika kolena; Von Willebran-dova bolest; anestezija
Abstract
Introduction: Total knee arthroplasty is the most exten-sive and the most commonly performed orthopedic pro-cedure which can be associated with numerous complica-tions. Von Willebrand disease is caused by the missing or defective vW factor, and has lower ability of hemostasis on a primary level of cogulation as a consequence. Diagnostic category and disease severity is defined by values of fVIII, vWfAc, vWfAg. Due to these values therapeutic control of a disease is done intravenously with vWf/fVIII concentra-tes. Case Report: We presented a 46-year old patient with a severe (type 3) von Willebrand disease and HIV infecti-on that was scheduled for the total knee replacement. Af-ter hospital admition, medical team established treatment strategy for underling disease control. Preoperative control of specific laboratory parameters including fVIII, vWfAc, vWfAg was performed and detailed plan for preoperative, intraoperative and postoperative vWf/fVIII concentra-te administration was made. The total knee replacement was performed under general anesthesia with control of intraoperative bleeding by antifibrinolytic administration and tourniquet application. In the post-operative period cephalosporin was used for antibiotic prophylaxis, whilst antiretroviral therapy and analgesic therapy including opioids and paracetamol were performed according to the time-scheduled dosing. Intermittent pneumatic compressi-on (IPC) device was used as the anticoagulant therapy. On a 6th postoperative day, the patient was transferred to he-mathology department in another hospital where further monitoring of underlying disease was continued. Conclu-sion: Organized expert team, adequate treatment strategy conduction is essential for prevention and early treatment of possible complication.
Key words: total knee arthroplasty; Von Willebrand di-sease; anesthesia
doi:10.5937/sjait1806149SISSN 2466-488X (Online)
Prikaz slučaja Case report
TOTALNA ALOARTROPLASTIKA KOLENA KOD BOLESNICE SA TEŠKOM FORMOM VON WILLEBRANDOVE (FON VILEBRANDOVE) BOLESTI (PERIOPERATIVNI TRETMAN KOD VON WILLEBRANDOVE BOLESTI)
Lazar Bralušić1, Svetlana Dinić1, Andrijana Cvijović1
1Institut za ortopedsko-hirurške bolesti „Banjica”, Beograd, Srbija
TOTAL KNEE ARTHROPLASTY IN A PA-TIENT WITH SEVERE VON WILLEBRAND DISEASE (PERIOPERATIVE TREATMENT OF VON WILLEBRAND DISEASE)
Lazar Bralušić1, Svetlana Dinić1, Andrijana Cvijović1
1Institute for Orthopedic Surgery „Banjica”, Belgrade, Serbia

194 SJAIT 2018/7-8
Uvod
Totalna aloartroplastika kolena (TAK) je jedna od najčešće izvođenih ortopedskih operacija u
razvijenim zemljama sveta. Predstavlja proceduru kojom se zglobni delovi kolena zamenjuju veštač-kim komponentama1. Glavne indikacije za TAK su svakodnevni jaki bolovi i funkcionalna onesposo-bljenost2.
Von Willebrandova bolest je jedna od najčešćih urođenih bolesti krvi. Vodeći simptomi bolesti su: produženo krvarenje nakon povrede, spontana krvarenja iz sluznica, produžena menstrualna kr-varenja3. Bolest nastaje zbog urođenog ili stečenog nedostatka, kao i disfunkcije Von Willebrandovog faktora (vWF). Nasleđuje se autozomno domi-nantno (tip 1 i 2 ) ili recesivno (tip 3), a kao po-sledica mutacije na hromozomu 12. Stečena forma se javlja u sklopu limfoproliferativnih i autoimunih bolesti4. VWf je protein koji omogućava adheziju i agregaciju trombocita i kofaktor je faktora VIII5. VWf nastaje u megakariocitima i endotelnim ćeli-jama, a skladišti se u Weibel-Paladeovim telašcima endotelnih ćelija i α granulama trombocita. Kom-pleks vWf/fVIII cirkuliše krvlju i podržva adheziju i agregaciju trombocita za kolagen na mestu povre-de endotela4,5.
Tip 1, kao najčešći urođeni poremećaj koagu-lacije, karakteriše se delimičnim nedostatkom, a tip 2 nekom od disfunkija vWf. Teška forma, tip 3, predstavlja potpuni nedostatak vWf sa udruženim nedostatkom faktora VIII i spada u retke bolesti. Karakterišu je česta, spontana krvarenja u zglo-bove i mišiće, što za posledicu ima teške artroze i disfunkcije zgloba5. Pozitivna anamneza indikuje kontrolu krvnih testova, kompletne krvne slike (KKS), aktiviranog parcijalnog tromboplastin-skog vremena (aPTT), protrombinskog vremena (PT), fibrinogena, vWDAg (Willebrand factor an-tigen), vWDrCo (ristocetin kofaktor), FVIII, kao i specifičnih testova za određivanje podtipova bo-lesti. U lečenju VWB se koriste koncetrati fakto-ra VIII/vW, kao i dezmopresin u lakim formama bolesti (tip 1)6.
Prikaz slučajaBolesnica, 46 godina starosti, primljena je u
bolnicu zbog obostrane hronične sekundarne gonoartropatije. Komorbiditet je predstavljala te-
ška forma (tip 3) vW bolesti, a terapija se sastoja-la od profilaktičke terapije koncetrata vWf/fVIII (Willate®, OCTAPHARMA PHARMAZEUTIKA PRODUKTIONSGES.M.B.H, Oberlaaer Strasse 235, Beč, Austrija) u dozi od 1000–2000 i.j. jed-nom do dva puta nedeljno. Dodatno, bolesnica je HIV pozitivna već 25 godina, bez manifestaci-ja AIDS-a do pre 3 godine, na antiretrovirusnoj terapiji, hepatitis C pozitivna, sa nedektabilnom viremijom. Infektološki i reumatološki status nisu predstavljeni u preoperativnom izveštaju?, bez kontraindikacija za operativnim lečenjem (vred-nost CD 4 Ly 400/mm³, metilpredniolon po šemi). Zbog promena na malim zglobovima, uvedeni su kortikosteroidi, sa manifestovanim sekundarnim Kušingovim sindromom. Hematološki preopera-tivni izveštaj je davao jasne smernice, kontrole i nadoknade vWf/fVIII u slučaju hirurškog zahvata (trebovanje 50000 i.j. koncetrata vWf/fVIII). Pre-operativni fizikalni nalaz je ukazivao na potpuno kompenzovano stanje pacijentkinje, a laboratorij-ske analize su bile u granici referentnih vrednosti (Tabele 1 i 2).
Tabela 1: Preoperativna krvna slika
Test Vrednost Referentna vrednost
Le 10,2 3,5–10
Er 4,89 4,3–5,72
Hgb 135 130–170
Htc 0,41 0,40–0,54
Tr 252 158–425
Nakon prijema, bolesnica je pregledana od strane konzilijarnog tima, koji su činili ortoped, anestezio-log, hematolog, internista, transfuziolog, mikrobio-log. Ortopedskom odlukom je predloženo hirurško lečenje oba kolena, i to aloartroplastika levog kolena i resekciona artrodeza desnog kolena. Tokom pre-gleda je utvrđen jasan plan hematološke i interni-stičke pripreme i vođenje operativnog i postopera-tivnog perioda; anesteziološka priprema i izbor vrste anestezije, kao i postoperativna intenzivna terapija; opsežnost i način hirurškog zahvata. Odlučeno je da se bolesnica podvrgne aloartroplastici jednog kole-na, i to levog, zbog lošijeg kliničkog stanja.

