Sepsis
-
Upload
timothy-zagada -
Category
Health & Medicine
-
view
807 -
download
0
description
Transcript of Sepsis

DEFINITION OF TERMS• BACTEREMIA: bacteria in blood, evidence with (+) blood culture
• SEPTICEMIA: presence of microbes or their toxins in blood
• SIRS - ANY Two or more of the following: 1. Temperature
◦ 1.1.Fever → oral T >38ʼC
◦ 1.2.Hypothermia <36ʼ
2. Respiratory Rate◦ 2.1.Tachypnea >24cpm
3. Tachycardia >90bpm 4. WBC
◦ 4.1.Leukocytosis >12,000/uL
◦ 4.2.Leukopenia <4,000/uL
◦ 4.3. >10%band cells
◦ 4.4. May have non-infectious etiology
• SEPSIS: SIRS + proven microbial etiology
Harrison’ s Internal Medicine 18th edition1
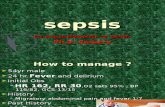
SEPSIS
GROUP 1
Camacho, Hans Robert C. Francisco, Rimmon Pineda, Francis Ivan G. Yang, Sheryl Ray B. Zagada, Timothy M.
SEPSIS

Sepsis
• SEPSIS + severe distant organ dysfunction = SEVERE SEPSIS•SEVERE SEPSIS + Hypoperfusion/Hypotension = SEPTIC SHOCK
• Sepsis often reversible• Septic shock usually succumb
SEPTIC SHOCK >1hr not respond to fluid resuscitation or pressor administration = REFRACTORY SEPTIC SHOCK
Dysfunction of more than one organ, requiring
Intervention to maintain Homeostasis = MODS
- according to National Institute of Health define as an illness in which the body has a severe response to microbial infections.
Harrison’ s Internal Medicine 18th edition
2

Severe sepsis can be a response to any class of microorganism
Microbial invasion in the blood stream –
not ESSENTIAL , since local inflammation can also illicit organ dysfunction and hypotension.
ETIOLOGY
Harrison’ s Internal Medicine 18th edition3

Blood cultures are positive:◦ 20–40% of Severe sepsis cases◦40–70% of septic shock cases
Of cases with positive blood cultures, ◦40% -gram-positive bacteria, ◦35% t - gram-negative bacteria,◦11 % - Polymicrobial◦7% - fungi ◦<5% - classic pathogens
•(-) blood culture patients: the etiologic agent is often established by culture or microscopic examination of infected material from a local site
ETIOLOGY
Harrison’ s Internal Medicine 18th edition4

The septic response is a contributing factor in >200,000 deaths per year in the United States.
The incidence of severe sepsis and septic shock has increased over the past 20 years
The annual number of cases is now >700,000 (~3 per 1000 population).
Epidemiology of sepsis: an update. (2001)National Center for Biotechnology Informationhttp://www.ncbi.nlm.nih.gov/pubmed/11445744
EPIDEMIOLOGY
5

EPIDEMIOLOGY
6

EPIDEMIOLOGY
7

Patients hospitalized for septicemia or sepsis were more severely ill than patients hospitalized for another diagnosis.
Patients hospitalized for septicemia or sepsis stayed longer than other inpatients.
Patients hospitalized for septicemia or sepsis were more than eight times as likely to die during their hospitalization.
8

11th National Convention on Statistics (NCS), 2010NEWBORN DEATHS IN THE PHILIPPINESAurora T. Reolalas* and Ma. Goretti M. Novilla
Chief, Vital Statistics DivisionNational Statistics Office9

Neonatal Sepsis in the PhilippinesGram-negative organisms
comprised the majority of the neonatal infections, with Pseudomonas and Burkholderia being the most prevalent.
PIDSP Journal 2011 Vol 12 No.2 ETIOLOGY OF NEONATAL SEPSIS IN FIVE URBAN HOSPITALS IN THE PHILIPPINESCopyright ® 2011
10

LBP
Bacteria
LPS Phagocyte
CD 14
Toxin Recognition by the Host
11

LBPBacteria
LPS Phagocyte
CD 14
LPS
MD-2
TLR-4
TLR4 – transmembrane protein, transmits the LPS recognition signal to the interior of the cell, where signal transduction and gene transcription pathways promote the production and/or secretion of numerous molecules that mediate the inflammatory response
LPS
MD-2Extracellular protein which binds the lipid A moiety of LPS
Toxin Recognition by the Host
Signaling complex
Mandell Principles of Infectious Disease
12

