Presentation haemangioma hyoid bone surgical meetingl.
-
Upload
isra-institute-of-rehab-sciences-iirs-isra-university -
Category
Health & Medicine
-
view
143 -
download
0
Transcript of Presentation haemangioma hyoid bone surgical meetingl.

Bone Haemangioma Of The Hyoid Bone
Author No.: 1. Dr. Ghulam Saqulain, D.L.O, F.C.P.S (ENT)Otolaryngologist (Head of Department)
Author No.: 2. Dr. Muhammad Mumtaz Khan,MBBS, M.Phil (Histopath)Pathologist
A Case Report:

Abstract & Key Words Abstract
Primary hemangiomas of bone are uncommon tumors. They constitute less than 1.0% of all bone neoplasms. Bone haemangiomas are most commonly found in the vertebral column followed by cranium and maxillofacial bones in decreasing order of frequency. Occurrence of bone haemangioma in association with long bones, short tubular bones and ribs is extremely rare. In this article, we report a case of hyoid bone haemangioma. The present case is the first reported case of bone haemangioma arising from the hyoid bone. A net search did not reveal any precedence in world literature for a bone haemangioma arising from the hyoid bone.
Key Words:
Hyoid boneHaemangiomaPrimary bone neoplasm

Case Report
A Thirty year old male presented, to the ENT Department at Capital Hospital, Islamabad, with a slow growing swelling in right submandibular region of 1 ½ year duration with no other symptom.
Examination showed a 8 cm x 5 cm, ovoid, non pulsatile mass in submandibular region extending to the retromandibular area.
The swelling lacked signs of inflammation. It was firm in consistency with well defined rounded margins and moving with the movement of the hyoid bone.
Cranial nerve examination did not reveal any involvement.
No other positive finding Ear Nose and throat examination.

Routine investigations were all normal save for a opaque shadow in sub- mandibular area observed on plain films.
Fine needle aspiration for cytology failed due to non yielding nature of the swelling.
Incision biopsy also failed due to the fact that we did not take a deep biopsy due to the hard nature of the swelling.
CP WBC 7.2 10^3/uL
NE% 52.2 Ly% 34.4 MO% 8.7 EO% 4.7
Hb 15.7 g/dl PLT 348 10^3/uL
ESR 05mm/1st hr. Blood Group A +ve. HCV Ab Negative HBsAg Negative LFT’s
ALAT 37 U/l Alk. Phos 106 U/l Total Bilirubin 0.8 mg/dl
RFT’S Urea 31 mg/dl Creatinine 0.7 mg/dl
RBG 84 mg/dl

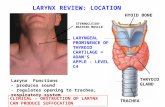
CT Scan14.6.2004, Iran
There is an ill-defined and heterogenous enhancing mass in rt. Parapharyngeal space extending caudally to the anterior aspect of the neck with erosion and expansion of the hyoid bone.
Possibility of salivary gland masses is suggested. Possibility of hyoid bone originating primary or secondary masses could be in the DDX. Biopsy on the guide to sonography would be helpful.


MRI12.12.2005 NIHd
MRI neck shows a well defined, iso-intense, moderately enhancing mass lesion occupying the right sub mandibular and retro mandibular region,pressing on adjacent structures, It measured 3.2 x 2.2 cms. The mass is slightly indenting the nasopharynx on the right side. The mass showed heterogeneous signal on T2W1 sequence.




Having taken advice from our pathologist, an excision biopsy was planned.
Keeping in view the immobile nature of the mass, after due preparation including arrangement for blood transfusion patient was operated on 24.12.05 10.30 am ( 1 ½ Hr. surgery) under General Anaesthesia with endotracheal intubation.

The mass was approached through a wide submandibular incision 2-3 cm below the mandibular margin.
On exposure a hard ovoid mass with well defined rounded margins was encountered arising from the hyoid bone and involving the greater cornu.


The muscular attachments were removed from the swelling, as if it were a giant greater cornu of the hyoid.

The mass had to be pulled out from the deep sub-mandibular and retro-mandibular area.
There was no extension into soft tissue of neck.
The mass was removed in toto including part of hyoid bone.
There was fortunately no significant bleeding.


Gross Examination
Gross examination of the specimen revealed a bony mass measuring 4.5 x3 x 1.5 cms.
After decalcification the mass was cut into two.