195
Tabela 2: Preoperativna biohemija
Test Vrednost Referentna vrednost
Glikemija 4,5 4,10–6,20
Urea 3,9 2,80–8,30
Kreatinin 63 48,00–96,00Ukupni bilirubin 9,1 4,0–21,0
Proteini 73 64–83Albumini 41 35–52Kalcijum 2,41 2,20–2,70
Natrijum 138 136–146
Kalijum 3,7 3,5–5,3
AST 21 0–35
ALT 20 0–35
Le – leukociti, Er – eritrociti, Hgb – hemoglobin, Ast – aspar-tat transaminaza, Htc – hematokrit, Tr – trombociti, Alt – alanin transaminaza
Bolesnica je primljena u sobu za premedikaciju, 120 minuta pre početka planiranog zahvata, radi preoperativne pripreme. Plasirane su dve kanile u periferne vene, jedna za kontrolu laboratorijskih analiza, a druga za primenu koncetrata faktora. Nakon uzimanja krvi za kontrolu vWDAc, FVIII, aplicirano je 3000 i.j. koncetrata vWf/fVIII (Hae-
mate® P 1000 CSL Behring GmbH, Emil-von-Be-hring-Straße 76, 35 041 Marburg, Nemačka) u bolus dozi. Petnaest minuta od apliciranog leka, ponovo je uzeta krv za kontrolu istih analiza. Na-kon dobijenih zadovoljavajućih vrednosti, započet je planirani operativni zahvat (Tabela 3).
Metilprednizolon (40 mg) ordiniran je 12 h pre operacije, doza je ponovljena jedan sat pre operativ-nog zahvata, zajedno sa antibiotskom profilaksom po protokolu (1 g cefazolina i.v.). U premedikaciji su ordinirani ranitidin, ondasetron i midazolam (3 mg i.v.), neposredno pred ulazak u salu. Indukcija u opštu endotrahealnu anesteziju je učinjena propo-folom, u dozi od 2 mg/kg, a za održavanje aneste-zije je korišćena kombinacija sevoflurana (1 vol %) i smeše gasova O2/N2O, uz održavanje bispektral-nog indeksa, u intervalu između 40–60. Analgezija je postignuta fentanilom (3–5 μg/kg/h), a mišićna relaksacija rokuronijumom (0,6 mg/kg/h). Praćen je neinvazivni monitorng arterijskog krvnog priti-ska, saturacije arterijske krvi, pulsa, kapnografije i elektrokardiografija. Nakon uvoda u opštu aneste-ziju, plasiran je dvolumenski centralni venski ka-teter u desnu jugularnu venu, za primenu tečnosti i lekova tokom anestezije. Učinjena je bleda staza leve noge i postavljena je poveska za kontrolu kr-varenja. Nakon toga, pristupilo se hirurškom rezu i operativnom zahvatu. Petnaest minuta pre ukla-njanja poveske, ordinirana je traneksamična kise-lina, u dozi od 15 mg/kg. Hirurška intervencija je
ULTRAZVUK PLUĆA – PRVI DEO
Tabela 3: Preoperativni specifični koagulacioni skrining
Vrednost 24 h nakon Th održavanja
PreoperativnoReferentne vrednosti
Pre Th Nakon Th
VWF Ac 12,8% < 4% 150% 50–150%
F VIII
APTT
FIBRINOGEN
PT
110%
30,0
7,77
103%
21%
41,6
7,78
96%
170%
29,8
7,44
98%
60–150%
25,1–36,5
2,00–5,50
75–120%
vWf – von Willebrandov faktor, fVIII – fakor VIII, APTT – aktivirano parcijalno tromboplastinsko vreme, PT – protrom-binsko vreme, Th – terapija