Inflammatory Mediators
TNF alpha ◦Potent mediator of the subsequent
inflammatory response◦Stimulates muscle breakdown and
cachexia, mediates coagulation activation, enhances expression of adhesion molecules, prostaglandin E2 & PAF
• IL-1– Released in response to inflammation– Endogenous pyrogen
• IL-6– Increasingly expressed during stress as
in septic shock.– Promote intravascular coagulation
• Other Interleukins, Cytokines and Chemokines increased capillary permeability and blood flow, infiltration of neutrophils, and pain.
Schwartz Principles of Surgery
Mandell Principles of Infectious Disease
13

Microbial killingThe major inherited mechanisms for killing
microbes in the blood are soluble molecules: ◦ the mannose-binding lectin & C-reactive protein
(CRP) pathways for activating complement◦ the alternative complement pathway ◦antibacterial proteins (such as bactericidal
permeability-increasing protein [BPI])◦natural IgM antibodies.
Increased capillary permeability allows these molecules to diffuse into tissues where there is local inflammation.
Mandell Principles of Infectious Disease
14

Control MechanismsLocal Control Mechanisms Intracellular factors
(e.g., suppressor of cytokine signaling 3 and IL-1 receptor associated kinase 3)
Molecules derived from essential polyunsaturated fatty acids (lipoxins, resolvins, and protectins)
Enzymatic inactivation of microbial signal molecules (e.g., LPS)
Systemic Control Mechanisms
• LPS-binding protein• Glucocorticoids• Epinephrine • Prostaglandin E2 • IL-10, and C-reactive
protein • IL-1 receptor
antagonist. • soluble TNF receptors • protease inhibitors or
antioxidants; • Hepcidin Harrison’s Principle of IM15

16

CLINICAL MANIFESTATIONPatients usually manifests symptoms and signs
related to primary infection.
Manifestations of Systemic Inflammatory Response
Evidence of shock
(-) fever: most common in neonates, elderly patients and in persons with uremia or alcoholism
Harrison’ s Internal Medicine 18th edition17

Hyperventilation Encephalopathy Hypotension DIC, acrocyanosis, ischemic necrosis of
peripheral tissues (e.g., digits)• Skin: hemorrhagic lesions, bullae, cellulitis.
Skin lesions may suggest specific pathogens—e.g., petechiae and purpura with Neisseria meningitidis, ecthyma gangrenosum with Pseudomonas aeruginosa.
• Gastrointestinal• Hypoxemia
CLINICAL MANIFESTATION
Harrison’ s Internal Medicine 18th edition
18

1. Cardiopulmonary Complications
◦Acute respiratory distress syndrome◦Hypotension◦Decrease Myocardial function
II. Renal ComplicationsoOliguiraoAzotemiao Proteinuriao Nonspecific casts
MAJOR COMPLICATIONS
19

III. Coagulopathy• Thrombocytopenia in 10-30%• Platelet usually very low
<50,000/uL in px with DIC
IV. Neurological Complications• DDX: Guillain-Barre
syndrome, metabolic disturbance, toxin activity
MAJOR COMPLICATIONS
Harrison’ s Internal Medicine 18th edition20

LEUKOCYTOSIS with a left shift
ThrombocytopeniaHyperbilirubinemi
aProteinuriaNeutrophils - may
contain toxic granulations, Dohle bodies or cytoplasmic vacuoles
Early sepsis: hyperventilation respiratory alkalosis
Respiratory muscle fatigue & accum. of lactate metabolic acidosis
ABG: hypoxemia (initially correctable with supplemental oxygen)
LABORATORY FINDINGS
Harrison’ s Internal Medicine 18th edition21

CXR: normal or may show evidence of underlying pneumonia, volume overload, or the diffuse infiltrates of ARDS
ECG: sinus tachycardia & nonspecific ST-T wave abnormalities
Diabetic patients: ◦ develops
hyperglycemia◦ Severe infection
diabetic ketoacidosis (may exacerbate hypotension)
◦ Serum albumin - initially within normal range, declines as sepsis continues
LABORATORY FINDINGS
Harrison’ s Internal Medicine 18th edition22

NO specific diagnostic test Diagnostically sensitive
findings: Fever or hypothermia Tachypnea Tachycardia Leukocytosis or
leukopenia
Acutely altered mental status
Thrombocytopenia
Elevated blood lactate level
hypotension
DIAGNOSIS
23

36% normal temperature40% normal respiratory rate10% normal pulse rate33% normal WBC count
Systemic responses of uninfected patients with other conditions are similar to those characteristic of sepsis
DIAGNOSIS
Harrison’ s Internal Medicine 18th edition24

