Sepsis: Current Dogma and New Perspectives
Click here to load reader
Transcript of Sepsis: Current Dogma and New Perspectives

Immunity
Review
Sepsis: Current Dogma and New Perspectives
Clifford S. Deutschman1,* and Kevin J. Tracey2,*1Department of Anesthesiology and Critical Care and Surgery and Sepsis Research Program, Perelman School of Medicine,University of Pennsylvania, Philadelphia, PA 19104, USA2Feinstein Institute for Medical Research, 350 Community Drive, Manhasset, NY 11030, USA*Correspondence: [email protected] (C.S.D.), [email protected] (K.J.T.)http://dx.doi.org/10.1016/j.immuni.2014.04.001
Sepsis, a clinical syndrome occurring in patients following infection or injury, is a leading cause of morbidityandmortality worldwide. Current immunological mechanisms do not explain the basis of cellular dysfunctionand organ failure, the ultimate cause of death. Here we review current dogma and argue that it is time to delin-eate novel immunometabolic and neurophysiological mechanisms underlying the altered cellular bioener-getics and failure of epithelial and endothelial barriers that produce organ dysfunction and death. Thesemechanisms might hold the key to future therapeutic strategies.
IntroductionSepsis, the quintessential medical disorder of the 21st century, is
the most frequent cause of death in hospitalized patients. It is a
direct consequence of the current medical and surgical capa-
bility to effectively care for critically ill patients who, until relatively
recently, would have died. It accounts for 1,000,000 cases and
200,000 deaths annually in the United States alone, but unlike
other major epidemic illnesses, treatment for sepsis is nonspe-
cific, limited primarily to support of organ function and adminis-
tration of intravenous fluids, antibiotics, and oxygen (Angus and
van der Poll, 2013). There are no approved drugs that specifically
target sepsis. It drains billions of dollars from the healthcare
system annually, expenses most often incurred during weeks-
or months-long stays in intensive care units. The necessity for
effective therapeutic approaches to this catastrophic illness
cannot be overstated.
Sepsis is a syndrome, not a disease (Vincent et al., 2013). It
often occurs in patients with infection, but not exclusively: as
many as 40% of cases occur during sterile tissue injury arising
from noninfectious sources such as pancreatitis, ischemia reper-
fusion injury, cancer, and a host of other disorders. Although
sepsis occurs sporadically in previously healthy patients, poten-
tially with tragic results (Dwyer, 2012), it most often occurs in pa-
tients with underlying disabilities or illnesses. There is no typical
patient with sepsis; it strikes across age groups, without regard
to race, geography, or health status. The combined number of
variables that influence whether a patient survives or succumbs
is poorly understood.
Here we argue that sepsis is not a stereotypical, steadily pro-
gressive immunological process that follows infection or injury;
that innate and adaptive immune responses do not inevitably
damage host cells; and that the long-held notion that sepsis
is a distinct immunological disorder is incorrect. Rather, under-
standing sepsis requires reframing the research focus to iden-
tify immunometabolic and neurophysiological mechanisms of
cellular and organ dysfunction. This approach might hold the
key to future therapeutic strategies.
Epidemiological and Historical Perspective‘‘Sepsis’’ is an imprecise clinical diagnostic term used to
describe patients that have a continuum of abnormalities in
organ function (Vincent et al., 2013). The modern terminology
applied to this syndrome originated from a 1991 Consensus
Conference that defined ‘‘sepsis’’ as documented or suspected
infection combined with two or more abnormalities in body tem-
perature, heart rate, respiratory rate, or white blood cell count
(Bone et al., 1992). Moreover, patients with sepsis and evidence
of organ dysfunction, including cardiovascular, renal, hepatic,
or neurological were classified as having ‘‘severe sepsis,’’ and
those with cardiovascular dysfunction not responsive to fluid
were said to have ‘‘septic shock.’’ In a revision published a
decade later, septic shock was also defined to include evidence
of inadequate tissue perfusion. It has recently been recognized
that patients with sepsis or septic shock can develop ‘‘persistent
critical illness’’ (PCI) with overt organ dysfunction that lasts for
weeks or months. The emergence of PCI is a historically recent
event; previously, these patients would have died, but today
they survive because of exogenously supported organ function.
Themortality from PCI is 20%–40%, and survivors are frequently
disabled by cognitive dysfunction, neuropathies and myopa-
thies, immunological dysfunction, and other complications.
Although the acute mortality from sepsis, severe sepsis, and
septic shock has been reduced to a historically low frequency
(15%–20%) (Kaukonen et al., 2014), annually some 500,000
new cases enter the survivor pool; these survivors are at risk
for early death, with 5 year mortality rates as high as 75% (Iwa-
shyna et al., 2010). Thus, in the United States currently there
are more than 2.5 million individual survivors at extremely high
risk of morbidity and mortality because of their prior experience
of severe sepsis or PCI.
Until the latter part of the 20th century, the principal research
focus and mechanistic understanding of sepsis pathogenesis
was directed toward controlling the spread of pathogens. This
perspective shifted to the immune system in the early 1980s,
when macrophage activation and release of tumor necrosis
factor (TNF) and other mediators was implicated in the patho-
genesis of acute septic shock. A series of highly cited studies
then established that TNF was both necessary and sufficient to
mediate acute septic shock (Tracey et al., 1986, 1987). Mono-
clonal antibodies to TNF administered to baboons infected
with live E. coli prevented the development of acutely lethal
septic shock despite the presence of replicating bacteria in
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 463

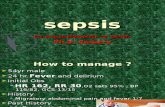
Figure 1. Intracellular and Extracellular ‘‘Danger Signals’’ ActivateInflammasomes and SignalosomesIntracellular or extracellular ‘‘danger signals,’’ which stimulate cellular re-sponses that disrupt homeostatic immunometabolic mechanisms, are medi-ated by pattern-recognition receptors (PPRs). PPRs recognize two types ofpatterns—those that reflect cellular damage (DAMPs) and those that are foundon pathogens (PAMPs). Pathogens or DAMPs (i.e., K+ overload secondary toionizing radiation of excessive reactive oxygen species, excessive quantitiesof intracellular debris, such as damaged protein, organelle content such asRNA, mitochondrial DNA, or cytochrome c) that are intracellular bind toPPRs of the platform protein family, primarily nucleotide-binding domainand leucine-rich-repeat-containing proteins (NLRs) and RIG-like receptors(RLRs). NLRs oligimerize and, via a connector protein, bind to pro-caspase-1to form structures called inflammasomes. In addition, HMGB1 binds nucleicacids and is a universal sentinel for the presence of intracellular viral products.Viral RNAs containing non-Watson-Crick short sections of dsRNA bind toand regulate PKR, which participates in inflammasome activation. Activatedinflammasomes cleave pro-caspase-1 to caspase-1, which in turn cleavespro-IL-1b and pro-IL-18 to their biologically active forms. ExtracellularDAMPs (extruded intracellular structures or autophagosomes) or PAMPscan find their way back into the cell, further stimulating inflammasome activity.In somatic (nonimmune) cells, activation of inflammasome signaling is alsoinduced in response to immunometabolic substrates, energy deficiency, or ERstress.
Immunity
Review
the bloodstream, establishing that TNF, not bacteria, mediated
acute shock and lethal tissue injury (Tracey et al., 1987; Tracey
et al., 1986). Although the shock syndrome represents only a
relatively small subset of the larger population of sepsis patients,
these results engendered widespread hope that targeting
mediators produced by the effector arm of the innate immune
system would lead to therapies for all patients with sepsis.
Unfortunately, clinical trials of anti-TNF in patients with acute
shock were never performed. Instead, for reasons reflecting
the inherent difficulty with early diagnosis and influenced by
business expediency rather than scientific rigor, ill-conceived at-
tempts were made to deploy TNF inhibitors without regard for
the presence of shock or even of TNF itself (Marshall, 2008).
Costly clinical trials using antibodies and other agents to inhibit
TNF in diversely heterogeneous patients with severe sepsis or
PCI not surprisingly failed to improve overall mortality.
Nonetheless, these early efforts produced a new class of clin-
ically useful biological agents (including anti-TNF, anti-inter-
464 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
leukin-1 [anti-IL-1], and anti-IL-6) now administered to millions
of patients with rheumatoid arthritis, inflammatory bowel dis-
ease, and other disorders. The search for the molecular mecha-
nism of septic shock culminated in products whose worldwide
sales currently exceed $50 billion per year.Moreover, as ongoing
investigations reveal other indications for treating patients with
diseases attributable to inflammatory and autoimmune mecha-
nisms, the use of these agents is likely to grow (Chan and Carter,
2010). Despite these gains derived from studying septic shock in
animals, the original objective of developing mechanism-based
therapy for sepsis has not been achieved. Is there hope that it
can be solved?
Failure of HomeostasisHere we review the evidence that unlike septic shock (mediated
by TNF), severe sepsis, and PCI are not immunopathologies
mediated directly by the immune system. Rather, they are syn-
dromes more properly defined as ‘‘a failure of homeostasis,’’
i.e., ‘‘an inability for the organism or cell to maintain internal equi-
librium by adjusting its physiological processes under fluctu-
ating environmental conditions in response to infection or injury.’’
Invertebrates and higher, multicellular organisms are subject to
internal and external environmental stressors. Health is charac-
terized by a state during which individual cells minimize fluctua-
tion around ‘‘ideal’’ intracellular electrochemical and metabolic
steady states. Homeostasis reflects the individual cell’s funda-
mental imperative to respond to stress and survive. The specific
processes needed tomaintain homeostasis include a barrier that
separates the milieu interior from the world at large, by the ability
to sense extracellular changes that threaten equilibrium, by
effector mechanisms that respond to sensory input to regulate
metabolic and cellular function, by mechanisms to eliminate
invaders or endogenous cellular constituents that can no longer
contribute to internal stability, by processes to recycle cellular
substrate, and by mechanisms for cell self-destruction when
survival is no longer possible.
Immunity, the state of having sufficient biological defenses to
avoid infection, disease, or other unwanted biological invasion, is
highly dependent upon a homeostatic or balanced response to
infection and injury. Considered in this light, the immune system
can mediate immunopathology directly, as in the case of exces-
sive TNFmediating acute septic shock (which is not ‘‘sepsis’’), or
autoantibodies mediating renal failure during autoimmunity.
These are examples of a failure of ‘‘immunity’’ to restore homeo-
stasis that results in excessive, deleterious consequences. At
the other extreme of failed homeostasis, excessive immunosup-
pression might render the host exquisitely susceptible to infec-
tion or cancer. Immunity preserves homeostasis by establishing
a healthy balance in between immunopathology and immuno-
suppression.