196 SJAIT 2018/7-8
trajala 1 h i 20 minuta. Nakon završene operacije, bolesnica je budna, spontanog disanja, ekstubirana je i smeštena u jedinicu intenzivnog lečenja (JIL) na dalju opservaciju. Po prijemu u JIL je ordini-rano 1000 i.j. Haemate® P 1000. Na svakih 8 sati je ordinirano po 1500 i.j. ovog koncentrata u pe-riodu od prvih 48 sati nakon operacije. Bolesnica je postoperativno bila stabilnih vitalnih parameta-ra, (pritisak 110/60 mmHg, srčana frekvencija 67/min, SpO2 97%), spontane diureze, drenaže manje od 100 ml/u prvih 2 h postoperativno. Kontrolna krvna slika i biohemija, dva sata nakon završenog zahvata, bile su u granicama referentnih vrednosti (Tabela 4 i 5).
Tabela 4. Postoperativna krvna slika
Test Vrednost Referentna vrednost
Le 12,2 3,5–10
Er 3,33 4,3–5,72
Hgb 118 130–170
Htc 0,29 0,40–0,54
Tr 190 158–425
Tabela 5: Postoperativna biohemija
Test Vrednost Referentna vrednost
Glikemija 7,37 4,10–6,20
Urea 3,01 2,80–8,30
Kreatinin 60,85 48,00–96,00Ukupni bilirubin 11,6 4,0–21,0
Proteini 59 64–83Albumini 32 35–52Kalcijum 2,13 2,20–2,70
Natrijum 140 136–146
Kalijum 38 3,5–5,3
AST 32 0–35
ALT 31 0–35Le – leukociti, Er – eritrociti, Hgb – hemoglobin, AST – aspa-trat transaminaza, Htc – hematokrit, Tr – trombociti, Alt – alanin transaminaza
U postoperativnom periodu je ordinirana anti-biotska profilaksa po ortopedskom protokolu in-stituta, cefazolinom 1 g i.v. na 6 sati. Analgetska te-rapija je postignuta paracetamolom, 1 g i.v. na 6 h, morfinom 2–3mg i.v. na 4 h, oralnim morfinom 10 mg per os po potrebi (pacijentkinji su ordinirane dve doze oralnog opioidnog analgetika u trenuci-ma proboja bola tokom prvih 24 h). Metilpredni-zolon u dozi od 40 mg je ponovljen 12 h nakon preoperativne doze. Ponovljena je doza od 1 g tra-neksamične kiseline, 8 h nakon prve doze. Apliko-van je IPC (intermitentna pneumatska kompresi-ja) aparat na neoperisanu nogu, radi stimulacije periferne cirkulacije. Prvog postoperativnog dana, pre jutarnje doze Haemate® P 1000, uzeta je krv za proveru vWDAc, fVIII, a zatim je aplikovan kon-cetrat faktora. Nakon dobijenih vrednosti, doza koncetrata je redukovana na prosečno 1000 i.j. / 12 h i.v. od trećeg do šestog postoperativnog dana. U tabeli 6 su prikazane vrednosti vWDAc, FVIII pr-vog i petog postoperativnog dana.
Tabela 6: Postoperativni specifični koagulacioni skrining
1. postope-rativni
dan
5. postope-rativni
dan
Referentne vrednosti
VWF Ac 105% 84% 50–150%
F VIIIAPTTFIBRINOGENPT
165%26,95,7885%
199%29,57,16114%
60–150%25,1–36,52,00–5,5075–120%
vWf – von Willebrandov faktor, fVIII – fakor VIII, APTT – aktivirano parcijalno tromboplastinsko vreme, PT – pro-trombinsko vreme
Pored navedene terapije, ponovo je uključena antiretrovirusna terapija i kortikosteroid Calcort 3 mg per os x 1. U analgetskoj terapiji više nije po-stojala potreba za korišćenjem oralnog opiodnog preparata. Drugog postoperativnog dana, nakon jutarnje vizite, bolesnica je prebačena na odeljenje. Bila je hemodinamski stabilna, urednih vitalnih parametara, sa drenažom 200 ml / 24 h. Analize KKS i biohemije su bile u granicama referentnih vrednosti (Tabela 7 i 8). IPC aparat je postavljen i na operisanu nogu. Analgetska terapija je spro-vedena paracetamolom 1 g / 8 h i.v. Antibiotska profilaksa cefazolinom je produžena do šestog postoperativnog dana, po preporuci ordinirajućeg