Its cut surface was bony in appearance and showed dark brown and grayish white areas..
Part bearing muscle attachment
Part separate from healthy hyoid bone.

Post Operative Treatment
Antibiotic Analgesics Stitches Removed after a week

HISTOPATHOLOGYand DIFFERENTIAL DIAGNOSIS

Differential Diagnosis
1. At clinical leveli. Site ii. Symptoms
2. X ray and MRI based
3. At Gross level
4. Microscopic

Osteochondroma

Osteochondroma


Osteochondroma

Osteochondroma





CavernousHemangioma

Capillary Hemangioma

Osteochondroma

DIAGNOSIS
BONE HAEMANGIOMA
OF THE HYOID BONE

Thanks and Have a nice day

BONE HAEMANGIOMABackground
Bone hemangiomas are benign, malformed vascular lesions, overall constituting less than 1% of all primary bone neoplasms.
They occur most frequently in the vertebral column (30-50%) and skull (20%), whereas involvement of other sites (including the long bones, short tubular bones, and ribs) is extremely rare.
Bone hemangiomas are usually asymptomatic lesions discovered incidentally on imaging or postmortem examination and mostly encountered in the middle-aged. The symptoms are largely nonspecific and depend on the site, size, and aggressiveness of the tumors.

Pathophysiology
Bone hemangiomas usually occur in the medullary cavity surface-based hemangiomas uncommonly are
encountered in the cortex, periosteum, and subperiosteal regions.
Gross pathology usually reveals well-demarcated, unencapsulated lesions with cystic red cavities. Microscopic examination shows hamartomatous proliferations of vascular tissue within endothelial-lined spaces.
There are 4 histologic variants of hemangioma, classified according to the predominant type of vascular channel: cavernous, capillary, arteriovenous, and venous.
These types can coexist.

Bone hemangiomas are predominantly of the cavernous and capillary varieties. Cavernous hemangiomas most frequently occur
in the skull Capillary hemangiomas predominate in the
vertebral column Overall the Cavernous type is most common in
bone Various types of nonvascular tissues may form the matrix
within which the angiomatous tissue is interspersed, typically in cavernous hemangiomas. These include fat, smooth muscle, bone trabeculae, fibrous tissue, and clotted blood products.

A greater proportion of fat in vertebral hemangiomas is associated with a reduced likelihood of symptoms. Conversely, neural compression is more likely with a greater proportion of hypervascular or hemangiomatous tissue.
Epithelioid hemangiomas are also benign vascular neoplasms
usually occurring in the skin and superficial tissues. They are uncommonly encountered in bone. Cytologically, they may be confused with malignant tumors. Indentation or erosion of bone cortex with or without reactive bone formation may occur due to secondary involvement from soft tissue hemangiomas.

Frequency In the US:
Vertebral hemangiomas are common, with a rate of 10-12% in autopsy series.
Osseous hemangiomas are less frequent at other sites.
Race: There is no documented racial variation in the frequency of hemangiomas.
Sex: Osseous hemangioma generally occurs more commonly in females than males, with a ratio of 3:2.
Age: The peak incidence is in the fifth decade osseous hemangiomas can be encountered at any age. The rare periosteal and other surface-based
hemangiomas tend to occur in younger patients.

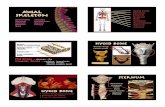
Anatomy:
Vertebral hemangiomas are the most common benign tumor of the spinal column, and they occur most frequently in the lower thoracic and upper lumbar spine. The lesions are most often solitary, but they may be multiple in up to one third of cases.
Calvarial hemangiomas constitute 20% of all hemangiomas, but only 0.2% of all bone neoplasms. They are centered in the diploic space and usually located in the frontal and parietal regions. They can be expansile, usually affecting the outer table to a greater extent.

The skull base and facial bones are extremely rarely involved. The mandible is the commonest site of facial osseous hemangiomas.
Long-bone hemangiomas are uncommon. They are found mainly in the tibia, femur, or humerus. They have a predilection for the metaphyseal or diaphyseal regions but can involve the epiphyses and even extend across the joint space.
The rare surface-based hemangiomas occur predominantly in the extremities, typically in the anterior tibial diaphysis.