In many instances, perturbed homeostasis evokes autophagy,
a process that removes or recycles damaged proteins or organ-
elles. When autophagy proves to be insufficient, activation of
innate immunity initiates inflammation via recently uncovered
mechanisms (Figure 1). Danger-associated molecule patterns
(DAMPs, or alarmins) derived from host products within cells
are sensed by the genome encoded retinoic acid inducible
gene 1–like receptors (RLRs) and nucleotide-binding oligomeri-
zation domain-like receptors (NLRs), a process that leads to

Immunity
Review
the assembly of inflammasomes, cytosolic complexes that, by
activating caspase-1, produce active IL-1 and IL-18 for secretion
into the extracellular space. A key step in inflammasome assem-
bly is the phosphorylation of double-stranded RNA-dependent
protein kinase (PKR, also known as EIF2AK2), a process trig-
gered by DAMPs and pathogen-associated molecular patterns
(PAMPs) (Lu et al., 2012). The endogenous products of cell injury
and IL-1 and IL-18 become extracellular DAMPs and, in concert
with PAMPs derived from foreign products, stimulate Toll-like
receptors (TLRs), C-type lectin receptors (CLRs), and receptor
of advanced glycation end products (RAGE) to catalyze the
formation of cell surface signalosomes. Prototypical DAMPs
implicated in sepsis pathogenesis include high-mobility group
protein B1 (HMGB1), S100 proteins, and extracellular RNA,
DNA, and histones. Activation of signalosomes and inflamma-
somes mediate the onset of apoptosis, endoplasmic reticulum
(ER) stress and other metabolic responses, cell proliferation,
and expression of genes encoding TNF and other cytokines
(Figure 1). Inflammasomes mediate the release of HMGB1, IL-
1b, and IL-18, which are secreted into the extracellular space
and function to amplify the innate immune response (Lu et al.,
2012; Lamkanfi et al., 2010; Schroder et al., 2010). Inflamma-
somes also mediate pyroptosis, a form of programmed cell
death that scatters additional cell components and contents
into the extracellular space (Wree et al., 2014). This debris in-
cludes mitochondrial DNA, cytochrome C, and heat-shock pro-
teins functioning as DAMPs. The release of DAMPs and alarmins
during sterile injury, ischemia, or trauma incites pathogenic
mechanisms of multiple organ dysfunction that do not distin-
guish between infectious and noninfectious illness (Andersson
and Tracey, 2011). Ultimately, components of the innate immune
response activate adaptive immunity.
Inflammation resolution is essential to maintain immunological
homeostasis and health. Mechanisms that promote resolution
include release of anti-inflammatory mediators that suppress
inflammation, the deployment of decoy receptors that interfere
with inflammatory mediator activity, the secretion of resolvins
that accelerate the efflux of inflammatory cells and debris, and
feedback from the nervous system that suppresses the release
of inflammatory mediators and stimulates the release of resol-
vins (Nathan and Ding, 2010; Schwab et al., 2007; Medzhitov,
2010; Andersson and Tracey, 2012a). The coordination of inflam-
mation and its resolution involves the major homeostatic regula-
tory systems that sense environmental changes and regulate
organ function: the nervous and immune systems (Andersson
and Tracey, 2012b). Impairment or dysfunction of these systems
converts a balanced immune response into a state of failed
homeostasis and immunopathology. In this context, the impact
of inflammation on the host cannot be fully understood as an
isolated function of bone-marrow-derived cells; rather, it reflects
the combined activity of the nervous and immune systems that
prevents immunopathology by maintaining homeostasis. Feed-
back interaction between the immune and nervous systems
orchestrate the complex responses that allow higher organisms
to function as an integrated unit. Restoration of homeostasis
during inflammation occurs when the interaction between
these systems produces a balanced, highly adaptive response
that can eliminate threats, repair damage, restore organ function
and metabolism to normal setpoints, and create memories
of the events to optimize subsequent neural and immune
responsiveness.
Neurological and Immunological Feedback SystemsSepsis should not be exclusively considered as the immuno-
logical response to injury or infection because the origins of
impaired homeostasis also involve critical regulatory neuroendo-
crine mechanisms. The regulatory feedback loops that link the
immune, neuroendocrine, and nervous systems comprise two
components: an afferent (sensory) and an efferent (regulatory)
arm. Afferent neural systems affect neuroendocrine output,
which is also modulated by cytokine and hormone transfer
across the attenuated blood-brain barrier of the pituitary portal
system. The efferent arm of the nervous system is best exempli-
fied by the ‘‘inflammatory reflex’’, whereas neuroendocrine feed-
back systems are well-known (Figure 2). The efferent arm of the
immune system comprises the two divisions, the innate and the
adaptive. Impairment of homeostasis in afferent and efferent
signaling in both the immune and nervous systems are the hall-
mark of shock, severe sepsis, and PCI, each of which will be
considered separately.
When the host is challenged by exposure to LPS, the acutely
enhanced release of TNF and other mediators by macrophages,
monocytes, and dendritic cells produces diminished tissue
perfusion (shock), tissue injury, and acute organ failure, even in
the absence of infection. The afferent, sensory pathway in the
innate immune system modulates the magnitude of the TNF
response to LPS. Within species, genetic variation of receptor
mechanisms and signal transduction molecules influences
the sensitivity to LPS and the magnitude of the TNF response.
Genetic deficiency of TLR4, MD2, or HMGB1, and other mole-
cules implicated in the sensing and signal transduction mecha-
nisms of LPS responsiveness each confer protection against
LPS-mediated TNF release, and therefore, protect against shock
(O’Neill et al., 2013; Kawai and Akira, 2011; Yanai et al., 2009).
The nervous system also directly influences the capacity of the
immune system to produce TNF and the host sensitivity to LPS
as well (Andersson and Tracey, 2012a).
LPS, other bacterial toxins, TNF, IL-1, andother hostmediators
all interact directly with sensory neurons to mediate the genera-
tion of afferent action potentials that rise in the sensory vagus
nerve to terminate in the nucleus tractus solataris in thebrainstem
(Figure 2). These afferent signals are required to induce fever,
sickness behavior, and other neurological inflammatory re-
sponses. Seminal experiments by Linda Watkins demonstrated
that the fever response in rodents mediated by administration
of intra-abdominal IL-1 requires functional sensory vagus nerve
signals (Watkins et al., 1995). Signal transduction mechanisms
in this IL-1-mediated vagus nerve activation have been attributed
to IL-1 receptors expressed in sensory neurons and in glomus
cells that reside along the vagus nerve pathway to the brain
(Goehler et al., 1997). Direct IL-1 receptor ligand interaction in
neurons modulates neuronal firing, and glomus cell release of
dopamine and other neurotransmitters also modulates vagus
nerve sensory signals (Binshtok et al., 2008; Chiu et al., 2012).
Recordings of IL-1-mediated sensory neural spikes has traced
their progression from the sensory vagus nerve to the brainstem,
which regulates efferent responses via the hypothalamic-pitui-
tary-adrenal axis and via descending neural signals in the vagus
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 465

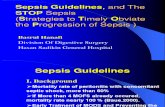
Figure 2. Neuroendocrine Afferent and Efferent Pathways Restore HomeostasisInflammatory signals arising in organs are conducted along the afferent vagus nerve to the nucleus tractus solitaries of the brainstem. Sensory impulses fromsomatic tissue generate electrical impulses that are modulated in the dorsal root ganglia (DRG) and relayed via the spinal cord to nuclei in the brainstem andhypothalamus. Descending neuronal impulses are conducted in both the efferent vagus nerve and the sympathetic chain. Vagal signals terminate in the celiacganglion and interact with adrenergic nerve-cell bodies that project distally via the splenic nerve. The termini of these nerves in the spleen release norepinephrine(NE) that in turn stimulates T cells expressing choline acetyltransferase (ChAT), enhancing acetylcholine (Ach) biosynthesis. Ach interacts with a7nACh receptors(a7nAChRs) onmacrophages, suppressing NF-kB activation and limiting inflammatory cytokine expression and release. Activation of the sympathetic chain leadsto release of NE in target tissues. NE stimulation of alpha adrenergic receptors enhances, whereas beta-adrenergic receptor stimulation suppresses cytokinerelease. Vagal impulses also modulate dopamine release by the adrenal medulla. Stimulation of D1 receptors on monocytes and macrophages limitcytokine expression and/or release. Inflammatory afferents affecting the endocrine system arise from (1) signals carried via the afferent neuronal pathways, (2)cytokine transfer across the attenuated blood-brain barrier of the hypothalamic-pituitary junction, and (3) direct cytokine production by cells of the CNS. CNSfactors that modulate cytokine production and release in the brain include malanocyte-stimulating hormone (MSH), thyroid stimulating hormone (TSH), gluco-corticoids, leptin, ghrelin, and adrenocorticotropin (ACTH). Hypothalamic responses to cytokines alter the release of ACTH, TSH, prolactin (PRO), growthhormone (GH), and follicle stimulating hormone. Monocyte and macrophage activity, including cytokine production, and is altered by thyroid hormones (T3, T4),while both T and B cells function are decreased by estradiols (EST) and increased by androgens (AND). GH, prolactin, and insulin stimulate T cell activity.
Immunity
Review
and other nerves (Niijima, 1996; Niijima et al., 1991). Recently,
Woolf and colleagues discovered the neural mechanisms in
peripheral tissues that underlie calcium influx and neural spiking
mediated by the direct interaction of bacterial N-formylated pep-
tides and the pore-forming toxin a-haemolysin (Chiu et al., 2013).
The sensory neural net enshrouds nearly every somatic cell in
the body, as well as the blood vessels and the epithelial lining
of the body’s external surfaces. By sensing infection and injury
independent of the innate immune system sensing pathways,
466 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
the sensory neural network shares the front line with the innate
immune system (Chiu et al., 2012, 2013).
The inflammatory reflex is a prototypical, major efferent neu-
ral pathway that modulates TNF release in response to LPS
(Figure 2) (Tracey, 2002, 2009; Borovikova et al., 2000). Efferent
signals arising in the brainstem descend in the vagus nerve to
terminate in the celiac ganglion, wherein resides the adrenergic
nerve cell bodies of the splenic nerve (Rosas-Ballina et al.,
2008). At the splenic nerve terminus in spleen, norepinephrine

Immunity
Review
released by axons interacts with a subset of T cells that express
choline acetyl transferase, the rate-limiting enzyme for the
biosynthesis of acetylcholine (Rosas-Ballina et al., 2011). Acetyl-
choline produced by these T cells interacts with the a7nicotinic
acetylcholine receptor (a7nAChR) expressed on red pulp and
marginal zone macrophages. Signal transduction via a7 sup-
presses nuclear translocation of NF-kB, stabilizes mitochondrial
membranes, and inhibits activation of inflammasomes, which
inhibits release of TNF, IL-1b, HMGB1, and other cytokines (Lu
et al., 2012;Wang et al., 2003, 2004). Cutting the vagus or splenic
nerves, genetically ablating a7nAChR, or pharmacologically in-
hibiting signals along this pathway all enhance cytokine release
and the increase the severity of of lethal shock and tissue injury
(Bernik et al., 2002; Borovikova et al., 2000; Rosas-Ballina et al.,
2008; Wang et al., 2003).