197
infektologa, kada je bolesnica prebačena na hema-tološko odeljenje u drugu bolnicu, radi dalje kon-trole osnovne bolesti.
Tabela 7: Krvna slika pre otpusta
Test Vrednost Referentna vrednost
Le 11,9 3,5–10
Er 3,9 4,3–5,72
Hgb 106 130–70
Htc 0,34 0,40–0,54
Tr 232 158–425
Tabela 8: Biohemija pre otpusta
Test Vrednost Referentna vrednost
Glikemija 5,8 4,10–6,20
Urea 4,74 2,80–8,30
Kreatinin 60,40 48,00–96,00Ukupni bilirubin 7,6 4,0–21,0
Proteini 50 64–83
Albumini 32 35–52
Kalcijum 2,19 2,20–2,70
Natrijum 138 136–146
Kalijum 3,6 3,5–5,3
AST 34 0–35
ALT 26 0–35
DiskusijaTotalna aloartroplastika kolena je, iako jedna
od najčešćih ortopedskih intervencija, udružena sa intra i postoperativnim komplikacijama. Rizik od nastanka komplikacija i mortaliteta se povećava ukoliko se u jednom hirurškom aktu izvede alo-artroplastika oba kolena1,2,7. Preoperativna odluka konzilijarnog tima je iz tog raloga bila da, zbog brojnih teških komorbiditeta, kod bolesnice nije moguće odjednom izvesti obostranu hirurgiju.
Istraživanja su pokazala da dugotrajna profilak-sa fVIII i vWf, ako je započeta dovoljno rano, može
da redukuje intraartikularno krvarenje, a time i nastanak artropatije kod obolelih od vW bolesti8. Naša bolesnica je imala tip 3 bolesti, kao teške for-me, te je pored profilaktične terapije fVIII i vWf, razvila promene u zglobovima. Preoperativna pri-prema ovakvog bolesnika se, prema važećim smer-nicama, sprovodi koncetratom vWf/fVIII, nakon testiranja njegove farmakokinetike, kao i određi-vanja nivoa vWDAg, vWDAc, FVIII. Samo na taj način može da se odredi najbolja doza potrebna za prevenciju krvarenja i doza održavanja pomo-ću koncentrata kod bolesnika koji se podvrgava hirurškom zahvatu6,9. Poluživot koncetrata vWf/fVIII je 12 sati, a promena njegove koncetracije kroz vreme se smatra linearnom, pa je ordiniranje vršeno na svakih 8 sati u toku operacije i postope-rativno, kako bi se održao odgovarajući nivo fakto-ra9. Haemate® P 1000 predstavlja kombinaciju od 1000 i.j. fVIII i 2400 i.j. vWf. Preporučuje se doza od 40–80 i.j. vWf / kg telesne mase i 20–40 i.j. fVI-II / kg telesne mase za postizanje hemostaze. Kod pacijenata koji imaju tip 3 vW bolesti, potrebna je početna doza od 80 i.j./kg vWf, pa i više, zavisno od vrste i opsežnosti operativnog zahvata. Vred-nosti kontrolnih, koagulacionih analiza nakon pri-mene hemokoncetrata moraju biti u referentnim granicama, da bi se prešlo na sledeći korak lečenja bolesnice tokom operativnog i postoperativnog perioda.
Antibiotska preoperativna profilaksa je učinje-na antibiotikom koji je kreiran od strane mikrobi-ologa, a na osnovu bakterijske mikroflore prisutne na institutu. Vrednost CD4+ limfocita je bila (400/mm³), daleko iznad donje granice za osobe obolele od HIV infekcije. Referentna vrednost CD4+ ly je 500–1250/mm³, a iznad 200/mm³ je kod obolelih od HIV-a10. Antiretrovirusni lekovi su isključeni operativnog dana, zbog mogućnosti interakcije sa lekovima korišćenim tokom anestezije i u nepo-srednom postoperativnom periodu (sa lekovima za kardiovaskularna oboljenja, različitim antibioti-cima, antacidima, H2 blokatorima itd.)11.
Kod obolelih od vW bolesti, kontraindikova-na je intramuskularna primena lekova12. Bitno je napomenuti da savremeni način primene lekova isključuje intramsukularnu primenu. Plasiranje CVK je obavljeno tek nakon kontrole koagulacio-nog stanja pacijentkinje, kao i vrednosti vWDAc, FVIII. Urođeni ili stečeni poremećaji koagulacije predstavljaju kontraindikaciju za izvođenje bilo
ULTRAZVUK PLUĆA – PRVI DEO

198 SJAIT 2018/7-8
koje vrste regionalne anestezije (centralnih ne-uroaksijalnih blokova, kao i perifernih blok an-estezija)13,14. Zbog toga smo se opredelili za op-štu endotrahealnu anesteziju. Kod bolesnice nije postojao poremećaj metaboličke funkcije jetre ili funkcije bubrega, pa nije bilo potrebe za redukci-jom u dozama i vrsti lekova korišćenih tokom an-estezije. U operativnom i postoperativnom peri-odu, analgetski efekat je ostvaren opioidima, koji predstavljaju osnovne analgetike kod vW bolesti. Prilikom davanja saveta o upotrebi analgetika i antipiretika kod osoba sa poremećajima hemo-staze, treba imati u vidu da su aspirin i fenilbu-tazon inhibitori ciklooksigenaze, enzima koji konvertuje arahidonsku kiselinu u tromboksan, a koji je snažan medijator agregacije trombocita, te se bolesnici moraju upozoriti da ne upotre-bljavaju ove lekove. Nesteroidni antinflamatorni lekovi, mada imaju sličan mehanizam dejstva (re-verzibilna inhibicija ciklooksigenaze), ne izaziva-ju produženje vremena krvarenja, pa stoga nisu kontraindikovani. Problem je što ovi lekovi mogu da izazovu gastrointestinalna krvarenja, što u poremećajima hemostaze može da predstavlja veliki problem. Paracetamol je lek izbora, zbog manjeg broja potencijalnih štetnih dejstava (ne-vezanih za hemostazu) u odnosu na nesteroidne antiinflamatorne lekove15. Analgetska terapija u postoperativnom periodu je kod naše bolesnice sprovedena kao kombinacija opioidnih lekova i paracetamola po šemi (paracetamol 1 g na 6 sati, morfin 2–3 mg na 4 sata i.v. + 10 mg per os za proboj bola).
Traneksamična kiselina, koja je po funkci-ji antifibrinolitik, može da se koristi u lečenju i profilaksi krvarenja kod obolelih od vW bolesti. Primenjuje se u dozi od 10–15 mg/kg, 2–3 puta dnevno. Traneksamična kiselina se ne prime-njuje zajedno sa koncentratima kompleksa, jer može da dovede do tromboembolije16. Ona odla-že brzu razgradnju fibrina i održava formirani ugrušak stabilnim, duže nego fiziološki, pa tako sprečava krvarenje, što je posebno značajno u in-tra i neposrednom postoperativnom periodu15,16. S obzirom na određeno vreme polueliminacije koncetrata vWf/fVIII, linearni pada koncetraci-je faktora kroz jedinicu vremena, nemogućnost kretanja pacijentkinje narednih par dana nakon intervencije, kao i rizičnu hiruršku intervencije
za pojavu tromboembolijskih komplikacija, mo-rala je da se sprovede antikoagulantna terapija6. Hematolog je isključio upotrebu farmakološke antikoagulantne profilakse do petog postopera-tivnog dana, zbog mogućnosti pojačanog posto-perativnog krvarenja, kada je uveden niskomo-lekularni heparin, nadroparin – kalcijum 0,3 ml, jednom dnevno. Konzilijarni tim se odlučio za nefarmakološke metode profilakse, u periodu od operacije do petog postoperativnog dana, u formi intermitentne pneumatske kompresije. Osnovni mehanizam delovanja se zasniva na povećanju spoljašnjeg pritiska i poboljšavanju fibrinolize. Takođe, ostvaruju se hemodinamski, hematolo-ški i endotelni učinci17.
Bol posle totalne aloartroplastike kolena je ja-kog inteziteta i značajno se smanjuje nakon 48–72 sata od operacije. Efikasna kontrola bola dozvolja-va rano kretanje i započinjanje fizikalne terapije, koja ubrzava oporavak, smanjuje dužinu boravka u bolnici, smanjuje broj ponovnih hospitalizacija i snižava rizik od postoperativnih komplikacija18. Drugog postoperativnog dana, naša bolesnica je premeštena na odeljenje, intezitet bola je bio zna-čajno manji. Na numeričkoj skali za procenu bola (NRS – Numeric Rating Scale for pain) gradiran je kao nivo 4/10. Zadovoljavajući analgetski efekat kod bolesnice je postignut primenom paracetamo-la po šemi (1 g na 8 sati i.v.). Pristupilo se merama za ranu rehabilitaciju i postoperativni oporavak, po protokolu, a uz kontrolu ordinirajućeg ortope-da, interniste i hematologa.
Zaključak
Totalna aloartroplastika kolena, iako jedna od najčešćih, a po tehnici i rutinskih ortopedskih procedura, povezana je sa mnogim komplikaci-jama. Učestalost komplikacija je veća ukoliko su kod osobe prisutni dodatni komorbiditeti. Von Wilebrandova bolest, i to tip 3, kao teška, urođe-na forma, predstavlja izazov za ovu vrstu hirurgi-je, zbog potpunog nedostatka faktora vWf /fVIII i sklonosti ka nekontrolisanom krvarenju u intra i postoperativnom periodu. Ukoliko je pored ove bolesti prisutna i nekolicina dodatnih, taj izazov, kao i kompleksnost čitavog procesa raste. Dobro organizovan tim stručnjaka, izrada plana lečenja i sprovođenje tog plana, preveniraju nastanak kom-plikacija ili ih blagovremeno otklanjaju.