Definitive etiologic diagnosis ◦ requires isolation of the microorganism from blood
or a local site of infection
Culture: At least 2 blood samples (10mL each)◦ should be obtained (from different venipuncture
sites)
Gram (-) bacteremia ◦ typically low grade (10 organism/mL of blood),
prolonged incubation may be necessary
S. aureus grows more rapidly – detectable in blood within 48 hours
Harrison’ s Internal Medicine 18th edition25

Antimicrobial Agents
Given after blood and other relevant sites have been cultured.
major determinant of outcome: ◦interval between hypotension and the administration antimicrobial chemotherapy
◦a delay of 1 h is associated with lower survival rates.
Harrison’ s Internal Medicine 18th edition
Treatment:
27

A Single antimicrobial agent for treatment of known pathogens is adequate.
Combination antimicrobial therapy is NOT superior to monotherapy in treating Gram(-) bacteremia. EXCEPT in P.aeruginosa bacteremia where aminoglycoside monotherapy is less effective than combination of an aminoglycoside with an antipseudomonal -lactam agent.
antimicrobial therapy-at least 1 week;
Factors in duration of treatment:◦site of infection◦adequacy of surgical drainage, ◦underlying diseases◦susceptibility of the bacterial isolate(s) to
antimicrobials. Harrison’ s Internal Medicine 18th edition
Antimicrobial Agents
28

Factors in duration of treatment:
site of infection adequacy of surgical drainage, underlying diseases susceptibility of the bacterial isolate(s)
to antimicrobials.
Harrison’ s Internal Medicine 18th edition
Antimicrobial Agents
29

Clinical Condition Antimicrobial Regimens (Intravenous Therapy)
Immunocompetent adult The many acceptable regimens include (1) ceftriaxone (2 g q24h) or ticarcillin-clavulanate (3.1 g q4–6h) or piperacillin-tazobactam (3.375 g q4–6h); (2) imipenem-cilastatin (0.5 g q6h) or meropenem (1 g q8h) or cefepime (2 g q12h). Gentamicin or tobramycin (5–7 mg/kg q24h) may be addedto either regimen. If the patient is allergic to -lactam agents, use ciprofloxacin (400 mg q12h) or levofloxacin (500–750 mg q12h) plus clindamycin (600 mg q8h). If the institution or the community has a high prevalence of MRSA isolates, add vancomycin (15 mg/kg q12h) to each of the above regimens.
Neutropeniaa (<500 neutrophils/L)
Regimens include (1) imipenem-cilastatin (0.5 g q6h) ormeropenem (1 g q8h) or cefepime (2 g q8h); (2) ticarcillin-clavulanate (3.1 g q4h) or piperacillin-tazobactam (3.375 g q4h) plus tobramycin (5–7 mg/kg q24h). Vancomycin (15 mg/kg q12h) should be added if the patient has an infected vascular catheter, if staphylococci are suspected, if the patient has received quinolone prophylaxis, if the patient has received intensive chemotherapy that produces mucosal damage, if the institution has a high incidence of MRSA infections, or if there is a high prevalence of MRSA isolates in the community.
Splenectomy Cefotaxime (2 g q6–8h) or ceftriaxone (2 g q12h) should be used. If the local prevalence of cephalosporin-resistant pneumococci is high, add vancomycin. If the patient is allergic to -lactam drugs, vancomycin (15 mg/kg q12h) plus ciprofloxacin (400 mg q12h) or levofloxacin (750 mg q12h) or aztreonam (2 g q8h) should be used.
IV drug user Nafcillin or oxacillin (2 g q8h) plus gentamicin (5–7 mg/kg q24h). If the local prevalence of MRSA is high or if the patient is allergic to -lactam drugs, vancomycin (15 mg/kg q12h) with gentamicin should be used.
AIDS Cefepime (2 g q8h), ticarcillin-clavulanate (3.1 g q4h), or piperacillin-tazobactam (3.375 g q4h) plus tobramycin (5–7 mg/kg q24h) should be used. If the patient is allergic to -lactam drugs, ciprofloxacin (400 mg q12h) or levofloxacin (750 mg q12h) plus vancomycin (15 mg/kg q12h) plus tobramycin should be used.
Initial Antimicrobial Therapy for Severe Sepsis with No Obvious Source in Adults with Normal Renal Function
Harrison’ s Internal Medicine 18th edition
30