Neural signals can also descend from the brainstem via the
sympathetic chain, culminating in the release of adrenergic neu-
rotransmitters in tissues that interact with innate immune cells
expressing alpha-adrenergic and beta-adrenergic receptors to
modulate cytokine release (Bosmann and Ward, 2013). Another
efferent neural circuit modulating the cytokine response to LPS
comprises vagus nerve signals to the adrenal gland that releases
dopamine. Ligand interaction with D1 receptors expressed
on monocytes and macrophages attenuates TNF and other
cytokine responses to LPS (Torres-Rosas et al., 2014). The
magnitude of the TNF response to LPS is also highly regulated
by the efferent neuroendocrine arm of the nervous system.
Impaired neuroendocrine function by experimental adrenalec-
tomy or hypophysectomy, or by administration of pharmacolog-
ical hormone antagonists, renders the host exquisitely sensitive
to injury and death by logarithmically enhancing the magnitude
of the TNF response (Thayer and Sternberg, 2010). Together,
these findings indicate that the risk of developing severe shock
and tissue injury following acute exposure to LPS is highly
dependent upon the pre-existing functional state of neurological
afferent and efferent pathways that regulate the innate immune
system by reflexively controlled neural circuits.
Extrapolating mechanisms of afferent and efferent immune
and neural feedback circuits to patients either at risk for, or expe-
riencing, septic shock is exceedingly complex. Risk assessment
can theoretically identify subjects with allelic variants that pre-
dispose to enhanced immune sensory or effector functions.
For example, individual variations in the TLR4 and TNF genes
influence the magnitude of monocyte and macrophage TNF
release during endotoxin exposure. There is wide variability be-
tween patients in vagus nerve signaling pathways, as observed
by recording heart-rate variability as a measure of autonomic
neural function. Diminished vagus nerve signals predispose to
excessive or nonresolving inflammation, as evidenced by clinical
findings of enhanced mortality from shock in patients presenting
the hospital with depressed vagus nerve activity and signs of
infection (Barnaby et al., 2002) (Ahmad et al., 2009). Adminis-
tration of endotoxin to human volunteers increases heart-rate
variability, indicating that endotoxin modulates vagus nerve
efferent activity which in turn regulates TNF release (Lehrer
et al., 2010). Assessing these and other functional states of
feedback systems operating as an integrated physiological
network is difficult, at best, and beyond the capabilities of the
current clinical enterprise.
From the immunology research perspective, dissecting the
mechanisms of intersecting homeostatic neural and immune
systems is crucial, but this cannot be fully accomplished
in vitro, because isolated cellular approaches do not replicate
the controller networks. Consider the simple example of study-
ing mechanisms of TNF release in isolated monocytes and
macrophages, which produce TNF and other LPS-stimulated
mediators at rates 100 to 100,000 times higher in tissue culture
systems than in vivo. Once isolated from the efferent controlling
loops, individual cells are not subjected to counter-regulatory
control by the redundant neural-, neuroendocrine-, and im-
mune-derived inhibitory signals that are normally operative
in vivo. A balanced, self-resolving, noninjurious TNF response
to acute endotoxin exposure can only occur when communica-
tion between the major afferent and efferent arms of the nervous
and immune system is maintained. Thus, the immunopathology
mechanisms of acute shock are not restricted to the immune
system because the dysfunctional homeostasis process under-
lying excessive TNF release also involves the afferent and
efferent neural signaling systems.
Although understanding these regulatory feedback loops in
shock is complex, the situation is even more complicated in
severe sepsis and PCI. Widespread failure of homeostasis, the
sine quo non of severe sepsis and PCI, occurs in most, if not
all, components of the afferent and efferent arms of the immune
and nervous systems. Recent advances in immunology and
neuroscience have elucidated several impaired signaling
mechanisms during severe sepsis that will be discussed in order
to inform a model.
A consistent finding in animals and patients with severe
sepsis is that monocytes-macrophages are tolerant, i.e.,
exhibit diminished capacity to respond to LPS and other
PAMPs and DAMPs. This observation has been reproducibly
reported in studies of whole-blood organ culture, in which
LPS, HMGB1, or other stimulating agents are added directly
into fresh whole blood obtained from patients (Cavaillon and
Adib-Conquy, 2006; Monneret et al., 2008). When compared
to healthy subjects, the release of TNF, IL-1, and other media-
tors by monocytes in blood from patients with severe sepsis is
suppressed by 80%–90%. This sensitivity defect is not
restricted to LPS, because challenging monocytes from severe
sepsis patients with other immune stimulators all produce a
similar magnitude of attenuated cytokine release (Cavaillon
and Adib-Conquy, 2006; Monneret et al., 2008). The mecha-
nism of this tolerant state is unknown but might include down-
modulation of TLR4 expression, impairment of NF-kB signaling,
and differentiation to the alternatively activated phenotype
or M2 status (Monneret et al., 2008; Iskander et al., 2013).
Analysis of postmortem tissues indicates that cytokine re-
sponses are depressed in cells harvested from spleen and
lung (Boomer et al., 2011). Small clinical trials indicate that it
might be possible to enhance monocyte cytokine production
and human leukocyte antigen-DR (HLADR) expression and
increase numbers of IL-17-expressing CD4+ T cells by admin-
istration of granulocyte macrophage-colony stimulating factor
(GM-CSF) or interferon gamma, but whether this improves
organ function, physiological homeostasis, or survival is an un-
proven hypothesis (Meisel et al., 2009; Nierhaus et al., 2003;
Monneret et al., 2008).
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 467

Immunity
Review
Impaired responsiveness to products of injury and infection is
not restricted to the monocyte lineage because abundant evi-
dence indicates that T and B cells are also resistant to activation
and proliferation (Monneret et al., 2008). HLA-DR expression is
decreased; enhanced apoptosis of B cells, CD4+ T cells, and
follicular dendritic cells also occurs (Sarkar et al., 2006). This
corresponds with decreased numbers of circulating CD4+ T
lymphocytes in peripheral blood of severe sepsis patients
and decreased immunohistochemically detectable numbers of
B and T cells in postmortem spleen obtained from severe
sepsis victims (Inoue et al., 2013; Boomer et al., 2011; Felmet
et al., 2005). The numbers of CD4+CD25+ regulatory T cells is
increased, the expression of cytotoxic T lymphocyte associated
antigen (CTLA)-4-D152, which has been implicated as inhibitory
costimulatory ligand, is enhanced, and CD86 is suppressed in
T lymphocytes from severe sepsis patients (Stearns-Kurosawa
et al., 2011). T cell proliferation in response to antigen, and
delayed type hypersensitivity to measles and mumps are
depressed during severe sepsis and PCI. In addition to the in-
creases in T regulatory cell counts, the numbers of myeloid-
derived suppressor cells are also increased in sepsis (Iskander
et al., 2013). Analysis of postmortem tissues reveals that expres-
sion of the inhibitory receptors programmed cell death 1 (PD-1)
are increased in spleen and lung tissue and T regulatory and
myeloid derived suppressor cell counts enhanced (Boomer
et al., 2011). These findings indicate that immune homeostasis
is impaired, a state that has been widely described as ‘‘immuno-
suppression’’ and ‘‘T cell exhaustion.’’
It remains highly speculative whether there is a causal role for
immunosuppression in the development of impaired organ func-
tion and lethality in severe sepsis and PCI. There is correlative
evidence that increased lymphocyte apoptosis in the spleen
and other lymphoid organs victims is associated with decreased
lymphocyte number in peripheral blood, and that the presence of
apoptotic lymphocytes might contribute to anergy in monocytes
and dendritic cells (Monneret et al., 2008). It is entirely logical that
the observed homeostatic derangements in lymphocyte viability
and function render patients immunosuppressed, but uncon-
trolled infection does not occur in 20%–50% of lethal cases.
Blood cultures are sterile in 75% of lethal cases, and abundant
evidence indicates that antibiotics and surgery, although suffi-
cient to reverse the source of active infection, are insufficient
to prevent organ dysfunction and death. The nomenclature of
‘‘immunosuppression’’ in sepsis has also been used to describe
the increased incidence of organisms such as Pseudomonas
and Candida that are only rarely found in immunocompetent
patients. Reactivation of viruses, including cytomegalovirus
and herpes simplex virus (HSV), has been demonstrated in up
to a third of patients with severe sepsis, but missing from this
‘‘immunosuppression hypothesis’’ of sepsis is amechanism link-
ing impaired immunity to organ dysfunction and mortality. Post-
mortem analysis of organ specimens from severe sepsis and
PCI reveals a remarkable absence of inflammation, necrosis,
apoptosis, cell injury, cytoskeletal rearrangements, ischemia,
or microvascular coagulopathy (Stearns-Kurosawa et al.,
2011). The histopathology in the majority of lethal cases is strik-
ing for its blandness and absence of pathogens. Apoptosis of
CD4+ and CD8+ T and B lymphocytes occurs in the spleen,
thymus, lymph nodes, and gastrointestinal-associated lymphoid
468 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
tissue, but evidence of inflammation, immunopathology, or cyto-
lytic damage is lacking.
Thus, it has been clearly established that patients with severe
sepsis have impaired afferent and effector signaling in the im-
mune system. However, unanswered questions remain because
a causative link or mechanism between sensory and effector
immunosuppression and the development of organ damage
and lethality has not been established. It is plausible, if not likely,
that the presence of nonpathogenic organisms attributed to
‘‘immunosuppression’’ is a biomarker of impaired organ function
and homeostatic dysfunction, not the mechanistic cause of
organ dysfunction, and not the cause of death. Having reviewed
the importance of impaired homeostasis in the immunopa-
thology of acute septic shock, and the evidence that afferent
and efferent signaling in the immune system is impaired in severe
sepsis, it is now important to consider mechanisms of impaired
neurological homeostatic in severe sepsis and PCI.