199ULTRAZVUK PLUĆA – PRVI DEO
Literatura1. Turki AS et al. Total knee arthroplasty: Effect of obesity
and other patients characteristics on operative duration and outcome. World J Orthop 2015 Mat 18 6(2):284–9.
2. Harwin FS et al. Indications and patient selection; sur-gical techniques in total knee arthroplasty. 1sted. New York: Springer-Verlag; 2002:3–8.
3. Berntorp E, Blombäck M. Von Willebrand Disease. Basic and Clinical Aspects. Singapore: WileyBlackwell, 2011; 1–3.
4. Franchini M. Surgical prophylaxis in von Willebrand’s disease: a difficult balance to manage. Blood Transfus 2008; 6(2):31–8.
5. Castaman G, Rodeghiero F. Advances in the diagnosis and management of type 1 von Willebrand disease. Expert Rev Hematol 2011; 4(1):95–106.
6. Michiels JJ et al. Bleeding prophylaxis for major sur-gery in patients with type 2 von Willebrand disease with an intermediate purity factor VIII-von Willebrand factor concentrate (Haemate-P). Blood Coagul Fibrinolysis 2004; 15(4):323–30.
7. Hu J et al. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthro-plasty: a meta-analysis. Arch Orthop Trauma Surg 2011; 131(9):1291–8.
8. Dolatkhah R et al. Clinical use of Haemate-P in inhe-rited von Willebrand’s disease: a patient with type 3 VWD and recurrent menometrorrhagia. Haemophilia 2010; 16(3): 555–7.
9. Franchini M. Surgical prophylaxis in von Willebrand’s disease: a difficult balance to manage. Blood Transfus 2008; 6(2):33–8.
10. Alimonti JB et al. Mechanisms of CD4+ T lympho-cyte cell death in human immunodeficiency virus infection and AIDS. J. Gen. Virol 2003; 84(7):1649–1661.
11. European AIDS Clinical Society (EACS), verija 6.1, novembar 2012; 22–23.
12. Janić D et al. Lečenje hemofilije sa inhibitorima – pri-kaz bolesnika. Bilten za hematologiju 28(1; 2/3):1–105, 200.
13. Miller RD, Millers Anesthesia, Churchill Livingstone, 2009.
14. Karadža V et al. Klinička anesteziologija i reanimato-logija, Zagreb, Katedra za anesteziologiju i reanimatologiju, 2004.
15. Zupančić Šalek S et al. Smjernice za dijagnostiku i lije-čenje hemofilije. Zagreb, FotoSoft, Krohem; 2013.
16. Hvas AM et al. Tranexamic acid combined with re-combinant factor VIII increases clot resistance to accelerated fibrinolysis in severe hemophilia A. J Thromb Haemost 2007 Dec; 5(12):2408.
17. Tarnay TJ et al. Pneumatic calf compression, fibrino-lysis, and the prevention of deep venous thrombosis. Surgery 1980; 88:489.
18. Duarte VM et al. Effectiveness of femoral nerve bloc-kade for pain control aftertotal knee arthroplasty. J Peria-nesth Nurs. 2006 Oct 21(5):311–6.

doi:10.5937/sjait1806149SISSN 2466-488X (Online)
Izveštaj o XIII Kongesu anesteziologa i intenzivista Srbije I am here / Ja sam ovde