Removal of the Source of Infection Indwelling IV cathethers should be removed and the
tip should be rolled over an agar plate for culture.
After antibiotic therapy, a new catheter should be replaced at a different site and Foley and drainage catherters should be replaced
Consider paranasal sinusitis in patients who have undergone nasal intubation.
In patients with abnormal CXR, a CT of the chest may identify parenchymal,mediastinal or pleural diseases.
In neutropenic patients, sites of tenderness and erythema must be carefully sought.
In sacral or ischial decubitus ulcers, exclude pelvic of soft tissue pus collections wit CT/MRI
In severe sepsis from the urinary tract, rule out urethereal obstruction, pernephric abcess and renall abcess by sonography or CT. Harrison’ s Internal Medicine 18th
edition
Treatment:
31

Hemodynamic, Respiratory, and Metabolic Support
Primary goals ◦ restore adequate oxygen and substrate
delivery to the tissues.◦ improve tissue oxygen utilization and cellular
metabolism. Initial management of hypotension
• Administration of IV fluids (1-2L of NSS over 1-2 h)
Circulatory adequacy can be assessed by:◦ clinical parameters (mentation, urine output,
skin perfusion) ◦ measurements of oxygen delivery and
consumption. Harrison’ s Internal Medicine 18th
edition
Treatment:
32

"early goal-directed therapy" (EGDT) • resuscitation based on maintenance of the
SvO2 at >70% was associated with significantly improved survival of patients
• The treatment algorithm ◦rapid administration of fluids, ◦antibiotics, and ◦vasopressor support; erythrocyte transfusion (to maintain the hematocrit above 30%); and
◦Dobutamine is administered if fluids, erythrocytes, and pressors did not result in an SvO2 of >70%. Harrison’ s Internal Medicine 18th
edition
Hemodynamic, Respiratory, and Metabolic Support
33

Vasopressin ◦potent vasoconstrictor ◦Useful in vasodilatory shock and relative
resistance to other pressor hormones.
Ventilator therapy ◦For progressive hypoxemia, hypercapnia,
neurologic deterioration, or respiratory muscle failure.
Bicarbonates administered if severe metabolic acidosis <7.2ph
FFP and platelet transfusion in DIC if complicated by major bleeding.
In hypercatabolic patients and Acute renal failure, hemodialysis or hemofiltration is beneficial.
Harrison’ s Internal Medicine 18th edition34

General SupportNutritional supplementation may reduce
the impact of protein hypercatabolism in patients with prolonged sepsis.
Prophylactic heparinization to prevent deep venous thrombosis for patients without active bleeding or coagulopathy.
Maintenance of blood glucose improved survival rates among patients who have undergone major surgery and received IV glucose.
Hypoglycemia was much more common in the intensive-insulin group.
Harrison’ s Internal Medicine 18th edition
Treatment:
35

Other MeasuresEndotoxin-neutralizing proteins, inhibitors of COX or nitric oxide synthase, anticoagulants, polyclonal immunoglobulins, glucocorticoids, andantagonists to TNF-, IL-1, PAF, and bradykinin.
Harrison’ s Internal Medicine 18th edition
Treatment:
36

Recombinant activated protein C (aPC) ◦Treatment of patients with severe
sepsis or septic shock. ◦The FDA approved aPC for use in adults
(>18 years of age) who meet the APACHE II criterion and have a low risk of hemorrhage-related side effects.
◦aPC is administered as a constant IV infusion of 24 g/kg per hour for 96 h.
Harrison’ s Internal Medicine 18th edition37

should not be given to patients• platelet counts of <30,000/L • dysfunction of one organ system and
surgery within 30 days. Treatment with aPC should not be
started >24 h after the onset of severe sepsis, nor should it be used in the patient subsets—e.g., patients with pancreatitis or AIDS—that were excluded from the clinical trial.
Harrison’ s Internal Medicine 18th edition38

"bundling" of multiple therapeutic maneuvers as the standard of care for severe sepsis.
The proposed resuscitation (6-h) bundle incorporates most of the elements discussed above for acute (EGDT) resuscitation.
The management (24-h) bundle includes three measures of uncertain or marginal benefit: ◦tight control of blood glucose,
administration of low-dose hydrocortisone, and treatment with aPC.
Harrison’ s Internal Medicine 18th edition39

Harrison’ s Internal Medicine 18th edition
PreventionLimit the use of indwelling vascular and
bladder catheters
Reduce the incidence and duration of profound neutropenia (<500 neutrophils/L)
Aggressively treating localized nosocomial infections
Indiscriminate use of antimicrobial agents and glucocorticoids should be avoided, and optimal infection-control measures should be used
40