Abundant evidence implicates impaired signaling in afferent
and efferent neural pathways that normally maintain homeosta-
sis in the immune system and other organs. During severe
sepsis, dorsal root ganglion cells function to transfer sensory
information about temperature, stretch, and osmolarity to the
brainstem. These sensory neurons are also activated by expo-
sure to cytokines, DAMPs, and PAMPs, and afferent signals
are relayed to the nucleus tractus solatarius and other brainstem
centers that are proximal to the efferent nuclei that regulate the
hypothalamus, pituitary, and themajor outflow tracts to the sym-
pathetic chain and vagus nerves (Chiu et al., 2013) (Binshtok
et al., 2008) (Chiu et al., 2012) (Watkins et al., 1995). Cytokines
also modulate postganglionic sympathetic neural activities,
thereby regulating the sensory information in the periphery
prior to transmission to the brain. For example, exposure of
dissociated murine superior mesenteric ganglion neurons to
TNF decreases voltage-gated calcium currents and depolariza-
tion-induced Ca2+ influx, by a mechanism attributable to altered
u-conotoxin GVIA-sensitive N-type Ca2+ channel function
(Motagally et al., 2009a, 2009b). IL-1b inhibits norepinephrine
release from adrenergic neurons and modulated the activity of
neuronal NMDA and AMPA receptor signal transduction (Liu
et al., 2013). TNF has been directly implicated as a neuromo-
dulatory factor that establishes synaptic scaling, the process
by which neurons adapt to repetitive stimulation responses
(Stellwagen and Malenka, 2006). LPS, IL-1b, and other PAMPs
and alarmins can directly activate capsacin-sensitive vagus
nerve sensory fibers, dorsal root ganglion neurons, and neurons
residing in the nodose ganglion (Chiu et al., 2013). Axon-axon
reflexes, in which neural impulses send return signals back to
the source tissue via the sensory nerves, culminate in the release
of substance P, CGRP, galanin, somatostatin, and other neuro-
peptides. These ligands interact with receptors expressed on
monocytes and lymphocytes to regulate the immune function
of these cells (Chiu et al., 2013). Thus, the sensory nervous sys-
tem, which is positioned to receive input from nearly every cell in
the body, has the requisitemolecular mechanisms tomonitor not
only the cardiovascular, chemical, mechanical, and metabolic
status of the host but also the immunological status.
The activity of efferent neural pathways that regulate homeo-
stasis is measured in laboratory mammals and humans by
recording continuous electrocardiographs and measuring heart

Figure 3. Epithelial and Endothelial Barriers Are Disrupted byHMGB1DAMPs, and in particular HMGB-1, enhance epithelial permeability byinducing paracellular gaps and cytoskeletal rearrangement. These changesoccur through decreased expression of the tight-junction proteins occludin,claudin-1, and ZO-1 as a result of decreased availability of ATP or increasedgeneration of reactive oxygen species (ROS). It is plausible that decreasedprotein expression and loss of intercellular integrity reflect an immune meta-bolic defect in the generation of energetic substrate. Alternatively, intercellularbarrier failure can occur from damage by reactive oxygen species andincreased production of DAMPs or inflammasome-induced pyroptosis.
Immunity
Review
rate variability (HRV). Spectral analysis of HRV indicates that
during severe sepsis and PCI there is impairment in vagus nerve
and sympathetic neural signals (Thayer and Lane, 2009) asso-
ciated with impaired cardiac function, depressed cardiac con-
tractility, increased heart rate, and decreased activity of the
cytokine-inhibiting inflammatory reflex (Frasure-Smith et al.,
2009; Werdan et al., 2009; Buchan et al., 2012). A study exam-
ining HRV in emergency room patients found that decreased
vagus nerve activity in patients with sepsis is associated with
an increased risk of developing septic shock, severe sepsis, or
death (Barnaby et al., 2002). Altered HRV increased the risk of
subsequent shock, and decreased vagus nerve activity corre-
lated with increased CRP and decreased IL-10 concentrations,
suggesting that the HRV measures reflect the activity of the in-
flammatory reflex (Buchan et al., 2012; Chen and Kuo, 2007). It
has also been suggested that pharmacological agents, including
statins and centrally cholinergic agonists, might confer a survival
advantage by enhancing vagus nerve and thereby restoring the
anti-inflammatory activity of the inflammatory reflex (Werdan
et al., 2009; Satapathy et al., 2011; Tracey, 2007).
Sepsis also impairs the efferent functionality of the neuroendo-
crine system, which limits the capacity of humoral mediators to
modulate the immune system and other organs (Figure 2). These
include impaired conversion of T4 to T3 resulting fromdecreased
deiodinase activity in target tissues (Ma et al., 2011) and
impaired tissue responsiveness to glucocorticoids, which nor-
mally play an important counterregulatory role in attenuating
cytokine release (Thayer, 2009; Thayer and Sternberg, 2010).
Serum catecholamine concentrations are increased in severe
sepsis and PCI, attributed to enhanced tyrosine hydroxylase
activity in the myenteric nervous system of the gut, decreased
expression of norepinephrine transporters, increased concen-
trations of syntaxin 1A, and reduced adrenergic receptor expres-
sion and G protein link signal transduction (Kumar and Sharma,
2010; Lukewich et al., 2014). Ghrelin decreases in serum during
murine CLP sepsis, whereas ghrelin administration enhances
vagus nerve signaling and decreases cytokine release (Wu
et al., 2007, 2009). These illustrative examples, together with
abundant additional evidence, have established that severe
sepsis is a state of impaired neuroendocrine signaling, and
impaired afferent and efferent neuronal signaling.
Barrier Failures, Impaired Cell Function, and EnergeticsUp to this point we have argued that the pathophysiology of
severe sepsis can be described by impaired or dysfunctional
homeostatic regulation by the sensory and effector arms of the
immune and nervous system, that the mechanism of acute sep-
tic or endotoxic shock is immunopathology mediated by TNF
released during the acute innate immune response, and that
there is a dearth of evidence supporting an immune-pathologic
mechanism of severe sepsis. However, the mechanism of lethal
organ dysfunction in severe sepsis and PCI remains unknown.
One particularly intriguing hypothesis is termed ‘‘barrier failure’’
(Figure 3). A basic principle of organ function is that homeostasis
is dependent upon the presence of intracellular barriers that
establish gradients between tissue compartments. These pro-
vide separation of blood and air in lung, blood and urine in the
kidney, blood and bile in liver, and humoral molecules and the
brain. These barriers are maintained by specialized epithelial
and endothelial cells that actively regulate the movement of
molecules and substrates across the gradients. A hallmark of
impaired homeostasis in severe sepsis is barrier incompetency.
The interface between compartments becomes porous, a defect
that leads to the appearance of hepatic enzymes, bile, renal
creatinine and other substrates in the blood, and to hypoxemia.
Endothelial cell permeability failure underlies leakage of serum
out of the blood and into the tissues, where it accumulates to
produce edema and anasarca. Leakage across the blood-brain
barrier enables cytokines, prostaglandins, and other mediators
to infiltrate the central nervous system; in severe cases, these
leaks are large enough to enable entry of monocytes, lympho-
cytes, and neutrophils as well.
Two major features of the ‘‘barrier failure’’ hypothesis align
with the evidence from clinical and animal studies of severe
sepsis. First, organ dysfunction in severe sepsis is characterized
by the appearance of cellular substrates in the serum. Second,
barrier failure can occur in the absence of appreciable significant
cell death. Failure can be visualized in experimental systems by
measuring the transit of labeled substrates across barriers or by
electron micrographs that reveal the breakdown of intracellular
barriers (Yang et al., 2006). However, these findings are not
apparent with routine histopathological analysis methods typi-
cally performed at postmortem. Thus, this is a mechanism that
can severely impair organ function without leaving many, if
any, visible traces, a finding that corresponds with the results
from postmortems in severe sepsis and PCI victims.
DAMPs and alarmins have been implicated in themechanisms
of epithelial and endothelial barrier. A prototypical example of
this mechanism is the cytokine-like transcription factor high
mobility group B-1 (HMGB1). Serum HMGB1 accumulation
in response to infection or injury is nearly universally found
in animal studies and clinical investigations of severe sepsis
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 469

Immunity
Review
(Angus et al., 2007; Andersson and Tracey, 2011; Wang et al.,
2004; Wang et al., 2004). As a universal sentinel for infection or
injury, HMGB1 appears as a delayed mediator after the onset
of infection and serum concentrations might remain elevated in
survivors—for up to 30 days in mice, and even longer in humans
(Chavan et al., 2012; Yanai et al., 2012; Yanai et al., 2009).
Inhibition of HMGB1 by administration of specific, neutralizing
monoclonal antibodies or by pharmacological agents that
suppress serum HMGB1 concentrations confers survival
advantages to animals with severe sepsis and protects against
impaired organ function and homeostasis (Qin et al., 2006; Ulloa
et al., 2002; Yang et al., 2004, 2011). HMGB1 is not elevated in
immunodeficient severe combined immunodeficient (SCID)
mice subjected to cecal ligation puncture (CLP), and these
animals are protected from sepsis-induced mortality (Ye et al.,
2012). Reconstitution with human hematopoietic stem cells prior
to CLP in these mice led to elevated serum concentrations of
human HMGB1 and was associated with lethal organ failure
(Ye et al., 2012). Further, the targeted delivery of HMGB1 small
interfering RNA attenuated serum HMGB1, reduced concen-
trations of other cytokines, prevented human lymphocyte
apoptosis, and conferred protection against lethality (Ye et al.,
2012). Direct administration of HMGB1 gives rise to elevated
serum concentrations of hepatic and renal enzymes, evidence
of organ dysfunction (Wang et al., 1999).
In molecular terms, HMGB1-induced downregulation of
epithelial permeability results from inactivation of Rac and acti-
vation of Rho, a process that results in decreased expression
of zonula occludens (ZO1) and occludin, cytoplasmic membrane
proteins that form intercellular tight junctions (Liu et al., 2006;
Sappington et al., 2002; Yang et al., 2006). HMGB1 exposure
impairs endothelial barrier function with the appearance of para-
cellular gaps and cytoskeletal rearrangement and increased
expression of surface activation markers (Wolfson et al., 2011;
Rao et al., 2007). There are three HMGB1 isoforms, termed disul-
fide HMGB1, fully reduced HMGB1, and sulfonyl HMGB1, and
each signal through mutually exclusive HMGB1 receptor super-
family members expressed on endothelial and epithelial cells
(Antoine et al., 2014; Venereau et al., 2012; Yang et al., 2012).
These HMGB1-mediatedmechanisms of epithelial and endothe-
lial barrier failure are one potential mechanism of sepsis-induced
organ dysfunction.
A second hypothesis for the pathogenic mechanism of organ
dysfunction in severe sepsis and PCI is that impaired bioener-
getics, ER stress, and mitochondrial dysfunction underlie organ
dysfunction. This model is consistent with the evidence of bland
histological findings in septic patients and animals. Patients and
animals with severe sepsis have defective function in the elec-
tron transport chain (ETC). Sepsis impairs ETC complexes I II,
III, and IV (Singer, 2014; Singer, 2007; Brealey et al., 2002;
Levy and Deutschman, 2007), findings that correlate with nitric
oxide production and might reflect a sepsis-induced generation
of reactive oxygen species and other free radicals. Complexes II
and III activity in the quadriceps was the earliest mitochondrial
abnormality noted in septic rats—all complexes became
impaired at later time points (Peruchi et al., 2011). Complex IV
dysfunction also occurs early in rodents and can act as a
sensor—increased binding of free radicals such as NO can block
the access of oxygen to the heme moiety and shut down oxida-
470 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
tive phosphorylation (Levy and Deutschman, 2007; Verma et al.,
2009). In addition to impaired electron transport, mitochondrial
membranes become permeable, resulting in the leakage of cyto-
chrome c, mitochondrial DNA, and other substrates from the
mitochondria into the cytosol. Damaged mitochondria and mito-
chondrial DNA can be removed by autophagy or can leak out of
cells, eventually accumulating in the bloodstream asDAMPs that
interact with innate immune cells (Nakahira et al., 2011; Zhang
et al., 2010). Under normal conditions, mitochondria can be re-
placed through biogenesis, which is enhanced in early experi-
mental sepsis (Haden et al., 2007) but becomes deficient later
in the time course (C.S.D., data not shown). HMGB1 modulates
biogenesis to disrupt homeostasis (Tang et al., 2011). Autophagy
participates in antigen presentation by the major histocompti-
bilty complex (MHC) class II glycoproteins in dendritic cells,
can provide metabolic fuel during T cell development, and can
affect energy metabolism in lymphocytes (Tang et al., 2011).