202 SJAIT 2018/7-8

SJAIT 2018/7-8 203
U Beogradu, u hotelu Crowne Plaza, od 22. do 25. novembra 2018. godine je održan XIII Kongres anesteziologa i intenzivista Srbije, kao najznačajniji događaj u nizu aktivnosti koje su obeležile kampanju pod nazivom: Mesec anesteziologa. U isto vreme, ovo je najznačajniji stučni i naučni skup koji svake četvrte godine organizuje Udruženje anesteziologa i intenzivista Srbije (UAIS). Pored obrazovnih i stručnih tema koje su bile dostupne učesnicima, komunikacija, povezivanje i saradnja anesteziologa iz Srbije, čitavog regiona i Evrope su najznačajniji ciljevi ovog kongresa.
Osnovna ideja oko koje je osmišljen stručni program se odnosila na bezbednost bolesnika (Patient Safety) i na obrazovanje, kao jedan od osnovnih instrumenata unapređenja kvaliteta rada anesteziologa i lečenja bolesnika. Program je organizovan u nekoliko tematskih celina, koje su se održavale tokom 4 dana, kao predkongresne i kongresne aktivnosti, sa posebnim naglaskom na interaktivnost, praktične radionice i izbor najznačajnijih tema u oblasti anestezije i intenzivne terapije. Većini interaktivnih kurseva i radionica sa ograničenim brojem učesnika nije mogao da prisustvuje veliki broj zainteresovanih učesnika, što ukazuje na planiranje budućih aktivnosti i organizaciju sličnih obrazovnih sadržaja u budućnosti.
Kao predkongresne aktivnosti organizovani su: 1) Poslednji, šesti u ciklusu, CEEA kurs kontinuirane edukacije u anesteziji i intenzivnoj terapiji2) Osnovni kurs iz Fokus ehokardiografije, organizovan kao izraz saradnje UAIS-a, udruženja
WinFokus Srbija i Ehokardiografskog udruženja Srbije (Echos)3) Radionica o otežanom disajnom putu, koja je podržana od strane Evropskog udruženja za disajni
put (EAMS)4) Primena ultrazvuka u regionalnoj anesteziji 5) Simpozijum o bezbednosti bolesnika (Patient Safety Symposium), koji je po prvi put održan u
našoj zemlji.Naučni program je bio raspoređen u 10 sesija, 6 industrijskih simpozijuma, 5 radionica i interaktivnih
sesija. Organizovana je sesija simulacije kritičnog incidenta i demonstracija simulacije kao metode obrazovanja u anesteziji, radionica torakalne anestezije i primene viskoelastičnih testova za koagulaciju. Poslednja sesija je posvećena Evropskoj diplomi iz anestezije i intenzivne terapije, a završena je kvizom u kojem se takmičilo 4 ekipe iz 4 različite ustanove, a kojim je u pozitivnoj i veseloj atmosferi i okončan stručni deo kongresa. Jedan od članova pobedničkog tima je osvojio besplatno polaganje prvog, pismenog ispita EDAIC. Nagrađena je najbolja Final 4 prezentacija, a po prvi put smo uspeli da obezbedimo značajne nagrade za finaliste.
Na ovom kongresu smo dostigli rekordni broj učesnika: online je prijavljeno 560 učesnika, od čega oko 100 učesnika van Srbije. On-site je registrovano još 60 učesnika. U naučnom programu je učestvovalo 80 predavača, 30 iz inostranstva. Kongres je podržalo 35 sponzora, koji su nam nesebično pomogli pri realizaciji ovog događaja, na čemu im se posebno zahvaljujemo. Kongres je podržan od strane ESA, WFSA, EACTA, EAMS-a i Society of anesthesiology of Northern Greece, što ukazuje na internacionalnost ovog sastanka i predstavlja rezultat višegodišnjeg rada našeg udruženja na koji smo veoma ponosni.
Svečano otvaranje kongresa je obeležio veliki broj učesnika, a tokom programa su dodeljene nagrade UAIS-a: Zlatna medalja Sever Kovačev – prof. dr Predragu Romiću za izuzetan doprinos radu udruženja i unapređenju profesije, Srebrna medalja Sever Kovačev – dr Dragani Unić-Stojanović za izuzetan doprinos mlađeg doktora radu udruženja za period 2014–2018. godine i priznanje dr Jeleni Jovičić kao najproduktivnijem autoru časopisa SJAIT za period 2014–2018. godine. Takođe, dodeljene su i nagrade Fonda Svetlana Ceca Erdeljan, dr Andrijani Stanojević i Tijani Nastasić za 2018. i 2019. godinu. Fond je osnovala prof. dr Zoka Milan, a podržan je od strane UAIS-a.
Rekordni broj broj učesnika, sa potpuno prepunjenim salama tokom sesija, značajan broj interaktivnih sadržaja, veliki broj poena koji su učesnici mogli da sakupe za potrebe akreditacije, predavači koji predstavljaju sam vrh evropske anestezije i najbolji predavači iz naše zemlje, samo su neki od zaštitnih znakova ovog kongresa. Ali ono što je izdvojilo XIII Kongres anesteziologa i intenzivista Srbije od ostalih sastanaka jeste raspoloživost vrhunske opreme obezbeđene od strane sponzora, koju su naši učesnici imali prilike da vide i probaju kako kroz radionice tako i tokom čitavog kongresa u izložbenom delu. Identitet

204 SJAIT 2018/7-8
UAIS-a je kroz ovaj događaj potpuno zaokružen u savremeno, evropsko, profesionalno udruženja koje ima mogućnosti, volje i znanja da organizuje sastanke koji zadovoljavaju najviše standarde.
Sav materijal sa kongresa raspoloživ je na sajtu UAIS-a: http://www.uais.rs/Fotografije sa kongresa možete da pogledate na linku:https://drive.google.com/drive/folders/1yS2_9id6iINRepd9mcUPz4j_N88Um4yRI na kraju, verujemo da je ovo bio izuzetan događaj za sve učesnike kongresa, koji je obeležio prethodnu
godinu. Organizatorima je postavljen veoma zahtevan zadatak za budućnost, dok je za učesnike ovo bio skup koji su mogli da završe zadovoljni i motivisani za dalji rad. Zbog toga ću ponoviti završne reči sa svečanog otvaranja, koje su dale osnovni ton čitavom kongresu:
„Just before we leave for the networking cocktail, this was a lecture to remind us that we are living in modern, but difficult times, with turbulent changes, political and economical challenges, where medical professionals, anesthesiologists between them, are not spared. We are facing lot of problems, discontent, burnout and disappointments. Sometimes we do forget that we are a powerful profession that affects and may change people`s lives, lives of our patients, their families and loved ones, but also we are touching the lives of our colleagues that we work with and people we care for and love.
Anesthesiologists have become migrants for their own, searching for better work conditions, incomes and professional achievements. However, wherever you are, and whether you decide to go or stay, lets hope that days like this, dedicated to sharing knowledge and experience, will motivate you to do your best for your patients and our profession.”
Doc. dr Vojislava NeškovićPredsednik Udruženja anesteziologa i intnezivista Srbije