Clinical Features & Complications
Complications arising from osseous hemangiomas are rare, and their severity depends on the location of the lesions.
The large majority of lesions are asymptomatic, and clinically significant symptoms develop in only 1-2%. When symptoms occur, they can be vague and nonspecific.
Lesions in the spine and other sites may cause: pain and discomfort from pressure effects, displacement or invasion of adjacent structures, and pathologic fracture.

Vertebral collapse complicating spinal hemangiomas can cause neural compression due to impingement from bone. Neural
compression can produce paralysis and/or paraplegia or bladder and bowel dysfunction, whereas radicular symptoms occur from nerve-root impingement
hematoma, or extraosseous/epidural soft-tissue extension of the
hemangioma itself. This may result in paraplegia (cord compression), radiculopathy (nerve-root impingement), or varying degrees of autonomic neurologic dysfunction.
Expansion and collapse of previously asymptomatic spine hemangiomas has been known to occur in pregnancy.
Bone overgrowth with limb-length discrepancy may occur in long bones due to localized hypervascularity.
Hemorrhagic complications can occur; these are usually iatrogenic and are due to biopsy or surgery. Fatalities have been reported, although these are rare.

Thrombocytopenic coagulopathies due to platelet sequestration within intraosseous or subperiosteal hemangiomas, most commonly in flat bones, have been known to occur, but this phenomenon is better associated with cutaneous or soft-tissue hemangiomas in infancy.
Calvarial lesions tend to be most significant clinically.
Craniofacial hemangiomas may result in a palpable lump.
Lesions in extremeties. Localized swelling, limb hypertrophy, and pain can be characteristics of hemangiomas in the extremities. Hemorrhage can occur, usually in the setting of trauma, biopsy, surgery or other medical or dental interventions.

Radiology
Preferred Examination: Plain radiography is useful for evaluation as the first line imaging modality in most cases. Radiographic appearances differ depending on the anatomic site and histologic variant of the lesion. However, the radiographic hallmark of bone hemangiomas is a prominent trabecular pattern. Radiographic appearances in craniofacial hemangiomas are often nonspecific. Mixed radiopacity, radiolucency, and honeycomb patterns are observed.
Radiographic patterns may be nonspecific, necessitating further imaging or histology to achieve diagnosis. This is especially true in extraspinal hemangiomas occurring in an age group and location in which other more ominous diagnostic entities, such as myeloma or metastases, are more common.

CT is especially useful for assessing changes in bone trabeculae.
The superior soft tissue and bone marrow contrast resolution of MRI allows for better evaluation of extraosseous extension and depiction of the characteristic fatty content in vertebral hemangiomas and also flow patterns in general. The multiplanar capabilities of MRI are also crucial in defining the extent of neural involvement in the spine and planning therapeutic interventions.
Limitations of Techniques: Despite the added diagnostic information available with CT and MRI, the angiomatous nature of many extraspinal lesions can be confirmed only with histologic analysis.

Intervention
Hemangiomas should be treated only if symptomatic Treatment options depend on:
Site of the lesion, the severity of the symptoms, and the medical expertise available.
Medical treatment and clinical observation can be used as first-line management, especially in cases with mild-to-moderate symptoms. When this does not suffice or when clinically appropriate, other treatment options are available.

Treatment Modalities Embolization
Embolization of hemangiomas is performed prior to surgery and helps reduce the vascularity of the lesions and, therefore, intraoperative blood loss.
Surgery
Surgery is usually reserved for refractory cases and in those complicated by vertebral collapse with neural compression. It is ideally preceded by lesion embolization and may be combined with postoperative radiation therapy, especially when pain occurs with neurologic compression. The surgical options may entail lesion excision, decompressive laminectomy, resection of epidural extension, bone grafting, and use of metallic prostheses.
Percutaneous vertebroplasty Radiotherapy






![Automatic hyoid bone detection in uoroscopic images using deep …imedlab.org/pdfs/papers/...bone-dysphagia-tracking-detection-multib… · You Only Look Once (YOLO) [34] and Single](https://static.fdocuments.in/doc/165x107/5ece30f06bbfcd259117911d/automatic-hyoid-bone-detection-in-uoroscopic-images-using-deep-you-only-look-once.jpg)