The importance of this pathway has been the focus of recent
work showing that administration of anthracyclines in low doses
confers protection against severe sepsis lethality in mice by a
mechanism that is dependent on activation of DNA damage
responses and autophagy pathways, revealed by deletion of
the ataxia telangiectasia mutated and autophagy-related protein
7 expression (Figueiredo et al., 2013). This and other strategies
to restore mitochondrial membrane stability and bioenergetic
capacity can protect against organ dysfunction and prevent
death.
Mitochondrial dysfunction leading to depletion of ATP is a
major feature of severe sepsis and PCI. During energy depletion,
cells revert to their most primitive level of activity, expending
energy only to support activity that is essential for cell survival.
This comes at the expense of systemic homeostasis, because
individual cells regress to function like unicellular organisms—
maintaining intracellular homeostasis but no longer performing
their specialized function that is critical for interorgan homeo-
static stability (Buchman, 2002; Gomez et al., 2014). Myocardial
cells do not contract appropriately (myocardial depression);
endothelial cells do not constrict (hypotension); the junctions
between cells fail (capillary leak); epithelial intracellular junctions
and endothelial interfaces are not maintained (barrier failure);
hepatocytes do not synthesize needed reactants and do not
detoxify endogenous or exogenous toxins (jaundice); renal
tubular cells do not properly resorb (electrolyte and water loss,
eventual shut down); transport across GI epithelial cells de-
creases; neurotransmission is impaired (peripheral neuropathy,
encephalopathy); and skeletal muscle contracts poorly (myop-
athy). Each of these hallmarks of failed cellular homeostasis is
a characteristic pathophysiological feature of severe sepsis
and PCI, and moreover, is also entirely consistent with micro-
scopic immunohistochemical pathology findings. Postmortem
analysis of animal and human sepsis victims reveals that sepsis
does not produce appreciable cell death, that cell viability is
largely preserved, and that findings of cell death are primarily
limited to lymphocyte compartments (Singer, 2014). It can be
strongly argued that cellular energetic deficiencies impair the
ability of the nervous and immune systems to modulate and
coordinate physiological homeostasis and that there are
shared molecular mechanisms of bioenergetics in somatic and
hematopoietic cells.

Immunity
Review
Impaired cellular energetics and mitochondrial dysfunction
such as occurs in sepsis activate inflammasomes (Figure 1). In-
hibition or deletion of pro-caspase-1, caspase-1, or PKR inter-
feres with inflammasome signaling and confers protection
against lethality in murine sepsis by inhibiting HMGB1 release
without suppressing antimicrobial mechanisms (Kayagaki
et al., 2011; Lamkanfi et al., 2010; Lu et al., 2012). Inflammasome
activation is also stimulated by increased production of palmi-
tate and other free fatty acids that diminish the activity of
AMP- activated kinase (AMPK), an intracellular signal transduc-
tion mechanism that modulates energy biosynthesis and lipid
metabolism (McGettrick and O’Neill, 2013; Wen et al., 2012).
Impaired mitochondrial autophagy (‘‘mitophagy’’) results in
the intracellular persistence of dysfunctional mitochondria,
increased generation of reactive oxygen species, and the
release of cytochrome c and mitochondrial DNA into the cytosol
to activate the NLRP3 inflammasome. There are numerous ex-
amples of the intersection between metabolic substrates and
activation of PKR and inflammasomes, and other immune
response pathways that are the focus of the emerging field of
‘‘immunometabolism.’’ Recent findings from this field have
important implications for understanding themechanisms of bio-
energetics and barrier failure that likely drive the pathophysi-
ology of organ dysfunction in severe sepsis and PCI.
Consider that the metabolic consequences of cellular activa-
tion are costly, requiring high rates of glycolysis, protein synthe-
sis, and ATP. For instance, in macrophages or dendritic cells,
stimulation by endotoxin or HMGB1 increases glycolysis and
enhances lactate production (Tannahill et al., 2013). O’Neill and
colleagues, by using ametabolomic screen andmicroarray anal-
ysis, recently uncovered a shift from oxidative phosphorylation
to glycolysis (Tannahill et al., 2013). They observed increases
in glycolytic intermediates, pentose phosphate pathway activity,
and altered activity in the tricarboxylic acid (TCA) cycle that re-
sulted in an increase in succinate. Elevated succinate inhibits
prolyl hydroxylase 2, the enzyme that catalyzes hydroxylation
of hypoxia inducible factor-1a (HIF-1a), leading to its degrada-
tion. Higher HIF-1a concentrations have profound effects on
the functional capacity of immune and somatic cells. In this
example, the critical metabolic substrate, succinate, also func-
tions as a signaling molecule linking intracellular bioenergetics
andmetabolism to immune responsiveness. These and other im-
munometabolic mechanisms can be activated by other DAMPs
such as nigericin, ATP, and uric acid crystals that can damage
mitochondria and thus decrease cellular NAD availability (Hane-
klaus et al., 2013; McGettrick and O’Neill, 2013; Wen et al., 2012)
with increased acetylation of tubulin, enhancing NLRP3 in-
flammasome activity. Different cell types are variably sensitive
to damage, activation, autophagy, ER stress, and programmed
cell death, reflected as the degree of tolerance to potentially
damaging stressors (Medzhitov et al., 2012). In sum, the bioen-
ergetic state that develops during severe sepsis is characterized
by disruption of metabolic enzyme pathways and substrates
that, although primarily the catalysts and products of energy
cycles, protein turnover, and ER stress, also function as intracel-
lular signaling molecules that regulate immunity and underlie
barrier failure.
Thus, we propose that severe sepsis occurs when bioener-
getic mechanisms within the cell fail, leading to intercellular bar-
riers that fail, followed by failure of homeostatic interactions
between organ systems. Prior to the availability of modern crit-
ical care to support or even replace organ function, patients
died. As Tim Buchman noted, severe sepsis and PCI that
disrupt harmony and balance in ‘‘the community of the self’’
are a manifestation of widespread network failure (Buchman,
2002). As we have argued here, disrupted cellular bioenergetics
might represent a root mechanistic cause that generates test-
able hypotheses in immunometabolism to understand severe
sepsis and PCI. Under normal circumstances, individual organ
system function is intimately tied to that of other systems. For
example, renal function and cardiac performance must be
closely coordinated to optimize blood volume, and liver func-
tion needs to be attuned to skeletal muscle activity to assure
adequate metabolism of lactate. The small oscillations in normal
function observed in most biologic measurement, for example,
HRV, result from miniscule, second-to-second adjustments
to fine-tune this coupling. These oscillations reflect orderly
coupling via a communications network that includes the neural,
endocrine, and humoral (i.e., immune) systems (Buchman,
2002). Disruption of communication between organ systems re-
sults in an uncoupling of functional interactions. The systemic
failure of homeostasis is manifested as severe sepsis, and if it
persists, as PCI.
Research Questions and Therapeutic PossibilitiesThere remain critical gaps in our fundamental knowledge of
the role of immunity in severe sepsis and PCI, but advances in
immunometabolism and the molecular intersection of the ner-
vous and immune systems are ripe for exploration. For example,
metabolic reprogramming during T cell activation is not uni-
form; rather, specific T cell lineages utilize mixed fuel oxidative
phosphorylation, aerobic glycolysis (utilizing a range of pro-
grams including mTor, HIF, or AMPK), or lipid oxidation as their
primary bioenergetic mechanism, depending upon their specific
lineage (McGettrick and O’Neill, 2013; Wen et al., 2012). Activa-
tion of the PI3K-Akt-mTOR pathway has been implicated in up-
regulating signaling through Glut1 to stimulate glycolysis and
anabolism. T cell costimulation is critical to the mechanisms
that fuel aerobic glycolysis, and failure to receive costimulation
attenuates glucose uptake and limits glycolysis. Acetylcholine
and other neurotransmitters regulate cell metabolism andmodu-
late the activity of inflammasome signals (Lu et al., 2013). These
immunometabolic signals might provide additional insight into
T cell nonresponsiveness, also termed ‘‘exhaustion,’’ that can
result from chronic persistent antigen exposure during severe
sepsis or PCI. The exhausted T cells fail to provide protection
against infection, do not self-renew, and have attenuated cyto-
kine production and cytolytic capacity. Impaired glucose meta-
bolism might contribute to T cell exhaustion and anergy, which
may be central to understanding T cell anergy, apoptosis, and
exhaustion in severe sepsis.
A rapidly expanding field is the neurophysiological regulation
of immunity, which has produced discoveries of functional and
molecular mechanisms that have been clinically deployed with
vagus nerve stimulation to treat rheumatoid arthritis (Andersson
and Tracey, 2012c). In addition to systems biological ap-
proaches that aremapping interorgan oscillatory networks in an-
imal models and in the clinic, basic advances in defining neural
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 471

Immunity
Review
circuits have been extended beyond the inflammatory reflex
control of acute TNF. Several specific neural circuits have
recently been mapped and defined by anatomic and molecular
mechanisms. For example, the ‘‘gateway reflex’’ is activated
by skeletal muscle afferents that respond to metabolic activity
and culminates in efferent adrenergic signals that modulate
pathogenic T cell entry into the CNS via expression of endothelial
cell-derived chemokine CCL20 (Arima et al., 2012). This is a po-
tential mechanism by which altered skeletal muscle metabolism
or decreased activity in bed-ridden, metabolically-stressed se-
vere sepsis patients can modulate blood-brain barrier porosity
to inflammatory cells andmediators. Another reflex neural circuit
that is mediated by peripheral sensory stimulation culminates in
vagus nerve signals to the adrenal gland (Torres-Rosas et al.,
2014). The adrenal, in turn, responds by enhancing dopamine
release to suppress innate immunity. The use of adrenergic
and cholinergic modulators is widespread in severe sepsis, but
the influence of these interventions on the molecular mecha-
nisms governing immunometabolism is not known. Moreover,
there have been a number of pharmacological approaches to
enhance anti-inflammatory neural circuits that are highly protec-
tive in animal models of sepsis. For instance, CNI-1493 (Semapi-
mod), galatamine, and centrally acting M1 muscarininc receptor
agonists have all been shown to stimulate the inflammatory re-
flex, inhibit HMGB1 release, and confer protection against organ
dysfunction and death in animal models of severe sepsis. Further
functional, pharmacological, and molecular mapping of these
regulatory circuits seems warranted and timely.