ISSN 2466-488X (Online)
Final four competition for the best written and presented abstract on national meetings
Final4 (F4) competition was established in 2014. The aim of F4 is to promote research among young people interested in research in the field of anesthesiology. Final 4 includes students, young doctors, residents and young specialist who present their work.
The founder and organizer of F4 competition is Dušica Stamenković, MD PhD. The name was proposed by Vojislava Nešković, MD PhD, and F4 is supported by Serbian association of Anesthesiologists and Intensivists (SAAI). So far, we encouraged and supported recipients to publish their work in scientific journals and present them on national meetings. The XIII Serbian Congress of Anesthesiologists and Intensivists held on 22nd–25th November 2018. in Crowne Plaza, Belgrade, Serbia was the first time that SAAI presented valuable prizes for the first four competitors i.e. four competitors with the highest scores based on three blinded independent reviewers.
The process of F4 competition is as follows; first we collect abstracts and authors’ decision for participation in F4. The abstracts are coded, blinded and sent to three independent reviewers (outside of Serbia) for scoring. The scores are summarized and four abstracts with the highest scores are included in F4 session for oral presentation. Presenters are informed and they should be able to present and defend their work in front of three judges and the audience. The final score includes overall impression of their presentation and scores from the blinded review.
We encourage all authors to submit their papers for publication in Serbian Journal of Anesthesia and Intensive Therapy (SJAIT), official journal of SAAI with an open access policy.
The overall number of 46 abstracts was submitted for XIII Serbian Congress of Anesthesiologists and Intensivists and 18 of them were in included in F4 competition. Here we announce the winners for the F4 session of 13th Serbian Congress of Anesthesiologists and Intensivists 22nd–25th November 2018, Crown Plaza, Belgrade, Serbia:
Place 1 Adductor canal block or femoral nerve block for anterior cruciate ligament
reconstruction. Which is better?Malinovska–Nikolovska L1, Shirgoska B2
1Department of Anesthesiology and Intensive Care, City General Hospital „8-mi Septemvri”, Skopje 2University Clinic for Otorhinolaryngology, Medical Faculty, Skopje
doi:10.5937/sjait1806149S

206 SJAIT 2018/7-8
Place 2
How to predict neurogenic pulmonary edema in aneurysmal subarachnoid haemorrhage?
Tijana Nastasović, Branko Milaković, Mila Stošić, Dragana Vićovac, Ivana Lazarević, Dragana Lazarević, Branislava Baljozović, Ivana Šašić, Miloš Kaluđerović, Veljko Terzić, Igor Lazić, Danica
Grujičić, Clinical Center Serbia, Belgrade, Serbia
Place 3
Serratus anterior block for multiple ribs fractures – case reportIlić S. Nataša1, Ilić M. Radomir2
1Clinical center of Vojvodina, Emergency center, Department of anesthesiology and intensive care, Novi Sad, Serbia 2Clinical center of Vojvodina, Emergency center, Department of emergency surgery, Novi Sad, Serbia
This year, 2018 was special for F4 competition as we celebrated its fourth birthday and presented our F4 competition logo!
We would like to thank the reviewers – supporters of F4 competition for their enthusiasm and dedication in the mission to ensure quality and fairness of the competition: Carsten Bantel MD PhD, Prof. Davide Cattano MD PhD and Prof. Mohamed El Tahan MD PhD and Andrey Varvinsky MD and, off course, the great work of Assistant Professor Goran Rondović, enabled the F4 competition to be interesting and encouraging for all abstract presenters.
We invite you to follow UAIS (SAAI) website and apply for F4 competition on our next national meeting!

SJAIT 2018/7-8 207

208 SJAIT 2018/7-8
Assoc. Prof. Dušica Stamenković, MD PhD The founder and organizer of F4

Izveštaj sa Petog Evropskog kongresa posvećenog disajnom putu (5th European Airway Management Congress)
U Kataniji, na Siciliji, od 4. do 7. decembra je održan Peti Evropski kongres posvećen disajnom putu – 5th European Airway Management Congress, pod motom From past to the future of Airway Management.
EAMS (European Airway Management Society), kao panevropsko medicinsko društvo, osnovano je 2003. godine u Glazgovu. Danas je preraslo u svetsko udruženje, koje čine anesteziolozi, intenzivisti i lekari urgentne medicine iz 31 zemlje. Društvo je osnovano sa ciljem povezivanja i razmene iskustava među članovima, na polju uspostavljanja i održavanja disajnog puta, kao i njegovom naučnom napretku, kroz podsticanje novih tehnologija istraživanja, obrazovanja i nastave. U okviri ESA (European Society of Anaesthesiology) udruženje deluje posebno u predkongresnim tematskim radionicama i predavanji-ma vezanim za disajni put, i predstavlja podkomitet ESA (Learning track 11 – Respiration and Airway Management).
Na prelepom istorijskom lokalitetu, sa divnim pogledom na Jonsko more i vrhove Etne, održan je najveći Evropski naučni skup o disajnom putu, koji je okupio lidere u ovoj oblasti, a kojom se pored an-esteziologa bave i intenzivisti, pulmolozi, lekari urgentne medicine. Kongres je podržan od strane ESA (European Society of Anaesthesiology) i integrisanog WAM (Word Airway Management), u čijem sastavu su, pored EAMS, SAM (Society of Airway Managemnt – USA) i DAS (Difficult Airway Management of Great Britain).
Ovo je ujedno bila i prilika da se na jednom mestu okupe članovi nacionalnih udruženja iz Evrope, članovi i gosti iz zemalja Južne Amerike, Australije, Azije i Novog Zelanda, a u cilju razmene iskustava i naučnih informacija.
Program kongresa je bio sveobuhvatan, uključio je plenarna predavanja, panel diskusije, susrete eksperata u oblasti disajnog puta, simu-lacije, praktične radionice sa bazičnom opre-mom, kao i one sa najnovijom opremom za us-postavljanje disajnog puta, i poster prezentacije.
Prisustvo kompanija (industrija) nosi po-seban značaj na skupovima vezanim za disajni put. Ovoga puta je njihov doprinos bio od veli-ke važnosti, jer je predstavljena najnovija video intubaciona oprema vezana za uspostavljanje i održavanje disajnog puta.
Na svečanoj završnoj ceremoniji kongresa, održana je i dodela značajnih priznanja i nagra-da. Ja sam imala veliku čast da od strane direkto-ra Borda EAMS budem predložena za počasnog člana udruženja, što sam sa velikim ponosom i zadovoljstvom prihvatila. Na svečani način, uz jedan posvećen i za mene dirljiv govor, pred-sednika EAMS prof R. Greifa je govorio o mom doprinosu na polju disajnog puta, posebno u ju-goistočnom delu Evrope, dobila sam zlatnu pla-ketu i proglašena sam za počasnog člana. U rad EAMS-a sam uključena od 2004. godine, prvo
ISSN 2466-488X (Online) doi:10.5937/sjait1806149S