Recent controversy regarding the reliability and relevance
of animal models of sepsis has not dampened enthusiasm
for dissecting pathogenic mechanisms (Ward and Bosmann,
2012). As noted above, early work in rodent models of shock
has generated selective biological agents that are clinically
approved to inhibit inflammation in millions of patients. Animal
models are necessary in order to understand the in vivo interac-
tions between the nervous and immune systems, to reveal
mechanisms of barrier functionality, and to assess the activity
of cellular energetics in the context of systemically impaired
homeostasis. It has been known since the early 1980s that the
acute animal models represent a spectrum of disorders that
occurs prior to the time the patients will arrive for care, and
that targeting early mediators in these patients after the fact is
like closing the barn door after the animals have fled (Tracey
et al., 1987). The identification of HMGB1 as a mediator of auto-
phagy, barrier failure, and cognitive function in animal models
that survive severe sepsis raises testable hypotheses about
intervening late in pathogenesis (Chavan et al., 2012). A role of
late mediators in disrupting barrier function and cell energetics
is being pursued in acute and chronic surviving animal models.
For example, the persistent elevation of serum HMGB1 concen-
trations lasting for weeks or longer has been identified in murine
models and human sepsis survivors, and administration of
anti-HMGB1 antibodies restores cognitive and immunological
functions (Chavan et al., 2012; Angus et al., 2007). There is
a tremendous opportunity and need to use long-term animal
models to examine the molecular mechanisms underlying the
debilitating neurological and immunological impairments limiting
recovery for the more than 500,000 patients who will survive
sepsis each year. Recent data implicating enhanced expression
472 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
of TNF and IL-1 in the hippocampus as a result of persistently
elevated HMGB1 in survivors indicate that, by intervening to
inhibit this mediator during recovery, it might be possible to limit
sepsis-induced defects in cognition and immune function.
Concluding RemarksAcute septic shock is an immunopathology, mediated by
excessive TNF release, that represents a small proportion of
larger population of patients with sepsis. Timely administration
of antibiotics, fluids, and oxygen to patients with sepsis or
severe sepsis has lowered the mortality rate, although this
has not prevented or reversed the development of PCI, which
is often associated with ‘‘immunosuppression.’’ We suggest
that severe sepsis and PCI are not immunopathologies but
represent a failure of homeostasis that results from dysfunction
of the neuroendocrine and immune systems—the two major
systems that maintain healthy intercommunication between
organs. The afferent and efferent components of both systems
are impaired in severe sepsis and PCI by molecular and cellular
mechanisms that are currently the focus of active research. The
major unanswered questions about the onset and persistence
of cellular dysfunction and organ failure, which are the ultimate
causes of death, center on the immunometabolic signaling
pathways that impair cell function. These mechanisms likely
underlie the failure of intracellular barriers and immunity. It is
plausible that shared molecular mechanisms of apoptosis,
autophagy, bioenergetics, and cell stress are operative in
somatic cells and hematopoietic cells. The opportunity to delin-
eate these molecular mechanisms holds promise to deliver
future therapies based on understanding the fundamental
mechanisms of failed homeostasis and how these characterize
severe sepsis and PCI.
REFERENCES
Ahmad, S., Tejuja, A., Newman, K.D., Zarychanski, R., and Seely, A.J. (2009).Clinical review: a review and analysis of heart rate variability and the diagnosisand prognosis of infection. Crit. Care 13, 232.
Andersson, U., and Tracey, K.J. (2011). HMGB1 is a therapeutic target for ster-ile inflammation and infection. Annu. Rev. Immunol. 29, 139–162.
Andersson, U., and Tracey, K.J. (2012a). Reflex principles of immunologicalhomeostasis. Annu. Rev. Immunol. 30, 313–335.
Andersson, U., and Tracey, K.J. (2012b). Neural reflexes in inflammation andimmunity. J. Exp. Med. 209, 1057–1068.
Andersson, U., and Tracey, K.J. (2012c). A new approach to rheumatoidarthritis: treating inflammation with computerized nerve stimulation. Cerebrum2012, 3.
Angus, D.C., and van der Poll, T. (2013). Severe sepsis and septic shock.N. Engl. J. Med. 369, 840–851.
Angus, D.C., Yang, L., Kong, L., Kellum, J.A., Delude, R.L., Tracey, K.J., andWeissfeld, L.; GenIMS Investigators (2007). Circulating high-mobility groupbox 1 (HMGB1) concentrations are elevated in both uncomplicated pneu-monia and pneumonia with severe sepsis. Crit. Care Med. 35, 1061–1067.
Antoine, D.J., Harris, H.E., Andersson, U., Tracey, K.J., and Bianchi, M.E.(2014). A systematic nomenclature for the redox states of high mobility groupbox (HMGB) proteins.Mol. Med. Published online February 10, 2014. http://dx.doi.org/10.2119/molmed.2014.00022.
Arima, Y., Harada, M., Kamimura, D., Park, J.-H., Kawano, F., Yull, F.E., Kawa-moto, T., Iwakura, Y., Betz, U.A., Marquez, G., et al. (2012). Regional neuralactivation defines a gateway for autoreactive T cells to cross the blood-brainbarrier. Cell 148, 447–457.

Immunity
Review
Barnaby, D., Ferrick, K., Kaplan, D.T., Shah, S., Bijur, P., and Gallagher, E.J.(2002). Heart rate variability in emergency department patients with sepsis.Acad. Emerg. Med. 9, 661–670.
Bernik, T.R., Friedman, S.G., Ochani, M., DiRaimo, R., Ulloa, L., Yang, H.,Sudan, S., Czura, C.J., Ivanova, S.M., and Tracey, K.J. (2002). Pharmacolog-ical stimulation of the cholinergic antiinflammatory pathway. J. Exp. Med. 195,781–788.
Binshtok, A.M., Wang, H., Zimmermann, K., Amaya, F., Vardeh, D., Shi, L.,Brenner, G.J., Ji, R.-R., Bean, B.P., Woolf, C.J., and Samad, T.A. (2008).Nociceptors are interleukin-1beta sensors. J. Neurosci. 28, 14062–14073.
Bone, R.C., Sibbald, W.J., and Sprung, C.L. (1992). The ACCP-SCCMconsensus conference on sepsis and organ failure. Chest 101, 1481–1483.
Boomer, J.S., To, K., Chang, K.C., Takasu, O., Osborne, D.F., Walton, A.H.,Bricker, T.L., Jarman, S.D., 2nd, Kreisel, D., Krupnick, A.S., et al. (2011). Immu-nosuppression in patients who die of sepsis and multiple organ failure. JAMA306, 2594–2605.
Borovikova, L.V., Ivanova, S., Zhang, M., Yang, H., Botchkina, G.I., Watkins,L.R., Wang, H., Abumrad, N., Eaton, J.W., and Tracey, K.J. (2000). Vagusnerve stimulation attenuates the systemic inflammatory response to endo-toxin. Nature 405, 458–462.
Bosmann, M., and Ward, P.A. (2013). The inflammatory response in sepsis.Trends Immunol. 34, 129–136.
Brealey, D., Brand, M., Hargreaves, I., Heales, S., Land, J., Smolenski, R.,Davies, N.A., Cooper, C.E., and Singer, M. (2002). Association between mito-chondrial dysfunction and severity and outcome of septic shock. Lancet 360,219–223.
Buchan, C.A., Bravi, A., and Seely, A.J.E. (2012). Variability analysis and thediagnosis, management, and treatment of sepsis. Curr. Infect. Dis. Rep. 14,512–521.
Buchman, T.G. (2002). The community of the self. Nature 420, 246–251.
Cavaillon, J.-M., and Adib-Conquy, M. (2006). Bench-to-bedside review:endotoxin tolerance as a model of leukocyte reprogramming in sepsis. Crit.Care 10, 233.
Chan, A.C., and Carter, P.J. (2010). Therapeutic antibodies for autoimmunityand inflammation. Nat. Rev. Immunol. 10, 301–316.
Chavan, S.S., Huerta, P.T., Robbiati, S., Valdes-Ferrer, S.I., Ochani, M., Dan-cho, M., Frankfurt, M., Volpe, B.T., Tracey, K.J., and Diamond, B. (2012).HMGB1 mediates cognitive impairment in sepsis survivors. Mol. Med. 18,930–937.
Chen, W.-L., and Kuo, C.-D. (2007). Characteristics of heart rate variability canpredict impending septic shock in emergency department patients withsepsis. Acad. Emerg. Med. 14, 392–397.
Chiu, I.M., von Hehn, C.A., and Woolf, C.J. (2012). Neurogenic inflammationand the peripheral nervous system in host defense and immunopathology.Nat. Neurosci. 15, 1063–1067.
Chiu, I.M.I., Heesters, B.A., Ghasemlou, N., Von Hehn, C.A., Zhao, F., Tran, J.,Wainger, B., Strominger, A., Muralidharan, S., Horswill, A.R., et al. (2013). Bac-teria activate sensory neurons that modulate pain and inflammation. Nature501, 52–57.
Dwyer, J. (2012). One Boy’s DeathMoves State to Action to Prevent. New YorkTimes. A25.
Felmet, K.A., Hall, M.W., Clark, R.S.B., Jaffe, R., and Carcillo, J.A. (2005). Pro-longed lymphopenia, lymphoid depletion, and hypoprolactinemia in childrenwith nosocomial sepsis and multiple organ failure. J. Immunol. 174, 3765–3772.
Figueiredo, N., Chora, A., Raquel, H., Pejanovic, N., Pereira, P., Hartleben, B.,Neves-Costa, A., Moita, C., Pedroso, D., Pinto, A., et al. (2013). Anthracyclinesinduce DNA damage response-mediated protection against severe sepsis.Immunity 39, 874–884.
Frasure-Smith, N., Lesperance, F., Irwin, M.R., Talajic, M., and Pollock, B.G.(2009). The relationships among heart rate variability, inflammatory markersand depression in coronary heart disease patients. Brain Behav. Immun. 23,1140–1147.
Goehler, L.E., Relton, J.K., Dripps, D., Kiechle, R., Tartaglia, N., Maier, S.F.,and Watkins, L.R. (1997). Vagal paraganglia bind biotinylated interleukin-1 re-ceptor antagonist: a possible mechanism for immune-to-brain communica-tion. Brain Res. Bull. 43, 357–364.
Gomez, H., Ince, C., De Backer, D., Pickkers, P., Payen, D., Hotchkiss, J., andKellum, J.A. (2014). A unified theory of sepsis-induced acute kidney injury:inflammation, microcirculatory dysfunction, bioenergetics, and the tubularcell adaptation to injury. Shock 41, 3–11.
Haden, D.W., Suliman, H.B., Carraway, M.S., Welty-Wolf, K.E., Ali, A.S., Shi-tara, H., Yonekawa, H., and Piantadosi, C.A. (2007). Mitochondrial biogenesisrestores oxidative metabolism during Staphylococcus aureus sepsis. Am. J.Respir. Crit. Care Med. 176, 768–777.
Haneklaus, M., O’Neill, L.A., and Coll, R.C. (2013). Modulatory mechanismscontrolling the NLRP3 inflammasome in inflammation: recent developments.Curr. Opin. Immunol. 25, 40–45.
Inoue, S., Suzuki-Utsunomiya, K., Okada, Y., Taira, T., Iida, Y., Miura, N., Tsuji,T., Yamagiwa, T., Morita, S., Chiba, T., et al. (2013). Reduction of immunocom-petent T cells followed by prolonged lymphopenia in severe sepsis in theelderly. Crit. Care Med. 41, 810–819.
Iskander, K.N., Osuchowski, M.F., Stearns-Kurosawa, D.J., Kurosawa, S.,Stepien, D., Valentine, C., and Remick, D.G. (2013). Sepsis: multiple abnormal-ities, heterogeneous responses, and evolving understanding. Physiol. Rev. 93,1247–1288.
Iwashyna, T.J., Ely, E.W., Smith, D.M., and Langa, K.M. (2010). Long-termcognitive impairment and functional disability among survivors of severesepsis. JAMA 304, 1787–1794.
Kaukonen, K.M., Bailey, M., Suzuki, S., Pilcher, D., and Bellomo, R. (2014).Mortality Related to Severe Sepsis and Septic Shock Among Critically Ill Pa-tients in Australia and New Zealand, 2000-2012. J. Am.Med. Assoc. Publishedonline March 18, 2014. http://dx.doi.org/10.1001/jama.2014.2637.
Kawai, T., and Akira, S. (2011). Toll-like receptors and their crosstalk with otherinnate receptors in infection and immunity. Immunity 34, 637–650.
Kayagaki, N., Warming, S., Lamkanfi, M., Vande Walle, L., Louie, S., Dong, J.,Newton, K., Qu, Y., Liu, J., Heldens, S., et al. (2011). Non-canonical inflamma-some activation targets caspase-11. Nature 479, 117–121.
Kumar, V., and Sharma, A. (2010). Is neuroimmunomodulation a future thera-peutic approach for sepsis? Int. Immunopharmacol. 10, 9–17.
Lamkanfi, M., Sarkar, A., Vande Walle, L., Vitari, A.C., Amer, A.O., Wewers,M.D., Tracey, K.J., Kanneganti, T.-D., and Dixit, V.M. (2010). Inflammasome-dependent release of the alarmin HMGB1 in endotoxemia. J. Immunol. 185,4385–4392.
Lehrer, P., Karavidas, M.K., Lu, S.-E., Coyle, S.M., Oikawa, L.O., Macor, M.,Calvano, S.E., and Lowry, S.F. (2010). Voluntarily produced increases in heartrate variability modulate autonomic effects of endotoxin induced systemicinflammation: an exploratory study. Appl. Psychophysiol. Biofeedback 35,303–315.
Levy, R.J., and Deutschman, C.S. (2007). Cytochrome c oxidase dysfunctionin sepsis. Crit. Care Med. Suppl. 35, S468–S475.
Liu, S., Stolz, D.B., Sappington, P.L., Macias, C.A., Killeen, M.E., Tenhunen,J.J., Delude, R.L., and Fink, M.P. (2006). HMGB1 is secreted by immunostimu-lated enterocytes and contributes to cytomix-induced hyperpermeability ofCaco-2 monolayers. Am. J. Physiol. Cell Physiol. 290, C990–C999.
Liu, T., Jiang, C.-Y., Fujita, T., Luo, S.-W., and Kumamoto, E. (2013). Enhance-ment by interleukin-1b of AMPA and NMDA receptor-mediated currents inadult rat spinal superficial dorsal horn neurons. Mol. Pain 9, 16.
Lu, B., Nakamura, T., Inouye, K., Li, J., Tang, Y., Lundback, P., Valdes-Ferrer,S.I., Olofsson, P.S., Kalb, T., Roth, J., et al. (2012). Novel role of PKR in inflam-masome activation and HMGB1 release. Nature 488, 670–674.
Lu, B., Wang, H., Andersson, U., and Tracey, K.J. (2013). Regulation ofHMGB1 release by inflammasomes. Protein Cell 4, 163–167.
Lukewich, M.K., Rogers, R.C., and Lomax, A.E. (2014). Divergent neuroendo-crine responses to localized and systemic inflammation. Semin. Immunol.Published online January 30, 2014. http://dx.doi.org/10.1016/j.smim.2014.01.004.
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 473

Immunity
Review
Ma, S.-F., Xie, L., Pino-Yanes, M., Sammani, S., Wade, M.S., Letsiou, E., Sie-gler, J.,Wang, T., Infusino, G., Kittles, R.A., et al. (2011). Type 2 deiodinase andhost responses of sepsis and acute lung injury. Am. J. Respir. Cell Mol. Biol.45, 1203–1211.
Marshall, J.C. (2008). Sepsis: rethinking the approach to clinical research.J. Leukoc. Biol. 83, 471–482.
McGettrick, A.F., and O’Neill, L.A. (2013). How metabolism generates signalsduring innate immunity and inflammation. J. Biol. Chem. 288, 22893–22898.
Medzhitov, R. (2010). Inflammation 2010: new adventures of an old flame. Cell140, 771–776.
Medzhitov, R., Schneider, D.S., and Soares, M.P. (2012). Disease tolerance asa defense strategy. Science 335, 936–941.
Meisel, C., Schefold, J.C., Pschowski, R., Baumann, T., Hetzger, K., Gregor,J., Weber-Carstens, S., Hasper, D., Keh, D., Zuckermann, H., et al. (2009).Granulocyte-macrophage colony-stimulating factor to reverse sepsis-associ-ated immunosuppression: a double-blind, randomized, placebo-controlledmulticenter trial. Am. J. Respir. Crit. Care Med. 180, 640–648.
Monneret, G., Venet, F., Pachot, A., and Lepape, A. (2008). Monitoring immunedysfunctions in the septic patient: a new skin for the old ceremony. Mol. Med.14, 64–78.
Motagally, M.A., Lukewich, M.K., Chisholm, S.P., Neshat, S., and Lomax, A.E.(2009a). Tumour necrosis factor alpha activates nuclear factor kappaB signal-ling to reduce N-type voltage-gated Ca2+ current in postganglionic sympa-thetic neurons. J. Physiol. 587, 2623–2634.
Motagally, M.A., Neshat, S., and Lomax, A.E. (2009b). Inhibition of sympa-thetic N-type voltage-gated Ca2+ current underlies the reduction in norepi-nephrine release during colitis. Am. J. Physiol. Gastrointest. Liver Physiol.296, G1077–G1084.
Nakahira, K., Haspel, J.A., Rathinam, V.A.K., Lee, S.-J., Dolinay, T., Lam, H.C.,Englert, J.A., Rabinovitch, M., Cernadas, M., Kim, H.P., et al. (2011). Auto-phagy proteins regulate innate immune responses by inhibiting the releaseof mitochondrial DNA mediated by the NALP3 inflammasome. Nat. Immunol.12, 222–230.
Nathan, C., and Ding, A. (2010). Nonresolving inflammation. Cell 140, 871–882.
Nierhaus, A., Montag, B., Timmler, N., Frings, D.P., Gutensohn, K., Jung, R.,Schneider, C.G., Pothmann, W., Brassel, A.K., and Schulte Am Esch, J.(2003). Reversal of immunoparalysis by recombinant human granulocyte-macrophage colony-stimulating factor in patients with severe sepsis. IntensiveCare Med. 29, 646–651.
Niijima, A. (1996). The afferent discharges from sensors for interleukin 1 beta inthe hepatoportal system in the anesthetized rat. J. Auton. Nerv. Syst. 61,287–291.
Niijima, A., Hori, T., Aou, S., and Oomura, Y. (1991). The effects of interleukin-1beta on the activity of adrenal, splenic and renal sympathetic nerves in the rat.J. Auton. Nerv. Syst. 36, 183–192.
O’Neill, L.A., Golenbock, D., and Bowie, A.G. (2013). The history of Toll-likereceptors - redefining innate immunity. Nat. Rev. Immunol. 13, 453–460.
Peruchi, B.B., Petronilho, F., Rojas, H.A., Constantino, L., Mina, F., Vuolo, F.,Cardoso, M.R., Goncalves, C.L., Rezin, G.T., Streck, E.L., and Dal-Pizzol, F.(2011). Skeletal muscle electron transport chain dysfunction after sepsis inrats. J. Surg. Res. 167, e333–e338.
Qin, S., Wang, H., Yuan, R., Li, H., Ochani, M., Ochani, K., Rosas-Ballina, M.,Czura, C.J., Huston, J.M., Miller, E., et al. (2006). Role of HMGB1 in apoptosis-mediated sepsis lethality. J. Exp. Med. 203, 1637–1642.
Rao, D.A., Tracey, K.J., and Pober, J.S. (2007). IL-1alpha and IL-1beta areendogenousmediators linking cell injury to the adaptive alloimmune response.J. Immunol. 179, 6536–6546.
Rosas-Ballina, M., Ochani, M., Parrish, W.R., Ochani, K., Harris, Y.T., Huston,J.M., Chavan, S., and Tracey, K.J. (2008). Splenic nerve is required for cholin-ergic antiinflammatory pathway control of TNF in endotoxemia. Proc. Natl.Acad. Sci. USA 105, 11008–11013.
Rosas-Ballina, M., Olofsson, P.S., Ochani, M., Valdes-Ferrer, S.I., Levine, Y.A.,Reardon, C., Tusche, M.W., Pavlov, V.A., Andersson, U., Chavan, S., et al.
474 Immunity 40, April 17, 2014 ª2014 Elsevier Inc.
(2011). Acetylcholine-synthesizing T cells relay neural signals in a vagus nervecircuit. Science 334, 98–101.
Sappington, P.L., Yang, R., Yang, H., Tracey, K.J., Delude, R.L., and Fink, M.P.(2002). HMGB1 B box increases the permeability of Caco-2 enterocytic mono-layers and impairs intestinal barrier function in mice. Gastroenterology 123,790–802.
Sarkar, A., Hall, M.W., Exline, M., Hart, J., Knatz, N., Gatson, N.T., andWewers, M.D. (2006). Caspase-1 regulates Escherichia coli sepsis and splenicB cell apoptosis independently of interleukin-1beta and interleukin-18. Am. J.Respir. Crit. Care Med. 174, 1003–1010.