210 SJAIT 2018/7-8
kao predstavnik Srbije u savetu (Council), a zatim kao član borda u funkciji sekreta-ra. U okviru Euroanestezije, kao član EAMS odgovornog za organizaciju tematskih radi-onica i predavanja, devet godina sa bila in-struktor za hiruršku krikotiroidotomiju.
Kongres je u potpunosti ispunio sva pro-fesionalna očekivanja, pozitivne povratne informacije i entuzijazam više od 600 uče-snika iz celog sveta, kompanija i gostiju su dokaz da su ciljevi vezani za mnoge aspekte uspostavljanja i održavanja disajnog puta bili ispunjeni.
dr sc. med. Dušanka Janjević, Počasni član Evropskog udruženja za
disajni put (EAMS) Honorary Member of EAMS (European
Airway Management Society)

Otežan disajni put – radionica
U okviru 13th Serbian Congress of Anesthesiologists and Intensivists održana je radionica posvećena otežanom uspostavljanju disajnog puta, a koja je podržana od strane European Airway Management Society (EAMS), sa renomiranim instruktorima, kao što su Massimiliano Sorbello (ITL), Ilijaz Hodžović (UK), Davide Cattano (USA), Mohamed R. El Tahan (SA) i Dušanka Janjević (Srb).
Ukupno 33 polaznika radionice je imalo mogućnost da, pored praktičnog segmenta, razmenjuju mišljenja i da diskutuju o brojnim situacijama otežanog uspostavljanja disajnog puta, koje su obuhvatile izvođenje okseganacije, videolaringiskopije i fiberoptičkim bronhoskopom izvedene intubacije kod sediranog pacijenta.
Laringealna maska se svakodnevno korsiti u praksi, njena kombinacija sa fiberoptičkim bronhoskopm i različiti inovativni vidovi njene primene prikazani su na jednoj od stanica (instruktori: Branka Terzić, Dušica Stamenković, Srbija). Videolaringoskopija je savremeni vid obezbeđivanja disajnog puta, čije su nam različite vidove primene prikazali Ilijaz Hodžović (UK) i Vesna Antonijević Jovanović i Goran Rondović (Srb). Perkutana traheostomija se izvodi u jedinici intenzivne nege, a zahvaljujući našim instruktorima mogli smo da naučimo osnovne korake u njenom izvođenju (Miodrag Golubović, Ana Popadić i Duško Maksimović, Srbija). Specijalno za ovu priliku, Ana Popadić i Duško Maksimović (Srb) napravili su video prezentaciju fiberoptičkog praćenja izvođenja perkutane traheostomije.
Krikotireotomija se najćešće izvodi na životno ugroženom pacijentu, a način na koji se ona izvodi su predstavili Dušanka Janjević i Vladimir Dolinaj (Srb). Kao i na većini radionica, fiberoptički bronhoskop privlači posebnu pažnju, a zahvaljujući iskusnim instruktorima, pored prvih koraka u izvođenju fiberoptičke bronhoskopije, bili smo u mogućnosti da naučimo i određene manevre. Po prvi put u našoj zemlji, polaznici radionice su upoznati sa izvođenjem retrogradne intubacije i principima ektubacije pacijenta koji je bio težak za intubaciju.
Radionica disajni put je održana zahvaljujući velikoj pomoći i zalaganja brojnih firmi, koje su omogućile 12 lutaka, specijalno konstruisanih za obezbeđivanje disajnog puta, kao i celokupnu opremu koja je korišćena za radionicu. Zahvaljujemo se na pomoći firmama Aixmed, Cook (Telemed), MIT – Medicinski instrumenti i tehnologija d.o.o., Olympus, Storz (Ranex) i Winmedic (firme su raspoređene po abecednom redu).
Delić atmosfere sa radionice Vam prenosimo kroz slike. Na našu žalost, nismo bili u mogućnosti da primimo veliki broj zainteresovanih, zbog uslova koji su neophodni za adekvatno izvođenje obuke.
Predavanja sa plenarne sesije i radionice posvećene uspostavljanju otežanog disajnog puta se nalaze u zborniku radova, koji će od januara 2019. godine biti dostupan na www.uais.rs.
Doc. dr Dušica Stamenković
ISSN 2466-488X (Online) doi:10.5937/sjait1806149S

212 SJAIT 2018/7-8

SJAIT 2018/7-8 213

214 SJAIT 2018/7-8

SJAIT 2018/7-8 215