Satapathy, S.K., Ochani, M., Dancho, M., Hudson, L.K., Rosas-Ballina, M.,Valdes-Ferrer, S.I., Olofsson, P.S., Harris, Y.T., Roth, J., Chavan, S., et al.(2011). Galantamine alleviates inflammation and other obesity-associatedcomplications in high-fat diet-fed mice. Mol. Med. 17, 599–606.
Schroder, K., Zhou, R., and Tschopp, J. (2010). The NLRP3 inflammasome:a sensor for metabolic danger? Science 327, 296–300.
Schwab, J.M., Chiang, N., Arita, M., and Serhan, C.N. (2007). Resolvin E1and protectin D1 activate inflammation-resolution programmes. Nature 447,869–874.
Singer, M. (2007). Mitochondrial function in sepsis: acute phase versus multi-ple organ failure. Crit. Care Med. Suppl. 35, S441–S448.
Singer, M. (2014). The role of mitochondrial dysfunction in sepsis-inducedmulti-organ failure. Virulence 5, 66–72.
Stearns-Kurosawa, D.J., Osuchowski, M.F., Valentine, C., Kurosawa, S., andRemick, D.G. (2011). The pathogenesis of sepsis. Annu. Rev. Pathol. 6, 19–48.
Stellwagen, D., and Malenka, R.C. (2006). Synaptic scaling mediated by glialTNF-alpha. Nature 440, 1054–1059.
Tang, D., Kang, R., Zeh, H.J., 3rd, and Lotze, M.T. (2011). High-mobility groupbox 1, oxidative stress, and disease. Antioxid. Redox Signal. 14, 1315–1335.
Tannahill, G.M., Curtis, A.M., Adamik, J., Palsson-McDermott, E.M.,McGettrick, A.F., Goel, G., Frezza, C., Bernard, N.J., Kelly, B., Foley, N.H.,et al. (2013). Succinate is an inflammatory signal that induces IL-1b throughHIF-1a. Nature 496, 238–242.
Thayer, J.F. (2009). Vagal tone and the inflammatory reflex. Cleve. Clin. J. Med.76 (Suppl 2 ), S23–S26.
Thayer, J.F., and Lane, R.D. (2009). Claude Bernard and the heart-brainconnection: further elaboration of a model of neurovisceral integration. Neuro-sci. Biobehav. Rev. 33, 81–88.
Thayer, J.F., and Sternberg, E.M. (2010). Neural aspects of immunomodula-tion: focus on the vagus nerve. Brain Behav. Immun. 24, 1223–1228.
Torres-Rosas, R., Yehia, G., Pena, G., Mishra, P., Del Rocio Thompson-Bonilla, M., Moreno-Eutimio, M.A., Arriaga-Pizano, L.A., Isibasi, A., and Ulloa,L. (2014). Dopamine mediates vagal modulation of the immune system byelectroacupuncture. Nat. Med. 20, 291–295.
Tracey, K.J. (2002). The inflammatory reflex. Nature 420, 853–859.
Tracey, K.J. (2007). Physiology and immunology of the cholinergic antiinflam-matory pathway. J. Clin. Invest. 117, 289–296.
Tracey, K.J. (2009). Reflex control of immunity. Nat. Rev. Immunol. 9, 418–428.
Tracey, K.J., Beutler, B., Lowry, S.F., Merryweather, J., Wolpe, S., Milsark,I.W., Hariri, R.J., Fahey, T.J., 3rd, Zentella, A., Albert, J.D., et al. (1986). Shockand tissue injury induced by recombinant human cachectin. Science 234,470–474.
Tracey, K.J., Fong, Y., Hesse, D.G., Manogue, K.R., Lee, A.T., Kuo, G.C.,Lowry, S.F., and Cerami, A. (1987). Anti-cachectin/TNFmonoclonal antibodiesprevent septic shock during lethal bacteraemia. Nature 330, 662–664.
Ulloa, L., Ochani, M., Yang, H., Tanovic, M., Halperin, D., Yang, R., Czura, C.J.,Fink, M.P., and Tracey, K.J. (2002). Ethyl pyruvate prevents lethality in micewith established lethal sepsis and systemic inflammation. Proc. Natl. Acad.Sci. USA 99, 12351–12356.
Venereau, E., Casalgrandi, M., Schiraldi, M., Antoine, D.J., Cattaneo, A., DeMarchis, F., Liu, J., Antonelli, A., Preti, A., Raeli, L., et al. (2012). Mutually

Immunity
Review
exclusive redox forms of HMGB1 promote cell recruitment or proinflammatorycytokine release. J. Exp. Med. 209, 1519–1528.
Verma, R., Huang, Z., Deutschman, C.S., and Levy, R.J. (2009). Caffeine re-stores myocardial cytochrome oxidase activity and improves cardiac functionduring sepsis. Crit. Care Med. 37, 1397–1402.
Vincent, J.-L., Opal, S.M., Marshall, J.C., and Tracey, K.J. (2013). Sepsis def-initions: time for change. Lancet 381, 774–775.
Wang, H., Bloom, O., Zhang, M., Vishnubhakat, J.M., Ombrellino, M., Che, J.,Frazier, A., Yang, H., Ivanova, S., Borovikova, L., et al. (1999). HMG-1 as a latemediator of endotoxin lethality in mice. Science 285, 248–251.
Wang, H.H., Yu, M., Ochani, M., Amella, C.A., Tanovic, M., Susarla, S., Li, J.H.,Wang, H., Yang, H., Ulloa, L., et al. (2003). Nicotinic acetylcholine receptoralpha7 subunit is an essential regulator of inflammation. Nature 421, 384–388.
Wang, H.H., Liao, H., Ochani, M., Justiniani, M., Lin, X., Yang, L., Al-Abed, Y.,Wang, H., Metz, C., Miller, E.J., et al. (2004). Cholinergic agonists inhibitHMGB1 release and improve survival in experimental sepsis. Nat. Med. 10,1216–1221.
Wang, H., Liao, H., Ochani, M., Justiniani, M., Lin, X., Hong, L., Al-abed, Y.,Wang, H., Metz, C., Miller, E.J., et al. (2004). Cholinergic Agonists InhibitHMGB1 Release and Improve Survival in Established Severe Sepsis. NatMed. 10, 1216–1221.
Ward, P.A., and Bosmann, M. (2012). A historical perspective on sepsis. Am. J.Pathol. 181, 2–7.
Watkins, L.R., Goehler, L.E., Relton, J.K., Tartaglia, N., Silbert, L., Martin, D.,and Maier, S.F. (1995). Blockade of interleukin-1 induced hyperthermia bysubdiaphragmatic vagotomy: evidence for vagal mediation of immune-braincommunication. Neurosci. Lett. 183, 27–31.
Wen, H., Ting, J.P.-Y., and O’Neill, L.A. (2012). A role for the NLRP3 inflamma-some in metabolic diseases—did Warburg miss inflammation? Nat. Immunol.13, 352–357.
Werdan, K., Schmidt, H., Ebelt, H., Zorn-Pauly, K., Koidl, B., Hoke, R.S., Hein-roth, K., and Muller-Werdan, U. (2009). Impaired regulation of cardiac functionin sepsis, SIRS, and MODS. Can. J. Physiol. Pharmacol. 87, 266–274.
Wolfson, R.K., Chiang, E.T., and Garcia, J.G.N. (2011). HMGB1 induceshuman lung endothelial cell cytoskeletal rearrangement and barrier disruption.Microvasc. Res. 81, 189–197.
Wree, A., Eguchi, A., McGeough, M.D., Pena, C.A., Johnson, C.D., Canbay, A.,Hoffman, H.M., and Feldstein, A.E. (2014). NLRP3 inflammasome activation
results in hepatocyte pyroptosis, liver inflammation, and fibrosis in mice. Hep-atology 59, 898–910.
Wu, R., Dong, W., Cui, X., Zhou, M., Simms, H.H., Ravikumar, T.S., andWang,P. (2007). Ghrelin down-regulates proinflammatory cytokines in sepsis throughactivation of the vagus nerve. Ann. Surg. 245, 480–486.
Wu, R., Dong, W., Qiang, X., Wang, H., Blau, S.A., Ravikumar, T.S., andWang,P. (2009). Orexigenic hormone ghrelin ameliorates gut barrier dysfunction insepsis in rats. Crit. Care Med. 37, 2421–2426.
Yanai, H., Ban, T., Wang, Z., Choi, M.K., Kawamura, T., Negishi, H., Nakasato,M., Lu, Y., Hangai, S., Koshiba, R., et al. (2009). HMGB proteins functionas universal sentinels for nucleic-acid-mediated innate immune responses.Nature 462, 99–103.
Yanai, H., Chiba, S., Ban, T., Nakaima, Y., Onoe, T., and Ohdan, H. (2011).Suppression of immune responses by nonimmunogenic oligodeoxynucleoti-des with high affinity for high-mobility group box proteins (HMGBs). Proc.Natl. Acad. Sci. U. 108, 11542–11547.
Yanai, H., Ban, T., and Taniguchi, T. (2012). High-mobility group box family ofproteins: ligand and sensor for innate immunity. Trends Immunol. 33, 633–640.
Yang, H., Ochani, M., Li, J., Qiang, X., Tanovic, M., Harris, H.E., Susarla, S.M.,Ulloa, L., Wang, H.H., DiRaimo, R., et al. (2004). Reversing established sepsiswith antagonists of endogenous high-mobility group box 1. Proc. Natl. Acad.Sci. USA 101, 296–301.
Yang, R., Harada, T., Mollen, K.P., Prince, J.M., Levy, R.M., Englert, J.A., Gal-lowitsch-Puerta,M., Yang, L., Yang, H., Tracey, K.J., et al. (2006). Anti-HMGB1neutralizing antibody ameliorates gut barrier dysfunction and improves sur-vival after hemorrhagic shock. Mol. Med. 12, 105–114.
Yang, H., Lundback, P., Ottosson, L., Erlandsson-Harris, H., Venereau, E.,Bianchi, M.E., Al-Abed, Y., Andersson, U., Tracey, K.J., and Antoine, D.J.(2012). Redox modification of cysteine residues regulates the cytokine activityof high mobility group box-1 (HMGB1). Mol. Med. 18, 250–259.
Ye, C., Choi, J.-G., Abraham, S., Wu, H., Diaz, D., Terreros, D., Shankar, P.,and Manjunath, N. (2012). Human macrophage and dendritic cell-specificsilencing of high-mobility group protein B1 ameliorates sepsis in a humanizedmouse model. Proc. Natl. Acad. Sci. USA 109, 21052–21057.
Zhang, Q., Raoof, M., Chen, Y., Sumi, Y., Sursal, T., Junger, W., Brohi, K., Ita-gaki, K., and Hauser, C.J. (2010). Circulating mitochondrial DAMPs causeinflammatory responses to injury. Nature 464, 104–107.
Immunity 40, April 17, 2014 ª2014 Elsevier Inc. 475